History
Experimental Intestinal Transplantation
Fifty years after Alex Carrel performed the first attempts at canine intestinal transplantation in 1902,1 two major works were carried out independently at the University of Minnesota and Northwestern University. In 1959, Lillehei et al.2 reported a technique for isolated intestinal transplantation in dogs. Lillehei and co-workers removed the entire small bowel, except for short segments at the proximal jejunum and distal ileum, on a vascular pedicle of the superior mesenteric artery and the superior mesenteric vein. The graft was immersed in cold normal saline and transplanted orthotopically into the same dog or a companion animal. In 1960, Starzl and Kaupp3 described a multivisceral transplantation in dogs, a technique to transplant the small bowel as a composite of abdominal organs. The grafts included the stomach, liver, pancreas, intestine, and colon. Two central arteries, the celiac axis and the superior mesenteric artery in continuity with the aorta, were joined to the recipient infrarenal aorta. Both experiments clearly demonstrated the technical feasibility of intestinal transplantation, and became the standard method currently used for composite (either multivisceral or small bowel and liver) grafting or for isolated small-bowel grafting in intestinal transplantation. These two studies, along with a small animal experiment by Monchik and Russell,4 paved the way for investigating the problems related to this procedure, such as immunology, immunosuppression, graft preservation, metabolic events, and graft function.
Clinical Intestinal Transplantation
Although the intestine was one of the first organs to be transplanted experimentally, clinical intestinal transplantation had been unsuccessful until recently, primarily owing to the absence of potent immunosuppressive agents.
Before cyclosporine was introduced, seven unsuccessful intestinal transplants were performed5–9; the longest patient survival was 76 days.9 These patients had no other therapeutic option since total parenteral nutrition (TPN) had not yet been developed. Azathioprine, steroids, antilymphocyte globulin (ALG), or thoracic duct drainage were used for immunosuppressive therapy, but the patients died from rejection, as well as poor graft preservation, technical complications, and sepsis.
The development of TPN in the early 1970s, combined with the consecutive failures at transplanting the intestine, inhibited the development of clinical intestinal transplantation for almost a decade. However, the lull ended when Cohen et al., 10 at the University of Toronto in 1986, performed the first intestinal transplantation using cyclosporine. The patient survived for only 10 days.
Extended survival of an intestinal transplant recipient was first accomplished in 1987,11 when a 3½-year-old girl lived for 192 days after receiving a multiorgan transplant for short-gut syndrome and TPN-induced liver failure. Postoperative immunosuppression was with cyclosporine, steroids, OKT3, and irradiation. The intestinal graft, as well as the other organ allografts, was fully functional for almost 6 months until she died of postoperative lymphoproliferative disease. There was no histologic evidence of graft rejection at autopsy. The following year Grant and co-workers12 performed a successful combined intestine and liver transplant in London, Ontario. The patient was a 41-year-old woman who lost her small bowel as a result of superior mesenteric artery thrombosis caused by antithrombin III deficiency. Mild episodes of graft-vs.-host disease (GVHD) and rejection developed during the early postoperative period but were easily reversed by therapy. To date, this patient and a second patient13 who received the same procedure by Grant’s group are alive and doing well, with functioning grafts.
Experience with isolated small-bowel transplantation under cyclosporine has been unsatisfactory when compared to the experience in liver and intestinal transplantation. Including the case of Cohen et al.,10 a total of 13 isolated intestinal transplants were reported from centers in Chicago (n = 1),14 Paris (n = 7),15 Kiel, Germany (n = 2),16, 17 London, Ontario (n = 1),18 and Uppsala, Sweden (n = 1),19 of which 11 grafts were lost. Only two patients receiving grafts from living-related donors17 or cadaver donors20 are currently alive with functioning grafts, a success rate of 15%. Recent statistics from the International Small Bowel Transplantation Registry (Dr. D. Grant, personal communication, December 1992) show that the survival rate after isolated grafting and combined grafting was 6% (1/15) and 75% (3/4), respectively. Grant attributes the more favorable outcome of combined transplantation compared to isolated grafting to a protective or tolerogenic effect by the liver over the intestinal graft, a concept which was first indicated by Starzl in his multiorgan transplantation experiment, and later confirmed and extended by Calne et al.21 and Kamada et al.22
The advent of a new immunosuppressive agent, FK506, appears to have transformed intestinal transplantation from experimental to practical reality.23, 24 Although the chemical structure and binding immunophilin are different from cyclosporine, FK506 has a similar but more potent immunosuppressive action than cyclosporine. Nephrotoxic, neurotoxic, and diabetogenic side effects of the two drugs are similar, but FK506 causes no gingival hyperplasia or hirsutism. Encouraged by the results of experimental intestinal transplantation25, 26 as well as the results of clinical solid organ transplantations27 under FK506, we initiated a clinical trial of intestinal transplantation in May 1990. From that time through November 1992, a total of 30 patients received either isolated intestinal transplantation (n = 9), combined intestinal and liver transplantation (n = 17), or multivisceral transplantation (n = 4). Of these recipients, 24 are currently alive with functioning grafts on unrestricted oral diets after a minimum follow-up of 4 months.
