Abstract
Reflux-induced injury promotes esophageal adenocarcinoma, one of the most rapidly increasing, highly lethal cancers in Western countries. Here we investigate the efficacy of a combinatorial chemoprevention strategy for esophageal adenocarcinoma and characterize the underlying molecular mechanisms. Specifically, our approach involves the use of Ursodeoxycholic acid (Urso) due to its ability to decrease injury-inducing bile salts in combination with Aspirin to mitigate the consequences of injury. We find that Urso-Aspirin combination reduces the risk of adenocarcinoma in-vivo in animals with reflux, decreases the proliferation of esophageal adenocarcinoma cells and down-regulates a key cell cycle regulator, CDK2. Mechanistically, using cell growth, luciferase-reporter, expression and ChIP assays, we identify GLI1, a Hedgehog-regulated transcription factor, as a novel target of Urso-Aspirin combination. We demonstrate that GLI1 is upregulated during esophageal carcinogenesis and GLI1 can bind to the CDK2 promoter and activate its expression. While the Urso-Aspirin combination downregulates GLI1, the GLI1 overexpression not only abrogates the effect of this combination on proliferation but it also restores CDK-2 expression. These findings support that the chemopreventive effect of the Urso-Aspirin combination occurs, at least in part, via a novel GLI1-CDK2-dependent mechanism. To further understand the regulation of CDK2 by GLI1, both pharmacologic and RNAi-mediated approaches demonstrate that GLI1 is a transcriptional activator of CDK2 and this regulation occurs independent of Smoothened, the central transducer of the Hedgehog canonical pathway. Collectively, these results identify a novel GLI1-to-CDK2 pathway in esophageal carcinogenesis, which is a bona fide target for effective combinatorial chemoprevention with Urso and Aspirin.
Keywords: GLI1, Hedgehog signaling, Chemoprevention, Barrett’s esophagus, Esophageal Cancer
INTRODUCTION
Chronic injury and inflammation play a central role in several gastrointestinal cancers including Barrett’s-associated esophageal adenocarcinoma, a highly lethal and rapidly increasing cancer (1) (2–4). It is well-recognized that chronic injury induces an inflammatory response and activates pro-carcinogenic pathways in injured tissue (1–3, 5, 6). Although combinatorial approaches have been successfully used in HIV, tuberculosis and are proposed in carcinogenesis(7–9), the usual approach in cancer prevention involves targeting either the cause of injury or its consequences (2, 10, 11). We hypothesized that during carcinogenesis in Barrett’s esophagus, targeting both the cause (bile composition) and the consequence of injury (inflammation-associated pathways) will be an optimal chemoprevention strategy.
To address combinatorial chemoprevention in esophageal adenocarcinoma, we evaluated the effect of low-dose Aspirin and Urso on the development of this cancer. Interestingly, patients who use Urso for cholestatic liver disease are at lower risk of colon cancer (12). Although the effect of Urso in injury-induced carcinogenesis remains unknown, it does lower the levels of bile salts that are strongly implicated as the cause of injury and carcinogenesis in Barrett's esophagus (13). The rationale to combine Urso with Aspirin was that patients who chronically use anti-inflammatory drugs including Aspirin are less likely to be diagnosed with esophageal adenocarcinoma (14). While there is no in-vivo experimental evidence that Aspirin by targeting the effect of injury could prevent esophageal adenocarcinoma, anti-inflammatory agents like COX-2 inhibitors have been shown to reduce the risk of this cancer in animals with reflux (15). We elected to use Aspirin over these anti-inflammatory agents because unlike COX-2 inhibitors, Aspirin does not increase the risk of cardiovascular mortality (16).
In this study, using a battery of in-vitro and in-vivo experiments, we demonstrate that combinatorial chemoprevention using low-dose Urso-Aspirin reduced the risk of reflux-induced esophageal adenocarcinoma, while these agents were not effective in preventing cancer when used individually. The key cellular mechanism involved in this chemopreventive effect is the inhibition of cell proliferation and that the molecular target of this combination is the downregulation of CDK2, an important cell cycle regulator. Interestingly, further steps to resolve the molecular mechanisms revealed that CDK2 is regulated at transcriptional level via a previously unknown GLI1-mediated mechanism. Typically, GLI1, a known effector molecule of the oncogenic Hedgehog pathway, exerts transcriptional regulation upon its activation by Smoothened receptor; however, here we demonstrate that CDK2 upregulation by GLI1 is Smoothened-independent. The importance of GLI1 in context of combinatorial chemoprevention is further supported by our findings that GLI1 is overexpressed during injury-induced carcinogenesis in Barrett's mucosa, and the Urso-Aspirin combination downregulates GLI1. Finally, we demonstrate that GLI1 overexpression not only relieves the CDK2 repression caused by the Urso-Aspirin combination but also abrogates the effect of this combination on cell proliferation. Therefore, these novel findings expand our knowledge of mechanisms involved in chemoprevention, a relatively under-appreciated field of research.
MATERIALS AND METHODS
Reagents and cell cultures
Unless specified, all reagents were from Sigma (St. Louis, MO). BAR-T (Dr. Jerry Shay, UT Southwestern, Dallas, TX), CPC-A and CPC-C (Dr. P. Rabinovitch, U of Washington, Seattle, WA) cells were maintained in Barrett’s Plus media (17–19). Human Barrett’s-associated adenocarcinoma cell lines, SKGT4 and FLO-1(Dr. David Schrump, NCI, Bethesda, MD and Dr. David Beer, UMich, Ann Arbor, MI) were maintained in DMEM (Gibco) with 1%–10% FBS. Cell lines were authenticated with short tandem repeat (STR) and DNA fingerprinting within the last 6 months.
Rat Model of Barrett’s Esophagus, Interventions, and Monitoring
Esophagojejunostomy was performed on 100 rats to cause reflux injury, Barrett’s esophagus and adenocarcinoma (15). The Mayo Clinic IACUC approved this animal study. Eight week post-operatively, 86 surviving rats were kept in individual cages and randomized (2:2:2:3) to a diet containing 1% Urso (n=19), 0.3% Aspirin (n=19), 1% Urso+0.15% Aspirin (n=19) or control (n=29). The dose selection was based upon the available literature as well as Barrett’s mucosal tissue from 40 patients who received 80 to 325 mg of Aspirin daily for 3 months. The published range for Aspirin dose was 0.03 to 1.2%. We elected to use 0.15% Aspirin as we found that a dietary supplement of 0.1 to 0.2% Aspirin could achieve similar effect on biochemical and molecular markers of injury and inflammation as was achieved by 80 to 325 mg of Aspirin in patients with Barrett’s esophagus. The published doses of Urso range from 0.1% to 1% and we found that 1% Urso supplementation resulted in similar bile salt profile as we have noted in Barrett’s esophagus patients who received 250 mg Urso three times a day for three months (20) (21–23). Animals were euthanized eight months after randomization for evaluation of endpoints as outlined below. Autopsy was performed as we have previously described (15).
Cell Proliferation and apoptosis
Proliferation was assessed by Bromodeoxyuridine (BrdU) and apoptosis was detected using Annexin-5 positive cell on immunostaining using fluorescence microscope (19). MTS assay for metabolically active, viable cells and morphologic features of apoptosis via Hoechst staining were also examined. All experiments were repeated three times in triplicates
RNA Extraction and Reverse Transcription-PCR
Total RNA isolated from patient samples, rat tissue, and cell lines (using Trizol reagent, Invitrogen) were purified with RNeasy columns (Qiagen). Using OneStep RT-PCR kit (Qiagen), with primers specific for GLI1 and CDK1, PCR was performed (primers and conditions available upon request). The amplified products were analyzed on a 2% agarose gel.
