Abstract
Objective
To evaluate a faith-based intervention (“Sisters in Motion”) intended to increase walking among older, sedentary African American women.
Design
RCT, using within-church randomization.
Setting
Three Los Angeles churches.
Participants
Sixty-two African American women >60 years who reported being active <30 minutes 3×/week and walked <35,000 steps/week as measured by a baseline pedometer reading.
Intervention
Intervention participants received a multi-component curriculum including Scripture readings, prayer, goal-setting, a community resource guide, and walking competitions. Both intervention and control participants participated in physical activity sessions.
Measurements
The primary outcome was change in weekly steps walked as measured by pedometer. Secondary outcomes included change in systolic blood pressure (SBP). Outcomes were assessed at baseline and 6 months post intervention.
Results
Eighty-five percent of participants attended at least 6 of 8 sessions. Intervention participants averaged 12,727 steps per week at baseline, compared to 13,089 steps among controls. Mean baseline SBP was 156 mmHg for intervention participants and 147 mmHg among controls (p=0.10). At 6 months, intervention participants had increased their weekly steps by 9,883 on average, compared to an increase of 2,426 for controls (p=0.016); SBP decreased on average by 12.5 mmHg among intervention participants and only 1.5 mmHg among controls (p=0.007).
Conclusions
The Sisters in Motion intervention led to an increase in walking and a decrease in SBP at 6 months. This is the first RCT of a faith-based physical activity program to increase physical activity among older African American women, and represents an attractive approach to stimulate lifestyle change within this population.
Keywords: Physical Activity, African Americans, Randomized Controlled Trial
Regular physical activity provides substantial health benefits for older adults, by preventing or ameliorating chronic diseases and disabilities and by helping maintain personal independence.1-4 Older African American women are the least physically active race-gender subgroup in the United States.5 Despite this disparity in rates of physical activity, few of the reported physical activity interventions for older adults report outcomes by race and gender.6-8 In addition, there are very few physical activity interventions that have specifically targeted older, sedentary African American women.8
Integrating behavioral strategies such as building self-efficacy for exercise within a faith-based structure holds promise for decreasing sedentary lifestyles among older African American women.2, 8, 9 Spirituality and religion are powerful cultural influences for many African Americans, and over 95% of African American older adults report praying nearly every day.10 Spirituality and faith are often used as resources to help overcome personal crises and barriers, and together with approaches such as personal goal setting may help to overcome obstacles to behavior change.
We developed a faith-based, physical activity intervention (“Sisters in Motion”) for African American women 60 years of age and over, and tested it in a pilot randomized controlled trial within 3 churches located in South Los Angeles. We hypothesized that the multi-component Sisters in Motion curriculum would increase physical activity levels among intervention participants compared to control participants, measured at 6 months of follow-up. In addition, we hypothesized that this increase in physical activity would in turn lead to improvement in multiple secondary outcomes, including blood pressure reduction, weight loss, and a decrease in chronic pain.
Methods
Study Design and Participants
The study design was a randomized, controlled trial. The purpose of the study was to evaluate whether a multi-component, faith-based intervention, delivered in a small-group format, could successfully increase physical activity among older, sedentary African American women in the community. The University of California, Los Angeles Institutional Review Board approved the research protocol.
Inclusion criteria were African American race, female sex, age of at least 60 years, self-reported physical activity of less than 30 minutes three times per week, and ability to ambulate without a walker. Exclusion criteria were failure to attend each of 2 baseline, pre-randomization data collection sessions, walking more than 35,000 steps per week at baseline as measured by pedometer, and an affirmative response to any item from the CHAMPS Modified Physical Activity Questionnaire. These items included chest pain with exercise, any history of loss of consciousness, any “heart problems” that participants had been told might make exercise risky, or any other reason why the participant themselves felt that they should not exercise. In addition, we contacted the primary care physician of each potential research subject with a medical consent form, informing the physicians of the study protocol. We were able to identify a primary care physician for all participants. Subjects were excluded if their physician responded and indicated a medical contraindication to participation.