Indications
Intestinal Failure
Intestinal failure is defined as a state of inability to maintain nutrition or positive fluid and electrolyte balance without special support owing to the loss of absorptive surface or function of the native small bowel.28
Normally, an adult ingests 2 L of fluid daily, and produces 7 to 8 L of fluids as gastric, biliary, pancreatic, and intestinal secretions, of which only 100 to 200 mL of fluid is expelled with feces. The intestine has an enormous capacity to absorb water as well as nutrients, electrolytes, vitamins, minerals, and substances that recirculate via the enteric route. If absorptive function or the intestinal surface area is excessively lost, malnutrition, dehydration, metabolic abnormalities, sepsis, and mortality are the sequelae of events, unless management with TPN takes place. Currently, most patients receive TPN at home, as home parenteral nutrition (HPN). From Medicare data, approximately 19,700 patients, or 80 per million, were on HPN in the United States in 198729; this figure is much higher than the 2 to 4 per million in Europe because of more liberal use of the therapy in the United States.28
Causes of Intestinal Failure
Causes of intestinal failure can be classified into two categories: (1) failure due to surgical or anatomic loss, or (2) failure due to functional abnormality. Surgical intestinal failure (short-bowel syndrome) may occur after major resection of the intestine for such indications as congenital anomaly, vascular thrombosis, volvulus, necrotizing enterocolitis, inflammatory bowel disease, trauma, and desmoid tumor. Functional intestinal failure is caused by either an enterocyte abnormality or by intestinal dysmotility. Microvillus inclusion disease and radiation enteritis are examples of an enterocyte abnormality. Functional intestinal failure due to motility disorder (intestinal pseudo-obstruction) is caused by either a myopathy or neuropathy of the intestinal wall. Table 1 summarizes the cause of intestinal failure for the 204 patients who were referred to our center for evaluation for intestinal transplantation from 1990 through 1992.
TABLE 1.
Cause of Intestinal Failure for Patients Referred to the Pittsburgh Transplantation Center
| Adults | Children | ||
|---|---|---|---|
| Indication | No. | Indication | No. |
| Crohn’s disease | 22 | Necrotizing enterocolitis | 25 |
| Thrombotic disorder | 22 | Gastroschisis | 19 |
| Trauma | 12 | Volvulus | 14 |
| Pseudo-obstruction | 11 | Pseudo-obstruction | 10 |
| Radiation enteritis | 5 | Intestinal atresia | 6 |
| Familial polyposis | 4 | Hirschsprung’s disease | 3 |
| Volvulus | 4 | Megacystic colon | 3 |
| Budd-Chiari syndrome | 2 | Microvillus inclusion disease | 3 |
| Desmoid tumor | 2 | Malrotation | 2 |
| Gardner’s syndrome | 2 | Other | 14 |
| Other | 19 | ||
Intestinal Adaptation
After massive enteric resection, the residual bowel is known to undergo adaptive changes to compensate for the loss of absorptive surface area by widening the circumference and increasing the villus height.30 Intraluminal nutrients, pancreatobiliary secretions, hormones, and enterotrophic factors facilitate the adaptation process. Clinically, the adaptive process has been divided into stages: stage I at 7 to 10 days, when massive diarrhea impels intensive repletion of fluid and electrolyte losses; stage II at 1 to 3 months, when diarrhea stabilizes and full TPN support and other medical management are required; and stage III at 3 to 12 months, when diarrhea is controlled to institute enteral feeding and discontinue TPN. If TPN cannot be discontinued from 12 to 24 months after the initial insult, intestinal failure approaches an irreversible state, and most of the patients require TPN permanently. Typically, one half of the patients who are placed on TPN require permanent therapy (1–2 per million with irreversible intestinal failure).28
The irreversibility of surgical intestinal failure, although difficult to determine at the time of small bowel resection, correlates with the length of remaining bowel, the site of intestinal resection, and the presence or absence of the ileocecal valve. Willmore,31 in 1972, stated that the survival of infants is highly unlikely if remaining bowel length is less than 40 cm and if the ileocecal valve is removed. More recently, patients with as little as 10 cm of bowel length and an intact ileocecal valve have been reported32 to recover from intestinal failure. In general, resection of more than 80% of the small bowel, along with the ileocecal valve, are high-risk factors for permanent loss of intestinal absorptive function. Resection of the jejunum and retention of the ileum are favorable since the remaining ileum has active adaptive capacity. The loss of the large bowel is also serious since the gastrointestinal tract loses the ability to absorb water.
Problems Associated with TPN
Patients who are placed on TPN cannot escape the threat of TPN-related complications. Along with problems that occur at the time of catheterization, long-term TPN management is beset by various complications and frequent hospital admissions for care. These complications include vascular thrombosis, metabolic abnormality, bone disease, cholelithiasis, and often lethal sepsis and liver disease. Of the 1,594 HPN patients followed by the OASIS registry since 1984, those with benign intestinal diseases experienced 2.6 complications requiring hospitalization per year.29 Three-year survival ranged from 65% to 80% depending on the cause of disease, of which 6.7% of the deaths were from TPN-related complications. In Europe, sepsis, major vessel thrombosis, and liver failure are ascribed to 28% of the patient deaths under TPN therapy.33
Liver disease induced by TPN is very serious, especially in infants. Cholestasis usually appears in 30% to 40% of the patients under long-term TPN management, and sometimes progresses to significant liver failure. The analysis by Grosfeld et al.34 of 60 infants showed that cholestasis was reversible if the patient was switched from TPN to complete enteral feeding and if the total bilirubin was less than 30 mg/dL. If the total bilirubin was greater than 30 mg/dL, reversal did not occur. Five of the nine deaths in Grosfeld’s series were due to liver failure. The same trend was observed with pediatric patients who were referred to our center. Of the 99 pediatric patients referred to us (see Table 1), 25 died from liver failure and sepsis while awaiting intestinal transplantation.