Luciferase Reporter Assays
Approximately 60% confluent cells in six-well plates were incubated with 1 ml serum-free OptiMEM (Invitrogen) containing 12 µl of LipofectAMINE (Invitrogen) and 1.2 µg of DNA. After 6 hours, media was replaced with DMEM containing 10% FBS. Luciferase activities were measured using the Dual-Luciferase Reporter assay (Promega) and normalized by protein quantification. Each data point represents an average of three independent transfections (24).
Chromatin Immunoprecipitation Assay (ChIP)
Cells were transfected with GLI1 or parental vector. Samples were immunoprecipitated using a GLI antibody (R&D Systems) (25). Immunoprecipitated DNA was amplified by PCR using primer sets for the 4 areas containing GLI biding sites in CDK2 promoter sequence (Please see supplemental file for primers).
Plasmids Constructs
The CDK2 promoter-Luciferase reporter (8×GLI) was kindly provided by Dr. van Wijnen (University of Massachusetts, Worcester, MA). The GLI reporter expression constructs were kindly provided by Dr. Chi-chung Hui (Research Institute, Toronto, Ontario, Canada). The cDNA for GLI1 was cloned in pCMV-Tag2B vector (Stratagene, Santa Clara, CA) and shRNA were designed and cloned into pFRT vector (Invitrogen) using standard recombinant DNA methodology as previously described (the targeted sequences are in the supplemental file) (24).
Statistical methods
The statistical analyses were performed using the SAS software. All tests were two-sided, and a p-value of <0.05 was considered statistically significance (Bonferroni adjustments were made when indicated). The Student’s t-tests (or when appropriate, the Wilcoxan rank-sum tests) were used to compare the groups. All experiments performed in triplicate were repeated at least three times.
RESULTS
Urso-Aspirin combination decreases the rate of esophageal adenocarcinoma in-vivo and inhibits Barrett’s epithelial cell proliferation
To test the hypothesis that targeting both the cause and consequence of chronic reflux injury will be an optimal chemoprevention strategy during carcinogenesis in Barrett’s esophagus we used Urso, and Aspirin, in an established animal model. We found that, the incidence of esophageal adenocarcinoma was significantly lower in animals treated with Urso-Aspirin compared to controls (p<0.05, FIGURE 1A). In the combination group, 26% animals (5/19) developed esophageal cancer, while 62% (18/29) developed cancer in the control group (an absolute risk reduction of 58%, with 95%CI, 45–69%). There was no significant difference in risk of esophageal adenocarcinoma between the Urso-alone treated group (8/19, p=0.28) or Aspirin-alone treated group (9/19, p=0.48), compared to the control group.
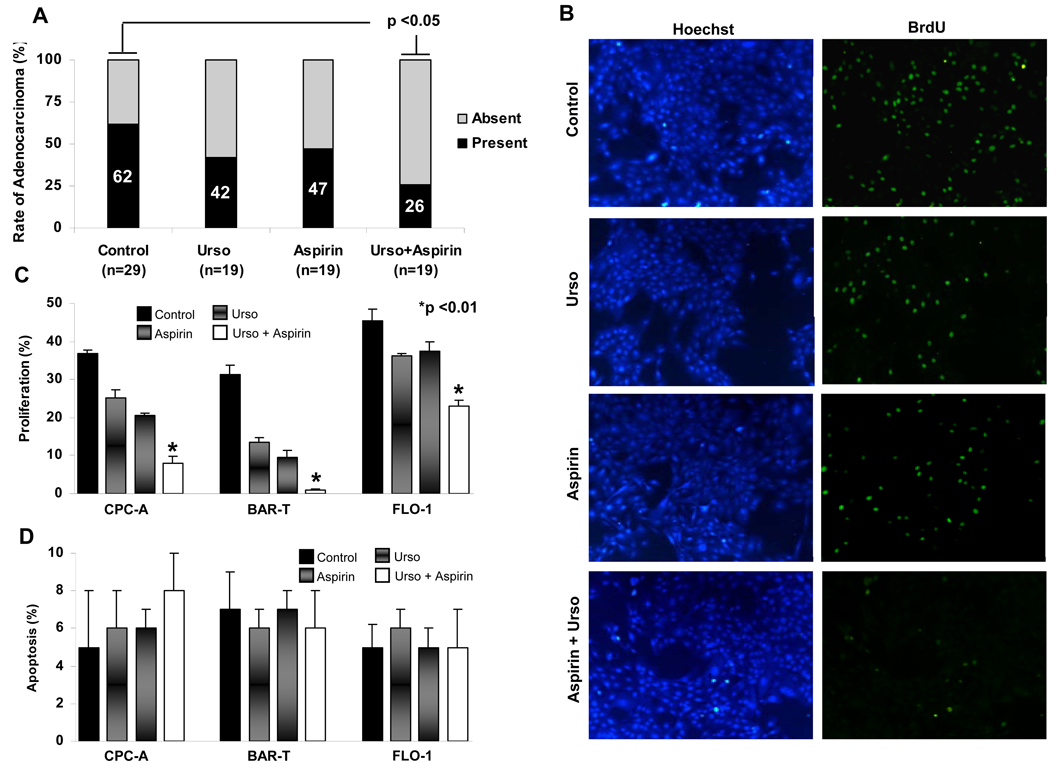
Figure 1. Combination treatment with Urso and Aspirin reduces tumor incidence in-vivo and inhibits cell proliferation in-vitro.
A, The esophageal cancer risk reduction was noted only when Urso and Aspirin were combined (p<0.05, compared to control). B, At 48 hours, compared to control, BAR-T cell proliferation was reduced by 91±6.7% with Urso-Aspirin (150 Urso and 1.5 mmol/L Aspirin), 42±3.3% with Urso-alone (150µmol/L) and 44±4.2% with Aspirin-alone (1.5 mmol/L). The Urso-Aspirin combination treatment had more robust inhibition of proliferation compared to either Urso or Aspirin alone (P<0.05) C and D, A 48-hour treatment with Urso-Aspirin (150 Urso and 1.5 mmol/L Aspirin) significantly decreased (p<0.01, compared to control) the BrdU positive cells in CPC-A by 77±19.9%, BAR-T by 97±55%, and FLO-1 cells by 51±3.02%, however compared to control the rate of apoptosis (Annexin-5 and Hoechst staining) was not different in CPC-A (5±3 vs. 8±2.1%), BAR-T (7±2 vs. 6±1%), or FLO-1 cells (5±1.2% vs. 6±2%).
To examine the cellular processes by which Urso-Aspirin combination exerts this tumor inhibitory effect, pre-malignant BAR-T cells were treated for 48 hours with either 150 µmol/L Urso, 1.5 mmol/L Aspirin, or 150 µmol/L Urso+1.5 mmol/L Aspirin. Urso-Aspirin combination resulted in a robust reduction in proliferation (91±6.7% reduction compared to control, p<0.01), which was significantly enhanced over Urso-alone (42±3.3% reduction) or Aspirin-alone (44±4.2% reduction; p<0.01). To further confirm this finding, premalignant (CPC-A, BAR-T) and malignant (FLO-1) esophageal epithelial cell lines, were treated with either 150 µmol/L Urso + 1.5 mmol/L Aspirin or vehicle. At 48 hours, the Urso-Aspirin combination decreased BrdU positive cells in CPC-A by 77±19.9%, BAR-T by 97±55%, and FLO-1 cells by 51±3.02% compared to control (FIGURE 1B and C, p<0.05). However, the proportion of cells undergoing apoptosis with Urso-Aspirin were not different compared to vehicle-treated cells (FIGURE 1D). Together, these findings demonstrate that Urso-Aspirin is effective in preventing Barrett’s-associated neoplasia and the cellular process that it targets is proliferation (not apoptosis). While both Aspirin and Urso can target distinct regulatory proteins that are involved in the cell cycle (26, 27), the mechanism underlying down-regulation of proliferation by their combination remains unknown.
