Abstract
Background: Observational studies have linked higher intakes of whole grains to lower abdominal adiposity; however, the association between whole- and refined-grain intake and body fat compartments has yet to be reported.
Objective: Different aspects of diet may be differentially related to body fat distribution. The purpose of this study was to assess associations between whole- and refined-grain intake and abdominal subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT).
Design: Cross-sectional associations between whole- and refined-grain intakes, waist circumference measures, and abdominal SAT and VAT volumes were examined in 2834 Framingham Heart Study participants (49.4% women; age range: 32–83 y). Dietary information was assessed with the use of a semiquantitative food-frequency questionnaire.
Results: Whole-grain intake was inversely associated with SAT (2895 compared with 2552 cm3 in the lowest compared with the highest quintile category, P for trend < 0.001) and VAT (1883 compared with 1563 cm3, P for trend < 0.001), after adjustment for age, sex, current smoking status, total energy, and alcohol intake. In contrast, refined-grain intake was positively associated with SAT (2748 compared with 2934 cm3, P for trend = 0.01) and VAT (1727 compared with 1928 cm3, P for trend < 0.001) in multivariable models. When SAT and VAT were evaluated jointly, the P value for SAT was attenuated (P = 0.28 for whole grains, P = 0.60 for refined grains), whereas VAT remained associated with both whole grains (P < 0.001) and refined grains (P < 0.001).
Conclusions: Increasing whole-grain intake is associated with lower VAT in adults, whereas higher intakes of refined grains are associated with higher VAT. Further research is required to elicit the potential mechanisms whereby whole- and refined-grain foods may influence body fat distribution.
INTRODUCTION
Obesity rates continue to escalate in the United States with one-third of the population classified as obese (1), thus predisposing them to increased risk of type 2 diabetes. The economic burden associated with this epidemic is enormous, and estimated medical costs for an obese patient are 42% higher than for those who are normal weight (2). Observational studies have found that middle-aged adults who consume more whole-grain foods have a lower body mass index (BMI) and central obesity (3), and people tend to gain significantly less weight over time if they consume on average ≥3 servings whole grains/d (4).
Whole grains are defined as grains that “consist of the intact, ground, cracked or flaked fruit of the grains, whose principal components—the starchy endosperm, germ and bran—are present in the same relative portions as they exist in the intact grain” (5). Because the outer bran and inner germ of the grain are discarded during the milling process, there is a substantial loss in dietary fiber, B vitamins, iron, magnesium, vitamin E, and other measured and unmeasured dietary constituents (6). As a consequence, refined-grain products are nutritionally inferior to their whole-grain counterparts, are less nutrient-dense, and thus do not confer the same potential health benefits. Despite the apparent nutritional differences between whole and refined grains, few studies have linked refined grains to weight gain (4).
In epidemiologic studies, BMI is typically used as an indicator of overall adiposity, and waist circumference as a proxy measure of abdominal adiposity. Waist circumference is a composite of both the subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) compartments. Emerging evidence suggests that these different fat compartments may be associated with differential metabolic risk factors. In particular, the VAT compartment is a more pathogenic fat depot (7). To date, there are limited observational data on the consumption of whole and refined grains in relation to more valid measures of body fat distribution. We have previously observed that a higher diet quality as assessed by the 2005 Dietary Guidelines for Americans Adherence Index was associated with lower volumes of both SAT and VAT (8). Given that VAT is more strongly related to metabolic risk factors than is SAT, examining the association of whole- and refined-grain intake on body fat depots may provide further insight into the health correlates of grain intake and cardiometabolic risk factors. Thus, the objective of the current study was to examine the association of whole- and refined-grain intakes and SAT and VAT volumes (n = 2834), as assessed by multidetector-computed tomography (MDCT), and waist circumference (n = 2645) in a large population-based cohort of ambulatory adults.
SUBJECTS AND METHODS
Participants from this study were part of the Framingham Heart Study MDCT Study, a substudy of the Framingham Heart Offspring and Third Generation study cohorts. The Framingham Offspring Study began in 1971 by enrolling 5124 adult offspring (and offspring's spouses) of the original Framingham Heart Study cohort participants. Framingham Offspring Study follow-up visits occur every 3–4 y and include physical examinations, anthropometric measurements, laboratory tests, and diet- and health-related questionnaires (9). In 2002, 4095 adults who had at least one parent in the Offspring cohort were enrolled in the Framingham Heart Study Third Generation cohort and underwent physical examinations and questionnaires similar to the Offspring cohort (10).
Between June 2002 and April 2005, a total of 1418 Offspring and 2111 Third Generation participants underwent MDCT scanning for coronary and abdominal aortic calcium as described elsewhere (7). Younger adults were excluded from the MDCT substudy, because the purpose of this study was to determine coronary artery calcification. The measure of SAT and VAT volumes were ascertained secondarily after the study completion. Of the 3529 participants imaged, 3370 had interpretable computed tomographic measures of both SAT and VAT. Participants were excluded from this analysis if they had a previous diagnosis of diabetes or a fasting plasma glucose concentration ≥7.0 mmol/L (126 mg/dL) or if they used medications for diabetes (n = 214). After exclusion for invalid dietary information and incomplete covariate information, the final sample size was 2834 participants (men, n = 1434, women, n = 1400). The Institutional Review Board for Human Research at Boston University Medical Center and Massachusetts General Hospital and the Human Investigation Research Committee at Tufts Medical Center approved the protocol. All subjects provided written informed consent before study participation.