Through word of mouth and existing community contacts, we identified a convenience sample of 3 churches with predominantly African American members that were interested in joining the study. These churches included a Catholic parish, an African Methodist Episcopal (AME) church, and a Seventh Day Adventist church. Study participants at each of the churches were recruited with the assistance of church members, typically the leaders of existing “senior groups” within each church. In addition, we placed flyers advertising the research study in community centers in the vicinity of each participating church. The program was particularly well-received at 1 of the 3 churches, with high participant demand, so we recruited a second cohort after the first group finished.
Once participants provided informed consent and were enrolled in the study, they attended two data gathering sessions in which they completed a baseline survey and had their weight and blood pressure measured. Blood pressure was measured on two occasions at least 15 minutes apart, and the values were averaged together to provide a single result. Participants were also provided with a Yamax SW-200 Digiwalker pedometer and instructed in proper wearing technique and procedure, including the need to wear the pedometer at all times other than when bathing or sleeping.
Randomization
After enrolling at least 15 participants at each church and collecting baseline data as described above, we implemented a modified randomization procedure within that church. We identified two different weekdays for study implementation, based on the availability of space at each church. We then allowed participants to sign up for the day that best fit their personal schedule before we designated one day for the intervention group and the other day for the control group. Approximately 65% of participants expressed no preferences about scheduling, and we assigned these participants to one of the two weekdays with the use of a random number generator. Once participants were evenly distributed between the two study days, we used the random number generator to designate one as the “intervention” day and the other as the “control” day. We used this modified randomization procedure, allowing participants to select the day on which they attended the study, in order to provide the African American women with greater control of their experience as research participants.
Description of the Intervention
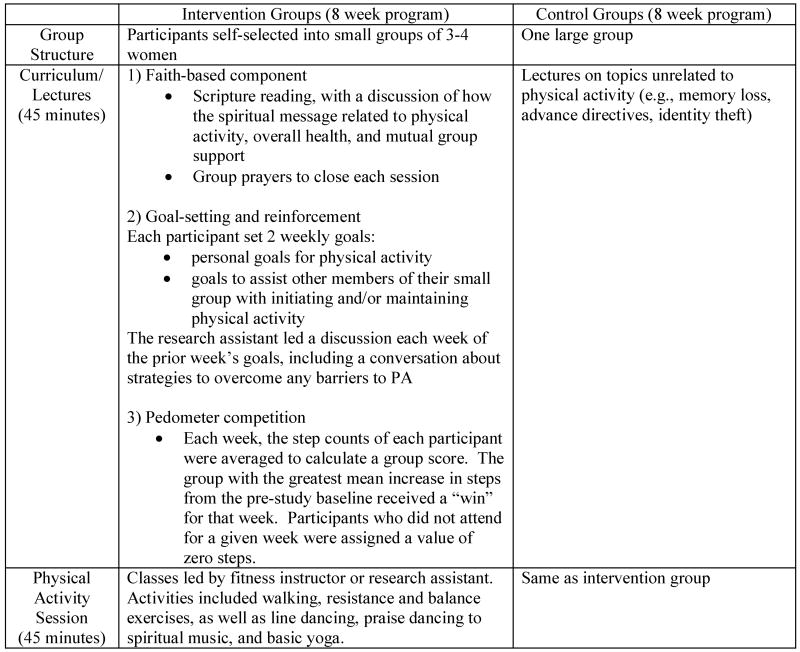
The intervention and control protocols were implemented separately during 8 weekly 90-minute meetings on two different days of the week, followed by separate once-monthly meetings for 6 months also on two different days of the week. One research assistant led the intervention group meetings while another led the control group meetings, following separate scripted protocols. While both the intervention and control groups engaged in 45 minutes of physical activity each week, only the intervention participants were exposed to the faith-based curriculum. Since we explained the purpose of this behavioral intervention study in detail during the informed consent process, it was not possible to “blind” the participants to their randomized study assignment. The research assistants were also aware of the randomized study assignment for their groups. The Principal Investigator met individually with each research assistant for 2 hours prior to the first weekly session to discuss the research protocols, and then weekly for 1 hour thereafter to discuss the previous session and plan the next session.