Urso-Aspirin combination down-regulates CDK2, an important cell cycle regulator, both in-vitro and in-vivo in Barrett’s esophagus
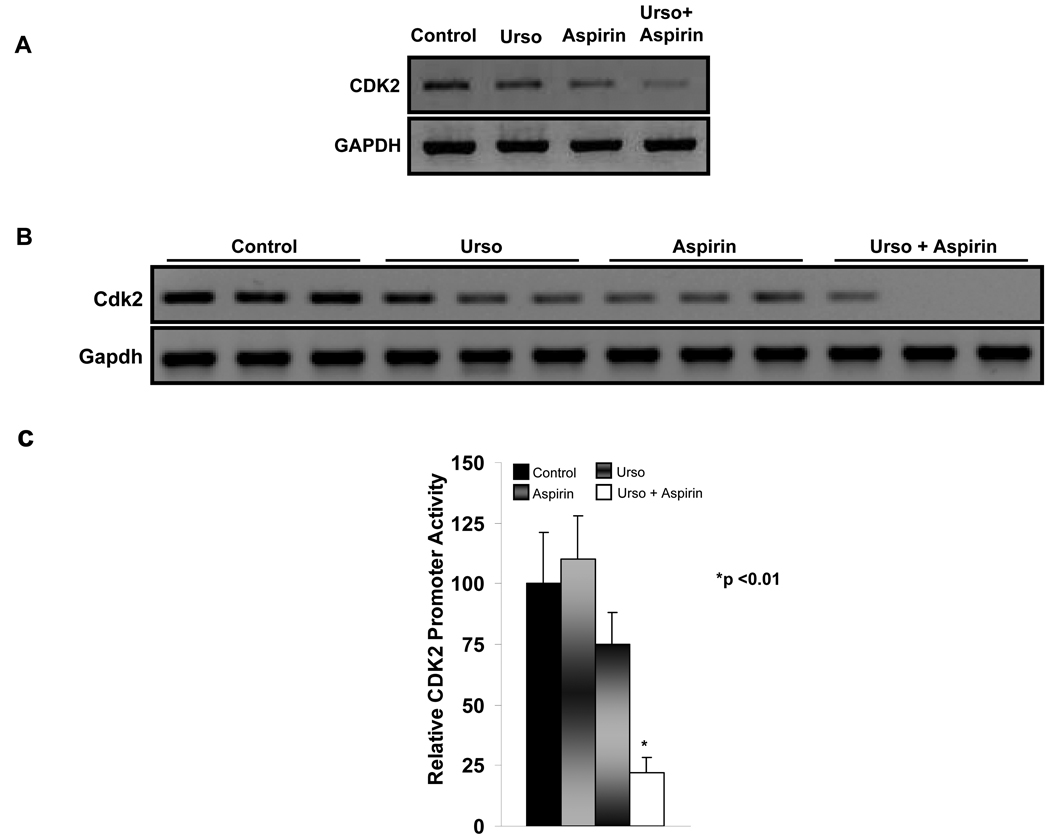
Having determined the efficacy of Urso-Aspirin in preventing esophageal adenocarcinoma, to identify molecular targets of this combination we conducted a pathway-specific gene expression profile. As Urso-Aspirin down-regulated proliferation in Barrett’s epithelium, it was interesting to find cell cycle regulator, CDK2, as a promising target from this profiling (28). We therefore examined CDK2 expression in esophageal cell lines treated with the Urso-Aspirin and found that this combination downregulated CDK2 expression (FIGURE 2A). These results were further confirmed in-vivo where animals treated with Urso-Aspirin showed a reduction in Cdk2 expression in Barrett’s mucosa compared to controls (FIGURE 2B). To determine whether the effect of Urso-Aspirin on CDK2 expression occurs at the transcriptional level, FLO-1 cells were initially transfected with CDK2 promoter-luciferase reporter constructs; Twenty-four hours post-transfection, cells were further treated with Urso-Aspirin for 24 hours. The protein normalized luciferase activity showed that Urso-Aspirin caused a four-fold reduction in CDK2 promoter activity compared to control (100±20 vs. 22.2±6, p<0.01 FIGURE 2C). These results provide evidence, for the first time, that CDK2, a cell cycle regulator known to play an important role in proliferation, is a target of Urso-Aspirin and can be regulated at the transcriptional level by this combination. These novel findings led us to further examine CDK2 regulation in context of combinatorial chemoprevention in Barrett’s esophagus.
Figure 2. Urso-Aspirin combination decreases CDK2 expression and promoter activity both in-vitro and in-vivo in Barrett’s esophagus.
A, RT-PCR showed that FLO-1 cells treated with Urso-Aspirin combination (150 µmol/L + 1.5 mmol/L) for 24 hours had a marked reduction in CDK2 expression compared to control cells as well as cells treated with either Urso or Aspirin alone. B, A similar reduction in Cdk2 expression is seen in esophageal tissue derived from rats receiving the combination therapy but not when these agents were used individually. C, FLO-1 cells transfected with CDK2 promoter-luciferase reporter constructs were treated 24 hours post-transfection with either vehicle, Urso, Aspirin or a combination of Urso-Aspirin (150 µmol/L + 1.5 mmol). 24 hours later, compared to control, the Urso-Aspirin combination markedly reduced CDK2 promoter activity (100±20 vs. 22.2±6, p<0.01).
Urso-Aspirin combination down-regulates CDK2 by antagonizing a GLI1 mediated, Smoothened independent mechanism in Barrett’s epithelial cells
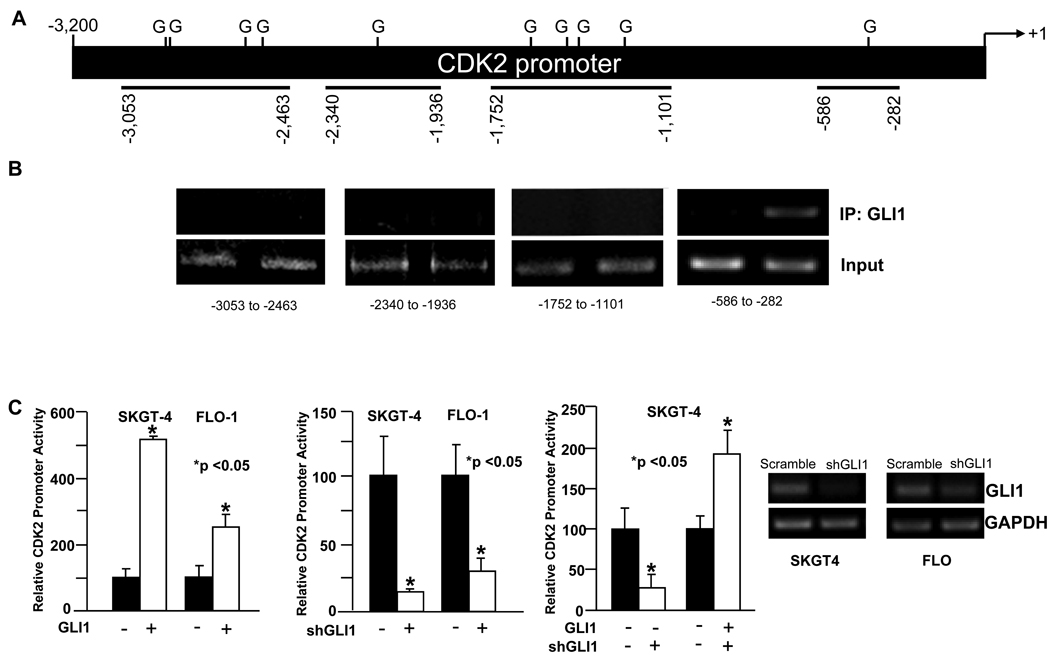
Since Urso-Aspirin down-regulated CDK2 expression and repressed its promoter activity, we next conducted bioinformatics sequence analysis of the CDK2 promoter using the TRANSFAC Public database along with the functional screening. We found GLI proteins, particularly GLI1, as promising candidate regulators of CDK2 promoter (FIGURE 3A). To confirm this prediction, we first examined whether GLI1 binds to endogenous CDK2 promoter. We transfected Barrett’s epithelial cells with either control vector or a GLI1 construct. Chromatin immunoprecipitation using a GLI1 antibody showed that CDK2 promoter sequence was enriched in cells transfected with GLI1 (FIGURE 3B) suggesting that GLI1 binds to the endogenous CDK2 promoter which is therefore a direct target of GLI1. To further solidify these findings and to determine functional relevance, we co-transfected Barrett’s epithelial cell lines with a CDK2 promoter-luciferase reporter construct along with either control vector or GLI1 expression constructs. At 48 hours, GLI1 transfected cells had up to five-fold increase in CDK2 promoter activity compared to control (FIGURE 3C), suggesting that not only did GLI1 bind the CDK2 promoter but also acted as a transcriptional activator of CDK2. To further substantiate these findings, esophageal cells were co-transfected with a CDK2 promoter-luciferase reporter construct along with either shRNA against GLI1 (shGLI1) or scrambled shRNA control. Congruent with the above data, the shGLI1 transfected cells had up to a five-fold reduction in CDK2 promoter activity when compared to control.
