Abstract
Insomnia is a major health problem, with significant psychological, health, and economic consequences. Studies have demonstrated that cognitive-behavioural therapy can effectively treat insomnia; however, treatment availability is limited by many factors, including a lack of trained clinicians. One potential way to overcome these barriers is to use the Internet to deliver treatment. Toward this aim, we developed a self-guided, interactive, tailored Internet intervention for adults with insomnia (SHUTi: Sleep Healthy Using The Internet). The current paper provides a detailed description of SHUTi and examines users’ perceptions of the intervention’s usefulness and effectiveness. The study was part of a larger randomised controlled trial (RCT) to test the efficacy of SHUTi, but findings in this paper are based only on the 21 participants who completed the post-assessment after using SHUTi. The overwhelming majority rated SHUTi as convenient, understandable, and useful. Nearly all (95%) indicated that the program had at least somewhat improved their sleep, sleep efficiency, and overall quality of life. Ninety percent perceived the intervention as effective and predicted it would be effective in producing a long-term cure. Although these results were based on a small sample, they provide encouraging evidence of the potential for Internet interventions to be accepted by patients.
Keywords: Internet, Web-based, Insomnia, Patient Acceptance, Behaviour Treatment, Intervention
Introduction
Sleep difficulties are one of the most prominent medical complaints among Americans. Epidemiologic studies indicate that 30% to 48% of the adult population report insomnia symptoms (Ohayon, 2002), with approximately 10% to 15% suffering from chronic insomnia (Ford & Kamerow, 1989; Mellinger, Balter, & Uhlenhuth, 1985; Ohayon; Simon & VonKorff, 1997). Despite the prevalence of insomnia, fewer than 15% of individuals with chronic insomnia have received any type of treatment (Mellinger et al., 1985) and less than 5% have sought medical care specifically for their sleep problems (Gallup Organization, 1991). When help is obtained, it is usually in the form of pharmacotherapy (Morin, LeBlanc, Daley, Gregoire, & Merette, 2006; National Sleep Foundation, 2005). Although sleep medications have been shown to be an effective short-term treatment for acute insomnia (Holbrook, Crowther, Lotter, Cheng, & King, 2000; Nowell et al., 1997), their use is also associated with several limitations, including the risk of dependency, adverse daytime effects, decreased effectiveness over time and sleep stage alterations (Holbrook et al., 2000; Morin & Wooten, 1996).
Cognitive-behavioural therapy (CBT) for insomnia (Morin, 1993; Morin & Espie, 2003) is a non-pharmacological treatment alternative that targets the maladaptive behaviours and dysfunctional thoughts believed to perpetuate sleep difficulties, and it has been identified as one of the most effective insomnia treatments (Edinger, Wohlgemuth, Radtke, Marsh, & Quillian, 2001; Morin et al., 2006). Meta-analyses have confirmed the reliability of cognitive and behavioural techniques in treating insomnia (Morin; Morin et al., 1999; Murtagh & Greenwood, 1995; Pallesen, Nordhus, & Kvale, 1998). In addition, CBT for insomnia has been associated with longer lasting treatment gains and greater patient satisfaction, with individuals rating the treatment as more effective and acceptable than medication (Morin, Gaulier, Barry, & Kowatch, 1992; Morin, Colecchi, Stone, Sood, & Brink, 1999).
Despite the positive outcomes associated with CBT for insomnia, its ability to address insomnia on a public health scale is currently limited by inaccessibility to treatment and clinicians, including a shortage of trained clinicians and poor geographic distribution of knowledgeable professionals (Edinger & Means, 2005). Using the Internet to deliver treatment could be an effective and efficient way to overcome these barriers, allowing for greater dissemination and access for underserved patient populations. The interactive Internet intervention called Sleep Healthy Using The Internet (SHUTi) was created to investigate the efficacy of delivering a fully automated CBT intervention for insomnia via the Web. This paper provides a detailed description of the SHUTi system and summarizes users’ reactions to SHUTi in terms of perceived usefulness and effectiveness.
SHUTi System Description
The Internet intervention (SHUTi) is accessed through the main welcome page at www.shuti.net where users enter their unique username and password to gain access to the full system. From this welcome page, some features of the system are open to both authorized users and the general public, including: information about how to contact the research team, a “Frequently Asked Questions” (FAQ) page addressing technical issues, links to sleep organizations in the United States, and a “Learn About the Program” tab that provides a brief introduction to the system. Given online security concerns and the importance of maintaining patient confidentiality, all user data is protected and not accessible to unauthorized parties.