Social problems are another important issue related to long-term TPN therapy. Because of the limitations on social and personal activities, some TPN patients become very dependent on their caregiver, and sometimes experience psychiatric disturbances and drug abuse. The cost of TPN maintenance is very expensive, and increasing. In 1980, the cost per patient ranged from $16,506 to $24,939 per year, increased to $17,000 to $127,000 per year by 1983,35 and is currently estimated at $75,000 to $150,000 per year.29
Types and Indications of Intestinal Transplantation
Surgical procedures performed to correct short-bowel syndrome are not always successful.36 Implantation of the intestine is therefore the theoretical and only reliable choice to cure patients who are at the irreversible stage of anatomic and functional intestinal failure. Currently, three different types of intestinal transplantation can be performed depending upon the cause and severity of intestinal failure and the presence of extraenteric organ dysfunction.
Isolated intestinal transplantation is indicated for patients who have irreversible small-bowel failure with no other organ dysfunction. Since it is still at the experimental stage, at this time we perform this procedure in highly selected patients, such as those whose venous accesses are running out because of major vessel thrombosis or for Crohn’s disease patients who are refractory to any conventional surgical and medical treatments.
Transplantation of combined intestine and liver grafts is performed for patients who have intestinal failure and liver disease caused by TPN or inborn error. Particularly, the patients who have very high bilirubin levels or recurrent variceal bleeding require transplantation urgently. Multiorgan transplantation is less frequent. It is reserved for patients who have severe dysmotility of the entire gastrointestinal tract, occlusion of both the celiac axis and the superior mesenteric artery, thrombosis of the entire mesenteric venous system, or extensive polyposis throughout the digestive tract.
Donors
Selection of Donors
Grafts for intestinal transplantation are obtained from cadaver donors. The general criteria for donor selection do not differ from those for liver donors. Donors with stable cardiopulmonary status and liver function are suitable. Those with systemic infection and malignancy are excluded. ABO blood type should be identical between donor and recipient. HLA matching is not currently considered and is universally poor. Donors with prior cytomegalovirus (CMV) infection require special consideration, especially when recipients are negative for CMV. These recipients always develop severe and persistent CMV infection postoperatively despite aggressive prophylaxis and treatment. Donors who are of similar size as the recipients, or preferably one fourth to one third smaller, are recommended to avoid tight and difficult closure of the abdominal wound at transplantation.
Theoretically, living-related donors can donate isolated intestinal grafts, a minimum of 60 cm in adults,17 but this may not be justified except in cases of complete HLA matching between donor and recipient. Organ supply from cadaver donors, 4,000 to 4,500 annually in the United States, exceeds the estimated number of patients, 1 to 2 per million, or 200 to 400,28 who will require permanent TPN. More important, isolated intestinal transplantation can be delayed until the most suitable organ becomes available since it is not an urgent, lifesaving procedure.
Donor Operation
After the donor is accepted, selective decontamination of the gastrointestinal tract is begun through a nasogastric tube (10–30 mL/min) using a polyethylene glycol–electrolyte solution (Golytely) containing amphotericin B 500 mg; tobramycin 80 mg; and polymixin E 100 mg. Intravenously, cefotaxim 25 mg/kg and ampicillin, 25 mg/kg are also administered.
Immunomodulation of the graft using radiation, mesenteric lymph node dissection, or antilymphocyte antibody administration has been recommended to lessen rejection episodes in many experimental studies, but without significant benefit in clinical cases. 14 None of these procedures have been adopted with our patients.
Logistics and steps of the donor operation were described elsewhere.37, 38 Briefly, the abdomen is opened through a thoracoabdominal incision. For procurement of an isolated graft, the whole small bowel and the ascending and transverse colon are mobilized by dividing retroperitoneal fusions. The terminal ileum adjacent to the ileocecal valve is stapled and divided, and vessels within the ascending and transverse mesocolon are divided. When the middle colic vessels are divided, the superior mesenteric artery and vein are exposed at the inferior border of the pancreas. The proximal jejunum is stapled and transected close to the ligament of Treitz. Dissection of the superior mesenteric vein is extended to its confluence with the splenic vein. Transection of the pylorus and the neck of the pancreas facilitates exposure of both vessels and the portal vein. The superior mesenteric artery is dissected to the root at the anterior surface of the abdominal aorta. Care must be taken to preserve the right hepatic artery from the superior mesenteric artery if it is found.