Waist circumference and abdominal adipose tissue measurements
Waist circumference was measured at the level of the umbilicus while the participant was standing. An 8-slice MDCT scanner (LightSpeed Ultra; GE Health Care, Milwaukee, WI) was used to determine volumes of SAT and VAT (Aquarius 3D Workstation; TeraRecon Inc, Sam Mateo, CA) with use of a standard protocol, as previously described (11). In brief, 25 contiguous 5-mm-thick slices (120 kVp, 400 mA, gantry rotation time 500 ms, and table feed 3:1) were obtained covering 125 mm above the level of S1 (protocol began at bottom of S1). To identify fat pixels, an image display window width of –195 to –45 Hounsfield units and a window center of –120 Hounsfield units were used. The abdominal muscular wall was manually traced to separate the visceral from the subcutaneous compartment. In a subset of 100 randomly selected participants, the interreader reproducibility of VAT and SAT was assessed by 2 independent readers, and the interreader reproducibility was high (interclass correlations of 0.997 for SAT and 0.992 for VAT) (11).
Dietary assessment
Usual dietary intakes for the previous year were assessed with use of a 126-item semiquantitative food-frequency questionnaire (12). The questionnaires were mailed to participants before the Framingham Heart Study examination, and the participants were asked to bring the completed questionnaire with them to the study appointment. Dietary information was considered valid if reported energy intakes were ≥2.51 MJ/d (600 kcal/d) for both men and women and <6.74 MJ/d (4000 kcal/d) for women and <17.54 MJ/d (4200 kcal/d) for men and if fewer than 13 food items were left blank. The relative validity of this food-frequency questionnaire has been evaluated for both nutrients and foods in other studies (12–14). Intakes of whole and refined grains and dietary covariates, alcohol, fruit and vegetables, and dairy were estimated for each individual by multiplying the frequency of consumption by the portion consumed and summing food items. Dietary fiber was estimated by multiplying the frequency of consumption by the fiber content for each food item and summing across items.
The whole-grain category included whole-grain cold breakfast cereal, oatmeal, dark bread, brown rice, other grains (eg, bulgur, kasha, couscous), popcorn, bran, and wheat germ. A serving of whole grains included any one of the following: 1 cup cold breakfast cereal; 0.5 cup cooked oatmeal, brown rice, or other grains; a slice of dark bread; 3 cups popcorn; or 2 tablespoons added bran or added germ. The refined-grain category included refined-grain cold breakfast cereal, other cooked breakfast cereal, white bread, English muffins, bagels, muffins, biscuits, white rice, pasta, pancakes, waffles, crackers, and pizza. A serving of refined grains included any one of the following: 1 cup cold breakfast cereal, 0.5 cup cooked cereal, 1 slice white bread, one-half English muffin or bagel, 1 muffin or biscuit, 0.5 cup white rice or pasta, 1 pancake or waffle, 7 crackers, or 1 slice pizza. Brand names were used to classify cold breakfast cereals as either whole grain (≥25% whole grain or bran by weight) or refined grain (<25% whole grain or bran by weight), as defined originally by Jacobs et al (15). In the absence of information on brand names, breakfast cereals were not included in the overall whole- or refined-grain categories (n = 19).
Assessment of covariates
Lifestyle covariates included sex, age (y), current smoking status (yes or no; ie, smoked regularly in the past year), total energy intake (kJ/d), and alcohol intake (g/d). Dietary covariates included calories from total fat (percentage energy/d), intakes of fruit and vegetables, and dairy (servings/d) and dietary fiber intake (g/d), added bran (g/d), and dietary glycemic index, an indicator of carbohydrate quality as assessed by its influence on blood glucose measures. BMI was calculated as weight (kg) divided by height squared (m2).
Statistical analyses
We conducted statistical analyses using SAS statistical software (release 9.2; SAS Institute, Cary, NC). VAT and SAT displayed a moderate positive skewing that was normalized by applying a square root transformation. Analyses were performed on both the transformed and untransformed data; because results were similar and for ease of interpretation, we present the results of analyses completed with use of the untransformed data. To relate the subject characteristics to whole- and refined-grain intake, age- and sex-adjusted descriptive comparisons across quintile categories of whole- and refined-grain intake were evaluated with use of least-squares means from the general linear models procedure (PROC GLM). A test for linear trend across quintile categories of whole- and refined-grain intake was performed by assigning the median value of grain intake for each category and treating these as a continuous variable. Dietary characteristics were also adjusted for energy intake.
