Abstract
Background
Mutations of the transcription factor Nkx2-5 cause pleiotropic heart defects with incomplete penetrance. This variability suggests that additional factors can affect or prevent the mutant phenotype. We assess here the role of genetic modifiers and their interactions.
Methods and Results
Heterozygous Nkx2-5 knockout mice in the inbred strain background C57Bl/6 frequently have atrial and ventricular septal defects (ASD, VSD). The incidences are substantially reduced in the Nkx2-5+/− progeny of first generation (F1) outcrosses to the strains FVB/N or A/J. Defects recur in the second generation (F2) of the F1 × F1 intercross or backcrosses to the parental strains. Analysis of >3000 Nkx2-5+/− hearts from five F2 crosses demonstrates the profound influence of genetic modifiers on disease presentation. Based upon their incidences and co-incidences, anatomically distinct malformations have shared and unique modifiers. All three strains carry susceptibility alleles at different loci for ASD and VSD. Relative to the other two strains, A/J carries polymorphisms that confer greater susceptibility to ASD and atrioventricular septal defects, and C57Bl/6 to muscular VSD. Segregation analyses reveal that two or more loci influence membranous VSD susceptibility, whereas three or more loci and at least one epistatic interaction affect muscular VSD and ASD.
Conclusion
Alleles of modifier genes can either buffer perturbations on cardiac development or direct the manifestation of a defect. In a genetically heterogeneous population the predominant effect of modifier genes is health.
Keywords: Congenital Heart Defect, Genetic Variation, Genetics
Introduction
Significant progress has been made toward defining genetic etiologies in congenital heart disease.1, 2 Current knowledge of the few dozen genes implicated in cardiac development does not explain, however, the basis of common epidemiologic and clinical observations. The incidence of heart defects in newborns is 0.5-1%, making it a leading cause of death in children. Still, the vast majority is born with a normal heart. Selection against fetuses that have cardiac defects does not cause the prevalence of the norm.3, 4 Insults on the embryonic heart may be rare or weak, or mechanisms may have evolved to ensure the robustness of development. Direct evidence for either hypothesis is minimal, but the latter can better explain the breadth of observations related to incomplete penetrance and phenotypic variability.5, 6
Although family studies led to the discovery of mutations of prototypical cardiac developmental genes such as TBX5, NKX2-5, and GATA4 7-10, most cases of congenital heart disease have no identified cause or association. Such sporadic cases may be due to an unknown teratogen, spontaneous mutation or inconsistent expression of an inherited etiology. The last possibility is supported by the increased incidence of congenital heart disease in subsequent first-degree relatives, 2-11%, compared to the general population.11-13 Some normal relatives of sporadic patients must somehow escape the manifestation of a genetic mutation. Furthermore, among the affected relatives the cardiac phenotypes are usually dissimilar and of wide-ranging severity.11, 13 Modifying factors likely influence the incomplete penetrance and phenotypic variability associated with the expression of a causative mutation. In a family, the activity of modifiers in pathways involved in the development of an affected cardiac structure could determine whether a particular relative develops a heart defect, its type and severity. The unknown factors could be genetic, environmental or entirely stochastic. Of these, genetic modifiers are most amenable to investigation in a laboratory where environmental factors can be controlled between experimental groups.
Small studies have demonstrated the effect of the background strain on cardiac phenotypes related to embryonic viability and myocardial, valvar, or ventricular septal morphology in Tbx5, Gata4 and Hey2 mutations.14-16 The extent to which genetic modifiers contribute to incomplete penetrance and phenotypic variability as observed in humans might only be appreciated, however, in a much larger study. In this regard, the diverse anatomic phenotypes described in association with NKX2-5 mutation offer a foothold into the genetic modifiers that influence the susceptibility of developmental pathways. NKX2-5 mutations were first reported in families with highly penetrant ASDs and atrioventricular block, but not every member of these and subsequent families who carried a mutation had an ASD or even a cardiac malformation. Among affected persons the various defects seem neither related to each other by any known developmental pathway nor correlated with NKX2-5 genotype.9, 17, 18 Thus, while mutations of NKX2-5 or other cardiac transcription factors like TBX5 and GATA4 undoubtedly cause heart defects, modifying factors could have effects on phenotype as great as the causative mutation.
As the first step toward the elucidation of these factors, we examined the effect of genetic background variation on the incidence of specific heart defects in heterozygous Nkx2-5 knockout animals in the inbred mouse strain C57Bl/6 and in crosses to the strains FVB/N and A/J. The survey of thousands of Nkx2-5+/− animals reveals the important role that genetic modifiers play in buffering cardiac developmental pathways against a major perturbation in a population while directing the manifestation of disease in a few. The results intertwine the genetic basis of health and congenital heart disease, providing a conceptual framework to understand common clinical observations.
Methods
Mouse strains and crosses
Nkx2-5+/− animals were backcrossed to C57Bl/6 for 10-13 generations. The knockout allele was generated and genotyped as described.19 Nkx2-5+/− C57Bl/6 males were crossed to FVB/N or A/J females to generate F1 progeny. C57Bl/6 and FVB/N animals were obtained from Charles River Laboratories, and A/J from the Jackson Laboratory. Nkx2-5+/− F1 animals were intercrossed or backcrossed to the parental strains C57Bl/6 or FVB/N to generate F2 progeny. The backcross to A/J was not performed. Animals were housed under standard conditions in the same room and fed the same chow. The experiments were approved by the animal studies committee at Washington University School of Medicine.
Diagnosis of congenital heart defects
Neonatal pups were collected each morning within hours of birth to prevent cannibalization of animals that have serious congenital heart defects. The pups were euthanized. The thorax was fixed in 10% neutral buffered formalin overnight and then transferred to 70% ethanol. Fixed hearts were dissected, embedded in paraffin, and entirely sectioned in the frontal plane at 6 μm thickness. Each heart was inspected under a 5× microscope objective by at least two individuals. Defects were diagnosed by the appearance of the septae, valves, or blood in consecutive sections. Genomic DNA was isolated from every animal by phenol-chloroform extraction.