When the intestine is procured with the liver, hepatic hilar dissection, as usually done in harvesting the liver graft, is performed initially. The distal common bile duct is transected. The hepatic artery is dissected to the origin of the celiac axis by dividing the gastroduodenal artery, splenic artery, and left gastric artery. After the intestine is isolated, the portal vein is completely isolated by dividing tributaries draining into the portal vein carefully to procure both organs in continuity with the portal vein. Multivisceral procurement follows the hepatic hilar dissection, intestinal isolation, and dissection of the left upper abdominal organs (stomach, pancreas, and spleen), in that order. After the intestine is isolated, the pancreas and spleen are mobilized from the retroperitoneum, and the abdominal esophagus is stapled and transected a few centimeters proximal to the esophagogastric junction. The celiac axis and the superior mesenteric artery are resected together as a Carrel patch without injuring the origins of the renal arteries. Procurement of both donor iliac artery and vein, and the thoracic aorta are mandatory for vascular reconstruction at transplantation.
Preservation of the Graft
After systemic heparinization, the intestine and other abdominal organs are flushed with 1 to 2 L of chilled University of Wisconsin (UW) solution via a catheter inserted into the lower abdominal aorta. When the liver is harvested with the intestine, an additional 1 L of UW solution is given, in situ or on the back table, into the liver through the inferior mesenteric vein. Care needs to be taken to minimize the amount of UW solution used for intestinal perfusion to avoid swelling of tissues. Although luminal flushing with an electrolyte solution containing antibiotics is common practice in the other center,15 it was omitted with our patients to simplify the procedure and to avoid bacterial contamination. The graft is stored on ice for transport. Preservation time varies from 2.8 to 11.1 hours, with a mean of 7.7 hours.
Similar to the transplantation of other solid organs, an effective method to maintain better graft viability during preservation is a key to success in intestinal transplantation. Simple cold storage with UW solution39 has been used for this purpose in all of our cases except for one, where an isolated intestinal graft was excised and simply immersed in cold lactated Ringer’s solution. Although no postoperative problems were seen in any of these cases, it has not yet been determined whether UW solution is the most appropriate preservation solution for intestinal preservation. Better animal survival and motility function have been shown in rat intestinal grafts preserved with UW solution,40 but energy stores were inferior to the grafts preserved with Euro-Collins solution.41 Additionally, UW-preserved canine small bowel showed more lipid peroxidation damage when compared to Euro-Collins-preserved grafts.42
Recipients
Evaluation of the Recipient
Hematologic studies, infectious status, hepatic and renal function, cardiopulmonary status, and immunologic studies are performed as is routine with most of the solid organ recipients. The nature and course of intestinal failure and the anatomic and functional status of the remaining gastrointestinal tract are particularly important since the type of transplantation is decided on these factors. Anatomic assessments include a detailed history of past surgery (frequency, reason, and type of operation), length and location of remaining intestine, presence or absence of the ileocecal valve, and abnormality of the splanchnic vessels and major systemic vessels. Barium study, endoscopy, computed tomography (CT), ultrasound, and angiography are used for anatomic assessment. Motility studies of the entire gastrointestinal tract, from the stomach to the rectum, are essential to determine the severity and extent of functional intestinal failure. Total gastric resection is considered if there is a marked gastric atony. If rectal function is normal and if lesions are confined only within the mucosal layer (e.g., multiple polyposis), a pull-through technique using transplanted intestine may be added to gastrointestinal reconstructions. If patients have evident liver failure, such as high bilirubin, cirrhosis, variceal bleeding, or splenomegaly, they are candidates for combined intestine and liver transplantation. However, if the liver damage is not advanced, accompanied only by mild fibrosis at the portal triad or a lower bilirubin level, isolated intestinal transplantation is chosen.
Finally, determination of absorptive function of the remaining intestine is important, since some intestinal failure patients who were referred to our center were able to be switched from TPN to enteral feeding to avoid intestinal transplantation.
Recipient Operation
Final judgment on the type of transplantation that will be performed is made after laparotomy by careful investigation of native vessels and abdominal organs. Close and frequent communication between the donor team and the recipient surgeons is essential.