Relations between grain intakes and SAT and VAT volumes were examined with use of least-squares means determined within quintile categories of whole- and refined-grain intake, with adjustment for the following lifestyle covariates: age, sex, smoking status, total energy, and alcohol intake. Additional models were used with adjustment for dietary covariates including percentage energy from total fat, dairy, and fruit and vegetable intake. To consider the effect of attributes of whole grains, dietary fiber, added bran, and glycemic index were adjusted in separate models. SAT models were also adjusted for VAT volumes, and VAT models were adjusted for SAT volumes. Similarly, the whole-grain models were adjusted for intakes of refined grain, and the refined-grain models were adjusted for intakes of whole grain. A test for linear trend for SAT and VAT volumes across quintile categories of whole- and refined-grain intake was performed by assigning the median value of grain intake for each category and treating these as a continuous variable, with adjustment for the covariates listed above. In VAT and waist circumference models only, further adjustments for BMI were performed to determine whether associations were independent of overall obesity. We did not adjust for BMI in SAT models due to collinearity between SAT and BMI. To examine whether the associations between whole- and refined-grain intake and VAT may be mediated by insulin concentration, we further adjusted for fasting insulin.
To assess whether associations between whole- and refined-grain intakes and SAT and VAT outcomes were similar in men and women, interactions between sex and whole- and refined-grain intake were tested in multivariate models adjusted for age, smoking status, total energy, and alcohol intake. Furthermore, because increasing age is associated with larger VAT, we assessed for effect modification by age (modeled as a both a continuous variable and categorical variable, <50 compared with ≥50 y of age) by testing interaction terms in the multivariable models.
For presentation of the joint association of whole- and refined-grain intake on VAT, quintile (Q) categories, Q2 through Q4, were combined to represent the medium intake, whereas Q1 and Q5 represent the lowest and highest categories of intake, respectively. The joint association of whole- and refined-grain intake with VAT was modeled as the interaction of the 3 categories of intake (resulting in 9 least-squares means) with terms for their main effects included in the models and Tukey's adjustment for multiple comparisons.
Secondary analyses were performed on the multivariate least-squares means models adjusted for lifestyle factors, with further adjustment for physical activity, on a limited subset of subjects for whom physical activity data were available (n = 2643). The general estimating equation procedure (PROC GEE) was applied to the models to account for familial correlations in the study sample and to examine its influence on the observed associations.
RESULTS
In this study sample, on the basis of servings per week, the major dietary sources of whole grains included dark bread (31%), ready-to-eat breakfast cereals (26%), oatmeal (22%), popcorn (20%), and brown rice (20%). With respect to refined grains, the major dietary sources included pasta (24%), English muffins (17%), white bread (17%), pizza (12%), white rice (11%), and ready-to-eat-breakfast cereal (4%). Multivariable-adjusted participant characteristics across whole- and refined-grain intake quintile categories are summarized in Tables 1 and 2, respectively. The median intake of whole grain ranged from 0.14 to 2.93 servings/d in the lowest to highest quintile category of whole-grain intake, respectively. Participants with higher whole-grain intakes were more likely to be older, have a lower BMI, and have higher intakes of fruit and vegetables and dairy. The median intake of refined grain ranged from 0.79 to 4.06 servings/d from the lowest to highest quintile category of refined-grain intake, respectively. Participants with higher refined-grain intake were more likely to be younger and male, have a higher BMI, and have a lower intake of fruit, vegetables, and dairy.
TABLE 1.
Subject characteristics by quintile (Q) categories of whole-grain intake1
| Whole-grain intake categories |
||||||
| Q1 | Q2 | Q3 | Q4 | Q5 | P for trend2 | |
| n | 575 | 559 | 567 | 566 | 567 | |
| Whole-grain intake (servings/d)3 | 0.14 (0.00–0.30) | 0.50 (0.31–0.71) | 0.98 (0.72–1.21) | 1.48 (1.22–2.03) | 2.93 (2.04–12.7) | — |
| Age (y)4 | 51.0 (50.2, 51.9) | 49.9 (49.1, 50.7) | 50.4 (49.6, 51.2) | 50.0 (49.2, 50.8) | 51.9 (51.9, 52.8) | 0.04 |
| Women (%)5 | 46 (42, 50) | 50 (46, 54) | 51 (47, 56) | 51 (47, 55) | 49 (45, 53) | 0.56 |
| BMI (kg/m2)67 | 27.4 (27.0, 27.8) | 27.5 (27.2, 27.9) | 27.5 (27.1, 27.9) | 26.5 (26.1, 26.8) | 26.3 (25.9, 26.7) | <0.001 |
| Waist circumference (cm)6 | 96.9 (95.8, 97.9) | 97.6 (96.5, 98.7) | 97.4 (96.4, 98.5) | 94.6 (93.5, 95.6) | 94.3 (93.2, 95.3) | <0.001 |
| Current smoker (%)6 | 17 (14, 20) | 16 (14, 19) | 11 (9, 14) | 9 (6, 12) | 8 (6, 11) | <0.001 |
| Energy intake (kJ)6 | 7278 (7074, 7481) | 7641 (7439, 7844) | 8166 (7963, 8368) | 8674 (8471, 8877) | 9636 (9434, 9839) | <0.001 |
| Alcohol intake (g/d)78 | 5.2 (4.6, 5.9) | 5.4 (4.8, 6.1) | 4.3 (3.8, 4.9) | 4.9 (4.4, 5.6) | 3.9 (3.4, 4.4) | <0.001 |
| Refined-grain intake (servings/d)8 | 2.9 (2.7, 3.0) | 2.7 (2.6, 2.8) | 2.6 (2.5, 2.7) | 2.4 (2.3, 2.5) | 2.0 (1.9, 2.1) | <0.001 |
| Fruit and vegetable intake (servings/d)78 | 4.0 (3.9, 4.2) | 4.7 (4.5, 4.8) | 4.8 (4.6, 5.0) | 5.3 (5.1, 5.5) | 5.7 (5.5, 5.9) | <0.001 |
| Dairy intake (servings/d)78 | 2.0 (1.9, 2.1) | 1.9 (1.8, 2.0) | 2.0 (1.9, 2.1) | 2.1 (2.0, 2.2) | 2.1 (2.0, 2.2) | 0.03 |
| Total fat (% of energy)8 | 33.7 (33.2, 34.3) | 32.8 (32.2, 33.3) | 32.1 (31.6, 32.6) | 30.6 (30.1, 31.1) | 28.6 (28.1, 29.2) | <0.001 |
Values are means; 95% CIs in parentheses (unless otherwise noted).