Figure 3. GLI1 binds to endogenous CDK2 promoter and activates CDK2 promoter.
A, Outline of CDK2 promoter with putative GLI binding site (marked as G). B, Chromatin immunoprecipitation assay show that GLI1 could directly binds to endogenous CDK2 promoter in the core promoter region. C, SKGT4, and FLO-1 cells were co-transfected with GLI1 and CDK2. In both cell lines, there was an increase in CDK2 activity in the GLI1 transfected cells when compared with control (p<0.05) and this increase is prevented by the transfection of shGLI1. The latter effect is rescued by overexpression of shRNA resistant GLI1 construct, which does not contain the 3’end of GLI1 mRNA that is the target of shRNA.
To determine if the decrease in the CDK2 promoter activity by shGLI1 could be relieved by GLI1 overexpression, we co-transfected esophageal cells with a CDK2 promoter reporter construct along with shGLI1 or scrambled shRNA together with a shRNA resistant GLI1 expression construct. We found that under these experimental conditions GLI1 restored CDK2 promoter activity (FIGURE 3C).
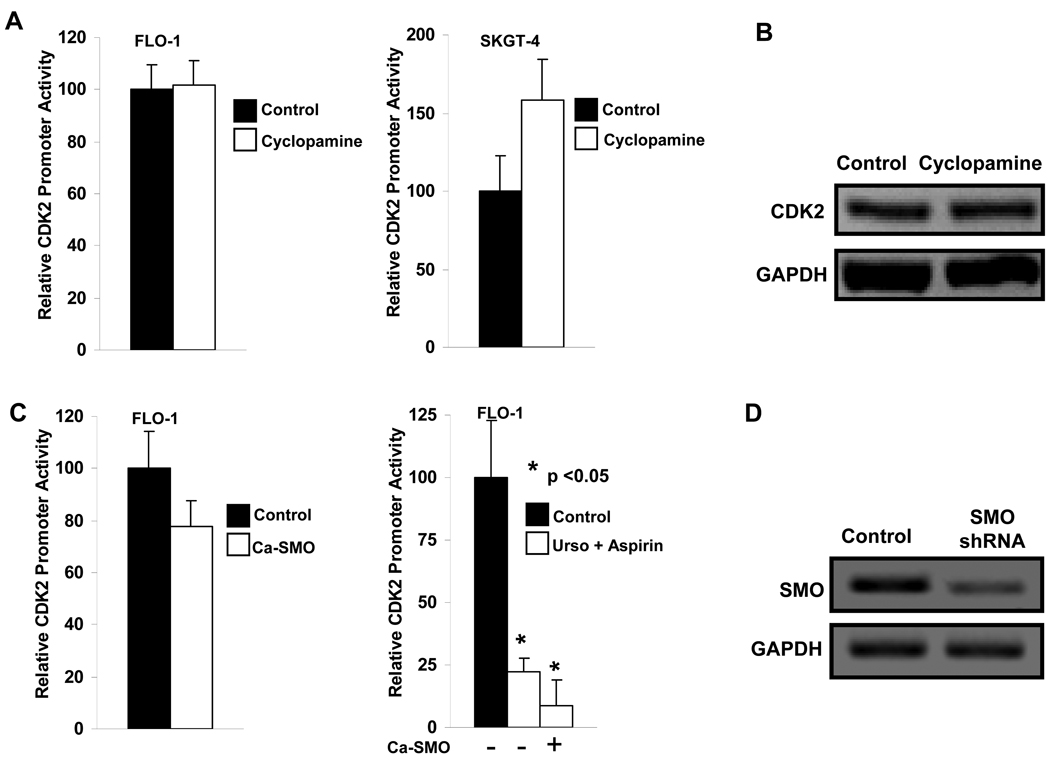
GLI1 is a downstream effector of the Hedgehog pathway (29). To determine the involvement of this cascade in the modulation CDK2 expression and promoter activity, esophageal cancer cell lines, FLO-1 and SKGT4, were transfected with CDK2 promoter-luciferase reporter constructs. At 24 hours, these cells were treated with either vehicle or cyclopamine (5 µM), which blocks Hedgehog pathway at the level of Smoothened, a central transducer of canonical Hedgehog pathway (30). Protein normalized luciferase activity showed that cyclopamine failed to decrease the CDK2 promoter activity compared to control, (FIGURE 4A). Moreover, there was no change in CDK2 expression with cyclopamine treatment (FIGURE 4B). The failure of cyclopamine to decrease CDK2 activity suggests that the GLI1-dependent increase in CDK2 activity occurs in a Smoothened independent manner (non-canonical) or suppression of GLI1 by cyclopamine is insufficient to block CDK2 expression. To confirm these pharmacological experiments, FLO-1 cells were co-transfected with CDK2 promoter-reporter with either empty vector or a constitutively active Smoothened (Ca-SMO) construct. At 48 hours, Smoothened transfected cells had no significant change in CDK2 promoter activity compared to empty vector (100±14 vs. 78.5±8.9, p>0.05, FIGURE 4C). These findings further support the observation that GLI1 dependent activation of CDK2 promoter is Smoothened independent. Finally, FLO-1 cells were co-transfected with CDK2 promoter reporter along with empty vector or Ca-SMO. The next day, cells were treated with either vehicle or Urso-Aspirin. Twenty-four hours later, as anticipated, compared to control, Urso-Aspirin combination reduced CDK2 promoter activity by 78% (100±21.7 vs. 21.74±4, p<0.05) and Ca-SMO failed to rescue the CDK2 promoter inhibition by the chemoprevention combination (FIGURE 4C right panel). Together, these findings show that Urso-Aspirin combinatorial therapy downregulated CDK2 via a GLI1 mediated, Smoothened independent mechanism.
Figure 4. GLI1 regulates CDK2 promoter in Barrett’s epithelial cells and this GLI activity is independent of upstream canonical Hedgehog pathway.