Home Page
The SHUTi system was created with an emphasis on both usability and appeal, with the ultimate goal of creating an online environment that was engaging, effective, and secure. Figure 1 shows the basic structure of the program.
Figure 1.
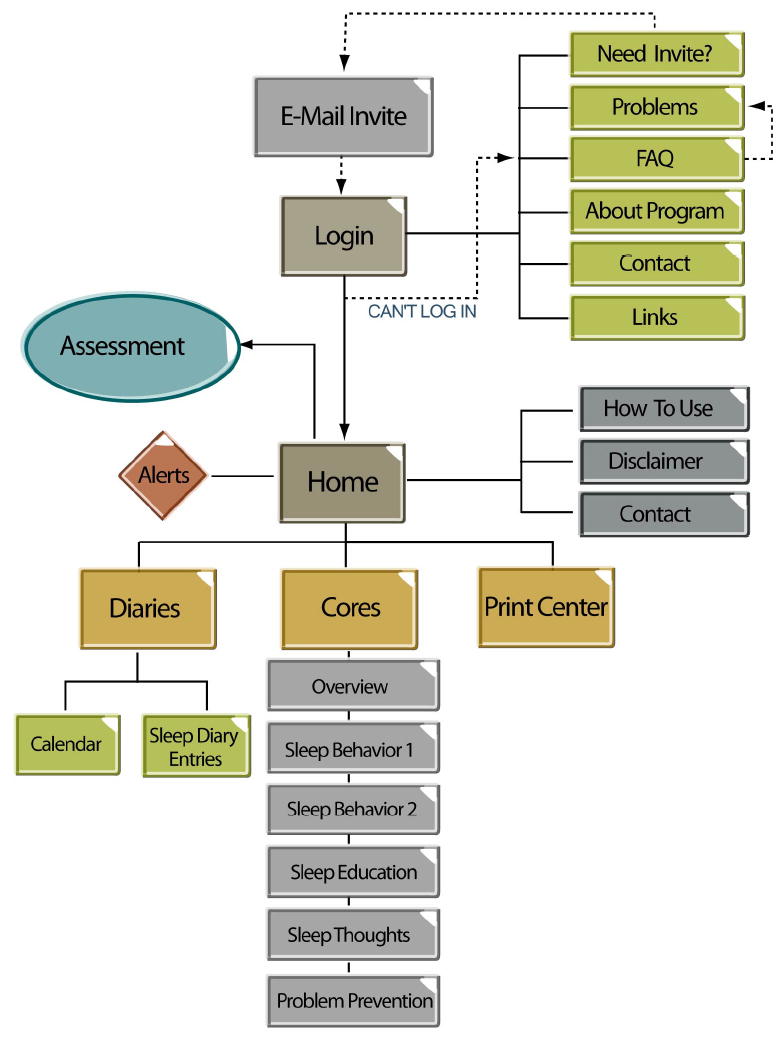
SHUTi Framework
Once logged in, each user is presented with a personalized “Home Page” (see Figure 2) that provides information based on that user’s progress in the SHUTi system (for example, a new user would have a welcome page and instructions about beginning the program, whereas a user who is further along might have information about completing the next treatment assignment). The left side of the screen contains the “Information Center,” which also allows for easy navigation to each of the main sections of the site: Home, Diaries, Cores and Print Center. The “Alerts” section of the Information Center provides messages about user progress through the program including upcoming assignments. In addition, the Information Center has tabbed links to Sleep Diary entry forms and the Diary Calendar, which are two frequently visited sections users access to complete sleep diaries. The Print Center contains the printable elements completed in the program. The Diaries and Cores sections are described in greater detail below.
Figure 2.