Statistical analyses
To compare the genotypic distribution in a particular strain or cross to the expected Mendelian ratio, all the pups from consecutive litters were counted up to at least 100 animals. Statistically significant deviation was defined in a χ2-test by P < 0.05.
The incidence of specific types of heart defects in crosses were compared by a two-tailed Fisher’s exact test. The co-incidence of heart defects in the same mouse was evaluated by comparison to the expected incidence, as determined by the product of their separate incidences, using a χ2-test.
Correlation of muscular and membranous VSD incidence with the average number of C57Bl/6 alleles per locus as expected from the Mendelian distribution in the F2 crosses was evaluated by Pearson’s product-moment correlation followed by a two-tailed t-test with significance defined by P < 0.05.
Segregation models were analysed by comparison of their predictions and observed incidences by a χ2-test. The models and derivation of equations are detailed in the Supplemental Materials.
Results
Newborn Nkx2-5+/− animals in the C57Bl/6 background have a high incidence of ASD and VSD
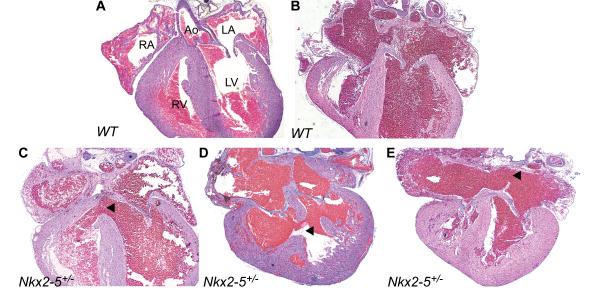
Human NKX2-5 mutations cause congenital heart defects, some of which are lethal if untreated in the newborn period. While such serious defects in Nkx2-5+/− mice have not been described, we observed that ~17% of Nkx2-5+/− pups in the C57Bl/6 background were missing at 2-3 weeks of age when they were weaned from their mothers. The attrition of Nkx2-5+/− animals occurs after birth because newborn pups were obtained at the expected Mendelian ratio (Table 1). We therefore examined newborn hearts that were collected within hours of birth. A high incidence of ASD of the secundum type was found in Nkx2-5+/− but not wild-type hearts (Figures 1, 2). A secundum ASD was diagnosed by an insufficiency in covering the fossa ovale due to a deficiency in its rim or of the septum primum. Hearts in which a potentially small ASD could not be distinguished from a patent foramen ovale were considered normal. The ASD incidence is greater than the ~20% previously reported by two different groups for adult Nkx2-5+/− animals in the C57Bl/6 background possibly because of spontaneous closure or postnatal death.20-22 VSDs of the membranous and muscular types were also found in Nkx2-5+/− but not wild-type hearts (Figures 1, 2). VSDs were not previously reported in adult animals possibly because of spontaneous closure or death from pulmonary overcirculation in the newborn period, as seen in mouse mutants that have a persistent patent ductus arteriosus.23
Table 1.
The observed and expected distributions of Nkx2-5+/− and wild-type pups in various crosses either at birth or weaning.
| Background | Nkx2-5 Genotype |
Age | N | Nkx2-5+/− | Wildtype | P | ||
|---|---|---|---|---|---|---|---|---|
| Observed | Expected | Observed | Expected | |||||
| C57Bl/6 | HET X HET | P21 | 505 | 62.5 | 66.7 | 37.4 | 33.3 | <0.05 |
| C57Bl/6 | HET X WT | P21 | 854 | 45.3 | 50 | 54.7 | 50 | <0.01 |
| C57Bl/6 | HET X WT | P0 | 100 | 56 | 50 | 44 | 50 | NS |
|
C57Bl/6 X FVB/N
F1 |
HET X WT | P21 | 214 | 46.7 | 50 | 53.3 | 50 | NS |
|
C57Bl/6 X A/J
F1 |
HET X WT | P21 | 156 | 51.9 | 50 | 48.1 | 50 | NS |
|
C57Bl/6 X FVB/N
F2 |
HET X HET | P0 | 212 | 66.5 | 66.7 | 33.5 | 33.3 | NS |
|
C57Bl/6 X A/J
F2 |
HET X HET | P0 | 562 | 64.4 | 66.7 | 35.6 | 33.3 | NS |
Pups were collected within hours of birth (P0) or at weaning (P21).
N, number of pups. NS, not significant.
Figure 1.
Atrial and ventricular septal defects in newborn Nkx2-5+/− animals. An intact ventricular septum (A) and a normal atrial septum with a patent foramen ovale (B) in wild-type hearts. (C) Membranous VSD and (D) muscular VSD in Nkx2-5+/− hearts. (E) Secundum ASD in an Nkx2-5+/− heart. Arrowheads point to the relevant defect in each section. Ao, Aorta. RA, LA, right, left atrium. RV, LV, right, left ventricle.
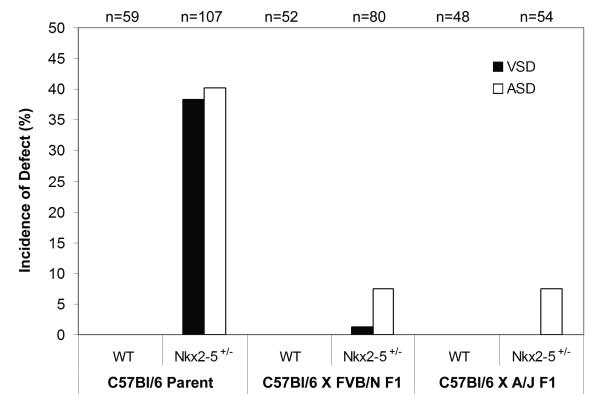
Figure 2.
The incidence of septal defects in wild-type and Nkx2-5+/− animals in the C57Bl/6 background and in F1 crosses to FVB/N and A/J. The incidence of ASD and VSD in Nkx2-5+/− hearts is substantially reduced in the F1 hybrids compared to the C57Bl/6 parental strain (P < 0.001).