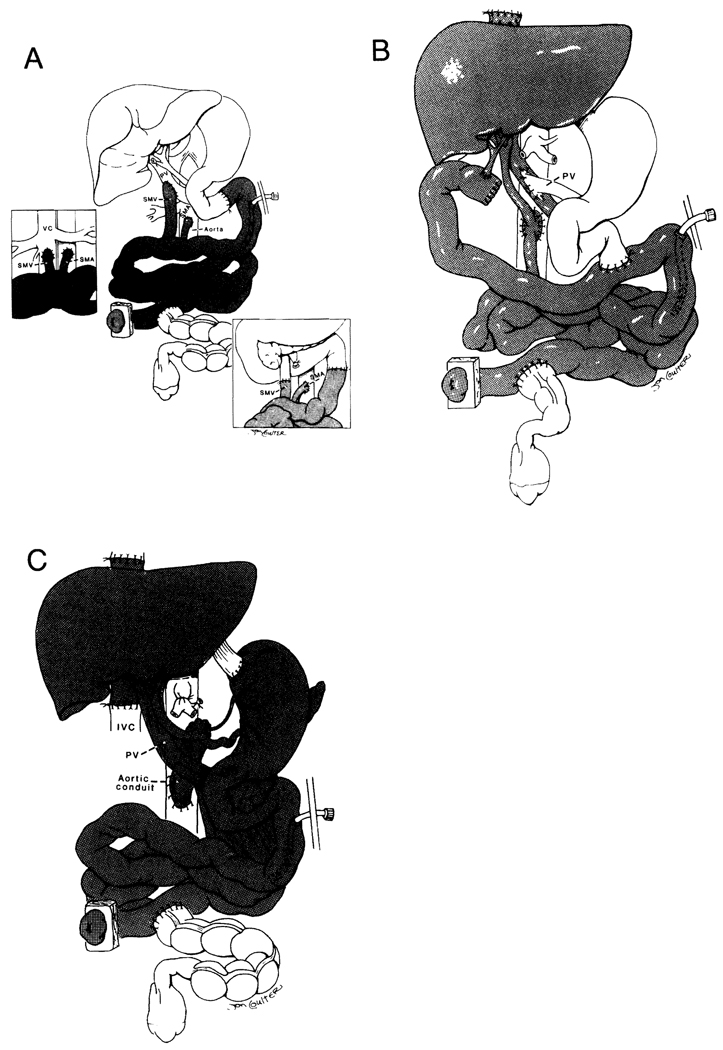
The abdomen is opened through a midline incision with a unilateral or bilateral transverse incision. All of the adhesions from the multiple surgeries (if any) are carefully dissected. Figure 1 illustrates the methods of vascular and gastrointestinal reconstruction for the three types of intestinal transplantation. For arterial reconstruction, the anterior wall of the recipient infrarenal aorta is used exclusively for end-to-side anastomosis with the superior mesenteric artery in isolated intestinal grafting, or with a Carrel patch containing both the celiac axis and the superior mesenteric artery for combined intestinal and multivisceral grafting. Venous outflow from the isolated small-bowel graft is drained into the recipient mesenteric venous system (rather than into the vena cava) either by anastomosing the donor superior mesenteric vein to the distal end of the recipient superior mesenteric vein, to the confluence of the superior mesenteric vein with the splenic vein, or to the main trunk of the portal vein at the hepatic hilum (mesenteric piggyback technique).43 Mesocaval anastomosis was required only on one occasion for the retransplantation of an isolated graft. In one combined intestine and liver transplant, a portacaval shunt was created before the native hepatectomy. This decreases venous congestion in the remaining organs and bleeding during the procedure. Venovenous bypass, used in orthotopic liver transplantation, is not applicable in most cases because of the thromboses of major vessels from TPN. After the liver is replaced by the piggyback method,44 the portacaval shunt is converted to a portaportal shunt by anastomosing the recipient portal vein to the side of the graft portal vein. This ensures that the transplanted liver is being perfused by the recipient splanchnic venous blood containing so-called hepatotrophic substances.45 If the recipient portal vein is too short, or the graft portal vein is too small for anastomosis, a portacaval shunt can be left in place permanently. In multivisceral transplantation, removal of the native organs is performed in the same way as the donor operation, and the grafts are transplanted en bloc.
FIG 1.
Intestinal transplantation. A, isolated grafting; B, combined intestine and liver grafting; C, multivisceral grafting. PV = portal vein; SMV = superior mesenteric vein; SMA = superior mesenteric artery; IVC = inferior vena cava. (From Todo S, Tzakis A, Abu-Elmagd K, et al: Ann Surg 1992; 216:223–234. Used by permission.)
Reconstruction of gastrointestinal continuity in isolated and combined grafting is achieved by joining each end of the intestinal graft to each of the remaining bowel ends. It is important to leave the recipient intestine as long as possible, since it will enable reanastomosis or enterostomy if the graft needs to be taken out later. Proximal intestinal reconstruction in multivisceral transplantation is achieved by anastomosing the distal esophagus to the anterior wall of the graft stomach, to which pyloroplasty is added routinely. Three enterostomies are necessary for intestinal transplantation. Gastrostomy is made to decompress intestinal congestion during the early postoperative period and to control delayed gastric emptying, which occurs postoperatively in most recipients. Jejunostomy is made for intestinal decompression and as a route for enteral feeding. The distal end of the graft is exteriorized by the chimney method, in which the recipient ileum or colon is anastomosed to the side of the graft below the stoma. The stoma is used as a route for endoscopic examination and mucosal biopsy. Cholecystectomy is performed in all cases, and biliary reconstruction by choledochojejunostomy is made in all combined graftings.