The 8-week intervention curriculum was designed to incorporate evidence-based best practice approaches for physical activity programs targeting older adults, including providing activity choices, providing positive reinforcement, enhancing self-efficacy and building social support for exercise.9 The goal during the first 8 weeks was to establish active behaviors that would persist over time after the curriculum had been completed. Control participants were not exposed to any of the intervention curriculum, but instead received lectures of the same time duration that addressed unrelated topics such as advanced directives and identity theft. Intervention and control groups met on different days of the week to minimize contamination.
The intervention curriculum included 4 components, including a community resource guide based on the Community Healthy Activities Model Program for Seniors (CHAMPS) model,11 and weekly Scripture readings and group prayer (Figure 1). Participants in the intervention group at each church self-selected into small groups of 3 or 4, and set personal activity goals for themselves as well as to help other members of their small group become and remain active. Finally, the small groups competed in a weekly pedometer competition. The small group with the greatest mean increase in step counts each week compared to baseline was credited with a “win,” although the pedometer readings were never revealed to participants. Members of the small group with the most wins at the end of the 8 weeks each received a $15 gift card. A score of zero steps was averaged into the group mean for any participant who missed a weekly session, in order to encourage attendance.
Figure 1. Details of the Intervention and Control Group Protocols Implemented at Each Site.
Both intervention and control study arms participated in “exercise classes” during their weekly meetings, including flexibility, resistance, and aerobic exercises. The exercise classes were based on the National Institutes on Aging (NIA) Activities for Older Adults,12 and also included line dancing, praise dancing to spiritual music, and basic yoga exercises. After the initial few classes, participants were allowed as a group to decide the specific activities they wanted to emphasize for the remaining classes. An African-American fitness instructor from the community, who was blinded to the randomized study assignments, led the majority of the exercise classes. Although participants in each church were exposed to the main fitness instructor, she had conflicting commitments during some weeks. The research assistants stepped in to lead a minority of the exercise classes for their respective study groups. Of note, we removed the pedometers from participants before each exercise class, manually recorded the readings, and returned them afterwards in order to limit the measured primary outcome to steps that participants walked on their own, outside of the weekly meetings. During this initial phase of the study, the pedometers were taped shut between sessions and participants were specifically instructed not to remove the tape.
After the initial 8 weeks, the intervention groups shifted to monthly meetings for 6 months, with an emphasis on maintaining increases in physical activity (Figure 1). Although the Scripture readings and pedometer competition were discontinued, the groups were encouraged to continue setting activity goals, and some groups continued to engage in prayer around this issue. Participants were asked to wear their pedometers for the week prior to each session. During this phase of the study, pedometers were untaped and group members were able to discuss how many steps they walked and encouraged to discuss strategies to address any decline in steps from the previous month's total. Control groups also met monthly, but instead of discussions on physical activity they had additional lectures on unrelated topics.
Outcome Measures
The research protocol, including baseline and 6-month follow-up data collection, took place from August 2006 through October 2007. Persons not affiliated with the study, who were blinded to randomized study assignment, recorded the post-intervention outcomes. The primary study outcome was change in weekly steps walked at 6-months post-intervention, as measured by pedometer and entered by the research assistant into a study computer. We used Digiwalker Yamax SW-200 pedometers, which have been shown to correlate closely with readings from more expensive accelerometers such as the CSA and Tri-Trac R3D.13 In addition to change in steps walked, we also examined 6-month secondary, exploratory outcomes including change in systolic blood pressure, change in diastolic blood pressure, change in weight, and change in pain as measured by the American Geriatrics Society pain score. As an additional secondary outcome, we examined change in self-reported physical activity as measured by the CHAMPS Physical Activity Questionnaire using a modified version designed for an African American population.14 The CHAMPS questionnaire measures the time spent engaged in each of approximately 40 activities, and we compiled the responses to create a variable measuring weekly hours of overall physical activity.