Previous investigators have detected aortic stenosis by Doppler echocardiography in live animals and bicuspid aortic valves by gross examination of adult Nkx2-5+/− animals.21 Given that we examined histologic sections, minor valvular abnormalities that might cause regurgitation or stenosis are difficult to assess. Abnormal blood flow patterns have also been described by fetal echocardiography in association with severe lesions like truncus arteriosus.24 Severe defects and ones not easily detected by echocardiography like small VSDs because of physiologically elevated right-sided pressures in the fetus and newborn are easily recognized because of the greater spatial resolution of microscopy.
Nkx2-5+/− animals in hybrid strain backgrounds generally have normal cardiac anatomy
Nkx2-5+/− animals in the C57Bl/6 background were outcrossed to the FVB/N strain. The F1 progeny, which are C57Bl/6 X FVB/N hybrids, showed the expected Mendelian ratio of Nkx2-5+/− pups at weaning (Table 1). The absence of neonatal lethal defects was confirmed by direct inspection. Only one small VSD and 6 ASDs were found among 80 Nkx2-5+/− F1 newborn mouse hearts. All 52 wild-type hearts were normal. The incidence of either septal defect in the Nkx2-5+/− C57Bl/6 X FVB/N F1 hybrids is significantly lower compared to the C57Bl/6 background (Figure 2).
Nkx2-5+/− animals from the C57Bl/6 X A/J F1 hybrid cross similarly showed the expected Mendelian distribution of genotypes at weaning (Table 1). Direct inspection confirmed a reduced incidence of heart defects compared to the C57Bl/6 background, none of which was expected to be lethal. No VSDs and only 4 ASDs were found among 54 C57Bl/6 X A/J F1 Nkx2-5+/− newborn hearts. All 48 wild-type hearts were normal (Figure 2).
The C57Bl/6 X FVB/N F2 crosses reveal ASD and VSD susceptibility alleles in both strains
The C57Bl/6 X FVB/N F1 hybrid data suggest that C57Bl/6 carries one or more recessive alleles of modifier genes that increase susceptibility to heart defects in the presence of Nkx2-5 mutation. The data do not exclude the possibility of recessive susceptibility alleles from FVB/N at other loci. To investigate these possibilities, Nkx2-5+/− F1 animals were backcrossed to C57Bl/6 and FVB/N or intercrossed to generate F2 progeny. Newborn F2 pups showed the expected Mendelian distribution of genotypes, which indicates the absence of selection against defects that could cause prenatal demise (Table 1).
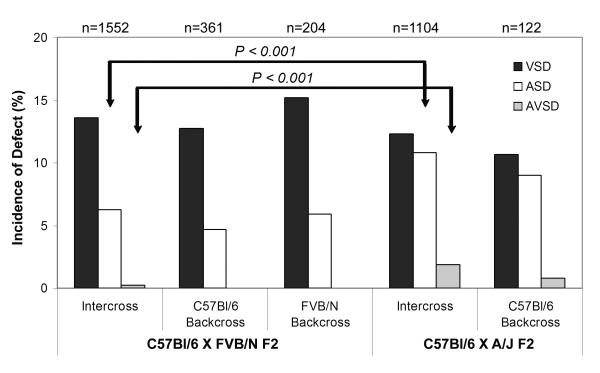
VSD and ASD were more common in the Nkx2-5+/− animals from each of the C57Bl/6 X FVB/N F2 crosses than from the F1 but less common than in C57Bl/6 (P < 0.001 for comparisons to both the F1 and C57Bl/6). A VSD was present in 12-16% of the Nkx2-5+/− F2 hearts, and an ASD in 4-7% (Figure 3). These results indicate that at least two loci affect VSD and ASD susceptibility in the presence of Nkx2-5 mutation. C57Bl/6 and FVB/N carry recessive, susceptibility alleles at different loci, given the increased incidence in the parental backcrosses compared to the F1. The Nkx2-5+/− F2 may have a lower incidence of particular defects compared to C57Bl/6 either because FVB/N susceptibility genotypes have smaller effects or because interactions between C57Bl/6 and FVB/N alleles reduce risk.
Figure 3.
The incidence of specific heart defects in Nkx2-5+/− animals from F2 intercrosses and parental backcrosses of C57Bl/6 and FVB/N or A/J. Cross-specific differences in the incidence of ASD and AVSD are significant between the C57Bl/6 X FVB/N and C57Bl/6 X A/J F2 intercrosses. The incidence of VSD is comparable between the C57Bl/6 X FVB/N and X A/J F2 crosses.
The C57Bl/6 X A/J F2 crosses reveal A/J susceptibility alleles for ASD and atrioventricular septal defects
Similar to the C57Bl/6 X FVB/N F2 results, the Nkx2-5+/− F2 progeny from the C57Bl/6 X A/J intercross and C57Bl/6 backcross showed an incidence of VSD and ASD greater than the F1 and less than C57Bl/6 (P < 0.001 for each of the comparisons; Figure 3). The backcross to A/J was not performed. Comparing the C57Bl/6 X A/J to the C57Bl/6 X FVB/N F2 crosses revealed two significant differences.
First, ASDs occurred at a higher frequency in the C57Bl/6 X A/J F2 intercross than in the C57Bl/6 X FVB/N (P < 0.001). There was a similar trend between the F2 backcrosses to C57Bl/6, which was not significant possibly because of the smaller sample sizes (P < 0.1). A/J may carry polymorphisms that confer greater susceptibility specifically to ASDs in the presence of Nkx2-5 mutation. The A/J polymorphisms do not increase susceptibility to septal defects in general because the VSD incidence was not different between the two intercrosses.
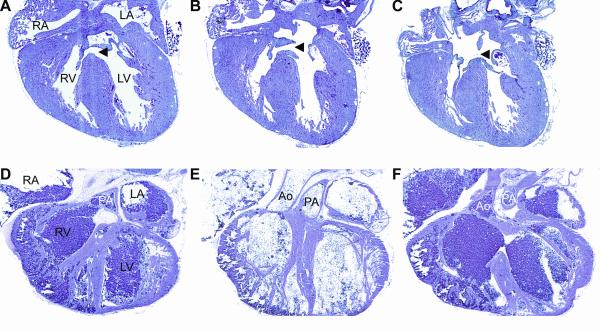
Second, atrioventricular septal defects (AVSD) occur at a low but significant incidence in the Nkx2-5+/− C57Bl/6 X A/J F2 intercross (Figures 3 and 4). Nkx2-5 mutation causes the defect because none of 238 wild-type littermates from the same cross had an AVSD (P < 0.05). An A/J polymorphism enhances susceptibility because the defect is much rarer in the C57Bl/6 X FVB/N F2 intercross (P < 0.001). The A/J polymorphism appears dominant with low penetrance because one AVSD was found among 121 Nkx2-5+/− hearts from the backcross to C57BL/6.
