Abstract
Objective
To investigate predictors of readmission to inpatient psychiatric treatment for children aged 5 to 12 discharged from acute-care hospitalization.
Method
One hundred nine children were followed for 1 year after discharge from inpatient care. Time to rehospitalization was the outcome of interest. Predictors of readmission, examined via the Cox proportional hazards model, were symptom and family factors assessed at admission, aspects of psychiatric treatment, and demographic variables.
Results
The Kaplan-Meier rehospitalization risk within 1 year of discharge, taking into account known readmissions and censored observations, was 0.37. Most readmissions (81%) occurred within 90 days of discharge. Four variables contributed simultaneously to predicting readmission risk. More severe conduct problems, harsh parental discipline, and disengaged parent–child relations conferred a higher risk for rehospitalization; these risks were attenuated when parents disclosed higher stress in their parenting roles.
Conclusions
Findings showed that psychiatric rehospitalization of children is common, most likely in the trimester after discharge, and highly related to both child symptoms and family factors measurable at admission. Results suggest that efforts to improve postdischarge outcomes of children should target the initial period following inpatient care, address vigorously the complex treatment needs of those with severe conduct problems, and aim to improve parent–child relations.
Keywords: hospitalization, psychiatric services, behavior disorder, family processes
Although lengths of stay and total expenditures for the inpatient psychiatric treatment of children and adolescents have declined in recent years, the number of preadolescents admitted to psychiatric inpatient services has increased markedly (Pottick et al., 2000; Ringel and Sturm, 2001). Studies conducted before the adoption of care and cost management by insurers indicated that over 25% of child and adolescent inpatients were readmitted within 1 year of discharge (Asarnow et al., 1988; Davis et al., 1980; Pavkov et al., 1997; Solomon et al., 1993), with similar or higher rates reported for longer follow-up periods (Parham et al., 1987; Pfeffer et al., 1992). Current readmission rates may be higher, since the shorter lengths of stay that accompanied managed care have been associated with increased medical rehospitalization for children and adolescents (Wickizer et al., 1999). Readmission to inpatient care is therefore a frequent, unfavorable outcome for a growing patient group. However, limited information on the risk factors for children’s rehospitalization constrains the development of practices to avert it.
Two prior studies of rehospitalization risk included a significant number of preadolescents in cohorts that combined children and adolescents (mean age 13 years), but the samples comprised dependents of military personnel (Foster, 1999) and children in state custody (Romansky et al., 2003). Another study followed a predominantly adolescent sample discharged from long-term state hospitals (mean age 14.5 years) (Pavkov et al., 1997); this group may not generalize to the majority of hospitalized children, who are admitted to acute-care units (Pottick et al., 2000).
Like most health services, psychiatric rehospitalization reflects the joint influence of symptom factors (such as illness type and severity) and contextual factors (Andersen and Newman, 1973). Accordingly, this study included diagnosis and overall disorder severity at admission as potential illness-related predictors of rehospitalization. Because disruptive and mood disorders have been reported to increase the readmission risk among youths (Foster, 1999), ratings to quantify these dimensions at admission were also used.
Among contextual influences, family factors seem particularly important to children’s readmission. First, parents have a pivotal role in seeking rehospitalization or accepting recommendations to readmit. Second, family factors may affect the child’s postdischarge clinical course and thereby have an impact on the rehospitalization risk. Parental stress, parenting practices, and family environment constituted a group of family-related predictors. In one study, children in residential treatment centers were hospitalized less often when staff were more involved with the children and provided better supervision (Leon et al., 2000). The family variables included in this study examined whether a similar process pertains to children residing at home.
Aspects of children’s psychiatric treatment may also influence the readmission risk. First, inpatient service use (length of stay and prior hospitalization) may influence the risk of rehospitalization (Appleby et al., 1993; Colenda and Hamer, 1989; Pavkov et al., 1997; Wickizer et al., 1999). Second, care-financing source (public versus private) may affect the threshold for rehospitalization (Dalton et al., 1997). Third, because inadequate stabilization during hospitalization may predispose to rapid return to inpatient care, this study examined the child’s condition at discharge and the magnitude of improvement from admission. In one study (Lyons et al., 1997), adults’ functioning at discharge did not predict readmission, although their condition at admission did, while another suggested that inpatient outcome might affect the latency to readmission, if not the overall readmission rate (Craig et al., 2000). Whether the clinical outcome of inpatient treatment predicts readmission among children requires investigation. Finally, postdischarge services may affect rehospitalization risk. Foster (1999) found that adolescents’ involvement in outpatient treatment reduced their risk of rehospitalization; however, patients with enhanced aftercare services did not have lower readmission rates.
This study prospectively assessed children’s rehospitalization at 3, 6, and 12 months after discharge from acute-care inpatient treatment to ascertain the frequency and timing of readmissions. It investigated the influences of selected symptom, family, and service factors to derive a parsimonious model of readmission risk that weights these factors appropriately.
METHOD
SETTING, PARTICIPANTS, AND RECRUITMENT
Participants were recruited from the guardians of children admitted to the 15-bed psychiatric inpatient service of a not-for-profit general pediatric hospital during a 14-month period. This facility draws from a highly demographically and socially diverse patient base. Consequently, children received their preadmission and postdischarge services (psychiatric, educational, and social) through a wide range of providers, jurisdictions, and agencies.
There were 192 children admitted during this period, and the families of 123 consented to participate in the follow-up study. Twenty others declined, 20 could not be contacted for recruitment mainly because of precipitous discharge, and 29 children were under the guardianship of foster care agencies that did not provide timely consent. The participant group therefore had a lower proportion of children in foster care (9%) relative to the entire group of admitted children (22%). In other respects (age, ethnicity, gender, and diagnoses), the participants and other children admitted during this period were comparable. Of those consenting, eight withdrew or were unreachable before the first follow-up assessment and six were transferred directly to another inpatient unit and are not included in this report.
At admission, research staff acquainted families or guardians with the follow-up study, provided a written description, and told them that they would be invited to participate when their child was discharged. At discharge, the study and the requirements of participation were fully described and any questions addressed. Caregivers who wished to participate then gave written informed consent and children over age 8 assented. The study was approved by the Institutional Review Board of the Long Island Jewish Medical Center.
FOLLOW-UP ASSESSMENTS OF REHOSPITALIZATION
The Services Utilization Survey, developed for this study, is a telephone interview that inquires about use of mental health and other services. It was administered to caregivers at 3, 6, and 12 months after discharge to obtain information on rehospitalization, including the dates of readmission and discharge.