The median value in each quintile category was used as a continuous variable in a linear regression as a test for trend.
Values are medians; ranges in parentheses.
Adjusted for sex only.
Adjusted for age only.
Adjusted for age and sex.
Values are geometric means.
Adjusted for age, sex, and total energy intake.
TABLE 2.
Subject characteristics by quintile (Q) categories of refined-grain intake1
| Refined-grain intake categories |
||||||
| Q1 | Q2 | Q3 | Q4 | Q5 | P for trend2 | |
| n | 566 | 568 | 567 | 564 | 569 | — |
| Refined-grain intake (servings/d)3 | 0.79 (0.00–1.13) | 1.42 (1.14–1.69) | 1.99 (1.70–2.29) | 2.62 (2.30–3.15) | 4.06 (3.16–11.50) | |
| Age (y)4 | 51.3 (50.5, 52.1) | 51.5 (50.7, 52.3) | 50.5 (49.7, 51.3) | 49.9 (49.1, 50.7) | 50.1 (49.2, 50.9) | 0.02 |
| Women (%)5 | 58 (54, 62) | 52 (48, 56) | 46 (42, 50) | 47 (43, 51) | 44 (40, 48) | <0.001 |
| BMI (kg/m2)67 | 27.0 (26.6, 27.3) | 26.9 (26.5, 27.3) | 26.6 (26.3, 27.0) | 27.1 (26.7, 27.4) | 27.6 (27.2, 28.0) | 0.01 |
| Waist circumference (cm)6 | 96.0 (94.9, 97.0) | 95.9 (94.8, 96.9) | 95.2 (94.2, 96.3) | 96.4 (95.3, 97.5) | 97.2 (96.2, 98.3) | 0.10 |
| Current smoker (%)6 | 15 (12, 18) | 12 (10, 15) | 12 (9, 14) | 13 (10, 15) | 10 (7, 13) | 0.03 |
| Energy intake (kJ)6 | 6679 (6490, 6868) | 7403 (7215, 7591) | 8168 (7979, 8356) | 8856 (8668, 9044) | 10,295 (10,107, 10,483) | <0.001 |
| Alcohol intake (g/d)78 | 5.3 (4.7, 6.0) | 4.5 (4.0, 5.1) | 5.3 (4.7, 6.0) | 4.9 (4.3, 5.5) | 3.7 (3.2, 4.2) | <0.001 |
| Whole-grain intake (servings/d)8 | 1.5 (1.4, 1.6) | 1.5 (1.4, 1.5) | 1.3 (1.2, 1.4) | 1.1 (1.0, 1.2) | 0.8 (0.7, 0.9) | <0.001 |
| Fruit and vegetable intake (servings/d)78 | 5.2 (5.0, 5.4) | 5.0 (4.9, 5.2) | 5.0 (4.8, 5.2) | 4.8 (4.7, 5.0) | 4.3 (4.1, 4.5) | <0.001 |
| Dairy intake (servings/d)78 | 2.3 (2.2, 2.4) | 2.2 (2.1, 2.3) | 2.0 (1.9, 2.1) | 1.9 (1.8, 2.0) | 1.7 (1.6, 1.8) | <0.001 |
| Total fat (% of energy)8 | 33.4 (32.9, 34.0) | 31.8 (31.2, 32.3) | 31.6 (31.1, 32.1) | 30.9 (30.4, 31.4) | 30.2 (29.6, 30.7) | <0.001 |
Values are means; 95% CIs in parentheses (unless otherwise noted).
The median value in each quintile category was used as a continuous variable in a linear regression as a test for trend.
Values are medians; ranges in parentheses.
Adjusted for sex only.
Adjusted for age only.
Adjusted for age and sex.
Values are geometric means.
Adjusted for age, sex, and total energy intake.