Figure 4.
Rarer heart defects are found in Nkx2-5+/− F2 progeny. Sections through an Nkx2-5+/− heart from the C57Bl/6 X A/J F2 intercross demonstrate an atrioventricular septal defect with its VSD (A), common valve (B) and primum ASD (C) marked by arrowheads in each section. Sections through an Nkx2-5+/− heart from the C57Bl/6 X FVB/N F2 intercross demonstrate double outlet right ventricle with the pulmonary artery (D, PA) and aorta (F, Ao) both arising from the right ventricle. An intermediate section (E) demonstrates the side-by-side arrangement of the great arteries.
Double-outlet right ventricle occurs rarely in Nkx2-5+/− F2 animals
Double-outlet right ventricle (DORV), in which both great arteries arise from the right ventricle and the aortic and mitral valves are separated by a muscular conus, has been reported in association with human NKX2-5 mutation. Two Nkx2-5+/− F2 animals were found to have DORV, one each from among 1552 C57Bl/6 X FVB/N and 1104 C57Bl/6 X A/J intercross hearts examined (Figure 4). The rarity of DORV precludes conclusions about the role of modifier genes in its pathogenesis. We note, though, that defects associated with human NKX2-5 mutation that are more common than DORV in the general population like hypoplastic left heart syndrome have not been found in any Nkx2-5+/− mouse.17, 18, 25 Such defects may have not been found either because the sample size remains too small or because the inbred strains examined do not carry the relevant susceptibility alleles.
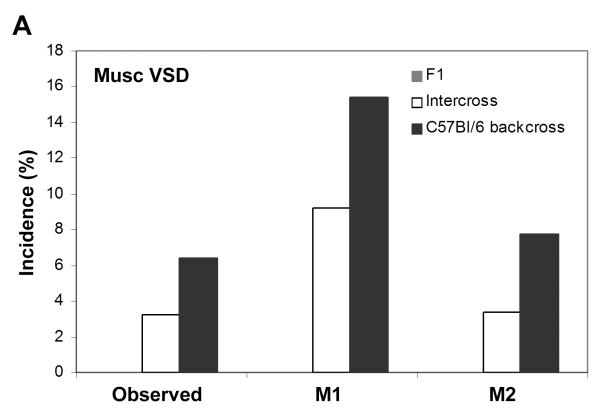
Genotypes at multiple modifier loci determine the VSD phenotype
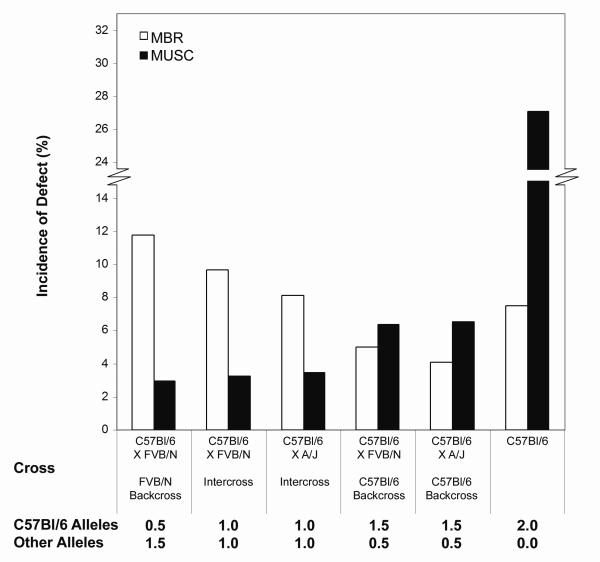
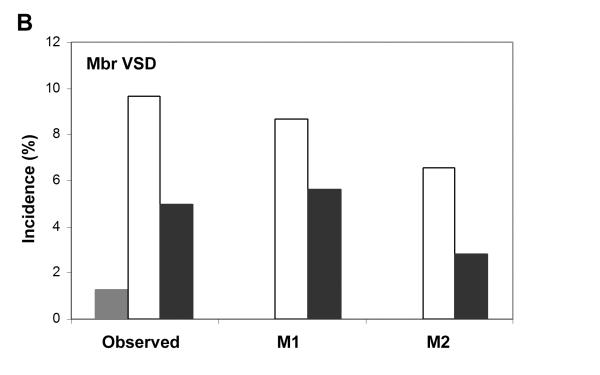
Membranous and muscular VSDs are found in Nkx2-5+/− hearts, but muscular VSDs are more common in the C57Bl/6 background (P < 0.0005; Figure 5). Which type of VSD develops appears to be determined by the cumulative effect of susceptibility genotypes at multiple modifier loci for either defect. We compared the incidence of each VSD type to the fraction of the C57Bl/6 genome in the genetically heterogeneous F2 crosses, as expected from a Mendelian distribution (Figure 5). There was a strong, positive correlation for muscular VSD (r = 0.91, P < 0.04) and a negative correlation for membranous VSD (r = −0.97, P < 0.006). Thus, C57Bl/6, FVB/N and A/J all carry recessive, susceptibility alleles at multiple loci for either VSD phenotype, but in the mixed strain backgrounds the additive effect of the C57Bl/6 susceptibility genotypes is less or greater than the other two strains for membranous and muscular VSD, respectively. Additional epistatic effects between loci may also influence the incidence of specific congenital heart defects, as shown by segregation analyses below.
Figure 5.