PREDICTORS OF REHOSPITALIZATION
Symptom Variables
Diagnosis
Structured assessment at admission included (1) interviews with caregivers and children following a written outline with prompts that queried for DSM-IV symptoms for specific disorders; (2) telephone interviews and rating scales from teachers; and (3) review of prior psychiatric evaluation and treatment records. Admission diagnoses were determined in case conferences that included at least two child and adolescent psychiatrists, applying DSM-IV criteria.
Symptom Rating Scales
Three symptom-focused questionnaires for this study were completed at admission. The total behavior problem score from the parent-completed Child Behavior Checklist gauged the overall severity of symptoms (Achenbach, 1991). The New York Parent Rating Scale for Disruptive Behavior measured the severity of conduct problem symptoms. This scale was used in a treatment study of outpatients with conduct disorder (Klein et al., 1997), and its item content is nearly identical to a published version for teacher completion (Miller et al., 1995). The Children’s Depression Inventory (Kovacs, 1992) is a child self-report measure of mood symptoms; this study used the total depression score.
Family Measures
The Alabama Parenting Questionnaire (APQ) (Shelton et al., 1996) contains five subscales for Parental Involvement, Corporal Punishment, Poor Monitoring, Rewarding Positive Behavior, and Inconsistent Discipline. The Parenting Stress Index (Abidin, 1995) evaluated parents’ self-reported stress in caring for the hospitalized child. This study used the total score from the 36-item Short Form. The Control and Cohesion subscales of the Family Environment Scale (Moos and Moos, 1994) evaluated these two dimensions of family climate.
Treatment Factors
Treatment-related variables pertaining to the index hospitalization were length of stay, prior hospitalizations, and payer (public versus private/commercial). At the time of this study publicly funded mental health care in New York was largely unmanaged, while all private/commercial payers used ongoing care review and cost authorization practices. Clinicians provided Global Assessment of Functioning (GAF) ratings at admission and at discharge, and difference scores (discharge minus admission) quantified change in impairment as an outcome of hospitalization.
Parents provided information pertaining to postdischarge services via the follow-up interview described earlier. The interview inquired about outpatient treatment, day hospital involvement, home-based services, and residential care. Services were analyzed as time-dependent variables (i.e., counted as present between the dates of service commencement and discontinuation, if any).
STATISTICAL ANALYSIS
A Kaplan-Meier survival curve was generated for the likelihood of remaining out of inpatient care during the follow-up period as a function of time since discharge. Children with no reported rehospitalizations were censored from the distribution after their last completed follow-up interview. Doing so led to censoring of 11 children after 90 days and 14 after 180 days; the remaining children who had not been rehospitalized participated in the 12-month assessment and were therefore right-censored at 365 days. From these data, a survival estimate was computed to represent the 1-year probability of rehospitalization based on known readmissions and data available from censored observations.
Preliminary analyses of the distributions for continuous predictor variables showed that length of stay and depression had a significantly positive skew, which logarithmic transformation normalized. The corporal punishment score from the APQ had a positively skewed distribution and change in GAF had a negatively skewed distribution that score transformations did not alter; consequently these variables were dichotomized near their medians.
The influence of predictors on the hazard ratio for rehospitalization was evaluated using the Cox proportional hazards regression model. First, a baseline hazard function depicts the rates at which individuals first experience rehospitalization throughout the follow-up period. The Cox model then estimates regression weights for potential predictors to test whether they improve the fit of the hazard function to the observed data, in a manner analogous to multiple regression; hazard ratios derive from these coefficients and are analogous to odds ratios in logistic regression. Predictors whose hazard ratios had p values of .10 and under were selected for a multivariable analysis to derive a parsimonious model that weighted the predictors appropriately.
The validity of the basic Cox model assumption, proportionality of the hazard function over time, was examined in each analysis by the correlations between days since discharge and Schoenfeld residuals for each variable (Schoenfeld, 1982). When predictors were nonproportional over time (i.e., the correlation was significant), a second analysis that included a predictor-by-time interaction term produced the results reported.
RESULTS
Sample Characteristics
Table 1 shows the age, gender, ethnicity, caregivers, and diagnostic groupings for the 109 participants.
TABLE 1.
Demographic, Symptom, Family, and Service Predictors of Rehospitalizarion
| Variable | Univariate Analyses |
|||||
|---|---|---|---|---|---|---|
| Mean (SD) or n (%) | 1-yr Readmission Estimatea | Hazard Ratiob | 95% CI | χ2c | p | |
| Demographic | ||||||
| Age, yr | 9.50 (2.15) | 1.09 | 0.93–1.28 | 1.21 | .27 | |
| ≤7 | 35 (32) | 0.32 | (Reference category) | |||
| 8–10 | 38 (35) | 0.31 | 0.85 | 0.37–1.92 | 0.16 | .69 |
| ≥11 | 36 (33) | 0.42 | 1.40 | 0.66–3.00 | 0.76 | .38 |
| Gender | ||||||
| Male | 71 (65) | 0.37 | (Reference category) | |||
| Female | 38 (35) | 0.38 | 1.05 | 0.50–2.22 | 0.02 | .90 |
| Ethnicity | ||||||
| African American | 39 (36) | 0.46 | (Reference category) | |||
| Hispanic | 10 (9) | 0.30 | 0.59 | 0.17–2.03 | 0.69 | .41 |
| White | 56 (51) | 0.32 | 0.64 | 0.33–1.25 | 1.69 | .19 |