Other recorded baseline data included information on patient demographics such as age, education, income, self-rated health, and need for assistance with any instrumental activities of daily living (IADL). We gathered information on the number of patient comorbidities,15 and measured several psychosocial characteristics at baseline, including patient self-efficacy for exercise,16 exercise-related social support from family and friends,17 and perceived barriers to exercise.18
Statistical Analyses
We used unadjusted t-tests to compare change scores between intervention and control participants for all study outcomes. As systolic blood pressure values differed significantly between the 2 randomized groups at baseline, we also conducted a linear regression with an indicator for control vs. intervention assignment as a post-hoc sensitivity analysis, controlling for baseline systolic blood pressure. All analyses were conducted with an intention-to-treat design based on initial randomization, regardless of the number of sessions attended.
Results
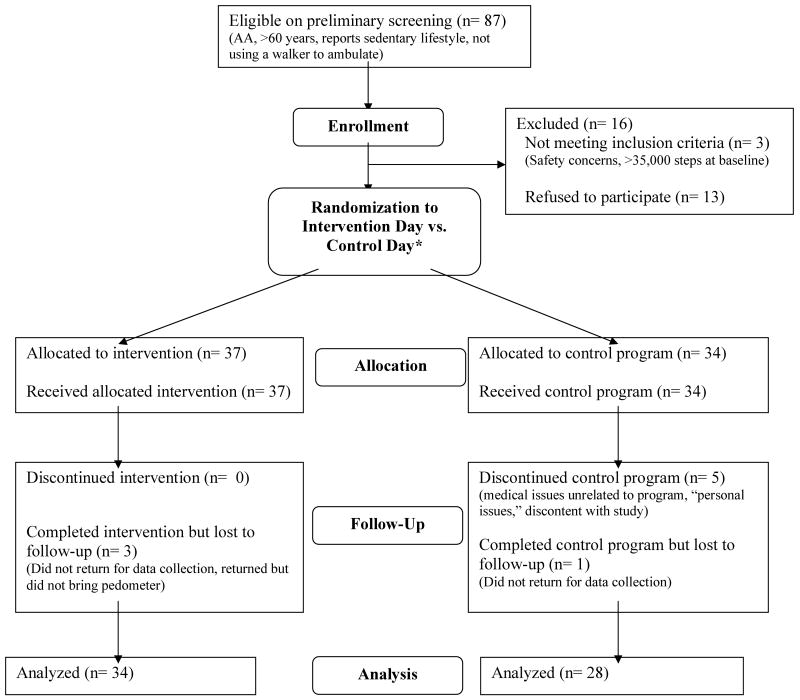
We recruited 87 women who met the study inclusion criteria (Figure 2). Sixteen of the 87 were excluded prior to randomization based on self-reported or provider-reported medical contraindications, participant self-withdrawal for non-medical reasons, or pedometer step counts greater than 30,000 per week at the data-gathering session. The 71 remaining participants were enrolled in the study, with 37 randomized to the intervention arm and 34 to the control arm. Approximately 85% of participants attended at least 6 of the initial 8 weekly sessions, and no research-related adverse events were recorded for any participant. Due to study attrition and loss to follow-up, the analysis of the primary outcome only includes data from 34 intervention participants and 28 control participants.
Figure 2. Flow diagram tracking Sisters in Motion participants.
*Participants were divided between two weekdays (35% selected a particular day, 65% were assigned by investigators). After participants were equally distributed between the two days, one was randomly designated as the intervention day and the other was randomly designated as the control day.
There were no statistically significant differences in baseline demographic and clinical characteristics between intervention and control participants (Table 1). Baseline values of the primary outcome measure were similar across study arms, as intervention participants walked 12,727 steps/week on average compared with 13,089 for control participants (p=0.88). While not statistically significant, there was a trend toward higher baseline systolic blood pressure among intervention as compared to control participants (155.8 mmHg as compared to 146.9 mmHg, p=0.10). There were no statistically significant differences observed at baseline for other secondary outcomes.