The incidence of muscular and membranous VSD among the F2 crosses and C57Bl/6 background is determined by the cumulative effect of multiple, strain-specific susceptibility genotypes. Muscular VSD is more common in Nkx2-5+/− animals in the C57Bl/6 background than membranous (P< 0.0005). In the F2 crosses, muscular VSD incidence is positively correlated with the average fraction of the C57Bl/6 genome in the progeny (R = 0.91, P < 0.02). Membranous VSD is negatively correlated (R = −0.97, P < 0.003). The average number of C57Bl/6 or non-C57Bl/6 alleles per locus based on a Mendelian distribution in each F2 cross is noted. MBR, membranous VSD. MUSC, muscular VSD.
ASD and VSD co-occur more frequently than expected by chance in Nkx2-5+/− hearts of mixed genetic background
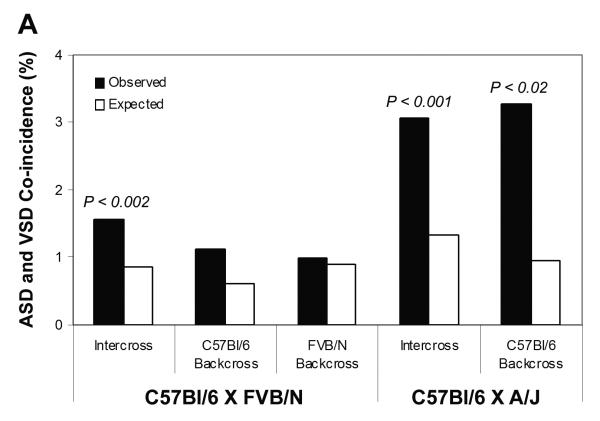
Polymorphic modifier genes clearly influence the development of specific types of defects in Nkx2-5 mutation. To test the hypothesis that the same polymorphism could increase susceptibility to two different defects, the incidence of hearts having both defects was compared to the product of the individual defect incidences in the population, i.e., the chance or null hypothesis. VSD and ASD co-occur more often than expected by chance in the C57Bl/6 X FVB/N intercross and the C57Bl/6 X A/J intercross and backcross to C57Bl/6 (Figure 6A). In the two F2 intercrosses where the sample sizes are large, ASD co-occurred with either muscular or membranous VSD more often than expected (Figure 6B). On the other hand, muscular and membranous VSD did not co-occur more often than expected. The co-occurrence of AVSD with other heart defects was not evaluated because of its low incidence. Therefore, some modifiers may increase the susceptibility to several types of heart defects in the presence of Nkx2-5 mutation whereas others may affect the development of just one.
Figure 6.
Some modifier loci may contribute to the development of both ASD and VSD. (A) ASD and VSD co-occur in the F2 intercrosses and C57Bl/6 backcross of the C57Bl/6 X A/J F1 more often than expected by the null hypothesis of complete independence between the defects. (B) The co-incidence rates are subdivided by VSD types in the two intercross populations, which have sufficiently large sample sizes for statistical comparison.
Segregation analysis of the genetic architecture of common septal defects
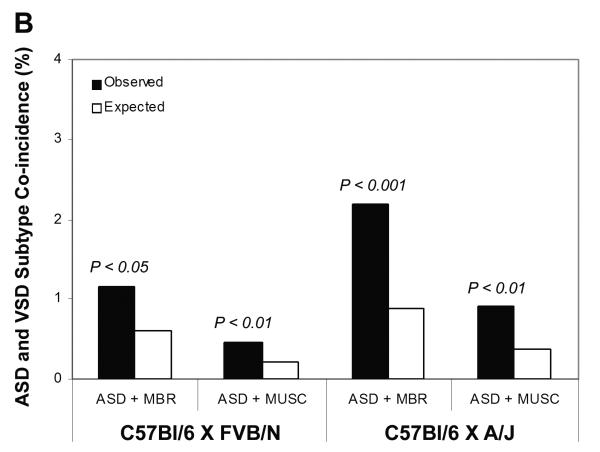
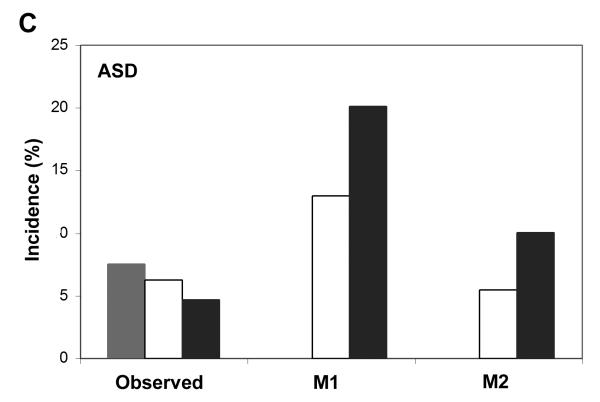
To characterize the genetic architecture of modifiers that influence ASD and VSD susceptibility in Nkx2-5+/− animals, we examine two segregation models. The models focus on the C57Bl/6 X FVB/N crosses because data from F2 backcrosses to both parental strains are available. How well the predictions of a model fit the observed data set lower bounds on the number of modifiers and interactions that are involved in the pathogenesis of particular defects.
The first model, M1, postulates two loci A and B that do not interact. C57Bl/6 and FVB/N carry the recessive, susceptibility alleles of A and B, respectively. The effects of susceptibility genotypes at A and B are estimated from the incidences in the C57Bl/6 strain and the F2 backcross to FVB/N. The expected incidences in the F2 intercross and C57Bl/6 backcross are then calculated from the model. Inclusion in the model of additional loci does not alter its predictions because the total effect of susceptibility alleles from one strain reduces to a single term. The predictions deviate significantly from the observed incidences of ASD and muscular VSD (P < 0.0001) but approximate the membranous VSD incidences (P = 0.14. Figure 7A-C). Therefore, at least two loci affect all three defect types.
Figure 7.
Segregation analyses define the minimum number of modifier loci and interactions involved in the susceptibility to ASD and VSD. The observed and expected incidences of (A) muscular VSD, (B) membranous VSD, and (C) ASD are predicted in the Nkx2-5+/− C57Bl/6 X FVB/N F1 and F2 progeny under two segregation models. Model M1 postulates two loci that do not interact. M2 postulates three loci, two of which interact. M1 approximates the observed incidences of membranous VSD but fits muscular VSD and ASD poorly. M2 fits muscular VSD well but not ASD or membranous VSD. Both models predict no defects in the F1, which contrasts with the ASDs observed.