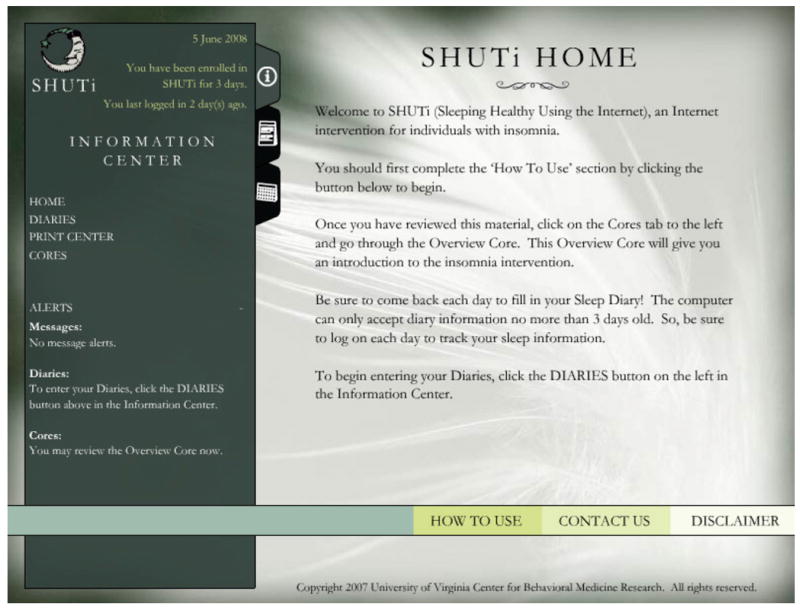
SHUTi Home Page
There are three tabs at the bottom of the home page that users are able to access at any time. New users are instructed to click on the “How to Use” tab, which brings them to a tutorial containing step-by-step instructions for how to navigate the program. The “Contact Us” tab on the home page provides contact information for the study office and researchers. The “Disclaimer” tab reminds users that the information provided is for educational purposes only and should not replace or override a physician’s care.
Sleep Diaries
The SHUTi system relies on standard Sleep Diary data that is entered by the user to track symptoms, record progress, and tailor treatment recommendations. The Sleep Diary (Morin, 1993) consists of ten questions inquiring about length of naps, hour of bedtime, minutes to fall asleep, number of nighttime awakenings, duration of nighttime awakenings, hour of awakening in the morning, hour of arising (getting out of bed) in the morning, and a description of any sleep aids that were used. In addition, users rate two questions on a 5-point scale: how exhausted/refreshed they feel upon awakening and how restless/sound they rate their sleep.
Users are required to keep two weeks of baseline diaries prior to beginning the intervention to establish a baseline, and are then encouraged to continue to keep diaries throughout the intervention. During treatment, this sleep diary information is used to calculate the users’ sleep efficiency and assign personalized “Sleep Windows” (an assigned bedtime and arising time which is the only time the user is instructed to sleep) based on their sleep efficiency of the past week. Use of Sleep Windows results in a form of sleep restriction that involves placing limits on the amount of time spent in bed to match the actual amount of time asleep to strengthen the homeostatic sleep drive and increase sleep efficiency. Users receive a new Sleep Window if they enter a sufficient number of diaries.
As is typically done in face-to-face insomnia treatment, Sleep Window changes are not made without documented improvements (or regressions) in sleep efficiency. If users do not enter the required diaries, and thus do not receive new Sleep Windows, this could hinder treatment progress. Because mandating diary entry during the intervention could lead to increased nonadherence, the program allows users to continue without entering daily diaries and receiving the weekly Sleep Window. Algorithms were developed and incorporated into the program to determine whether the Sleep Window should be increased, decreased, or maintained. Users then select their preferred arising time and the program assigns a Sleep Window.
Cores
The Cores act as an online analog for the weekly sessions conducted in face-to-face CBT for insomnia. The SHUTi intervention content contains the essential treatment elements of CBT, including behavioural, educational, and cognitive techniques (Morin, 1996; Morin, 1993). Operationalizing insomnia treatment into the Cores allowed for clear definition and separation of treatment components.
Each Core follows a similar structure: Core objectives, main content, homework, and review. The Core objectives provide a rationale for learning the material from that week’s Core by addressing the questions, “What will I learn in this core?” and “Why is this core important?” Each Core also includes a Homework page that lists suggestions for how to improve sleep over the coming week. Finally, each Core ends with a Summary page that provides a review of the main points presented in the Core.
A new Core becomes available one week after the completion of the previous week’s Core, and each Core typically requires 45-60 minutes to complete. Users are free to revisit Cores as many times as they like. The main content screens for each Core address a unique aspect of insomnia treatment through a variety of interactive features, including myth/reality buttons, animations that provide a topic visual to enhance comprehension, “learn more” buttons that provide in-depth information about a topic, quizzes to test a user’s knowledge and impart additional information, and vignettes.
The intervention involves a high degree of interactivity and personalization. In addition to the tailoring based on sleep diaries (described above), personalization also occurs in the form of goal-setting exercises. At the beginning of the program, for example, users are asked to set specific targets for different aspects of their sleep including their sleep onset latency, number of nighttime awakenings, and time spent awake in the middle of the night. At the end of the study, they are asked to re-evaluate their goals and to track their progress towards meeting these goals. They are then given the opportunity to set and work toward longer-term goals using the knowledge, skills, and cognitions gained while using SHUTi. Although they are not instructed to redo the program with these revised goals, they are invited to continue to use SHUTi to help them meet these longer-term goals. Further personalization occurs throughout the SHUTi program in the form of symptom checklists and homework assignments in which users are asked to describe the specifics of their experience with insomnia.