Table 1. Baseline Characteristics by Group Assignment.
| Intervention (n=34) |
Control (n=28) |
Unadjusted p-value | |
|---|---|---|---|
| Demographics | |||
| Mean age in years (SD) | 73.3 (9.6) | 72.2 (5.8) | 0.62 |
| Income < $2000/month | 62% | 42% | 0.13 |
| Education <12 years | 24% | 22% | 0.90 |
| Self-rated health (% excellent or very good) | 35% | 31% | 0.71 |
| Requiring assistance with any instrumental activity of daily living (IADL) | 21% | 18% | 0.79 |
| Body mass index, mean (SD) | 29.6 (5.5) | 31.6 (5.4) | 0.17 |
| Comorbidity score, mean (SD) | 2.6 (1.7) | 2.6 (1.4) | 0.86 |
| Psychosocial characteristics | |||
| Self-efficacy for exercise scale*, mean (SD) | 53.1 (22.2) | 55.0 (20.3) | 0.74 |
| Exercise support from family scale†, mean (SD) | 23.3 (8.3) | 22.7 (9.8) | 0.79 |
| Exercise support from friends scale‡, mean (SD) | 21.1 (10.1) | 20.0 (10.2) | 0.68 |
| Perceived barriers to exercise scale§, mean (SD) | 34.2 (10.3) | 33.9 (6.3) | 0.90 |
| Baseline measures of study outcomes | |||
| Primary outcome: Mean steps walked per week (SD) | 12727 (9387) | 13089 (8636) | 0.88 |
| Secondary outcomes: | |||
| CHAMPS score, hours/week of physical activity (SD) | 8.7 (8.9) | 9.5 (8.9) | 0.68 |
| Mean systolic blood pressure, mmHg (SD) | 155.8 (19.7) | 146.9 (22.2) | 0.10 |
| Mean diastolic blood pressure, mmHg (SD) | 82.5 (9.2) | 81.1 (11.3) | 0.61 |
| Mean weight in lbs (SD) | 177.5 (36.7) | 183.7 (43.4) | 0.55 |
| American Geriatrics Society pain score¶, mean (SD) | 25.3 (20.1) | 21.2 (19.3) | 0.42 |
Range from 0-90 with higher numbers indicating greater self-efficacy
Range from 13-65 with higher numbers indicating greater support
Range from 10-50 with higher numbers indicating greater support
Range from 14-70 with lower numbers indicating greater barriers
Range from 0-100 with higher numbers indicating more pain
At 6-month follow-up, intervention participants increased their mean weekly walking activity by 7,457 steps more than control participants, on average (Table 2, p=0.016). The decrease in systolic blood pressure at follow-up was greater for intervention participants as compared to control participants (p=0.007). In a post-hoc regression model controlling for systolic blood pressure at baseline, there was a non-significant trend toward lower blood pressure in the intervention group (data not shown, p=0.07). While intervention participants appeared to have an increase in overall physical activity as measured by the modified CHAMPS questionnaire, lower diastolic blood pressure, lower weight, and greater pain at follow-up compared to control participants, the differences were not statistically significant (p=0.50, p=0.48, p=0.51, and p=0.87 respectively).
Table 2. Study Outcomes at 6 Month Follow-Up, Unadjusted.