Model M2 permits interaction between two modifier loci. In the simplest case, C57Bl/6 carries the recessive susceptibility alleles at two modifier loci A and B, which interact synergistically. FVB/N carries the recessive susceptibility allele at a third locus C. If the effect of A or B alone is negligible compared to their interaction, then the incidence of the defect in C57Bl/6 provides an estimate of the epistatic effect. Based on this model, the incidences attributed to the epistatic effect and locus C, as estimated from the F2 FVB/N backcross, match the observed incidences of muscular VSD in the F2 intercross and C57Bl/6 backcross (Figure 7A).
M2 underestimates the incidences of membranous VSD in the F2 intercross and C57Bl/6 backcross (P < 0.0001, Figure 7B). M2 may not model the genetic architecture of membranous VSD because either epistatic interactions have no role (i.e., M1 is correct) or there are unaccounted interactions between C57Bl/6 and FVB/N alleles at other loci.
M2 poorly fits the ASD incidences in the F2 intercross and C57Bl/6 backcross (P < 0.0001; Figure 7C). ASDs appear more genetically complex than VSD. First, additional loci and interactions must be postulated to account for the >4-fold difference in the incidence of ASD between the C57Bl/6 backcross and C57Bl/6. Inspection of the incidences in the crosses indicates that more than two modifier loci in each of the lines are likely be involved. Second, M1 and M2 predict the absence of defects in the F1 because homozygosity of a susceptibility allele at a modifier locus is assumed necessary for a defect. The assumption appears reasonable for muscular and membranous VSDs but not for ASD. The presence of ASDs in the F1 suggests that heterozygosity at some loci confer susceptibility.
Taken together, the two segregation models indicate that three or more modifier loci and at least one epistatic interaction influence the susceptibility to muscular VSD and ASD in Nkx2-5+/− animals. At least two loci influence membranous VSD susceptibility. The loci and interactions inferred from the C57Bl/6 X FVB/N crosses probably represent only a subset of all that exist among inbred mouse strains or the human population. A more precise estimate of the number of modifier loci in the mouse model, whether independent or epistatic, involved in any of the defects requires additional information, such as genetic linkage analyses that are underway.
Discussion
Normal cardiac development is critical for the survival of an individual. Any mechanism that could ensure normal development would increase the fitness of a species. In the short term, natural selection would eliminate major deleterious mutations. In contrast, stabilizing selection could promote the evolution of a versatile system that buffers the effects of genetic and environmental perturbations to the developing heart. The invariance of the normal heart form would then be enhanced.6 Waddington described the general mechanism metaphorically as “canalization” in which development flows down channels to produce a highly invariant wild-type form. He considered the depth of the channels analogous to the degree of buffering, which he deduced to have a genetic basis.26 Crucial phenotypes are maintained about a stable optimum. Sufficiently great insults, however, decanalize an individual and reveal the influence of cryptic variants of modifier genes that do not affect the phenotype of genetically wild-type individuals.5 Investigation of modifier genes thus provides an alternative approach to the genetic pathways that shape a normal heart. Cryptic polymorphisms within them may give rise to much of the complexity of congenital heart disease.
The results of inbred strain crosses indicate that modifier genes contribute to the canalization and decanalization of cardiac development in the presence of Nkx2-5 mutation. A large fraction of Nkx2-5+/− animals in the C57Bl/6 background has atrial and ventricular septal defects, whereas few among F1 hybrid crosses to FVB/N or A/J do. Defects recur in F2 crosses at a lower incidence than in C57Bl/6. We interpret this to mean that strain-specific polymorphisms of modifier genes alter the susceptibility of certain cardiac developmental pathways to Nkx2-5 mutation but do not affect the wild-type form. Complementation of susceptibility alleles in the F1 and homozygosity at some but not all modifier loci in the F2 contribute to the relative differences in defect incidence in the successive crosses. Furthermore, analysis of the incidences of ASD and VSD in the F2 crosses and C57Bl/6 suggest that modifier loci act independently of or epistatically with other loci. Thus, a protective allele at a modifier locus might directly reduce the risk of a defect or abrogate a synergistic interaction between loci that increases risk.
The surprisingly normal hearts of Nkx2-5+/− animals from the F1 hybrid crosses illustrate the important role of polymorphic modifier genes in ensuring the robustness of cardiac development. Protective polymorphisms likely exist against a variety of insults, as reductions in heart defect incidence have also been observed in Tbx5 or Gata4 mutants in mixed compared to isogenic strain backgrounds.14, 15 The greater heterogeneity in humans could provide even more genetic material to buffer against numerous, potentially common insults like nutrient deprivation or congenital infection. For well-canalized traits, cryptic variation can accumulate in a population in the absence of a major perturbation because the phenotype is buffered against change.5 Natural selection due to diverse pressures in the wild could also maintain heterogeneity because normally cryptic polymorphisms may be protective or detrimental depending upon the context. The resulting genetic architecture could ensure that a fraction of the population survives almost any particular perturbation.
Recessive susceptibility alleles of modifier genes exist in each of the three inbred strains examined, given the presence of defects in the Nkx2-5+/− F2 progeny from all the parental backcrosses and intercrosses. Our statistical analysis of thousands of hearts reveals that modifier genes fixed for different variants in the inbred strains influence the development of specific types of defects in the presence of Nkx2-5 mutation. Relative to the other strain backgrounds, C57Bl/6 carries polymorphisms that increase the susceptibility to muscular VSD, and A/J carries polymorphisms that increase the susceptibility to ASD and AVSD. Modifier genes reside in pathways that affect the development of individual or multiple anatomic structures like the atrial and ventricular septum, based upon the higher than expected co-incidence of some defects. The observations inform how modifier loci and interactions could be mapped to define the genetic pathways leading from Nkx2-5 mutation to various types of defects.