Postoperative Management
Immunosuppression
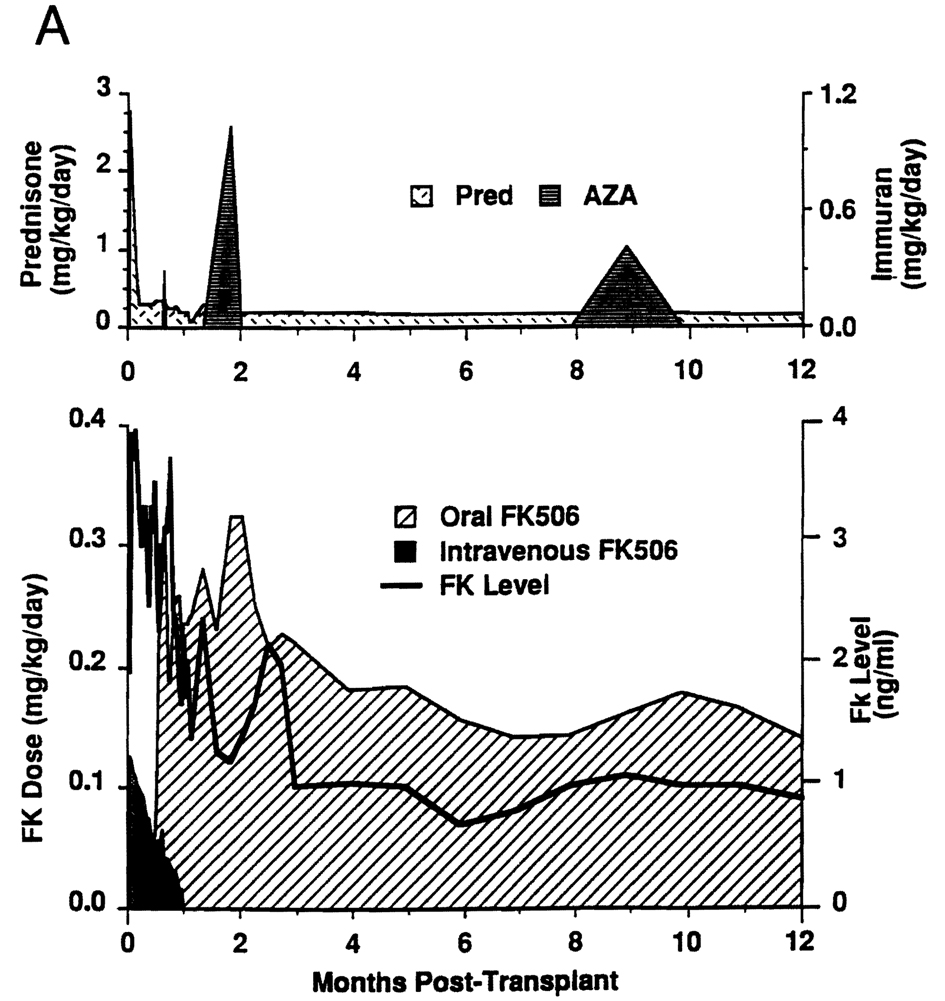
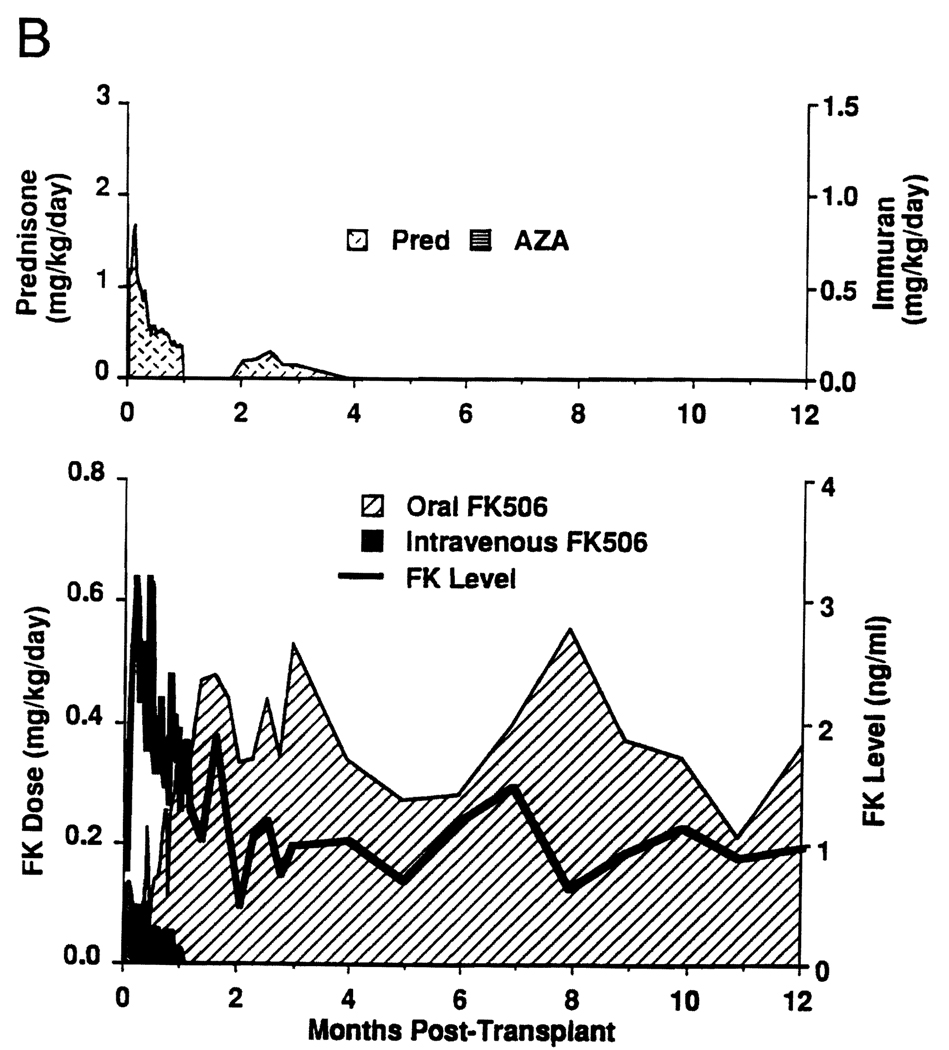
Postoperative immunosuppression is by a combination of FK506, steroids, and prostaglandin El (PGE1, Prostin), starting immediately after graft reperfusion. FK506 is administered by continuous intravenous infusion at doses of 0.1 to 0.15 mg/kg/day, and continued for 7 to 10 days until patients can tolerate enteral feeding. Intravenous FK506 is switched to oral formula at 0.3 mg/kg/day (divided doses) with several days of overlap. Since FK506 pharmacokinetics is influenced by intestinal function, hepatic abnormality, and other medications, it is important to measure drug levels frequently: daily during hospitalization, two to three times per week for several months, and weekly thereafter. Plasma trough levels of FK506 are maintained at 2 to 3 ng/mL, or slightly higher, for the first month, at 1 to 2 ng/mL till the third month, and approximately at 1 ng/mL thereafter (Fig 2).