A brief description of each of the six treatment Cores is included below. Figure 3 illustrates key content from the SHUTi Cores.
Figure 3.
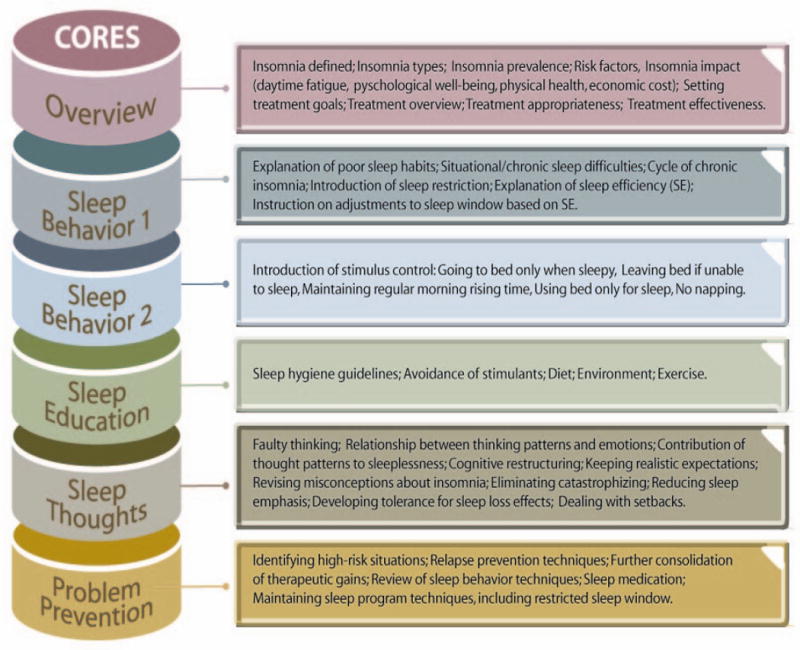
SHUTi Treatment Cores
Overview Core
The Overview Core provides an overview and rationale for treatment. It defines insomnia, discusses its impact, and lists the associated risk factors. The Core concludes by highlighting the appropriateness and effectiveness of CBT treatment for insomnia.
Sleep Behavior Core 1
Sleep Behavior Core 1 introduces sleep restriction (Spielman, Saskin, & Thorpy, 1987) and stimulus control (Bootzin, 1972; Bootzin, 1979). Sleep restriction is a form of systematic sleep deprivation in which a restricted Sleep Window is maintained to allow the body to relearn proper sleeping dynamics and increase sleep efficiency. Stimulus control aims to reduce the anxiety or conditioned arousal individuals may feel when attempting to go to bed.
Presented during the same week as the Overview Core, this Core lays out the rationale for the sleep restriction element of treatment. After users set a preferred arising time, they are assigned a restricted period for sleep (Sleep Window) for the upcoming week based on sleep efficiency calculations from their baseline diaries. Typical concerns about sleep restrictions are addressed (e.g., “…if I stay in bed less time, I won’t be able to function the next day”), and users are cautioned that they may initially feel more tired as they adjust to the new sleep schedule. Although Stimulus Control is covered in detail in the following Core (Behavior Core 2), a few “Ground Rules” are introduced in this Core, including going to bed only when sleepy, getting out of bed when not sleeping, maintaining a regular morning arising time, avoiding naps, and reserving the bed for sleep and sex only.
Sleep Behavior Core 2
Sleep Behavior Core 2 extends what is taught about sleep restriction and stimulus control in Sleep Behavior Core 1. It begins by addressing user’s concerns about the restricted sleep schedule and incorporates motivational elements because this is a critical point in treatment when people often feel tired after a week of sleep restriction. It acknowledges the difficulty of this step, while also reminding users that this is a common experience and that coping with daytime sleepiness will ultimately help them to sleep better at night. Behavior Core 2 then reviews and expands the “Ground Rules” of Stimulus Control taught in Behavior Core 1. Behavior Core 2 also provides additional instructions about the importance of developing a pre-sleep routine and “unwinding” for at least one hour prior to bedtime.