| Other | 4 (4) | 0.30 | 0.58 | 0.08–4.34 | 0.28 | .59 |
| Caregiver | ||||||
| Biological parents | 71 (65) | 0.37 | (Reference category) | |||
| Adoptive parents | 15 (14) | 0.49 | 1.46 | 0.63–3.39 | 0.79 | .37 |
| Grandparent | 10 (9) | 0.31 | 0.81 | 0.24–2.68 | 0.12 | .73 |
| Foster parent | 12 (11) | 0.26 | 0.65 | 0.20–2.16 | 0.49 | .48 |
| Diagnosis | ||||||
| Mood only | 9 (8) | 0.25 | (Reference category) | |||
| Disruptive only | 31 (28) | 0.52 | 4.18 | 1.21–14.44 | 5.11 | .02 |
| Mood + disruptive | 38 (35) | 0.43 | 3.14 | 0.67–7.89 | 3.30 | .07 |
| Anxiety + disruptive | 8 (7) | 0.27 | 1.81 | 0.22–7.94 | 0.42 | .52 |
| PDD + disruptive | 11 (10) | 0.18 | 1.16 | 0.19–6.19 | 0.87 | .87 |
| PDD only | 5 (5) | 0.00 | (Excluded) | |||
| Anxiety only | 3 (3) | 0.00 | (Excluded) | |||
| Psychotic | 4 (4) | 0.29 | (Excluded) | |||
| Symptom rating scales | ||||||
| Total beh. problem, T score (CBCL) | 74 (7.5) | 0.99d | 0.98–1.01 | 0.23 | .63 | |
| Low (<74) | 40 (37) | 0.30 | (Reference category) | |||
| Middle (74–76) | 31 (28) | 0.41 | 1.53 | 0.69–3.37 | 1.11 | .29 |
| High {>76) | 38 (35) | 0.40 | 1.45 | 0.65–3.23 | 0.82 | .37 |
| Conduct problems (NYPRS) | 56(18.7) | 1.02 | 1.003–1.04 | 5.34 | .02 | |
| Low (<48) | 40 (37) | 0.22 | (Reference category) | |||
| Middle (48–63) | 32 (29) | 0.45 | 2.43 | 1.08–5.80 | 3.99 | .04 |
| High (>63) | 37 (34) | 0.45 | 2.39 | 1.02–5.59 | 4.04 | .04 |
| Depression, T score (log) (CDI) | 54 (50) | 0.99 | 0.96–1.02 | 0.34 | .56 | |
| Low (<50) | 36 (33) | 0.45 | (Reference category) | |||
| Middle (50–60) | 34 (31) | 0.28 | 0.74 | 0.34–1.59 | 0.61 | .43 |
| High (>60) | 39 (36) | 0.24 | 0.59 | 0.27–1.26 | 1.85 | .17 |
| Family measures | ||||||
| Parental involvement (APQ) | 35 (8) | 0.96 | 0.92–0.99 | 4.83 | .03 | |
| Low (<33) | 42 (38) | 0.43 | (Reference category) | |||
| Middle (33–40) | 27 (25) | 0.34 | 0.53 | 0.24–1.20 | 2.33 | .13 |
| High (>40) | 40 (37) | 0.20 | 0.29 | 0.13–0.66 | 8.80 | .003 |
| Corporal punishment (APQ) | ||||||
| Low (<4) | 40 (36) | 0.22 | (Reference category) | |||
| High (≥4) | 69 (64) | 0.45 | 2.45 | 1.12–5.35 | 5.05 | .02 |
| Poor monitoring (APQ) | 15 (6) | 0.98d | 0.91–1.05 | 0.42 | .52 | |
| Low (< 12) | 45 (41) | 0.34 | (Reference category) | |||
| Middle (12–17) | 26 (24) | 0.36 | 1.08 | 0.47–2.50 | 0.03 | .85 |
| High (>17) | 38 (35) | 0.40 | 1.22 | 0.59–2.52 | 0.28 | .59 |
| Rewards positive behavior (APQ) | 25.3 (4) | 0.98 | 0.90–1.06 | 0.40 | .52 | |
| Low (<24) | 44 (40) | 0.42 | (Reference category) | |||
| Middle (24–28) | 28 (26) | 0.34 | .74 | 0.33–1.70 | 0.52 | .47 |
| High (>28) | 37 (34) | 0.33 | .74 | 0.35–1.54 | 0.66 | .42 |
| Inconsistent discipline (APQ) | 15.8 (4.3) | 1.00 | 0.92–1.07 | 0.02 | .89 | |
| Low (<14) | 44 (40) | 0.41 | (Reference category) | |||
| Middle (14–18) | 25 (23) | 0.34 | .80 | 0.34–1.85 | 0.28 | .60 |
| High (>18) | 40 (37) | 0.34 | .79 | 0.38–1.62 | 0.42 | .52 |
| Parenting stress (PSI) | 103 (24.7) | 0.99 | 0.96–0.99 | 2.57 | .10 | |
| Low (<91) | 41 (28) | 0.46 | (Reference category) | |||
| Middle (91–113) | 31 (38) | 0.35 | 0.68 | 0.31–1.47 | 0.96 | .33 |
| High (> 113) | 37 (34) | 0.28 | 0.53 | 0.25–1.25 | 2.55 | .11 |
| Family control (FES) | 5.3 (1.83) | 0.87 | 0.72–1.04 | 2.27 | .13 | |
| Low(≤5) | 58 (53) | 0.42 | (Reference category) | |||
| High (>5) | 51 (47) | 0.31 | 0.67 | 0.35–1.28 | 1.47 | .22 |
| Family cohesion (FES) | 5.9 (2.45) | 0.89 | 0.78–1.01 | 3.40 | .06 | |
| Low (≤7) | 51 (47) | 0.45 | (Reference category) | |||
| High (>7) | 58 (53) | 0.29 | 0.56 | 0.30–1.08 | 2.95 | .09 |
| Treatment factors | ||||||
| Length of stay (log) | 20.7 (22.3) | 1.18 | 0.80–1.75 | 0.69 | .41 | |
| ≤10 days | 39 (36) | 0.35 | (Reference category) | |||
| 11–20 days | 34 (31) | 0.38 | 1.15 | 0.53–2.53 | 0.13 | .72 |
| >20 days | 36 (33) | 0.37 | 1.11 | 0.51–2.39 | 0.07 | .80 |
| Prior hospitalization | ||||||
| No prior hospitalization | 85 (78) | 0.37 | (Reference category) | |||
| Prior hospitalization | 24 (22) | 0.35 | 0.94 | 0.43–2.05 | 0.03 | .87 |
| Change in GAF, d/c minus adm | ||||||
| ≤10 | 60 (55) | 0.32 | (Reference category) | |||
| >10 | 49 (45) | 0.42 | 1.42 | 0.75–2.70 | 1.19 | .27 |
| Payer source for care | ||||||
| Commercial | 54 (50) | 0.36 | (Reference category) | |||
| Public | 55 (50) | 0.37 | 0.51d | 0.19–1.34 | 1.87 | .17 |
| Outpatient child psychotherapy | ||||||
| Received between d/c & 2 mo | 80 (78) | 0.45 | (Reference category) | |||
| Received then discontinued | 8 (8) | 0.40 | 0.87d | 0.27–2.84 | 0.05 | .82 |
| Not received berween d/c & 3 mo | 15 (15) | 0.07 | 0.12d | 0.02–0.89 | 4.29 | .04 |
| Outpatient family psychotherapy | ||||||
| Received between d/c & 3 mo | 69 (68) | 0.46 | (Reference category) | |||
| Received then discontinued | 8 (8) | 0.38 | 0.76 | 0.23–2.51 | 0.20 | .66 |
| Not received between d/c & 3 mo | 24 (24) | 0.18 | 0.32 | 0.11–0.92 | 4.46 | .04 |
| Outpatient medication at 3 mo | ||||||
| No medication | 14 (13) | 0.24 | (Reference category) | |||
| 1 medication | 30 (28) | 0.29 | 1.28 | 0.34–4.83 | 0.13 | .71 |
| 2 medications | 37 (34) | 0.36 | 1.63 | 0.46–5.77 | 0.57 | .45 |
| >3 medications | 28 (25) | 0.47 | 2.34 | 0.67–8.23 | 1.77 | .18 |
| Day treatment program | ||||||
| Not received between d/c & 3 mo | 87 (80) | 0.38 | (Reference category) | |||
| Received berween d/c & 3 mo | 22 (20) | 0.38 | 1.00 | 0.46–2.20 | 0.0 | .99 |
| Home-based service | ||||||
| Not received between d/c & 3 mo | 80 (73) | 0.36 | (Reference category) | |||
| Not received between d/c & 3 mo | 29 (27) | 0.32 | 1.13 | 0.56–2.28 | 0.12 | .73 |
Note: CI = confidence interval; PDD = pervasive developmental disorder; CBCL = Child Behavior Checklist; NYPRS = New York Parent Rating Scale for Disruptive and Antisocial Behavior; CDI = Children’s Depression Inventory; APQ = Alabama Parenting Questionnaire; PSI = Parenting Stress Index; FES = Family Environment Scale; GAF = Global Assessment of Functioning; d/c = discharge; adm = admission.