FIG 2.
Immunosuppression of intestinal recipients. A, adult patients (n = 15); B (next page), pediatric patients (n = 15). Pred = prednisone; AZA = azathioprine.
Steroids, 1 g of methylprednisolone in adults, or hydrocortisone in children, are given intraoperatively, followed by a steroid taper from 200 mg/day (adult) or 100 mg/day (pediatric) in decrements of 40 mg/day (adult) or 20 mg/day (pediatric) over the first 5 days. Baseline steroid doses of 20 mg/day (adult) or 10 mg/day (pediatric) are gradually lowered over the next few months and maintained at 5 to 10 mg/kg/day, or discontinued.
Continuous intravenous infusion of PGEI is essential to success in intestinal transplantation. It allows maintenance of higher FK506 plasma levels, by protecting the kidney from FK506 renal toxicity, and possible augmentation of immunosuppression.46 Prostin is started at 0.2 µg/kg/hr, and gradually increased to 0.6 to 0.8 µg/kg/hr if recipient hemodynamics are stable. Prostin is continued until intravenous FK506 is discontinued.
In addition to these agents, azathioprine at doses of 0.5 to 1.0 mg/kg/day is supplemented if the therapeutic FK506 dose is not maintained due to renal dysfunction, or if there is recurrent rejection.
Monitoring and Treatment of Intestinal Rejection
Although a number of functional and biochemical markers of intestinal rejection have been proposed in experimental transplantation models, almost all of them are not clinically practical. Intestinal rejection progresses very rapidly from mild to severe if it is not treated immediately. Early detection of graft rejection is imperative. In our experience, a combination of clinical observation, endoscopic examination, and histopathologic analyses of multiple endoscope-guided mucosal biopsies have been used to achieve this objective. If rejection of the intestinal graft is suspected clinically, the native and transplanted intestine is immediately and thoroughly examined with the endoscope and by histopathologic study. A choice of treatments is made, based exclusively on the severity of graft rejection as determined by these investigations. Characteristic findings of mild, moderate, and severe intestinal rejection and their treatment is outlined in Table 2.
TABLE 2.
Monitoring of Acute Intestinal Graft Rejection and Treatment
| Acute Rejection | Clinical Findings | Endoscopic Findings | Mucosal Biopsy Findings |
Treatment |
|---|---|---|---|---|
| Mild to moderate | Fever | Ischemic/dusky mucosa | Cell infiltration | Increase of FK506 dose |
| Abdominal pain | Mucosal edema | Villus blunting | Bolus of steroids | |
| Vomiting | Hyperemia | Cryptitis | Recycle | |
| Increase in stomal output | Loss of fine mucosal pattern | Epithelial cell damage and regeneration | ||
| Watery diarrhea | Decrease of peristalsis | Mucous/Paneth’s cell reduction | ||
| Ileus | ||||
| Severe | Severe diarrhea | Ulceration | Mucosal hemorrhage | Increase of FK506 dose |
| Abdominal pain | Mucosal sluffing | Mucosal sluffing | Recycle of steroids | |
| Abdominal distention | Bleeding | Microabscess | OKT3 | |
| Metabolic acidosis | Loss of peristalsis | |||
| Positive blood culture | ||||
| Adult respiratory distress syndrome |
Prevention of Infection
The same kind of selective decontamination used in the donor is given to the recipient postoperatively, and continued for 4 to 6 weeks after transplantation. Prevention of systemic infection is achieved by intravenous administration of broad-spectrum antibiotics: ampicillin and cefotaxim, given for the first 5 days. Cultures of the blood, stool, urine, sputum, wound exudate, and stomal and peritoneal discharge are repeated frequently and proper antibiotic therapy is given accordingly. Gancyclovir, sulfamethoxazole-trimethoprim (Bactrim), and nystatin (Mycostatin) are given for prophylaxis of CMV, Pneumocystis carinii, and Candida infection, respectively.
Nutrition
Total parenteral nutrition is restarted within 1 to 2 days after transplantation (when patients become hemodynamically stable). At 7 to 10 postoperative days, enteral feeding via a jejunostomy tube is begun after integrity and continuity of the gastrointestinal (GI) tract is confirmed by an upper GI series. Standard commercial formulas, Peptamen and Compleat B (Clintec Nutrition, Deerfield, Ill), are used for enteral nutrition, starting with a diluted solution at a low infusion rate. Nutrition via the parenteral route is gradually tapered in conjunction with a reciprocal increase of enteric nutrition by tube feeding and oral intake. Supplementary administration of intravenous fluids is mandatory to compensate for postoperative fluid loss through the stomal output and diarrhea.