Sleep Education Core (Sleep Hygiene)
The Education Core (also called Sleep Hygiene) follows Sleep Behavior Core 2. In this Core, users learn about the many lifestyle (caffeine, nicotine, alcohol, diet, exercise) and environmental (room temperature, noise, lighting, air quality, bedroom and bedding comfort) factors that impact sleep. Users view an example of two different people’s rooms and are able to click through and “correct” the different problems that they encounter. For example, they can make a number of environmental changes to Peter’s bedroom including lowering the curtains to block out light from the street or changing the thermostat in the bedroom to avoid extreme temperatures. Users can help Yvonne adopt a more sleep-friendly lifestyle through a number of adjustments such as replacing her glass of wine with milk.
Sleep Thoughts Core (Cognitive Restructuring)
The Sleep Thoughts Core (also called Cognitive Restructuring) attempts to address and change the sleep-related negative beliefs and thoughts that may exacerbate sleep difficulties. This Core introduces common sleep-related cognitive distortions (called “thinking errors” in the program) including all-or-none thinking, exaggeration/catastrophic thinking, over-generalization, selective attention, and emotional reasoning. Among other exercises, users are asked to record their daily thoughts, beliefs, and attitudes about sleep. They are subsequently asked to evaluate which emotions result from these thoughts or beliefs. Lastly, they are taught strategies to challenge (and ultimately replace) unhelpful sleep cognitions.
Problem Prevention Core
The fifth and final treatment Core aims to solidify users’ knowledge from the previous Cores and prevent future problems by preparing users to cope with potentially difficult nights in the future. The Core provides instructions on how to continue adjusting the Sleep Window and reviews the educational, behavioural, and cognitive techniques presented in the previous Cores. The Core also provides an explanation of the difference between a lapse (an occasional bad night) and relapse (the return of insomnia) and works to prepare users for both. Users learn to identify situations that place them at high risk for experiencing poor sleep, as well as strategies to manage their thoughts and behaviours when the inevitable bad night occurs. They are encouraged to continue to use SHUTi as needed.
SHUTi Treatment Utility and Impact
Twenty-two adults with insomnia received access to SHUTi as part of a randomised, controlled, efficacy trial of the program. Twenty-one participants (95%) returned for post-assessment and described their experiences with SHUTi. This sample of 21 was primarily female (81%), Caucasian (95%), and well-educated (16.6±3.1 years of education). On average, participants were 45.0±10.8 years of age, and all participants reported using the Internet and checking email at least once per week. As part of study enrollment, participants went through a screening interview to determine that they met criteria for insomnia (based on a combination of requirements from the DSM-IV and the ICSD) and to introduce them to the online system. Their average duration of sleep problems was over 10 years (10.6±8.2 years) and they reported an average of 5.1±1.6 nights per week of sleep difficulties.
To assess their experience using SHUTi, users completed the Internet Intervention Utility Questionnaire (UQ) for SHUTi and the Internet Intervention Impact Questionnaire (IQ) for SHUTi. The UQ is a 16-item measure designed to assess usability, likeability, usefulness, understandability, and convenience of the Internet intervention. The IQ is a 14-item measure designed to assess users’ perceptions of the impact of the online program on targeted symptoms. Responses on both questionnaires are rated on 5-point Likert scales from 0 (“not at all”) to 4 (“very”). A previous Internet intervention study found good internal reliability for these measures (alpha =.69 for the IQ; and a range of .64 to .94 on the subscales of the IQ) (Ritterband et al., 2008). The UQ also includes two additional open-ended questions that inquire about the most and least helpful aspects of the program to assist with future modifications to the system.
Utility
With respect to utility, 100% of subjects indicated that the program was mostly (3) easy or very (4) easy and convenient to use. Ninety-five percent indicated that it was mostly or very understandable; eighty-six percent reported that it was mostly or very useful; and 81% indicated that it was mostly or very enjoyable (95% indicated that it was at least somewhat (2) enjoyable).
Information/Implementation
Ninety percent stated that the material was mostly (3) or very (4) consistent with what they heard from other doctors or clinicians. With respect to adhering to treatment, 86% said they were mostly or very able to keep the sleep diaries, and 62% stated that were mostly or very able to follow through with treatment recommendations (90% stated that they were at least somewhat (2) able to do so).
Service Reduction
Of those who responded to the service reduction items (n=14), at least half indicated that the Internet intervention at least somewhat (2) reduced their doctor visits (57%) and phone calls made to their doctors (50%).
Acceptability/Suitability
Ninety percent stated that they believed the treatment was mostly (3) or very (4) effective, and 81% indicated that the treatment would be mostly or very effective in producing a long term cure. Fifty-seven percent also believed it was mostly or very effective in improving other aspects of their daytime functioning (e.g., alertness, performance, mood), and 95% believed it was at least somewhat (2) effective in improving these aspects.