From Kaplan-Meier survival function.
For continuous variables, hazard ratio is change in risk from baseline hazard function associated with each unit increase in the predictor. For categorical variables, it is change relative to the reference category.
df = 1 for all χ2 tests.
Test included predictor-by-time interaction term due to nonproportionality of predictor’s hazard function over time.
For this clinically heterogeneous sample, DSM-IV principal diagnoses at admission were categorized into five major diagnostic classes (mood, disruptive, anxiety, psychotic, and pervasive developmental disorder [PDD]). Participants were then grouped into the mutually exclusive single or comorbid principal diagnoses shown under “Diagnosis.” Disruptive disorders (i.e., oppositional defiant and conduct disorder) alone or combined with another disorder were the most prevalent diagnostic class.
Rehospitalization Rates
In the year after discharge, 37 of 109 participants reported rehospitalization; the Kaplan-Meier 1-year estimate of rehospitalization risk, taking into account both reported hospitalizations and censored obserations, was 0.37. The great majority of readmisions (81%) occurred in the first 3 months after discharge.
Predictors of Rehospitalization
Table 1 shows the univariate associations of demographic, diagnostic, symptomatic, family, and treatment-related predictors with readmission risk. One-year rehospitalization risk estimates, based on Kaplan-Meier survival functions, are shown for each level of categorical variables. For continuous measures, the table contains overall hazard ratios (per unit increase) on the line showing the mean and SD. The table also presents categorical hazard ratios and regression analyses, using tertiles of continuous measures or, when more appropriate for a variable’s distribution, groups above and below its median.
For diagnosis, readmission risk was compared among the mutually exclusive groups of subjects formed by principal diagnoses and the major comorbid combinations. The analysis excluded groups with five and fewer subjects since a reliable estimate of their hazard ratios was not obtainable. With “Mood only” as the reference category, the disruptive group’s hazard ratio was significant. A simplified model that combined the disruptive only and disruptive plus mood groups (total N = 69) to estimate risk relative to the other groups combined (n = 40) also yielded a significant hazard ratio (2.98), but with a much narrower confidence interval (1.31–6.72) than the disruptive only group, so this division was used in the multivariate analysis below.
Among symptom rating scales, conduct problem ratings had a significantly elevated hazard ratio. In categorical analysis, the middle and high subgroups showed similar increases in risk over the low subgroup.
Among family measures, parental involvement yielded a significantly lower hazard ratio. Children in the high-involvement subgroup were significantly less likely to be readmitted than those in the low-involvement subgroup. Although the hazard ratio for the middle subgroup relative to the low-involvement subgroup was also smaller, it was not statistically significant.
The hazard ratio for corporal punishment showed a nearly 2.5-fold increase in the high group relative to the low group. (The severity of parent-reported corporal punishment among study participants was generally not at the level for which reporting to authorities is indicated or mandated. Modifying disciplinary practices was emphasized in treatment, and progress was monitored by unit staff and conveyed to outpatient providers as appropriate.)
Higher parenting stress carried a reduced readmission risk. Further analyses exploring this result appear below.
Among the treatment factors, noninvolvement in outpatient individual child or family psychotherapy was associated with a lower readmission risk relative to those who had these treatments consistently in the first 3 months after discharge. Because children with PDD, who had a lower readmission rate, may be referred less often for psychotherapy, this analysis was repeated excluding those with PDD, and the same result was obtained.
Table 2 shows the hazard ratios for a combined variable model that included predictors with univariate hazard ratios with p of .10 and less. The overall model’s likelihood-ratio χ2 8 was 43.54, p < .0001. Hazard ratios for the four statistically significant variables in this combined model (p < .01; conduct problems, parental involvement, corporal punishment, and parenting stress) were re-estimated to yield the final model shown in Table 2 (likelihood ratio χ2 4 = 40.02, p < .0001).
TABLE 2.
Multivariate Model of Rehospitalization Risk
| Variable | Combined Model |
Final Model |
||||||
|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | χ2 | p | Hazard Ratio | 95% CI | χ2 | p | |
| Disruptive or disruptive+mood disorder diagnosisa | 1.48 | 0.59–3.74 | 0.70 | .40 | ||||
| Conduct problemsb | 1.03 | 1.01–1.06 | 6.55 | .01 | 1.04 | 1.02–1.06 | 14.15 | <.001 |
| Parental involvementb | 0.93 | 0.89–0.98 | 7.97 | <.005 | 0.92 | 0.88–0.97 | 12.46 | <.001 |
| Corporal punishmenta | 4.57 | 1.64–12.72 | 8.45 | <.005 | 5.61 | 2.09–15.07 | 11.70 | <.001 |
| Parenting stressb | 0.97 | 0.95–0.99 | 11.36 | .01 | 0.96 | 0.95–0.98 | 20.80 | <.001 |
| Family cohesionb | 0.91 | 0.77–1.08 | 1.16 | .28 | ||||
| Outpatient child psychotherapya | 4.35 | 0.57–33.21 | 2.01 | .16 | ||||
| Outpatient family psychotherapya | 2.07 | 0.72–5.93 | 1.81 | .18 | ||||
Note: CI = confidence interval.
Categorical variable.
Continuous variable.