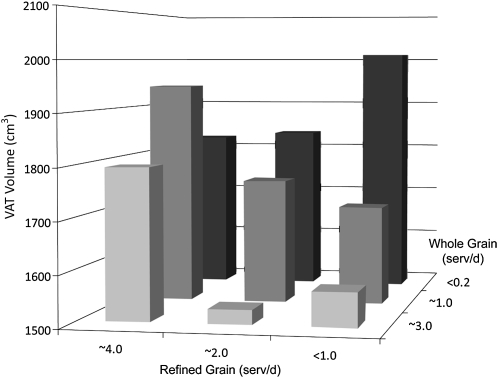
After adjustment for covariates, a significant inverse association was observed between whole-grain intake and waist circumference (97.0 compared with 93.7 cm in the lowest compared with highest quintile category, P for trend < 0.001), whereas a marginally significant positive association was observed with refined-grain intake (95.9 compared with 97.3 inches, P for trend = 0.06) (Table 3). The observed inverse association between whole-grain intake and waist circumference persisted after adjustment for other dietary and lifestyle factors (see Supplemental Table 1 under “Supplemental data” in the online issue). For VAT models, a weak interaction between sex and whole-grain intake was observed (P = 0.02). Although the slope was higher in men, the nature of the relation was similar in men and women, and so data from men and women were analyzed together. No significant interaction was observed with age. After adjustment for age, sex, smoking status, total energy, and alcohol intake, whole-grain intake was inversely associated with SAT and VAT in the lowest compared with the highest quintile category (Table 3). In contrast, refined-grain intake was positively associated with SAT and VAT. When VAT and SAT were jointly considered in models of whole- and refined-grain intakes, the P value for SAT was attenuated (P = 0.28 for whole grains, P = 0.60 for refined grains), whereas VAT remained associated with both whole grains (P < 0.001) and refined grains (P < 0.001). We further examined the joint effects of whole- and refined-grain intake on VAT (P for interaction = 0.005). Joint classification analysis showed that those who consumed more whole grains had lower VAT volumes but that this association was offset by increasing intake of refined grains (Figure 1).
TABLE 3.
Mean (95% CI) multivariate-adjusted waist circumference measures and abdominal measures of subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) models by whole- and refined-grain intake quintile (Q) categories
| Grain-intake categories |
||||||
| Q1 | Q2 | Q3 | Q4 | Q5 | P for trend | |
| Whole grain | ||||||
| Waist circumference (cm)1 | 97.0 (95.8, 98.2) | 97.6 (96.5, 98.8) | 97.2 (96.0, 98.4) | 94.2 (93.0, 95.5) | 93.7 (92.4, 94.9) | <0.001 |
| SAT (cm3)1 | 2895 (2772, 3017) | 2941 (2819, 3063) | 2917 (2793, 3041) | 2616 (2490, 2743) | 2552 (2422, 2682) | <0.001 |
| SAT (cm3)2 | 2756 (2661, 2852) | 2825 (2731, 2920) | 2855 (2759, 2952) | 2724 (2625, 2822) | 2739 (2638, 2841) | 0.28 |
| VAT (cm3)1 | 1883 (1807, 1959) | 1861 (1785, 1936) | 1808 (1731, 1885) | 1642 (1563, 1720) | 1563 (1482, 1643) | <0.001 |
| VAT (cm3)3 | 1864 (1805, 1923) | 1823 (1765, 1882) | 1780 (1720, 1840) | 1730 (1669, 1791) | 1676 (1614, 1739) | <0.001 |
| Refined grain | ||||||
| Waist circumference (cm)1 | 95.9 (94.7, 97.2) | 95.8 (94.6, 97.0) | 95.2 (94.0, 96.4) | 96.4 (95.2, 97.6) | 97.3 (96.0, 98.6) | 0.06 |
| SAT (cm3)1 | 2748 (2620, 2876) | 2743 (2618, 2868) | 2728 (2603, 2853) | 2862 (2737, 2987) | 2934 (2800, 3068) | 0.01 |
| SAT (cm3)2 | 2769 (2670, 2868) | 2812 (2715, 2909) | 2793 (2696, 2890) | 2789 (2692, 2886) | 2748 (2644, 2852) | 0.60 |
| VAT (cm3)1 | 1727 (1648, 1806) | 1680 (1602, 1757) | 1684 (1606, 1761) | 1818 (1741, 1895) | 1928 (1846, 2011) | <0.001 |
| VAT (cm3)3 | 1765 (1703, 1826) | 1720 (1660, 1780) | 1729 (1669, 1789) | 1811 (1752, 1871) | 1894 (1830, 1958) | <0.001 |
Adjusted for age, sex, smoking status, total energy, and alcohol intake.
Adjusted for covariates listed in footnote 1 with further adjustment for VAT.
Adjusted for covariates listed in footnotes 1 and 2 with further adjustment for SAT.
FIGURE 1.
Joint classification of whole- and refined-grain intake on visceral adipose tissue (VAT) volume. Multivariate-adjusted VAT was determined according to joint classifications of whole-grain and refined-grain intake. Analyses were adjusted for age, sex, current smoking status, alcohol intake, and total energy intake. (Supplemental Table 3 under “Supplemental data” in the online issue presents the multivariate-adjusted mean ± SE VAT volumes according to the joint classification of whole- and refined-grain intake.)