Perceived Effectiveness
Ninety percent stated that they believed the treatment was mostly (3) or very (4) effective, and 81% indicated that the treatment would be mostly or very effective in producing a long term cure. Fifty-seven percent also believed it was mostly or very effective in improving other aspects of their daytime functioning (e.g., alertness, performance, mood), and 95% believed it was at least somewhat (2) effective in improving these aspects.
Impact
Perceived Impact
Ninety-five percent of participants who used SHUTi indicated that they believed the program at least somewhat (2) improved their sleep. Ninety-five percent also believed that it at least somewhat improved their sleep efficiency. Ninety percent indicated that they believed it at least somewhat improved their overall quality of life. Although 45% (n=10) stated that sleep medications were “not a problem for me,” for those who responded to this item (n=11), 73% believed that the program at least somewhat helped them reduce or eliminate the need for sleep medications.
Discussion
Insomnia is a significant public health problem with few non-pharmacological treatment resources. The SHUTi intervention attempts to operationalize and transform a well-validated face-to-face treatment for insomnia (CBT for insomnia) into a Web-based system. The SHUTi program is an interactive system that tailors its recommendations to each user through the use of their input, such as daily sleep diaries and symptom checklists. SHUTi users overwhelmingly found the program to be easy, convenient, understandable, useful, and enjoyable to use. Most users felt able to keep sleep diaries, a key component of CBT treatment for insomnia, and the majority felt able to implement treatment recommendations. They reported that information was largely consistent with clinician recommendations and that it tended to reduce the frequency with which they needed to consult their physician regarding sleep problems. They indicated it was somewhat effective in improving sleep, sleep efficiency, and overall quality of life. Ninety percent reported that the system was mostly or very effective, and on the whole, users felt the program was an acceptable means of treatment for both themselves and others.
Limitations
Although these findings offer support for the acceptability of an Internet-based intervention for insomnia, they must be considered in light of some limitations. The sample in this study was small and homogenous in terms of racial / ethnic (95% Caucasian), geographic (all in central Virginia, United States) and diagnostic diversity (primary insomnia only). More research is needed to evaluate how different populations (e.g., diagnostic comorbidity, geographic diversity) respond to an Internet intervention for insomnia. This sample of SHUTi users also had a significantly lower attrition (5%) rate than is typically found in other Internet interventions (21%) (Wantland, Portillo, Holzemer, Laughter, & McGhee, 2004). Given the low attrition rate, this sample may have been more motivated than most Internet intervention populations and thus rated it more positively than would be seen in other populations. Further studies will need to examine whether patients in other samples (for insomnia, as well as other disorders) continue to evaluate Internet interventions as useful and effective.
Conclusion
Although these results were based on a small sample of users, they provide encouraging evidence of the potential for Internet interventions to be accepted by patients. Obviously the success of Internet interventions will depend not only on patient acceptance but also on treatment success, and efficacy trials will remain a critical part of the expanding Internet intervention literature (Murray, Burns, See, Lai, & Nazareth, 2005; Ritterband et al., 2003; Wantland et al., 2004). This indication of patient acceptance does, however, add support for the notion that Internet interventions have considerable potential for delivering structured behavioural programs.
Figure 4.
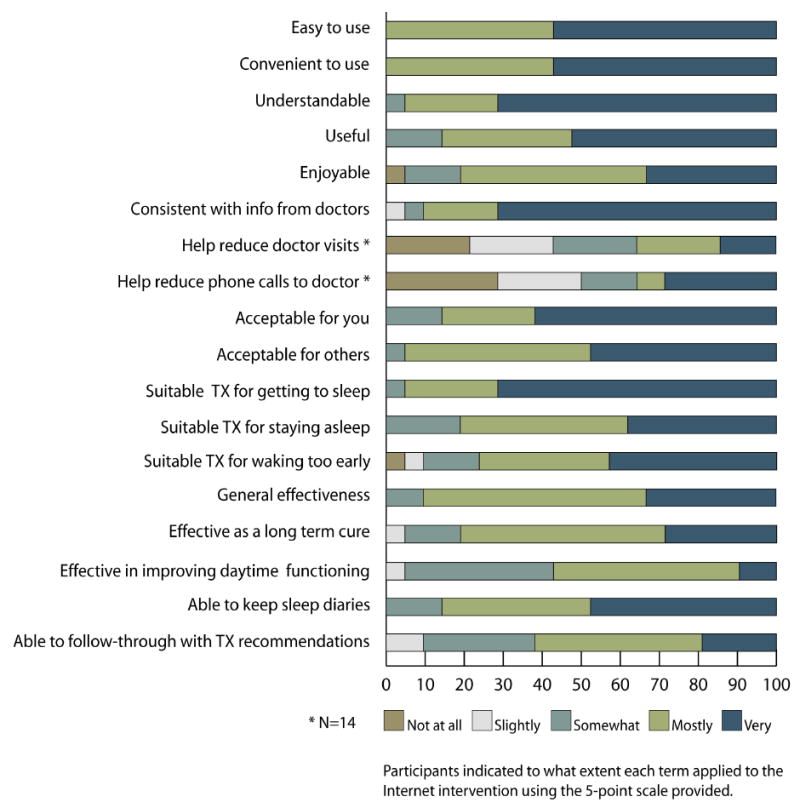
graphically depicts the findings from the Internet Intervention Utility Questionnaire (UQ).