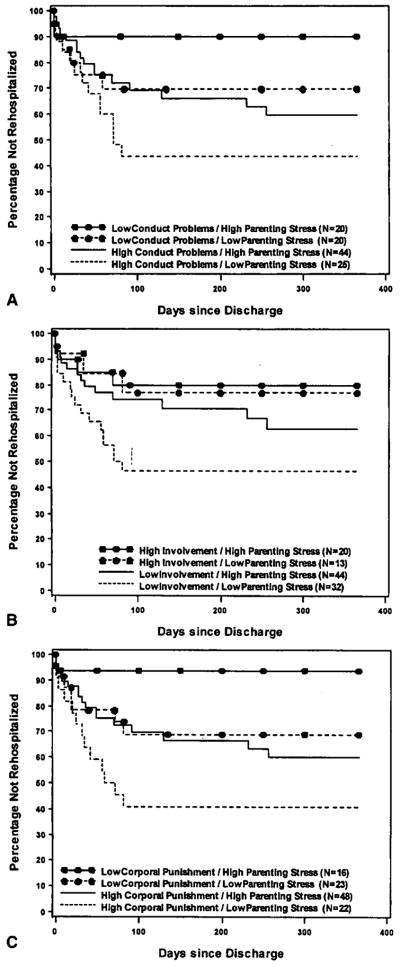
Parenting stress showed a marked increase in χ2 in the combined model over its univariate analysis. This suggested that understanding the association between higher parenting stress and reduced hospitalization risk should take into account the other variables for which the combined model adjusted. Figure 1 displays the joint influence on rehospitalization risk of parenting stress with conduct problems (top), with parental involvement (middle), and with corporal punishment (bottom). In each graph, the survival function closest to the x-axis (showing the highest rehospitalization risk) represents the group that combines low parenting stress with high values of the other risk factor. Put another way, high parenting stress attenuated somewhat the risks associated with conduct problems, parental underinvolvement, and corporal punishment. Further analyses supported this interpretation. For conduct problems, the hazard ratio for high parenting stress relative to low parenting stress was significantly smaller in the group with high conduct problems (0.39, 95% confidence interval 0.17–0.92, χ2 1 = 4.65, p < .03), but not in the group with low conduct problems (95% confidence interval 0.00 to >100). For parent involvement, the hazard ratio for high parenting stress relative to low parenting stress was significantly smaller in the low-involvement group (0.38, 95% confidence interval 0.16–0.93; χ2 1 = 4.47, p = .03), but not in the high-involvement group (0.56, 95% confidence interval 0.07–4.67). For corporal punishment, the hazard ratio for high parenting stress relative to low parenting stress was significantly smaller in the high corporal punishment group (0.48, 95% confidence interval 0.23–0.98, χ2 1 = 4.01, p < .05), but not in the low corporal punishment group (0.99, 95% confidence interval 0.96–1.03). Further analyses tested the inclusion in the model of interaction terms for parenting stress with the other variables, and all were nonsignificant.
Fig. 1.
Joint effects of parenting stress with conduct problems (A), with parental involvement (B), and with corporal punishment (C) on rehospitalization risk. The high parenting stress subgroup represented the highest tertile (Table 1). The lowest conduct problem tertile represented the low conduct problem subgroup. The highest parental involvement tertile represented the high involvement subgroup. All survival curves indicate the greatest hospitalization risk (viz., the lowest line in each graph) for the group which combines low parenting stress with the other risk factor (high conduct problems, low parental involvement, and high corporal punishment).
Rehospitalization Risk Index
Signal detection methods examined the utility of a simplified index of readmission risk. This index was the number of risk factors present for each child based on predictors in the final model (i.e., middle/high conduct problems, low parental involvement, high corporal punishment, low/middle parenting stress [Tables 1 and 2]) and therefore ranged from 0 to 4. Among those not censored before 1 year (N = 84), 80% of rehospitalized children had index scores of 3 or higher (sensitivity), a characteristic shared with 21% of the children who were not rehospitalized (i.e., specificity = 0.79). A score of 3 or higher carried a 75% risk of rehospitalization (positive predictive value), while 81% of those scoring 2 and lower were not rehospitalized (negative predictive value). All seven children with scores of 4 were rehospitalized. Total area under the curve was 0.83 (95% confidence interval 0.74–0.91).
Hospital Recommendations and Postdischarge Services
Cox regression for the service-related predictors in Table 1 did not support the hypothesis that less involvement with aftercare services would increase the rehospitalization risk. Nonetheless, further details of children’s care in relation to inpatient recommendations may aid in depicting the service context for our findings.
The large majority of children admitted (both participants and nonparticipants) had prior psychiatric care. All but six children (5.5%) received outpatient care at the time of their admission. At admission, 90.8% of the sample had pharmacological treatment.
Parents reported high rates of aftercare services for the study sample. Inpatient staff included outpatient psychotherapy in the discharge plans of 91.4% of the children. Table 1 shows the rates of individual and family therapies and of pharmacological treatment at the 3-month follow-up, covering the period with the highest readmission risk. For the two psychosocial treatments, the table distinguishes between those who had continuous therapy, those who had none, and those who discontinued. Children without outpatient individual or family psychosocial treatment were less likely to be rehospitalized, perhaps reflecting the calibration of aftercare to perceived risk. The same finding held for children who received neither. All the children not in outpatient psychotherapy, however, received pharmacotherapy.
Inpatient staff recommended pharmacotherapy for 99% of the sample. Parents reported medication treatment at any time between discharge and the 3-month assessment for 98% of the sample, while fewer (86%), received pharmacotherapy at the 3-month assessment point. Those who discontinued medication had a readmission rate (24%) nonsignificantly lower than those who did not (36%).
Inpatient staff referred 21% of the sample for day treatment and 20% for home-based services; at 3 months after discharge, these services were implemented for 65% and 55%, respectively, of those referred, reflecting their limited availability. A number of children who were not referred by inpatient staff to day treatment or home-based services obtained them after discharge nonetheless (7% and 15% respectively). The rehospitalization risk did not differ significantly between those referred for day treatment but not receiving it (50%) and those who were in day treatment (60%). Similarly, 33% of those referred for home-based services but not receiving them were rehospitalized, which does not differ significantly from the 45% readmission rate for those who did obtain home-based care.
Further Cox regressions for the influence of these services on readmission risk that adjusted for preadmission conduct problem ratings were not significant.
DISCUSSION
In a preadolescent group admitted to an acute-care psychiatric inpatient service, survival analysis indicated a 1-year rehospitalization risk estimate of 0.37. Readmissions clustered strongly in the first 3 months. Severity of conduct problems, low parental involvement, and corporal punishment made independent contributions to a heightened rehospitalization risk, but higher parenting stress appeared to attenuate these factors.