A. FLO-1 and SKGT4 transfected with CDK2 promoter-reporter constructs were treated with either vehicle or cyclopamine (5 µM to inhibit smoothened in the canonical Hedgehog pathway). Compared to control, cyclopamine treated cells did not show any change in CDK2 promoter activity. B. FLO-1 and SKGT4 were treated with either vehicle or cyclopamine (5 µM) and up to 24 hours, compared to control, no changes in CDK2 expression were noted with Cyclopamine treatment. C. FLO-1 cells were cotransfected with CDK2 promoter reporter along with either empty vector or constitutively active Smoothened construct (Ca-SMO) for 48 hours. Compared to empty vector, Ca-SMO transfected cells had no significant change in CDK2 promoter activity (100±14 vs. 78.5±8.9, p>0.05). D FLO-1 cells co-transfected with CDK2 promoter reporter along with empty vector or Ca-SMO construct. Twenty-four hours after later cells were treated either with vehicle or Urso-Aspirin. Compared to control, Urso-Aspirin reduced CDK2 promoter activity by 78% (100±21.7 vs. 21.74±4, p<0.05). A similar repression of CDK2 promoter activity was also noted in the cells that were co-transfected with Ca-SMO (100±21.7 vs. 10.5±8, p<0.050) suggesting that Ca-SMO failed to release the CDK2 promoter inhibition by Urso-Aspirin combination.
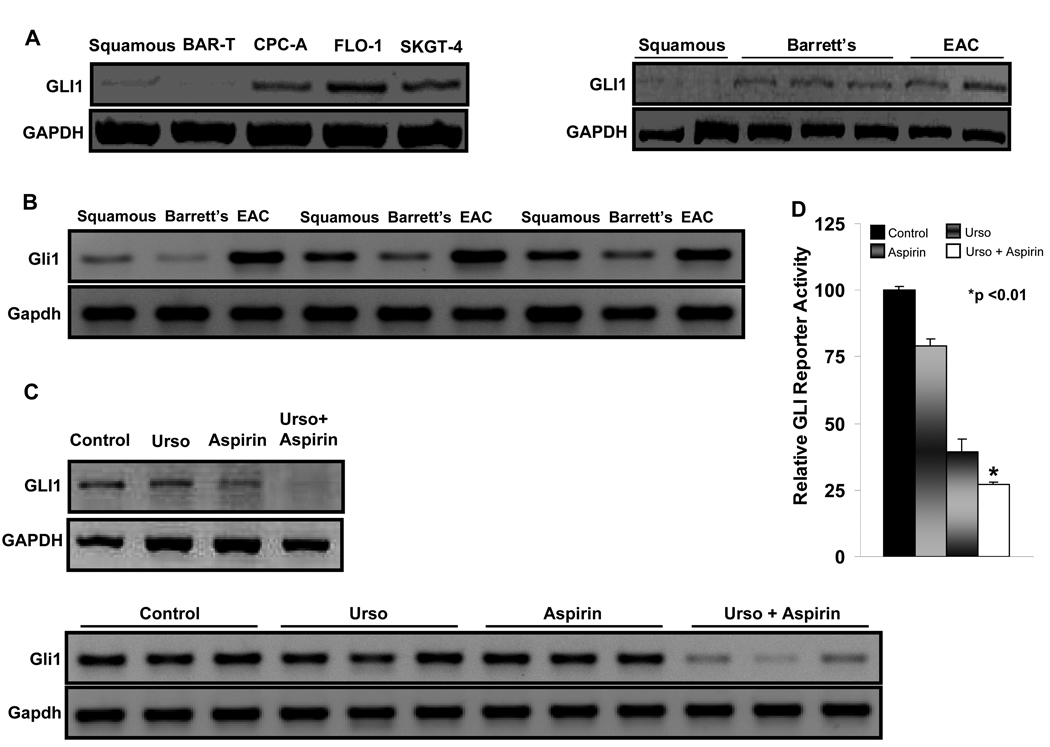
GLI1 is over-expressed during carcinogenesis in Barrett’s esophagus and can be down regulated by Urso-Aspirin
To determine translational relevance of GLI1 to carcinogenesis in Barrett’s esophagus, its expression was examined in vitro in cell lines, biopsy samples from Barrett’s esophagus patients and animal tissue. The esophageal adenocarcinoma (FLO-1 and SKGT4) cell lines had a higher GLI1 mRNA expression by RT-PCR compared to the normal squamous and Barrett’s cell lines (BAR-T and CPC-A). We also noted increased GLI1 expression in patients with adenocarcinoma compared to squamous, and Barrett’s tissue (FIGURE 5A). Corroborating these findings, we examined Gli1 expression in rat esophageal tissue and found that there was increased Gli1 expression in esophageal adenocarcinoma compared to Barrett’s and normal squamous samples (FIGURE 5B). To apply our understanding of the role of GLI1 in the context of the chemopreventive effect of Urso-Aspirin, FLO-1 cells were treated with either control or Urso-Aspirin for 48 hours. Compared to control, Urso-Aspirin significantly reduced GLI1 expression (FIGURE 5C). In agreement with this data, when Gli1 expression was examined in vivo, there was marked reduction in Gli1 expression in animals that received the Urso-Aspirin compared to animals that received the control diet (FIGURE 5C). Finally, to investigate if Urso-Aspirin dependent decrease in GLI1 expression has an impact on its transcriptional activity, FLO-1 cells were transfected with GLI-luciferase reporter construct that had 8 consecutive GLI binding sites (8×GLI) and 24 hours later they were further treated with either control or Urso-Aspirin for 24 hours. Luciferase activity showed that Urso-Aspirin caused a 59±8% reduction in the GLI-luciferase reporter activity compared to control, (p<0.01) (FIGURE 5D). These findings indicate that GLI1 is relevant to chronic injury associated carcinogenesis in Barrett’s esophagus and can be down-regulated by Urso-Aspirin.
Figure 5. GLI1 Expression increases during carcinogenesis in Barrett’s esophagus and can be targeted by the Urso-Aspirin combination.
A, GLI1 expression increased progressively from esophageal squamous to adenocarcinoma cell lines (left panel). RT-PCR revealed a progressive increase in GLI1 expression from squamous to cancer in patient samples (right panel). B, RNA was extracted from squamous, Barrett’s and adenocarcinoma rat samples from control diet group and RT-PCR revealed that Gli1 expression was increased from Barrett’s to cancer in rat. C, Esophageal cell line (FLO-1) treated with control or Urso, Aspirin or Urso+Aspirin (150 µmol/L+1.5 mmol/L) for 24 hours. RT-PCR revealed a decrease in GLI 1 expression in the cells treated with the Urso-Aspirin. RT-PCR performed on RNA extracted from rat esophageal tissue showed a similar decrease in Gli1 expression in the combination treated group compared to control or when these agents were used individually. D, FLO-1 cells transfected with GLI reporter to measure GLI activity were treated either with vehicle, Urso, Aspirin or Urso-Aspirin (150 µmol/L+1.5 mmol/L) for 24 hours. The combination treatment significantly decreased GLI activity in FLO-1 cells compared to control treatment (p<0.01).