Results from Internet Intervention Utility Questionnaire
Figure 5.
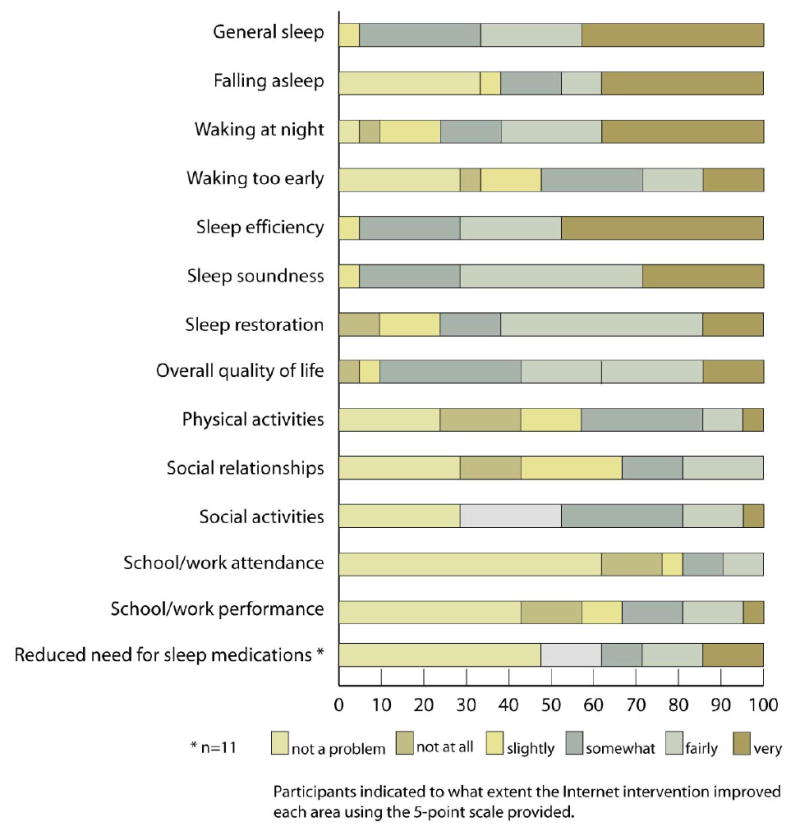
graphically depicts the above findings from the Internet Intervention Impact Questionnaire (IQ).
Results from the Internet Intervention Impact Questionnaire
Acknowledgments
We thank Jonathan Cole Sletten and Dominion Digital for their expertise in developing the SHUTi program. We also thank Michelle Hilgart for design expertise and Anne McEwan for help with manuscript preparation. This study was funded by grant R34MH70805 from the National Institutes of Health/National Institute of Mental Health.
Contributor Information
Frances P. Thorndike, Email: fpq4s@virginia.edu, Department of Psychiatry and Neurobehavioral Sciences, University of Virginia Health System, Charlottesville, VA, USA.
Drew K. Saylor, Email: dks6s@virginia.edu, Department of Psychiatry and Neurobehavioral Sciences, University of Virginia Health System, Charlottesville, VA, USA.
Elaine T. Bailey, Email: etb6n@virginia.edu, Department of Psychiatry and Neurobehavioral Sciences, University of Virginia Health System, Charlottesville, VA, USA.
Linda Gonder-Frederick, Email: lag3g@virginia.edu, Department of Psychiatry and Neurobehavioral Sciences, University of Virginia Health System, Charlottesville, VA, USA.
Charles M. Morin, Email: cmorin@psy.ulaval.ca, École de Psychologie, Université Laval, Québec, Canada.
Lee M. Ritterband, Email: lr5b@virginia.edu, Department of Psychiatry and Neurobehavioral Sciences, University of Virginia Health System, Charlottesville, VA, USA.