Further adjustment for refined-grain intake did not substantially change the associations between whole-grain intake and SAT or VAT volumes. In contrast, further adjustment for whole-grain intake attenuated associations between refined-grain intake and SAT (2772 compared with 2861 cm3, P for trend = 0.19 for lowest compared with highest quintile categories, respectively) but not VAT. The associations were substantially attenuated between refined-grain intake and VAT after adjustment for fasting insulin (1855 compared with 1871 cm3 in the lowest compared with highest quintile category, respectively; P for trend = 0.30), but associations remained significant between whole grains and VAT (1896 compared with 1677 cm3 in the lowest compared with highest quintile category, respectively; P for trend < 0.001) (see Supplemental Tables 1 and 2 under “Supplemental data” in the online issue).
Further adjustment for dietary factors (percentage energy from total fat; fruit and vegetable, and dairy intakes) and other individual dietary covariates, including dietary fiber, added bran, and glycemic index, did not substantially change associations between whole- or refined-grain intakes and SAT and VAT. Further adjustment for BMI (in VAT models only) did not change the associations between whole- or refined-grain intakes and VAT (see Supplemental Tables 1 and 2 under “Supplemental data” in the online issue).
The additional inclusion of physical activity as a covariate did not materially change associations between whole- or refined-grain intakes and SAT and VAT measurements, adjusted for age, sex, smoking status, total energy, and alcohol intakes (see Supplemental Tables 1 and 2). When the general estimating equation procedure was applied to the models to account for familial correlations in the study sample, results did not substantially differ (data not shown).
DISCUSSION
In this cohort of middle-aged adults, VAT volume was 10.1% lower in individuals consuming approximately ≥3 servings whole grains/d compared with those who essentially consumed no whole grains (<0.2 serving/d), even after accounting for other lifestyle and dietary factors. Although whole- and refined-grain intakes were associated with both SAT and VAT volumes when SAT and VAT were jointly considered, only the observed associations between whole- and refined-grain intake and VAT persisted, suggesting that refined and whole grains are differentially associated with SAT and VAT volumes. Furthermore, after considering the joint relation between whole- and refined-grain intake on VAT volume, the association between high whole-grain intake and VAT was diminished in people consuming ≥4 servings refined grains/d, indicating that refined grain may offset any potential benefits of whole grain on abdominal adiposity. We also observed an inverse association between whole-grain intake and waist circumference, whereas a positive association was observed between refined-grain intake and waist circumference, even after accounting for other lifestyle and dietary factors.
Although both SAT and VAT fat depots are metabolically active, the VAT compartment may be a unique pathogenic fat depot. Greater VAT may be responsible for the many aspects of the metabolic syndrome, including glucose intolerance, hypertension, dyslipidemia, and insulin resistance (16). In the Framingham Offspring cohort, we previously reported that higher intake of whole grain was inversely associated with the metabolic syndrome and insulin resistance (17). In the current study, fasting insulin concentrations were observed to attenuate the associations between refined-grain intake, but not whole-grain intake, and VAT volume, suggesting perhaps an intermediary role of insulin on the positive relation between refined-grain intake and VAT volume. The additional adjustment for insulin did not affect the relation observed between whole-grain intake and VAT. Higher intake of refined grain may lead to excess insulin secretion by pancreatic β cells, and this increased production leads to hyperinsulinemia and weight gain. The properties of refined grains (ie, the high glycemic index and low dietary fiber) may alter adipose tissue physiology, influence fuel partitioning (favoring storage over oxidation), and increase appetite (18). One prospective study observed that higher intakes of whole grain were related to less weight gain in women over 12 y, whereas higher intakes of refined grain were associated with greater weight gain (4).
To date, as far as we are aware, no observational study has differentially related whole-grain and refined-grain intake to direct measures of adiposity (such as those derived from CT) in adults. In a longitudinal analysis of high-risk Latino youth, higher intakes of total and insoluble dietary fiber were associated with significant decreases in VAT over a 1–2-y time period, whereas lower intakes of dietary fiber were associated with increases in VAT (19). In a diet and exercise intervention study in overweight Latino adolescents (20), small increases in dietary fiber (≈5 g/d) translated into significant reductions in VAT in 16 wk, whereas no significant effects of the intervention were observed on overall body weight or dual-energy X-ray absorptiometry (DXA) measures of body composition (21). However, DXA is unable to differentiate SAT from VAT.
Few studies have considered how dietary modification may alter body composition independent of changes in overall body weight. In a 12-wk, hypocaloric, free-living intervention study, obese adults with metabolic syndrome were instructed to either avoid whole-grain foods (ie, consume only refined grain) or to consume all their recommended grain servings from whole grain (22). Although similar changes in body weight, waist circumference, and percentage body fat (based on DXA) were observed in both groups, a significantly greater loss in percentage abdominal fat was observed in the whole-grain group than in the refined-grain group. In contrast, one small study found no change in body fat or fat mass (determined by underwater weighing) after 6 wk on a hypocaloric oat-containing diet (23).