Even genetic diseases thought to exhibit simple Mendelian inheritance manifest with incomplete penetrance and varying phenotypes. The properties of genetic modifiers of the Nkx2-5 mutant phenotype help to explain the basis of the variable presentations of congenital heart disease. Ostensibly sporadic cases of congenital heart disease could result from germline or somatic mutations, teratogens, or purely stochastic events. Our results offer an alternative, but not mutually exclusive possibility that polymorphisms of genetic modifiers can either suppress or promote the effect of a major mutation. Maximum genetic heterogeneity in the F1 is associated with near complete suppression of deleterious phenotypes, leading to normal carriers. On the other hand, homozygosity at some loci in the F2 contributes to the manifestation of a specific defect among multiple potential phenotypes, which in a heterogeneous human population could appear like sporadic disease or pleiotropic defects.
This large study, which systematically varies the genetic background of a mouse model, offers insights into how genetic modifiers ensure normal cardiac development and influence the manifestation of congenital heart disease. Knowledge resulting from the characterization and identification of the modifiers in the mouse will almost certainly be relevant to human disease because pathways in cardiovascular development and physiology are strongly conserved. For example, dozens of quantitative trait loci that affect blood pressure are common between rodent models and human populations.27, 28 Cardiac development is robust. Appreciating how, one could conceivably mimic nature to reduce the heavy burden of congenital heart disease on children and their families.
Supplementary Material
Acknowledgements
We thank Goska Bielinska, James Cheverud, D.C. Rao, Alan Schwartz, David Wilson, and members of the Jay laboratory for their helpful input.
Funding sources JBW was supported by a Ruth L. Kirschstein National Research Service Award from the Developmental Cardiology and Pulmonary Training Program (NIH/NHLBI T32 HL007873) and by the Lucille P. Markey Pathway in Human Pathobiology. PYJ is a Scholar of the Child Health Research Center of Excellence in Developmental Biology at Washington University School of Medicine (NIH K12-HD001487). This work was supported by the American Heart Association, Edward Mallinckrodt Jr. Foundation, Hartwell Foundation and March of Dimes (PYJ).
Footnotes
Disclosures: The authors have no financial conflicts of interest.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- (1).Bruneau BG. Transcriptional regulation of vertebrate cardiac morphogenesis. Circ Res. 2002;90:509–19. doi: 10.1161/01.res.0000013072.51957.b7. [DOI] [PubMed] [Google Scholar]
- (2).Gruber PJ, Epstein JA. Development gone awry: congenital heart disease. Circ Res. 2004;94:273–83. doi: 10.1161/01.RES.0000116144.43797.3B. [DOI] [PubMed] [Google Scholar]
- (3).Ursell PC, Byrne JM, Strobino BA. Significance of cardiac defects in the developing fetus: a study of spontaneous abortuses. Circulation. 1985;72:1232–6. doi: 10.1161/01.cir.72.6.1232. [DOI] [PubMed] [Google Scholar]
- (4).Chinn A, Fitzsimmons J, Shepard TH, Fantel AG. Congenital heart disease among spontaneous abortuses and stillborn fetuses: prevalence and associations. Teratology. 1989;40:475–82. doi: 10.1002/tera.1420400510. [DOI] [PubMed] [Google Scholar]
- (5).Gibson G, Dworkin I. Uncovering cryptic genetic variation. Nat Rev Genet. 2004;5:681–90. doi: 10.1038/nrg1426. [DOI] [PubMed] [Google Scholar]
- (6).Gibson G. Decanalization and the origin of complex disease. Nat Rev Genet. 2009;10:134–40. doi: 10.1038/nrg2502. [DOI] [PubMed] [Google Scholar]
- (7).Basson CT, Bachinsky DR, Lin RC, Levi T, Elkins JA, Soults J, Grayzel D, Kroumpouzou E, Traill TA, Leblanc-Straceski J, Renault B, Kucherlapati R, Seidman JG, Seidman CE. Mutations in human TBX5 cause limb and cardiac malformation in Holt-Oram syndrome. Nat Genet. 1997;15:30–5. doi: 10.1038/ng0197-30. [DOI] [PubMed] [Google Scholar]
- (8).Li QY, Newbury-Ecob RA, Terrett JA, Wilson DI, Curtis AR, Yi CH, Gebuhr T, Bullen PJ, Robson SC, Strachan T, Bonnet D, Lyonnet S, Young ID, Raeburn JA, Buckler AJ, Law DJ, Brook JD. Holt-Oram syndrome is caused by mutations in TBX5, a member of the Brachyury (T) gene family. Nat Genet. 1997;15:21–9. doi: 10.1038/ng0197-21. [DOI] [PubMed] [Google Scholar]
- (9).Schott JJ, Benson DW, Basson CT, Pease W, Silberbach GM, Moak JP, Maron BJ, Seidman CE, Seidman JG. Congenital heart disease caused by mutations in the transcription factor NKX2-5. Science. 1998;281:108–11. doi: 10.1126/science.281.5373.108. [DOI] [PubMed] [Google Scholar]
- (10).Garg V, Kathiriya IS, Barnes R, Schluterman MK, King IN, Butler CA, Rothrock CR, Eapen RS, Hirayama-Yamada K, Joo K, Matsuoka R, Cohen JC, Srivastava D. GATA4 mutations cause human congenital heart defects and reveal an interaction with TBX5. Nature. 2003;424:443–7. doi: 10.1038/nature01827. [DOI] [PubMed] [Google Scholar]