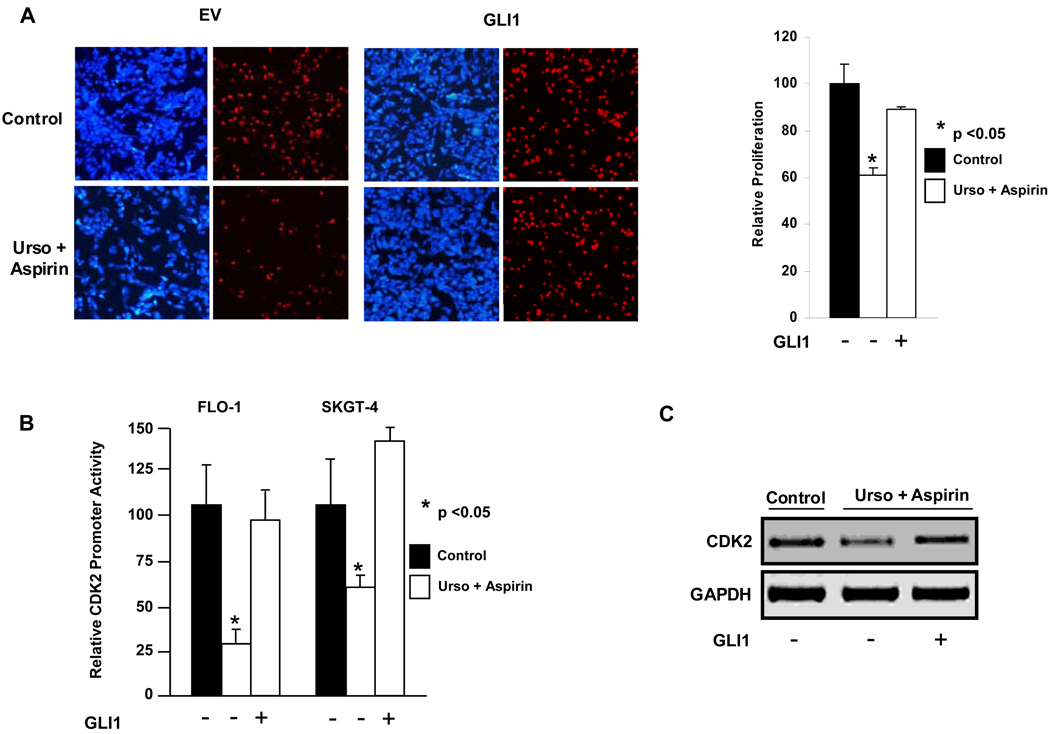
GLI1 overexpression antagonizes the chemopreventive effect of Urso-Aspirin combination on cell proliferation and restores CDK2 expression
Having established that GLI1 expression increases during esophageal carcinogenesis and Urso-Aspirin decreases GLI1 expression, we next examined whether the effect of Urso-Aspirin on cell proliferation and CDK2 is GLI1 dependent. To address this, FLO-1 cells were treated for 48 hours with either Urso-Aspirin or control. As expected, the combination decreased the proliferation of FLO-1 cells by 39% (p<0.05). However, in FLO-1 cells that were transfected with GLI1 prior to treatment with Urso-Aspirin, there was no significant reduction in proliferation compared to control (11%, p=0.54) (FIGURE 6A). After confirming that the effect of Urso-Aspirin on cell proliferation can be abrogated by GLI1 overexpression, we investigated whether GLI1 overexpression could also reverse Urso-Aspirin dependent down-regulation of CDK2 promoter activity. FLO-1 cells were co-transfected with CDK2 promoter-luciferase reporter constructs along with either GLI1 constructs or control vector for 24 hours. These cells were treated with either Urso-Aspirin or control for 24 hours. A 70% reduction in CDK2 promoter-Luciferase activity was noted in Urso-Aspirin only treated cells (p< 0.05), which was abrogated in GLI1 transfected cells (FIGURE 6B). To complement this finding, we investigated whether the effect of Urso-Aspirin on CDK2 expression was also GLI1 dependent. FLO-1 cells were transfected with either GLI1 or control vector and 24 hours later they were treated with either Urso-Aspirin or control. Whereas the combination caused a downregulation of CDK2 expression in the control vector transfected cells, it failed to do so in the GLI1 transfected cells (FIGURE 6C). Together, these findings demonstrate that the effect of Urso-Aspirin on cell proliferation and CDK2 expression occurs at least in part via GLI1 inhibition. These findings, along with prevention of esophageal cancer, inhibition of Barrett’s epithelial cell proliferation as well as down-regulation of CDK2 by Urso-Aspirin, support the observation that GLI inhibition is mechanistically linked to the prevention of neoplastic transformation by the Urso-Aspirin.
Figure 6. GLI1 overexpression antagonizes the effect of Urso-Aspirin combination on cell proliferation and CDK2 expression.
A, FLO-1 cells treated with the Urso-Aspirin combination had a significant reduction (p<0.05) in proliferation compared to control. This effect of Urso-Aspirin combination on proliferation of FLO-1 cells was reversed when the cells were transfected with GLI1 prior to treatment with the combination (p=0.54). B, FLO-1 cells treated with the combination treatment showed a decrease in CDK2 expression. When these cells were transfected with GLI1 and then subsequently treated with the combination treatment, the effect of Urso-Aspirin on CDK2 expression was abrogated.
DISCUSSION
A wealth of experimental and epidemiological evidence has established the importance of chronic injury-inflammation in carcinogenesis (1–3, 15). Given the epidemiological evidence that patients who use anti-inflammatory agents are at lower risk of developing several cancers (14, 31–34), anti-inflammatory agents have been widely investigated and found to have tumor suppressive effect both in-vivo and in-vitro (1, 35). This approach to target the effect of injury, while important, is usually not sufficient in preventing carcinogenesis, possibly because it does not take into account the cause of injury. This notion, along with the evolving concept of combinatorial chemoprevention (36, 37), led us to hypothesize that targeting both the cause and effect of chronic injury will lead to better control of carcinogenesis. We examined the injury-induced carcinogenesis in Barrett’s esophagus to address the effectiveness of the combinatorial chemoprevention approach and to examine the underlying mechanisms. A long premalignant phase and the association of Barrett’s esophagus with a highly lethal adenocarcinoma, makes it an important disease to examine chemoprevention strategy (2) (10). Moreover, the contents of reflux, particularly primary and secondary bile salts, that are implicated in chronic injury during carcinogenesis in Barrett’s esophagus (2) can be modified by the tertiary bile salt, Urso (13). Therefore, carcinogenesis in Barrett’s esophagus provides a distinct opportunity to test a combinatorial chemoprevention strategy that involves the modification of bile salts along with the use of anti-inflammatory agents, which minimize the consequence of injury.
Using low-dose Urso to reduce the concentration of injury-inducing bile salts along with a low-dose Aspirin in Barrett’s esophagus, we found that this combination significantly reduced the rate of esophageal adenocarcinoma in animals with reflux injury. In contrast, when used individually, both Urso and Aspirin were not effective in reducing the rate of esophageal adenocarcinoma. Our in-vitro results show that Urso-Aspirin decreases Barrett’s epithelial cell proliferation, a key cellular process that is known to be associated with neoplastic progression in Barrett’s epithelial cells (38, 39). While there is epidemiological data supporting the chemopreventive potential of aspirin in Barrett’s esophagus and there is indirect evidence that Urso, by modifying the concentration of injury inducing bile salts, may help prevent esophageal adenocarcinoma (13, 14, 18, 31–33, 40), this is the first in-vitro and in-vivo experimental evidence to support that these agents, when used together, prevent esophageal adenocarcinoma.
To our knowledge, this study, for the first time, provides evidence that GLI1 is involved in reflux injury-induced carcinogenesis and that it is a key molecular target of combinatorial chemoprevention by Urso-Aspirin. GLI proteins are highly conserved (41) (42) proteins that are emerging as important transcriptional regulators of oncogenic pathways by regulating apoptosis and epithelium to mesenchyme transformation (43) (29, 44–47). In this study, we uncovered an additional mechanism that GLI proteins could use to promote carcinogenesis by demonstrating that GLI1 binds to CDK2 promoter, upregulates CDK2 transcription, increases CDK2 expression and induces cell proliferation. Furthermore, the translational relevance of this molecular mechanism, in the context of chemoprevention, is supported by several novel findings in this study. First, GLI1 is upregulated both in patients as well as in animals during injury-inflammation induced carcinogenesis. Second, Urso-Aspirin combination downregulates GLI1, represses CDK2, decreases proliferation and prevents cancer development. Finally, GLI1 overexpression can reverse the effect of Urso-Aspirin combination not only on CDK2 expression but also on proliferation. Together, these findings provide alternative mechanisms that GLI1 could use during oncogenesis and reveal the role of GLI1 in chemoprevention.