In the present study, we further adjusted for added bran and dietary fiber and the associations persisted, suggesting that these were not the mediating attributes of the diet related to body fat distribution. Koh-Banerjee et al (24) examined the association between changes in whole-grain intake and weight gain over an 8-y period in middle-aged men. They observed that for every 40-g/d increment in whole-grain intake from all foods, weight gain was reduced by 0.49 kg. Consistent with the present study, Koh-Banerjee et al (24) observed that the associations observed were independent of both added bran or fiber intakes. Furthermore, other aspects of a healthy lifestyle, such as higher fruit and vegetable intakes and lower dietary fat, did not appear to explain the observed relation between whole-grain intake and VAT.
The potential mechanism or mechanisms by which whole grain may be related to regional adiposity are speculative. Whole grains are rich in fermentable carbohydrates such as dietary fiber, resistant starch, and oligosaccharides (6). A recent double-blind, randomized, crossover study (25) observed that daily consumption of a whole-grain wheat breakfast cereal exerted a pronounced prebiotic effect on the human gut microbiota composition in healthy adults. In the US diet, wheat is the predominant contributor of oligofructose, a nondigestible soluble fiber with prebiotic properties (26). Studies in animal models have observed that oligofructose feeding was associated with lower epididymal fat mass (an index of intraabdominal fat in rats) regardless of changes in body weight (27). These effects on fat mass development appear to be through the promotion of intestinal synthesis and portal release of glucagon-like peptide 1 (GLP-1) amide, a satiety hormone. In humans, however, it is not known if whole grains may influence body fat distribution through an effect on gut incretin hormones. Dietary fiber affects hunger and satiety by delaying gastric emptying, whereas other attributes of whole grain, such as dietary magnesium or particle size of whole-grain foods, may enhance insulin sensitivity and thereby prevent body fat accumulation.
It is important to recognize the limitations of this study. First, the cross-sectional and observational nature limits our ability to infer causality between diet and volumes of SAT and VAT. Second, the study participants and findings of this study may not be representative of the general population, because the majority was white. In addition, as a consequence of the prespecified exclusion criteria of the original study (7), our study lacks generalizability to younger adults. Third, although the apparent protective association with whole-grain intake persisted after adjustment for lifestyle and dietary factors associated with a healthier lifestyle, we cannot rule out residual confounding. Fourth, misclassification of dietary exposures is always a potential limitation of observational studies. The assumption is that certain foods, such as pasta and crackers, are largely made from refined flour. However, given the increasing availability of whole grain in the marketplace, it is possible that study participants are eating a whole-grain variety. Such misclassification would tend to bias our findings toward the null. Yet, we observed that higher refined-grain intake remains positively associated with VAT. The strengths of the present study include use of a highly reproducible volumetric method of SAT and VAT. In addition, we have a large sample with adequate power to detect potentially smaller but significant relations between diet, VAT, and SAT. Our findings extend the current literature on the relation between whole grain and body composition in adults with a comprehensive assessment of visceral abdominal fat, which cannot be assessed with DXA.
The current 2005 Dietary Guidelines for Americans recommends that Americans “consume 3 or more ounce equivalents of whole-grain products per day, with the rest of the recommended grains coming from enriched or whole-grain products” and that “in general at least half the grains should come from whole grains” (5). In our study, individuals who consumed whole-grain foods had lower VAT compared with nonconsumers; however, this benefit was not observed among those consuming more refined grains. These findings may suggest that if individuals are already consuming several daily servings of refined grains, the inclusion of whole grains in the diet may not translate into lower abdominal adiposity. Consequently, emphasis needs to be placed on the substitution of refined grains with whole grains rather than addition of whole grains to a diet already high in refined grains. To achieve this, greater education is needed for the public to understand clearly the term whole grain, what constitutes a serving, and the health benefits associated with substituting refined-grain with whole-grain foods. There is a need for both prospective and dietary intervention studies before any firm conclusions can be drawn with regard to the influence of different types of grains and body fat depots.
In conclusion, adults who consume ≥3 servings whole grains/d have significantly lower SAT and VAT compared with those who rarely consume whole-grain foods, but this beneficial association may be negated by higher refined-grain intake. Further research is required to elicit the potential mechanisms whereby whole- and refined-grain foods may influence body fat distribution.
Supplementary Material
Acknowledgments
We thank Enju Liu for initial statistical analysis on this project and Gail Rogers for reviewing the statistical code.