| Intervention | Control | Mean difference of I-C (SE) | Unadjusted p-value for difference | |
|---|---|---|---|---|
|
Primary outcome at 6 months: Change in mean steps walked per week (n=62) |
9883 | 2426 | 7457 (3020) | 0.016 |
| Secondary outcomes at 6 months: | ||||
| Change in CHAMPS score (n=61) | 9.5 | 6.9 | 2.6 (3.8) | 0.50 |
| Change in systolic blood pressure (n=61) | -12.5 mmHg | -1.5 mmHg | -11.0 (3.9) | 0.007 |
| Change in diastolic blood pressure (n=61) | -5.9 mmHg | -3.8 mmHg | -2.1 (3.0) | 0.48 |
| Change in weight (n=61) | -2.3 lbs | -1.5 lbs | -0.8 (1.3) | 0.51 |
| Change in American Geriatrics Society pain score (n=61) | 4.3 | 3.7 | 0.6 (3.5) | 0.87 |
Discussion
Sisters in Motion, one of the first physical activity interventions designed to specifically target sedentary, older African American women, resulted in increased walking behavior as measured at 6 months after intervention onset. The increase in steps walked excluded activity in guided exercise classes, and instead represented physical activity undertaken by participants on their own initiative. Compared to control participants, women in the intervention arm had lower systolic blood pressure at follow-up, although baseline values were different across study arms. In a sensitivity analysis that adjusted for baseline systolic blood pressure, this difference had a trend toward statistical significance (p=0.07). This multi-component, faith-based intervention may represent a promising approach to increase physical activity and lower blood pressure among a highly sedentary and hard-to-impact population subgroup.
The increase of approximately 7,000 steps per week walked by intervention participants translates to about 3 miles. This is an important improvement among a sedentary population of older women. Although the amount of time required to walk 3 miles depends on walking speed and stride length, the Sisters in Motion study participants likely increased their activity by about 60 minutes per week if walking at a moderate pace and 70-75 minutes per week if walking at a slower pace.19 Research has established a dose-response benefit to physical activity, with even light or moderate activity associated with some improvement in health outcomes.2 Walking at a light or moderate pace for only 10-15 minutes per day has been linked to lower rates of cardiovascular disease, cardiovascular mortality, and all-cause mortality in post-menopausal women.20-22 The effects of this increase in physical activity in terms of functional outcomes such as mobility, balance, and maintaining independence is less clear, although there may be some benefits as a result of increased energy expenditure and maintained muscular strength.23,24 Of note, recent guidelines endorse that any increase in regular physical activity by older adults is valuable and associated with some health benefits.25
While at least two large cognitive-behavioral interventions implemented in secular community settings have been able to increase physical activity among older African Americans,26,27 many faith-based interventions have been less successful.28-30 A recent pre-post trial of a faith-based program showed an increase in physical activity, although the interpretation of this study is complicated by the absence of a comparison control group.31
The results from the Sisters in Motion pilot randomized trial indicate that integrating a cognitive-behavioral intervention with a faith-based curriculum can in fact be an effective approach. Faith-based programs for older African Americans are attractive in part because they provide the potential for increased “reach” as measured within the RE-AIM model.32 While older African Americans may not be exposed to community centers that offer physical activity programs, over 85% attend church at least a few times per month.10 African Americans who identify strongly with the spiritual program content may also have improved attendance and therefore more intense exposure to the cognitive-behavioral program components.
At 6 month follow-up, the secondary study outcomes did not differ significantly between intervention and control participants. While the trend toward lower systolic blood pressure among intervention participants may represent actual improvement, it may also represent simple regression to the mean given the baseline differences in blood pressure values. A larger, adequately-powered trial of the Sisters in Motion intervention may help to clarify the importance of this finding. We found no significant evidence of either weight loss or decreased pain. While most participants were obese, the lack of weight change is not surprising as the increase in steps walked was unlikely to translate into the 60-90 minutes of daily activity required for weight loss.25, 33 Acute pain among intervention participants from initiating a new activity program may have offset any associated benefits in reduction of chronic pain, leading to a non-significant result.
Although we observed a significant difference in steps walked between the two groups, we did not find a similar difference in self-reported physical activity. This may be due in part to the limitations of a self-reported measure of physical activity. Although we attempted to minimize discussion of physical activity in the control group, participants were aware that the study was measuring changes in physical activity and may have overstated their activity for reasons of social desirability. Alternatively, control participants may have disproportionately engaged in activities not measured by the pedometer, such as stretching or resistance training.