References
- Bootzin RR. Stimulus control treatment for insomnia. Proceedings of the American Psychological Association. 1972;7:395–396. [Google Scholar]
- Bootzin RR. Effects of self-control procedures for insomnia. American Journal of Clinical Biofeedback. 1979;2:70–77. [Google Scholar]
- Edinger JD, Means MK. Cognitive-behavioral therapy for primary insomnia. Clinical Psychology Review. 2005;25(5):539–558. doi: 10.1016/j.cpr.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Does cognitive-behavioral insomnia therapy alter dysfunctional beliefs about sleep? Sleep. 2001;24(5):591–599. doi: 10.1093/sleep/24.5.591. [DOI] [PubMed] [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders, an opportunity for prevention? JAMA. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Gallup Organization. Sleep in America: A national survey of US adults. National Sleep Foundation; 1991. [Google Scholar]
- Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ : Canadian Medical Association Journal = Journal De l’Association Medicale Canadienne. 2000;162(2):225–233. [PMC free article] [PubMed] [Google Scholar]
- Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: Prevalence and correlates. Archives of General Psychiatry. 1985;42(3):225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- Morin CM. Relief from insomnia: Getting the sleep of your dreams. New York: Doubleday; 1996. [Google Scholar]
- Morin CM. Insomnia: Psychological assessment and management. New York: The Guilford Press; 1993. [Google Scholar]
- Morin CM, Wooten V. Psychological and pharmacological approaches to treating insomnia: Critical issues in assessing their separate and combined effects. Clinical Psychology Review. 1996;16(6):521–542. [Google Scholar]
- Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: Update of the recent evidence (1998-2004) Sleep. 2006;29(11):1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial. JAMA. 1999;281(11):991–999. doi: 10.1001/jama.281.11.991. [DOI] [PubMed] [Google Scholar]
- Morin CM, Gaulier B, Barry T, Kowatch RA. Patients’ acceptance of psychological and pharmacological therapies for insomnia. Sleep. 1992;15(4):302–305. doi: 10.1093/sleep/15.4.302. [DOI] [PubMed] [Google Scholar]
- Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia: An American Academy of Sleep Medicine review. Sleep. 1999;22(8):1134–1156. doi: 10.1093/sleep/22.8.1134. [DOI] [PubMed] [Google Scholar]
- Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: Prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Medicine. 2006;7(2):123–130. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- Morin CM, Espie CA. Insomnia: A clinical guide to assessment and treatment. New York: Kluwer Academic/Plenum Publishers; 2003. [Google Scholar]
- Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database of Systematic Reviews. 2005;(3) doi: 10.1002/14651858.CD004274.pub4. CD004274. [DOI] [PubMed] [Google Scholar]
- Murtagh DR, Greenwood KM. Identifying effective psychological treatments for insomnia: A meta-analysis. Journal of Consulting and Clinical Psychology. 1995;63(1):79–89. doi: 10.1037//0022-006x.63.1.79. [DOI] [PubMed] [Google Scholar]
- National Sleep Foundation. 2005 “Sleep in America” poll. A report prepared by WB&A Market Research for the National Sleep Foundation 2005 [Google Scholar]
- Nowell PD, Mazumdar S, Buysse DJ, Dew MA, Reynolds CF, Kupfer DJ. Benzodiazepines and zolpidem for chronic insomnia: A meta-analysis of treatment efficacy. JAMA. 1997;278(24):2170–2177. [PubMed] [Google Scholar]
- Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Pallesen S, Nordhus IH, Kvale G. Nonpharmacological interventions for insomnia in older adults: A meta-analysis of treatment efficacy. Psychotherapy. 1998;35(4):472–482. [Google Scholar]
- Ritterband LM, Ardalan K, Thorndike FP, Magee JC, Saylor DK, Cox DJ, et al. Real world use of an internet intervention for pediatric encopresis. Journal of Medical Internet Research. 2008;10(2):e16. doi: 10.2196/jmir.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Gonder-Frederick LA, Cox DJ, Clifton AD, West RW, Borowitz SM. Internet interventions: In review, in use, and into the future. Professional Psychology: Research & Practice. 2003;34(5):527–534. [Google Scholar]
- Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. The American Journal of Psychiatry. 1997;154(10):1417–1423. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- Spielman AJ, Saskin P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987;10:45–56. [PubMed] [Google Scholar]
- Wantland D, Portillo C, Holzemer W, Laughter R, McGhee E. The effectiveness of web-based vs. non-web-based interventions: A meta-analysis of behavioral change outcomes. Journal of Medical Internet Research. 2004;6(4):e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]