This study also provides an additional pharmacological option to inhibit emerging pro-oncogenic protein GLI1. It is well-accepted that the GLI1 activity can be upregulated either via canonical Hedgehog-Smoothened-dependent signaling or a less well-understood non-canonical pathway upon which several signaling pathways, including TGF-β or Ras, could converge (29). At present, cyclopamine is the only available FDA approved drug that inhibits GLI1 by targeting Smoothened in the canonical pathway (47) (48, 49). Our data, which demonstrates that Urso-Aspirin combination targets GLI1 in a smoothened-independent manner (likely through TGF-β and prostaglandin E2 mediated mechanisms, data not shown), provides an additional novel pharmacological approach to downregulate GLI1. Therefore, under the circumstances, where both canonical and non-canonical signaling up-regulate GLI1 during carcinogenesis, one can envision a combinatorial strategy involving cyclopamine to target the canonical pathway and Urso-Aspirin to inhibit the non-canonical pathway.
Since this was a proof of principal study, it was beyond the scope of this manuscript to test the efficacy of these agents at the lowest possible doses, however, it remains an important consideration for future animal or clinical study. As outlined in the method section, the doses selected in this study were within the published range and were further refined based upon the pharmacokinetic and/or molecular data available from patients who received Urso or Aspirin and will therefore be achievable in-vivo in patients. At this fixed, low-dose Urso-Aspirin combination, we did not encounter any side effects in animals. While both safety and the efficacy of this approach need to be investigated in patients with Barrett’s esophagus, we do not anticipate any serious side effects. Urso is well-tolerated by patients who take it up to 15 mg/kg/day on long-term basis and low-dose Aspirin is clinically safe given that the majority of Barrett’s patients take proton pump inhibitors, which can prevent gastrointestinal bleeding.
In conclusion, our study contributes several novel observations in the field of chemoprevention that, though discovered while studying carcinogenesis in Barrett’s esophagus, may find wider implications to other cancers.
Supplementary Material
Acknowledgments
This work is supported by the Mayo Foundation, Mayo Clinic Cancer Center, NIH grants CA110022-01 and DK076845-01 to N.S.B., and CA102701 and CA136526 to M.E.F.-Z.
Reference
- 1.Anderson LA, Johnston BT, Watson RG, et al. Nonsteroidal anti-inflammatory drugs and the esophageal inflammation-metaplasia-adenocarcinoma sequence. Cancer research. 2006;66:4975–4982. doi: 10.1158/0008-5472.CAN-05-4253. [DOI] [PubMed] [Google Scholar]
- 2.Buttar NS, Wang KK. Mechanisms of Disease: carcinogenesis in Barrett's esophagus. Nature Clinical Practice Gastroenterology & Hepatology. 2004;1:106–112. doi: 10.1038/ncpgasthep0057. [DOI] [PubMed] [Google Scholar]
- 3.Wild CP, Hardie LJ. Reflux, Barrett's oesophagus and adenocarcinoma: burning questions. Nature Reviews Cancer. 2003;3:676–684. doi: 10.1038/nrc1166. [DOI] [PubMed] [Google Scholar]
- 4.Rubin DT, Parekh N. Colorectal cancer in inflammatory bowel disease: molecular and clinical considerations. Current treatment options in gastroenterology. 2006;9:211–220. doi: 10.1007/s11938-006-0040-5. [DOI] [PubMed] [Google Scholar]
- 5.Onwuegbusi BA, Fitzgerald RC, Bajaj-Elliott M, Burnham WR, Farthing MJ. Distinct cytokine patterns in Barrett's oesophagus and associated adenocarcinoma: Evidence for a shift towards a Th-2 response. Gastroenterology. 2000;118:413. [Google Scholar]
- 6.Tselepis C, Perry I, Dawson C, et al. Tumour necrosis factor-alpha in Barrett's oesophagus: a potential novel mechanism of action. Oncogene. 2002;21:6071–6081. doi: 10.1038/sj.onc.1205731. [DOI] [PubMed] [Google Scholar]
- 7.Lauer GM, Walker BD. Hepatitis C virus infection. The New England journal of medicine. 2001;345:41–52. doi: 10.1056/NEJM200107053450107. [DOI] [PubMed] [Google Scholar]
- 8.Flexner C. HIV-protease inhibitors. The New England journal of medicine. 1998;338:1281–1292. doi: 10.1056/NEJM199804303381808. [DOI] [PubMed] [Google Scholar]
- 9.Small PM, Fujiwara PI. Management of tuberculosis in the United States. The New England journal of medicine. 2001;345:189–200. doi: 10.1056/NEJM200107193450307. [DOI] [PubMed] [Google Scholar]
- 10.Lagergren J, Bergstrom R, Lindgren A, Nyren O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. New England Journal of Medicine. 1999;340:825–831. doi: 10.1056/NEJM199903183401101. [DOI] [PubMed] [Google Scholar]
- 11.Ries LAG MD, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK. SEER Cancer Statistics Review, 1975–2005. Bethesda, MD: National Cancer Institute; 2008. [Google Scholar]
- 12.Pardi DS, Loftus EV, Jr, Kremers WK, Keach J, Lindor KD. Ursodeoxycholic acid as a chemopreventive agent in patients with ulcerative colitis and primary sclerosing cholangitis. Gastroenterology. 2003;124:889–893. doi: 10.1053/gast.2003.50156. [DOI] [PubMed] [Google Scholar]
- 13.Lindor KD. Ursodiol for primary sclerosing cholangitis. Mayo Primary Sclerosing Cholangitis-Ursodeoxycholic Acid Study Group . New England Journal of Medicine. 1997;336:691–695. doi: 10.1056/NEJM199703063361003. [DOI] [PubMed] [Google Scholar]
- 14.Farrow DC, Vaughan TL, Hansten PD, et al. Use of aspirin and other nonsteroidal anti-inflammatory drugs and risk of esophageal and gastric cancer. Cancer Epidemiology, Biomarkers & Prevention. 1998;7:97–102. [PubMed] [Google Scholar]
- 15.Buttar NS, Wang KK, Leontovich O, et al. Chemoprevention of esophageal adenocarcinoma by COX-2 inhibitors in an animal model of Barrett's esophagus. Gastroenterology. 2002;122:1101–1112. doi: 10.1053/gast.2002.32371. [see comment] [DOI] [PubMed] [Google Scholar]
- 16.Psaty BM, Furberg CD. COX-2 inhibitors--lessons in drug safety. The New England journal of medicine. 2005;352:1133–1135. doi: 10.1056/NEJMe058042. [DOI] [PubMed] [Google Scholar]
- 17.Hormi-Carver K, Zhang X, Zhang HY, et al. Unlike esophageal squamous cells, Barrett's epithelial cells resist apoptosis by activating the nuclear factor-kappaB pathway. Cancer research. 2009;69:672–677. doi: 10.1158/0008-5472.CAN-08-3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yen CJ, Izzo JG, Lee DF, et al. Bile acid exposure up-regulates tuberous sclerosis complex 1/mammalian target of rapamycin pathway in Barrett's-associated esophageal adenocarcinoma. Cancer research. 2008;68:2632–2640. doi: 10.1158/0008-5472.CAN-07-5460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buttar NS, Wang KK, Anderson MA, et al. The effect of selective cyclooxygenase-2 inhibition in Barrett's esophagus epithelium: an in vitro study. Journal of the National Cancer Institute. 2002;94:422–429. doi: 10.1093/jnci/94.6.422. [DOI] [PubMed] [Google Scholar]
- 20.Thun MJ, Henley SJ, Patrono C. Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. Journal of the National Cancer Institute. 2002;94:252–266. doi: 10.1093/jnci/94.4.252. [DOI] [PubMed] [Google Scholar]