- (11).Gill HK, Splitt M, Sharland GK, Simpson JM. Patterns of recurrence of congenital heart disease: an analysis of 6,640 consecutive pregnancies evaluated by detailed fetal echocardiography. J Am Coll Cardiol. 2003;42:923–9. doi: 10.1016/s0735-1097(03)00853-2. [DOI] [PubMed] [Google Scholar]
- (12).Nora JJ. From generational studies to a multilevel genetic-environmental interaction. J Am Coll Cardiol. 1994;23:1468–71. doi: 10.1016/0735-1097(94)90393-x. [DOI] [PubMed] [Google Scholar]
- (13).Whittemore R, Wells JA, Castellsague X. A second-generation study of 427 probands with congenital heart defects and their 837 children. J Am Coll Cardiol. 1994;23:1459–67. doi: 10.1016/0735-1097(94)90392-1. [DOI] [PubMed] [Google Scholar]
- (14).Bruneau BG, Nemer G, Schmitt JP, Charron F, Robitaille L, Caron S, Conner DA, Gessler M, Nemer M, Seidman CE, Seidman JG. A murine model of Holt-Oram syndrome defines roles of the T-box transcription factor Tbx5 in cardiogenesis and disease. Cell. 2001;106:709–21. doi: 10.1016/s0092-8674(01)00493-7. [DOI] [PubMed] [Google Scholar]
- (15).Rajagopal SK, Ma Q, Obler D, Shen J, Manichaikul A, Tomita-Mitchell A, Boardman K, Briggs C, Garg V, Srivastava D, Goldmuntz E, Broman KW, Woodrow BD, Smoot LB, Pu WT. Spectrum of heart disease associated with murine and human GATA4 mutation. J Mol Cell Cardiol. 2007;43:677–85. doi: 10.1016/j.yjmcc.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Sakata Y, Koibuchi N, Xiang F, Youngblood JM, Kamei CN, Chin MT. The spectrum of cardiovascular anomalies in CHF1/Hey2 deficient mice reveals roles in endocardial cushion, myocardial and vascular maturation. J Mol Cell Cardiol. 2006;40:267–73. doi: 10.1016/j.yjmcc.2005.09.006. [DOI] [PubMed] [Google Scholar]
- (17).Benson DW, Silberbach GM, Kavanaugh-McHugh A, Cottrill C, Zhang Y, Riggs S, Smalls O, Johnson MC, Watson MS, Seidman JG, Seidman CE, Plowden J, Kugler JD. Mutations in the cardiac transcription factor NKX2.5 affect diverse cardiac developmental pathways. J Clin Invest. 1999;104:1567–73. doi: 10.1172/JCI8154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).McElhinney DB, Geiger E, Blinder J, Benson DW, Goldmuntz E. NKX2.5 mutations in patients with congenital heart disease. J Am Coll Cardiol. 2003;42:1650–5. doi: 10.1016/j.jacc.2003.05.004. [DOI] [PubMed] [Google Scholar]
- (19).Tanaka M, Chen Z, Bartunkova S, Yamasaki N, Izumo S. The cardiac homeobox gene Csx/Nkx2.5 lies genetically upstream of multiple genes essential for heart development. Development. 1999;126:1269–80. doi: 10.1242/dev.126.6.1269. [DOI] [PubMed] [Google Scholar]
- (20).Azhari N, Shihata MS, Al-Fatani A. Spontaneous closure of atrial septal defects within the oval fossa. Cardiol Young. 2004;14:148–55. doi: 10.1017/S1047951104002069. [DOI] [PubMed] [Google Scholar]
- (21).Biben C, Weber R, Kesteven S, Stanley E, McDonald L, Elliott DA, Barnett L, Koentgen F, Robb L, Feneley M, Harvey RP. Cardiac septal and valvular dysmorphogenesis in mice heterozygous for mutations in the homeobox gene Nkx2-5. Circ Res. 2000;87:888–95. doi: 10.1161/01.res.87.10.888. [DOI] [PubMed] [Google Scholar]
- (22).Tanaka M, Berul CI, Ishii M, Jay PY, Wakimoto H, Douglas P, Yamasaki N, Gehrmann J, Maguire CT, Schinke M, Seidman CE, Seidman JG, Kurachi Y, Izumo S. A mouse model of congenital heart disease: cardiac arrhythmias and atrial septal defect caused by haploinsufficiency of the cardiac transcription factor Csx/Nkx2.5. Cold Spring Harb Symp Quant Biol. 2002;67:317–25. doi: 10.1101/sqb.2002.67.317. [DOI] [PubMed] [Google Scholar]
- (23).Nguyen M, Camenisch T, Snouwaert JN, Hicks E, Coffman TM, Anderson PA, Malouf NN, Koller BH. The prostaglandin receptor EP4 triggers remodelling of the cardiovascular system at birth. Nature. 1997;390:78–81. doi: 10.1038/36342. [DOI] [PubMed] [Google Scholar]
- (24).Shen Y, Leatherbury L, Rosenthal J, Yu Q, Pappas MA, Wessels A, Lucas J, Siegfried B, Chatterjee B, Svenson K, Lo CW. Cardiovascular phenotyping of fetal mice by noninvasive high-frequency ultrasound facilitates recovery of ENU-induced mutations causing congenital cardiac and extracardiac defects. Physiol Genomics. 2005;24:23–36. doi: 10.1152/physiolgenomics.00129.2005. [DOI] [PubMed] [Google Scholar]
- (25).Elliott DA, Kirk EP, Yeoh T, Chandar S, McKenzie F, Taylor P, Grossfeld P, Fatkin D, Jones O, Hayes P, Feneley M, Harvey RP. Cardiac homeobox gene NKX2-5 mutations and congenital heart disease: associations with atrial septal defect and hypoplastic left heart syndrome. J Am Coll Cardiol. 2003;41:2072–6. doi: 10.1016/s0735-1097(03)00420-0. [DOI] [PubMed] [Google Scholar]
- (26).Waddington CH. Canalization of development and the inheritance of acquired characters. Nature. 1942;150:563–5. doi: 10.1038/1831654a0. [DOI] [PubMed] [Google Scholar]
- (27).Cowley AW., Jr. The genetic dissection of essential hypertension. Nat Rev Genet. 2006;7:829–40. doi: 10.1038/nrg1967. [DOI] [PubMed] [Google Scholar]
- (28).Feng M, Deerhake ME, Keating R, Thaisz J, Xu L, Tsaih SW, Smith R, Ishige T, Sugiyama F, Churchill GA, DiPetrillo K. Genetic Analysis of Blood Pressure in 8 Mouse Intercross Populations. Hypertension. 2009;54:802–9. doi: 10.1161/HYPERTENSIONAHA.109.134569. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.