The authors' responsibilities were as follows—NMM, PFJ, and CSF: study concept and analysis design; CJO, UH, and CSF: acquisition of data; LMT: statistical analysis of data; NMM, LMT, PFJ, and CSF: interpretation of data; NMM: drafting of manuscript; and PFJ and CSF: critical revision of the manuscript for important intellectual content. The funders of this research played no role in the design, implementation, analysis, or interpretation of the data. None of the authors had a conflict of interest.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295:1549–55 [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood) 2009;28:w822–31 [DOI] [PubMed] [Google Scholar]
- 3.Harland JI, Garton LE. Whole-grain intake as a marker of healthy body weight and adiposity. Public Health Nutr 2008;11:554–63 [DOI] [PubMed] [Google Scholar]
- 4.Liu S, Willett WC, Manson JE, Hu FB, Rosner B, Colditz G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr 2003;78:920–7 [DOI] [PubMed] [Google Scholar]
- 5.US Department of Agriculture, US Department of Health and Human Services Dietary guidelines for Americans. Washington, DC: US Government Printing Office, 2005 [Google Scholar]
- 6.Slavin J. Whole grains and human health. Nutr Res Rev 2004;17:99–110 [DOI] [PubMed] [Google Scholar]
- 7.Fox CS, Massaro JM, Hoffmann U, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 2007;116:39–48 [DOI] [PubMed] [Google Scholar]
- 8.Molenaar EA, Massaro JM, Jacques PF, et al. Association of lifestyle factors with abdominal subcutaneous and visceral adiposity: the Framingham Heart Study. Diabetes Care 2009;32:505–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study. Design and preliminary data. Prev Med 1975;4:518–25 [DOI] [PubMed] [Google Scholar]
- 10.Splansky GL, Corey D, Yang Q, et al. The Third Generation Cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol 2007;165:1328–35 [DOI] [PubMed] [Google Scholar]
- 11.Maurovich-Horvat P, Massaro J, Fox CS, Moselewski F, O'Donnell CJ, Hoffmann U. Comparison of anthropometric, area- and volume-based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi-detector computed tomography. Int J Obes (Lond) 2007;31:500–6 [DOI] [PubMed] [Google Scholar]
- 12.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 1992;135:1114–26, discussion 1127–36 [DOI] [PubMed] [Google Scholar]
- 13.Willett WC, Reynolds RD, Cottrell-Hoehner S, Sampson L, Browne ML. Validation of a semi-quantitative food frequency questionnaire: comparison with a 1-year diet record. J Am Diet Assoc 1987;87:43–7 [PubMed] [Google Scholar]
- 14.Salvini S, Hunter DJ, Sampson L, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 1989;18:858–67 [DOI] [PubMed] [Google Scholar]
- 15.Jacobs DR, Jr, Meyer KA, Kushi LH, Folsom AR. Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: the Iowa Women's Health Study. Am J Clin Nutr 1998;68:248–57 [DOI] [PubMed] [Google Scholar]
- 16.Desprès J. Visceral obesity and dyslipidemia: contribution of insulin resistance and genetic susceptibility. : Angel A AH, Bouchard C, Lau D, Leiter L, Mendelson R, Seventh International Congress on Obesity, Toronto, Canada. London, United Kingdom: John Libbey & Company, 1996:525–32 [Google Scholar]
- 17.McKeown NM, Meigs JB, Liu S, Saltzman E, Wilson PW, Jacques PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham Offspring Cohort. Diabetes Care 2004;27:538–46 [DOI] [PubMed] [Google Scholar]
- 18.Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 2002;287:2414–23 [DOI] [PubMed] [Google Scholar]
- 19.Davis JN, Alexander KE, Ventura EE, Toledo-Corral CM, Goran MI. Inverse relation between dietary fiber intake and visceral adiposity in overweight Latino youth. Am J Clin Nutr 2009;90:1160–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ventura E, Davis J, Byrd-Williams C, et al. Reduction in risk factors for type 2 diabetes mellitus in response to a low-sugar, high-fiber dietary intervention in overweight Latino adolescents. Arch Pediatr Adolesc Med 2009;163:320–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis JN, Kelly LA, Lane CJ, et al. Randomized control trial to improve adiposity and insulin resistance in overweight Latino adolescents. Obesity (Silver Spring) 2009;17:1542–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katcher HI, Legro RS, Kunselman AR, et al. The effects of a whole grain-enriched hypocaloric diet on cardiovascular disease risk factors in men and women with metabolic syndrome. Am J Clin Nutr 2008;87:79–90 [DOI] [PubMed] [Google Scholar]
- 23.Saltzman E, Moriguti JC, Das SK, et al. Effects of a cereal rich in soluble fiber on body composition and dietary compliance during consumption of a hypocaloric diet. J Am Coll Nutr 2001;20:50–7 [DOI] [PubMed] [Google Scholar]
- 24.Koh-Banerjee P, Franz M, Sampson L, et al. Changes in whole-grain, bran, and cereal fiber consumption in relation to 8-y weight gain among men. Am J Clin Nutr 2004;80:1237–45 [DOI] [PubMed] [Google Scholar]
- 25.Costabile A, Klinder A, Fava F, et al. Whole-grain wheat breakfast cereal has a prebiotic effect on the human gut microbiota: a double-blind, placebo-controlled, crossover study. Br J Nutr 2008;99:110–20 [DOI] [PubMed] [Google Scholar]
- 26.Moshfegh AJ, Friday JE, Goldman JP, Ahuja JK. Presence of inulin and oligofructose in the diets of Americans. J Nutr 1999;129:S1407–11 [DOI] [PubMed] [Google Scholar]
- 27.Delzenne NM, Cani PD, Neyrinck AM. Modulation of glucagon-like peptide 1 and energy metabolism by inulin and oligofructose: experimental data. J Nutr 2007;137: S2547–51 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.