Point estimates of readmission risk do not generalize readily from one clinical site. Nonetheless, this study’s overall readmission rate is a bit higher but in line with prior estimates of readmission of young patient samples. The 34% rate of reported readmissions, though, exceeds that for several adult acute-care patient samples over a comparable follow-up interval (17%–22%) (Lyons et al., 1997; Swigar et al., 1991; Thomas et al., 1996) and at least one chronically ill adult sample (15%) (Sullivan et al., 1995), and is more typical of the one-third and higher rate reported among highly impaired, aggressive, or undermedicated adult patient samples (Appleby et al., 1993; Citrome et al., 1994; Craig et al., 2000; Hooley and Hoffman, 1999; Perlick et al., 1999; Rabinowitz et al., 2001; Schooler et al., 1997). The similarity on this outcome between child psychiatric acute-care inpatients and such markedly ill adult patients compels more detailed study of the treatment needs of hospitalized children.
Clustering of readmissions soon after discharge has been reported in other research with children and adolescents (Wickizer et al., 1999). If further research confirms this trend, interventions to reduce the rehospitalization period should focus on this period. The analysis of risk factors suggests which children and families might be most in need of such intervention.
The finding that the severity of conduct problems was a strong predictor of rehospitalization is consistent with data that aggressive behavior confers a heightened risk for hospitalization across a range of specific diagnoses (Citrome et al., 1994; Gutterman, 1998; Gutterman et al., 1993; Sourander et al., 1996). Aggressive children typically experience poor impulse control, affective instability, and numerous environmental and developmental adversities. Treatment for these difficulties is therefore often multifaceted, frequently yields an incomplete response, and may be difficult for families to implement or sustain effectively. Children with these problems are prone to extrusion from normal social arenas, including restrictive school placements and rejection by peers. Their higher vulnerability to serial hospital admissions may well be another aspect, albeit unintended, of this group’s social marginalization.
Effects on readmission risk emerged for harsh discipline and low positive involvement even after adjusting for the severity of conduct problems, a finding consistent with other data linking parenting practices and unfavorable child outcomes. Such parenting practices and other adverse family features mediate the influence of parental psychiatric disorders on their offspring’s development of psychiatric conditions and may exert an effect on children’s disturbances independent of parental diagnosis (Cadoret et al., 1995; Frick, 1998; Johnson et al., 2001). This study extends this line of evidence to suggest a link between parent–child relations and the intensity of service use.
Self-reported parenting stress seemed a likely candidate to increase a family’s need or acceptance of a child’s return to inpatient care. Instead it served mainly to attenuate the effects of the other risk factors. That is, given higher conduct problems, parental underinvolvement, or corporal punishment, higher parental stress at admission portended a better outcome than when they occurred in the context of low parent-reported stress. If self-reports of parenting stress reflect high emotional engagement, these results are consistent with findings that emotional involvement by family members, even if uncomfortable, yields better clinical outcomes for some disorders (Hooley and Hoffman, 1999). In a mixed child and adolescent group on military bases, lower parental subjective distress was associated with a greater risk for rehospitalization (Foster, 1999). Similarly, in pediatric research, children whose parents were less emotionally troubled by their asthma had a significantly higher risk for frequent asthma-related hospitalizations (Chen et al., 2003). Higher parenting stress may promote motivation to take steps that could improve clinical outcomes. In view of the observed associations with low involvement, corporal punishment, and conduct problems, one inference is that parents with antagonistic relations with their children who do not report distress or minimize it may be more guarded, less engaged in treatment, or appear to clinicians as less in need, or accepting, of support. Services to address these high-risk situations present a major clinical challenge.
Alternative interpretations for reduced readmission risk with higher parenting stress should also be noted. It is possible that a parent’s distress or guilt prevented a child’s readmission when further inpatient care could have been beneficial. Second, the parenting stress measure may also have been influenced by the admission itself: parents who experienced relief may have reported less overall parenting stress and developed a lower threshold to seek rehospitalization when problems flared after discharge. The measure of parenting stress, though, focuses on experiences and distress over an extended time frame, and therefore seems less susceptible to an abrupt shift in mood resulting from the child’s admission.
Failure to participate in recommended postdischarge care is a major factor in the rehospitalization of adult patients (e.g., Sullivan et al., 1995). In this sample, though, parental report of medication continuation was uniformly high. Participation in psychosocial treatment was also generally high, though more variable. Those not involved in psychotherapy had lower rates of rehospitalization. This may reflect an appropriate calibration of intensity of aftercare to perceived need, which in turn may correlate with readmission risk. Alternatively, increased surveillance and involvement by service providers may facilitate readmission. An important caveat about this study’s assessment of postdischarge services is that it focused on parents’ report of their receipt, and not other details of specific treatments, frequency, quality, and adherence (other than attendance or medication continuation). Because the reliability of parental reports for such detailed information about outpatient care is questionable (Horwitz et al., 2001), adequate examination of these features requires integration of several data sources. However, the accuracy of parental reports of inpatient care is quite good (e.g., Bean et al., 2000, 2003; Hoagwood et al., 2000; Stiffman et al., 2000), buttressing confidence in this study’s method of ascertaining rehospitalization.
Limitations
Because this study involved one inpatient setting, the extent of the findings’ applicability to other settings is uncertain. Other settings may yield different results because of variations in patients, treatment practices, threshold for admission, lengths of stay, payer mix, and postdischarge services available. However, the ability to include more detailed child, family, and service measures enabled a refined assessment of clinically relevant variables that proved important to the prediction of rehospitalization. This study’s findings may therefore contribute to further research on the influence of locality differences, because such research often needs to adjust statistically for patient-level variables to detect or interpret contextual effects on service use and outcomes.
Another impediment to generalization is the under-representation of children in foster care. We had approval from the appropriate state and local authorities, but problems coordinating with each foster care agency to obtain timely consents for each child caused the exclusion of many children in surrogate care. Although these youngsters represent a large proportion of high-intensity users of child psychiatric services, we lack information on whether outcomes and prognostic factors resemble or differ from those of similarly ill children residing with their parents. They are rarely considered in other cohort studies of this type. Given the prominence in this study of family factors for rehospitalization, further research with this most vulnerable patient group is warranted. Groundwork for this research will likely necessitate extensive prior outreach, partnership, and protocol review with the numerous foster care agencies serving the study site(s).
Generalization to longer postdischarge periods is also uncertain. Although the first trimester had the highest rehospitalization risk for the year after discharge, longer follow-up might reveal that risk rises again.
Clinical Implications
Findings suggest that information readily obtainable at admission may provide a useful index of readmission risk for children. This knowledge in turn can enable clinicians to address the identified risk factors more completely during hospitalization and to develop after-care recommendations that alleviate them.
Specifically, it seems important to strive toward a low likelihood of exacerbation in aggressive conduct problems upon discharge. Because it is unclear whether children’s functioning during short inpatient stays provides a sound basis to predict postdischarge outcomes (e.g., Blader et al., 1994), time spent out of the hospital before actual discharge can enable a more ecologically valid assessment. However, payer constraints now disfavor this practice in many locations.