Our study had several limitations. These include a relatively short duration of observation, so we were unable to assess the impact of Sisters in Motion on long-term rates of physical activity. While the competitions and external incentives for the intervention groups to use the pedometers ended after the first 8 sessions, intervention participants may have become more accustomed to using the pedometers regularly compared to control participants. This could have potentially led to an overestimation of the difference in effect size at 6 months. We allowed participants to self-select the weekday on which they wanted to participate before randomization, and there is a possibility that unmeasured differences could have contributed to bias (e.g., participants who selected Fridays were somehow different from participants who selected Tuesdays). In addition, given the multi-component intervention curriculum we were unable to assess which specific activities were the strongest determinants of behavior change. Although we made a deliberate effort to involve churches representing different Christian denominations, the restriction to a single, urban metropolitan area may somewhat limit our generalizability to other African American populations.
In conclusion, we found that a randomized, controlled trial of a faith-based physical activity intervention (Sisters in Motion) led to a moderate increase in walking behavior and decline in systolic blood pressure among older African American women. Although we did not observe significant differences in secondary outcomes such as weight and level of reported pain, this faith-based approach shows promise in increasing physical activity. A larger trial of the intervention protocol, with a longer follow-up period, will determine whether Sisters in Motion produces both sustained changes in walking behavior and blood pressure as well as improvement in outcomes such as chronic pain and health related quality of life, among this largely sedentary population.
Acknowledgments
Sponsor's Role: This study was funded by a diversity supplement awarded to Dr. Duru, by the National Institutes on Aging, to grant #R01-AG024460. Dr. Mangione was supported by UCLA/DREW Project EXPORT, NCMHD, 2P20MD000182. Dr. Mangione also received support from the UCLA Center for Health Improvement of Minority Elderly/Resource Centers for Minority Aging Research, NIH/NIA, under Grant 2P30AG021684. Drs. Duru, Sarkisian, and Mangione received support from the UCLA Older Americans Independence Center, NIH/NIA Grant P30-AG028748, and the content of this paper does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
The organizations funding this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors would like to gratefully acknowledge the support and guidance of Dr. Anita Stewart and Ms. Dawn Gillis at the Institute for Health and Aging, University of California, San Francisco who graciously shared their experiences in developing a physical activity intervention for translation in a community setting. The authors would also like to thank the program participants in the Seniors in Motion for Health (SIM) program in San Francisco, sponsored by the Network for Elders.
Footnotes
Conflict of Interest: The study authors have no financial or personal conflicts of interest related to this manuscript. This includes no employment or affiliations, grants, honoraria, consultancies, stocks, royalties, prior expert testimony, board memberships, patents, or personal relationships that would constitute a conflict.
Author's Contributions: Study Concept and Design: Drs. Duru, Sarkisian, Mangione
Acquisition of Data: Dr. Duru, Ms. Leng
Analysis and Interpretation of Data: Drs. Duru, Sarkisian, Mangione; Ms. Leng
Preparation of Manuscript: Drs. Duru, Sarkisian, Mangione
References
- 1.Physical activity and health: A report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 1996. [Google Scholar]
- 2.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Promoting Active Lifestyles Among Older Adults (online) [May 6, 2010]; Available at: www.cdc.gov/nccdphp/dnpa/physical/pdf/lifestyles.pdf.