- 21.Hess LM, Krutzsch MF, Guillen J, et al. Results of a phase I multiple-dose clinical study of ursodeoxycholic Acid. Cancer Epidemiol Biomarkers Prev. 2004;13:861–867. [PubMed] [Google Scholar]
- 22.Colombo C, Crosignani A, Assaisso M, et al. Ursodeoxycholic acid therapy in cystic fibrosis-associated liver disease: a dose-response study. Hepatology. 1992;16:924–930. doi: 10.1002/hep.1840160412. [DOI] [PubMed] [Google Scholar]
- 23.Nehra D, Howell P, Williams CP, Pye JK, Beynon J. Toxic bile acids in gastro-oesophageal reflux disease: influence of gastric acidity. Gut. 1999;44:598–602. doi: 10.1136/gut.44.5.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang JS, Moncrieffe MC, Kaczynski J, Ellenrieder V, Prendergast FG, Urrutia R. A conserved alpha-helical motif mediates the interaction of Sp1-like transcriptional repressors with the corepressor mSin3A. Molecular and cellular biology. 2001;21:5041–5049. doi: 10.1128/MCB.21.15.5041-5049.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernandez-Zapico ME, Mladek A, Ellenrieder V, Folch-Puy E, Miller L, Urrutia R. An mSin3A interaction domain links the transcriptional activity of KLF11 with its role in growth regulation. The EMBO journal. 2003;22:4748–4758. doi: 10.1093/emboj/cdg470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thoms HC, Dunlop MG, Stark LA. p38-mediated inactivation of cyclin D1/cyclin-dependent kinase 4 stimulates nucleolar translocation of RelA and apoptosis in colorectal cancer cells. Cancer research. 2007;67:1660–1669. doi: 10.1158/0008-5472.CAN-06-1038. [DOI] [PubMed] [Google Scholar]
- 27.Wali RK, Khare S, Tretiakova M, et al. Ursodeoxycholic acid and F(6)-D(3) inhibit aberrant crypt proliferation in the rat azoxymethane model of colon cancer: roles of cyclin D1 and E-cadherin. Cancer Epidemiol Biomarkers Prev. 2002;11:1653–1662. [PubMed] [Google Scholar]
- 28.Kastan MB. Cell cycle. Checking two steps. Nature. 2001;410:766–767. doi: 10.1038/35071218. [DOI] [PubMed] [Google Scholar]
- 29.Nolan-Stevaux O, Lau J, Truitt ML, et al. GLI1 is regulated through Smoothened-independent mechanisms in neoplastic pancreatic ducts and mediates PDAC cell survival and transformation. Genes & development. 2009;23:24–36. doi: 10.1101/gad.1753809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu FG, Ma QY, Wang Z. Blockade of hedgehog signaling pathway as a therapeutic strategy for pancreatic cancer. Cancer letters. 2009;283:119–124. doi: 10.1016/j.canlet.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 31.Smalley WE, DuBois RN. Colorectal cancer and nonsteroidal anti-inflammatory drugs. Advances in Pharmacology. 1997;39:1–20. doi: 10.1016/s1054-3589(08)60067-8. [DOI] [PubMed] [Google Scholar]
- 32.Fitzgerald RC. Review article: Barrett's oesophagus and associated adenocarcinoma--a UK perspective. Alimentary pharmacology & therapeutics. 2004;20:45–49. doi: 10.1111/j.1365-2036.2004.02229.x. [DOI] [PubMed] [Google Scholar]
- 33.Ulrich CM, Bigler J, Potter JD. Non-steroidal anti-inflammatory drugs for cancer prevention: promise, perils and pharmacogenetics. Nat Rev Cancer. 2006;6:130–140. doi: 10.1038/nrc1801. [DOI] [PubMed] [Google Scholar]
- 34.Gammon MD, Terry MB, Arber N, et al. Nonsteroidal anti-inflammatory drug use associated with reduced incidence of adenocarcinomas of the esophagus and gastric cardia that overexpress cyclin D1: a population-based study. Cancer Epidemiol Biomarkers Prev. 2004;13:34–39. doi: 10.1158/1055-9965.epi-03-0198. [DOI] [PubMed] [Google Scholar]
- 35.Reddy BS, Hirose Y, Lubet R, et al. Chemoprevention of colon cancer by specific cyclooxygenase-2 inhibitor, celecoxib, administered during different stages of carcinogenesis. Cancer research. 2000;60:293–297. [PubMed] [Google Scholar]
- 36.Gerner EW, Meyskens FL., Jr Combination chemoprevention for colon cancer targeting polyamine synthesis and inflammation. Clin Cancer Res. 2009;15:758–761. doi: 10.1158/1078-0432.CCR-08-2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sporn MB. Combination chemoprevention of cancer. Nature. 1980;287:107–108. doi: 10.1038/287107a0. [DOI] [PubMed] [Google Scholar]
- 38.Lauwers GY, Kandemir O, Kubilis PS, Scott GV. Cellular kinetics in Barrett's epithelium carcinogenic sequence: roles of apoptosis, bcl-2 protein, and cellular proliferation. Modern Pathology. 1997;10:1201–1208. [PubMed] [Google Scholar]
- 39.Wong DJ, Paulson TG, Prevo LJ, et al. p16(INK4a) lesions are common, early abnormalities that undergo clonal expansion in Barrett's metaplastic epithelium. Cancer research. 2001;61:8284–8289. [PubMed] [Google Scholar]
- 40.Zhang F, Altorki NK, Wu YC, Soslow RA, Subbaramaiah K, Dannenberg AJ. Duodenal reflux induces cyclooxygenase-2 in the esophageal mucosa of rats: evidence for involvement of bile acids. Gastroenterology. 2001;121:1391–1399. doi: 10.1053/gast.2001.29781. [DOI] [PubMed] [Google Scholar]
- 41.Leung C, Lingbeek M, Shakhova O, et al. Bmi1 is essential for cerebellar development and is overexpressed in human medulloblastomas. Nature. 2004;428:337–341. doi: 10.1038/nature02385. [DOI] [PubMed] [Google Scholar]
- 42.Ruiz i, Altaba A. Gli proteins encode context-dependent positive and negative functions implications for development and disease. Development. 1999;126:3205–3216. doi: 10.1242/dev.126.14.3205. [DOI] [PubMed] [Google Scholar]
- 43.Xie K, Abbruzzese JL. Developmental biology informs cancer: the emerging role of the hedgehog signaling pathway in upper gastrointestinal cancers. Cancer cell. 2003;4:245–247. doi: 10.1016/s1535-6108(03)00246-0. [DOI] [PubMed] [Google Scholar]
- 44.Qualtrough D, Buda A, Gaffield W, Williams AC, Paraskeva C. Hedgehog signalling in colorectal tumour cells: induction of apoptosis with cyclopamine treatment. International journal of cancer. 2004;110:831–837. doi: 10.1002/ijc.20227. [DOI] [PubMed] [Google Scholar]
- 45.Choi SS, Omenetti A, Witek RP, et al. Hedgehog pathway activation and epithelial-to-mesenchymal transitions during myofibroblastic transformation of rat hepatic cells in culture and cirrhosis. American journal of physiology. 2009;297:1093–1106. doi: 10.1152/ajpgi.00292.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Matise MP, Joyner AL. Gli genes in development and cancer. Oncogene. 1999;18:7852–7859. doi: 10.1038/sj.onc.1203243. [DOI] [PubMed] [Google Scholar]
- 47.Karhadkar SS, Bova GS, Abdallah N, et al. Hedgehog signalling in prostate regeneration, neoplasia and metastasis. Nature. 2004;431:707–712. doi: 10.1038/nature02962. [DOI] [PubMed] [Google Scholar]
- 48.Kubo M, Nakamura M, Tasaki A, et al. Hedgehog signaling pathway is a new therapeutic target for patients with breast cancer. Cancer research. 2004;64:6071–6074. doi: 10.1158/0008-5472.CAN-04-0416. [DOI] [PubMed] [Google Scholar]
- 49.Berman DM, Karhadkar SS, Maitra A, et al. Widespread requirement for Hedgehog ligand stimulation in growth of digestive tract tumours. Nature. 2003;425:846–851. doi: 10.1038/nature01972. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.