Caregiver–child interactions are the major focus of psychosocial treatment for child conduct difficulties, and this study indicates their centrality to the rehospitalization risk of young inpatients. Inpatient services can leverage several assets to help caregivers increase positive involvement and appropriate discipline strategies, such as opportunities for extensive observation, modeling, and guidance from staff. Doing so effectively, though, requires sustained personnel effort and capabilities that current staffing patterns may not accommodate. In addition, common caregiver obstacles to such intensive participation in treatment include lack of transportation, child care, and relief from other demands. In this context, home-based aftercare services (e.g., Henggeler et al., 1999) may fill a critical need for this patient group; however, their availability is uneven and the effectiveness of the various formats in use requires further examination. Children at the highest risk for rehospitalization had caregivers who reported low parenting stress in tandem with other risk factors. If replicated, this finding raises questions about whether these caregivers would be as accepting of family-focused interventions as parents who disclose more stress, and whether these different groups of parents might respond differently to such services.
Examination of symptom and family ratings at admission shows it is possible to gauge the risk for rehospitalization early in a patient’s stay, but it limits conclusions about how these factors affect readmission. For instance, it is not certain that conduct problems and parenting factors are themselves proximal contributors to readmission, since they may have changed in the postdischarge period. Unmeasured correlates of their admission values may directly influence readmission even if the measured variables change. The mechanisms by which the factors identified in this study relate to readmission and other clinical outcomes merit further investigation.
Footnotes
Disclosure: The author currently receives research support from Abbott Laboratories, and consulting compensation from Otsuka America Pharmaceutical, Inc.
References
- Abidin RR. Parenting Stress Index. 3. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- Achenbach TM. Integrative Guide for the 1991 CBCL/4–18, YSR and TRF Profiles. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Quarterly Health and Society. 1973;51:95–124. [PubMed] [Google Scholar]
- Appleby L, Desai PN, Luchins DJ, Gibbons RD, Hedeker DR. Length of stay and recidivism in schizophrenia: a study of public psychiatric hospital patients. Am J Psychiatry. 1993;150:72–76. doi: 10.1176/ajp.150.1.72. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Goldstein MJ, Carlson GA, Perdue S, Bates S, Keller J. Childhood-onset depressive disorders: a follow-up study of rates of rehospitalization and out-of-home placement among child psychiatric inpatients. J Affect Disord. 1988;15:245–253. doi: 10.1016/0165-0327(88)90022-5. [DOI] [PubMed] [Google Scholar]
- Bean D, Rotheram-Borus M, Leibowitz A, Horwicz S, Weidmer B. Spanish-language services assessment for children and adolescents (SACA): reliability of parent and adolescent reports. J Am Acad Child Adolesc Psychiatry. 2003;42:241–248. doi: 10.1097/00004583-200302000-00019. [DOI] [PubMed] [Google Scholar]
- Bean DL, Leibowitz A, Rotheram-Borus MJ, et al. False-negative reporting and mental health services utilization: parents’ reports about child and adolescent services. Ment Health Serv Res. 2000;2:239–249. [Google Scholar]
- Blader JC, Abikoff H, Foley C, Koplewicz HS. Children’s behavioral adaptation early in psychiatric hospitalization. J Child Psychol Psychiatry. 1994;35:709–721. doi: 10.1111/j.1469-7610.1994.tb01216.x. [DOI] [PubMed] [Google Scholar]
- Cadoret RJ, Yates WR, Troughton E, Woodworth G, Stewart MA. Genetic-environmental interaction in the genesis of aggressivity and conduct disorders. Arch Gen Psychiatry. 1995;52:916–924. doi: 10.1001/archpsyc.1995.03950230030006. [DOI] [PubMed] [Google Scholar]
- Chen E, Bloomberg G, Fisher E, Strunk R. Predictors of repeat hospitalizations in children with asthma: the role of psychosocial and socioenvironmental factors. Health Psychol. 2003;22:12–18. doi: 10.1037//0278-6133.22.1.12. [DOI] [PubMed] [Google Scholar]
- Citrome L, Green L, Fost R. Length of stay and recidivism on a psychiatric intensive care unit. Hosp Comm Psychiatry. 1994;45:74–76. doi: 10.1176/ps.45.1.74. [DOI] [PubMed] [Google Scholar]
- Colenda CC, Hamer RM. First admission young adult patients to a state hospital: relative risk for rapid readmission. Psychiatr Q. 1989;60:227–236. doi: 10.1007/BF01064798. [DOI] [PubMed] [Google Scholar]
- Craig TJ, Fennig S, Tanenberg-Karant M, Bromet EJ. Rapid versus delayed readmission in first-admission psychosis: quality indicators for managed care? Ann Clin Psychiatry. 2000;12:233–238. doi: 10.1023/a:1009038627449. [DOI] [PubMed] [Google Scholar]
- Dalton R, Moseley T, McDermott B. Psychiatric findings among child psychiatric inpatients grouped by public and private payment. Psychiatr Serv. 1997;48:689–693. doi: 10.1176/ps.48.5.689. [DOI] [PubMed] [Google Scholar]
- Davis DM, Gonzalez V, Piat J. Follow-up of adolescent psychiatric inpatients. South Med J. 1980;73:1215–1217. doi: 10.1097/00007611-198009000-00013. [DOI] [PubMed] [Google Scholar]
- Foster EM. Do aftercare services reduce inpatient psychiatric readmissions? Health Serv Res. 1999;34:715–736. [PMC free article] [PubMed] [Google Scholar]
- Frick PJ. Conduct Disorders and Severe Antisocial Behavior. New York: Plenum; 1998. [Google Scholar]
- Gutterman EM. Is diagnosis relevant in the hospitalization of potentially dangerous children and adolescents? J Am Acad Child Adolesc Psychiatry. 1998;37:1030–1037. doi: 10.1097/00004583-199810000-00012. [DOI] [PubMed] [Google Scholar]
- Gutterman EM, Markowitz JS, LoConte JS, Beier J. Determinants for hospitalization from an emergency mental health service. J Am Acad Child Adolesc Psychiatry. 1993;32:114–122. doi: 10.1097/00004583-199301000-00017. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Rowland MD, Randall J, et al. Home-based multisystemic therapy as an alternative to the hospitalization of youths in psychiatric crisis: clinical outcomes. J Am Acad Child Adolesc Psychiatry. 1999;38:1331–1339. doi: 10.1097/00004583-199911000-00006. [DOI] [PubMed] [Google Scholar]