- 4.Paterson DH, Jones GR, Rice CL. Ageing and physical activity: evidence to develop exercise recommendations for older adults. Can J Public Health. 2007;98 2:S69–108. [PubMed] [Google Scholar]
- 5.Prevalence of regular physical activity among adults--United States, 2001 and 2005. MMWR Morb Mortal Wkly Rep. 2007;56(46):1209–1212. [PubMed] [Google Scholar]
- 6.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults. A critical review and recommendations. Am J Prev Med. 1998;15(4):316–333. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 7.van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med. 2002;22(2):120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- 8.Marcus BH, Williams DM, Dubbert PM, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006;114(24):2739–2752. doi: 10.1161/CIRCULATIONAHA.106.179683. [DOI] [PubMed] [Google Scholar]
- 9.Cress ME, Buchner DM, Prohaska T, et al. Best practices for physical activity programs and behavior counseling in older adult populations. J Aging Phys Act. 2005;13(1):61–74. doi: 10.1123/japa.13.1.61. [DOI] [PubMed] [Google Scholar]
- 10.Taylor R, Chatters L, Levin J. Religion in the lives of African Americans. Thousand Oaks, CA: SAGE Publications; 2004. [Google Scholar]
- 11.Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M465–470. doi: 10.1093/gerona/56.8.m465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Exercise: a guide from the National Institute on Aging. National Institutes of Health; 2001. [Google Scholar]
- 13.Tudor-Locke C, Williams JE, Reis JP, Pluto D. Utility of pedometers for assessing physical activity: convergent validity. Sports Med. 2002;32:795–808. doi: 10.2165/00007256-200232120-00004. [DOI] [PubMed] [Google Scholar]
- 14.Stewart AL, Mills KM, King AC, et al. CHAMPS physical activity questionnaire for older adults: outcome for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Sangha O, Stucki G, Liang MH, et al. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49(2):156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 16.McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. J Behav Med. 1993;16(1):103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- 17.Sallis JF, Grossman RM, Pinski RB, et al. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 18.Sechrist KR, Walker SN, Pender NJ. Development and psychometric evaluation of the exercise benefits/barriers scale. Res Nurs Health. 1987;10(6):357–365. doi: 10.1002/nur.4770100603. [DOI] [PubMed] [Google Scholar]
- 19.Jordan AN, Jurca GM, Tudor-Locke C, Church TS, Blair SN. Pedometer indices for weekly physical activity recommendations in postmenopausal women. Med Sci Sports Exerc. 2005;37(9):1627–1632. doi: 10.1249/01.mss.0000177455.58960.aa. [DOI] [PubMed] [Google Scholar]
- 20.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 21.Gregg EW, Cauley JA, Stone K, et al. Relationship of changes in physical activity and mortality among older women. JAMA. 2003;289(18):2379–2386. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- 22.Oguma Y, Shinoda-Tagawa T. Physical activity decreases cardiovascular disease risk in women: review and meta-analysis. Am J Prev Med. 2004;26(5):407–418. doi: 10.1016/j.amepre.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Paterson DH, Jones GR, Rice CL. Aging and physical activity data on which to base recommendations for exercise in older adults. Appl Physiol Nutr Metab. 2007;32 2F:S75–S171. doi: 10.1139/H07-165. [DOI] [PubMed] [Google Scholar]
- 24.DiPietro L. Physical activity in aging: changes in patterns and their relationship to health and function. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):13–22. doi: 10.1093/gerona/56.suppl_2.13. [DOI] [PubMed] [Google Scholar]
- 25.Physical activity guidelines for Americans: Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services (online) [May 6, 2010]; Available at: www.health.gov/paguidelines/guidelines/summary.aspx.
- 26.Wilcox S, Dowda M, Dunn A, et al. Predictors of increased physical activity in the Active for Life program. Prev Chronic Dis. 2009;6(1):A25. [PMC free article] [PubMed] [Google Scholar]
- 27.Stewart AL, Gillis D, Grossman M, et al. Diffusing a research-based physical activity promotion program for seniors into diverse communities: CHAMPS III. Prev Chronic Dis. 2006;3(2):A51. [PMC free article] [PubMed] [Google Scholar]
- 28.Yanek LR, Becker DM, Moy TF, et al. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep. 2001;116 1:68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Young DR, Stewart KJ. A church-based physical activity intervention for African American women. Fam Community Health. 2006;29(2):103–117. doi: 10.1097/00003727-200604000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Wilcox S, Laken M, Bopp M, et al. Increasing physical activity among church members: community-based participatory research. Am J Prev Med. 2007;32(2):131–138. doi: 10.1016/j.amepre.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 31.Whitt-Glover MC, Hogan PE, Lang W, et al. Pilot study of a faith-based physical activity program among sedentary blacks. Prev Chronic Dis. 2008;5(2):A51. [PMC free article] [PubMed] [Google Scholar]
- 32.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]