- Hoagwood K, Horwitz SM, Stiffman A, et al. Concordance between parent reports of children’s mental health services and service records: the Services Assessment for Children and Adolescents (SACA) J Child Fam Stud. 2000;9:315–331. [Google Scholar]
- Hooley JM, Hoffman PD. Expressed emotion and clinical outcome in borderline personality disorder. Am J Psychiatry. 1999;156:1557–1562. doi: 10.1176/ajp.156.10.1557. [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Hoagwood K, Stiffman AR, et al. Reliability of the Services Assessment for Children and Adolescents. Psychiatr Serv. 2001;52:1088–1094. doi: 10.1176/appi.ps.52.8.1088. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Arch Gen Psychiatry. 2001;58:453–460. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- Klein RG, Abikoff HK, Jass E, Ganeles D, Seese LM, Pollack S. Clinical efficacy of methylphenidate in conduct disorder with and without attention deficit hyperactivity disorder. Arch Gen Psychiatry. 1997;54:1073–1080. doi: 10.1001/archpsyc.1997.01830240023003. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory Manual. Tonowanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Leon SC, Lyons JS, Uziel-Miller ND, Rawal P, Tracy P, Williams J. Evaluating the use of psychiatric hospitalization by residential treatment centers. J Am Acad Child Adolesc Psychiatry. 2000;39:1496–1501. doi: 10.1097/00004583-200012000-00009. [DOI] [PubMed] [Google Scholar]
- Lyons JS, O’Mahoney MT, Miller SI, Neme J, Kabat J, Miller F. Predicting readmission to the psychiatric hospital in a managed care environment: implications for quality indicators. Am J Psychiatry. 1997;154:337–340. doi: 10.1176/ajp.154.3.337. [DOI] [PubMed] [Google Scholar]
- Miller LS, Klein RG, Piacentini J, et al. The New York Teacher Rating Scale for Disruptive and Antisocial Behavior. J Am Acad Child Adolesc Psychiatry. 1995;34:359–370. doi: 10.1097/00004583-199503000-00022. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale Manual. 3. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- Parham C, Reid S, Hamer RM. A long-range follow-up study of former inpatients at a children’s psychiatric hospital. Child Psychiatry Hum Dev. 1987;17:199–209. doi: 10.1007/BF00706230. [DOI] [PubMed] [Google Scholar]
- Pavkov TW, Goerge RM, Lee BJ. State hospital reentry among youth with serious emotional disturbance: a longitudinal analysis. J Child Fam Stud. 1997;6:373–383. [Google Scholar]
- Perlick DA, Rosenheck RA, Clarkin JF, Sirey J, Raue P. Symptoms predicting inpatient service use among patients with bipolar affective disorder. Psychiatr Serv. 1999;50:806–812. doi: 10.1176/ps.50.6.806. [DOI] [PubMed] [Google Scholar]
- Pfeffer CR, Peskin JR, Siefker CA. Suicidal children grow up: psychiatric treatment during follow-up period. J Am Acad Child Adolesc Psychiatry. 1992;31:679–685. doi: 10.1097/00004583-199207000-00015. [DOI] [PubMed] [Google Scholar]
- Pottick KJ, McAlpine DD, Andelman RB. Changing patterns of psychiatric inpatient care for children and adolescents in general hospitals, 1988–1995. Am J Psychiatry. 2000;157:1267–1273. doi: 10.1176/appi.ajp.157.8.1267. [DOI] [PubMed] [Google Scholar]
- Rabinowitz J, Lichtenberg P, Kaplan Z, Mordechai M, Nahon D, Davidson M. Rehospitalization rates of chronically ill schizophrenic patients discharged on a regimen of risperidone, olanzapine, or conventional antipsychotics. Am J Psychiatry. 2001;158:266–269. doi: 10.1176/appi.ajp.158.2.266. [DOI] [PubMed] [Google Scholar]
- Ringel JS, Sturm R. National estimates of mental health utilization and expenditures for children in 1998. J Behav Health Serv Res. 2001;28:319–333. doi: 10.1007/BF02287247. [DOI] [PubMed] [Google Scholar]
- Romansky J, Lyons J, Lehner R, West C. Factors related to psychiatric hospital readmission among children and adolescents in state custody. Psychiatr Serv. 2003;54:356–362. doi: 10.1176/appi.ps.54.3.356. [DOI] [PubMed] [Google Scholar]
- Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–241. [Google Scholar]
- Schooler NR, Keith SJ, Severe JB, et al. Relapse and rehospitalization during maintenance treatment of schizophrenia: the effects of dose reduction and family treatment. Arch Gen Psychiatry. 1997;54:453–463. doi: 10.1001/archpsyc.1997.01830170079011. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. J Clin Child Psychol. 1996;25:317–329. [Google Scholar]
- Solomon P, Evans D, Delaney MA. Community service utilization by youths hospitalized in a state psychiatric facility. Community Ment Health J. 1993;29:333–346. doi: 10.1007/BF00761031. [DOI] [PubMed] [Google Scholar]
- Sourander A, Leijala H, Lehtilae A, Kanerva A, Helenius H, Piha J. Short-term child psychiatric inpatient treatment. Place of residence as one-year outcome measure. Eur Child Adolesc Psychiatry. 1996;5:38–43. doi: 10.1007/BF00708213. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Horwitz SM, Hoagwood K, et al. The Service Assessment for Children and Adolescents (SACA): adult and child reports. J Am Acad Child Adolesc Psychiatry. 2000;39:1032–1039. doi: 10.1097/00004583-200008000-00019. [DOI] [PubMed] [Google Scholar]
- Sullivan G, Wells KB, Morgenstern H, Leake B. Identifying modifiable risk factors for rehospitalization: a case-control study of seriously mentally ill persons in Mississippi. Am J Psychiatry. 1995;152:1749–1756. doi: 10.1176/ajp.152.12.1749. [DOI] [PubMed] [Google Scholar]
- Swigar ME, Astrachan B, Levine MA, Mayfield V, Radovich C. Single and repeated admissions to a mental health center: demographic, clinical and use of service characteristics. Int J Soc Psychiatry. 1991;37:259–266. doi: 10.1177/002076409103700405. [DOI] [PubMed] [Google Scholar]
- Thomas MR, Rosenberg SA, Giese AA, Fryer GE. Shortening length of stay without increasing recidivism on a university-affiliated inpatient unit. Psychiatr Serv. 1996;47:996–998. doi: 10.1176/ps.47.9.996. [DOI] [PubMed] [Google Scholar]
- Wickizer TM, Lessler D, Boyd-Wickizer J. Effects of health care cost-containment programs on patterns of care and readmissions among children and adolescents. Am J Public Health. 1999;89:1353–1358. doi: 10.2105/ajph.89.9.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]