Assessment of Intestinal Graft Function
Clinically, assessment of intestinal graft function is accomplished by studying TPN dependency, weight, height (in pediatrics), volume of stomal output, and frequency and nature of the stool. In addition, studies are conducted periodically to determine absorptive, secretory, and motility function of the graft. Absorptive function is examined by the d-xylose absorption test, 72-hour fecal fat secretion, FK506 pharmacokinetics, Schilling test, and serum levels of vitamins, protein, and minerals. Measurement of serum IgA levels reflects secretory activity of the intestine. Gastrointestinal motility and transit are studied by radionuclear scanning after test meal ingestion, manometry, and conventional barium studies.
Results
Case Material
Table 3 summarizes demographics of the 30 recipients who were treated by intestinal transplantation at our center from May 1990 to November 1992. Fifteen were children with a mean age of 2.7 years, and the other 15 were adults with a mean age of 29.8 years. All of the patients had been managed by TPN for 1 to 132 months and had experienced more than one episode of TPN-related complications, in which liver failure with mean bilirubin of 18.2 mg/dL, ranging from 2.3 mg/dL to 50.5 mg/dL, was seen in 19 patients. Twenty-seven patients had surgical intestinal failure, and functional disorder was the indication for transplantation in the remaining 3 patients. Nine patients received an isolated graft, 17 had combined grafts, and 4 received multivisceral grafts.
TABLE 3.
Intestinal Transplant Recipient Demographics*
| Patient | Age (yr) | Sex | Cause of Intestinal Failure |
Organs Transplanted |
Survival (mo)† | TPN Status | |
|---|---|---|---|---|---|---|---|
| Patient | Graft | ||||||
| 1 | 31.1 | M | Gunshot wound | Small bowel | 25 | 22 | Graft removed, retransplant |
| Small bowel | 2 | Died, sepsis | |||||
| 2 | 3.2 | F | Necrotizing enterocolitis | Small bowel–liver | >32 | >32 | Free |
| 3 | 26.7 | F | SMA thrombosis | Small bowel–liver | >32 | >32 | Free |
| 4 | 4.3 | M | Gastroschisis | Small bowel–liver | >28 | >28 | Free |
| 5 | 2.8 | M | Intestinal atresia | Small bowel–liver | 13 | 13 | Died, PTLD |
| 6 | 0.6 | F | Intestinal atresia | Small bowel–liver | 1 | 1 | Died, sepsis and GVHD |
| 7 | 1.1 | F | Volvulus | Small bowel–liver | >20 | >20 | Free |
| 8 | 1.7 | F | Volvulus | Small bowel–liver | >20 | >20 | Free |
| 9 | 21 | M | Traffic accident | Small bowel–liver | >19 | >19 | Free |
| 10 | 32 | M | CA and SMA thrombosis | Multivisceral | >18 | >18 | Partial |
| 11 | 2.5 | F | Microvillus inclusion disease | Small bowel | >17 | >17 | Free |
| 12 | 1.3 | M | Intestinal atresia | Small bowel | >15 | >15 | Free |
| 13 | 50 | F | Crohn’s disease | Small bowel | >15 | >15 | Free |
| 14 | 34 | F | Desmoid tumor | Small bowel | >14 | 8 | Graft removed |
| 15 | 38 | M | Crohn’s disease | Small bowel | >12 | >12 | Died, sepsis |
| 16 | 10.2 | F | Pseudo-obstruction | Small bowel | >13 | >13 | Partial |
| 17 | 22 | F | Crohn’s disease | Small bowel | >13 | >13 | Free |
| 18 | 25 | M | Crohn’s disease | Small bowel–liver | >12 | >12 | Free |
| 19 | 1.5 | M | Necrotizing enterocolitis | Small bowel–liver | 2 | 2 | Died, sepsis |
| 20 | 29 | F | Desmoid tumor | Small bowel–liver | >10 | >10 | Partial |
| 21 | 24 | M | CA and SMA thrombosis | Multivisceral | >10 | >10 | Free |
| 22 | 20 | F | Traffic accident | Small bowel | >10 | >10 | Free |
| 23 | 4.2 | F | Gastroschisis | Small bowel–liver | >10 | >10 | Free |
| 24 | 1.4 | M | Gastroschisis | Small bowel–liver | 1 | 1 | Died, sepsis |
| 25 | 0.75 | M | Microvillus inclusion disease | Small bowel–liver | >8 | >8 | Free |
| 26 | 0.5 | M | Gastroschisis | Small bowel–liver | >8 | >8 | Free |
| 27 | 31 | F | CA and SMA thrombosis | Multivisceral | >8 | >8 | Free |
| 28 | 19.1 | M | Traffic accident | Small bowel–liver | >8 | >8 | Free |
| 29 | 44 | F | SMA thrombosis | Small bowel–liver | >7 | >7 | Free |
| 30 | 4.5 | F | Pseudo-obstruction | Multivisceral | >5 | >5 | Free |
TPN = total parenteral nutrition; SMA = superior mesenteric artery; PTLD = postoperative lymphoproliferative disease; GVHD = graft-vs.-host disease; CA = coronary artery.
As of March 31, 1993.
Postoperative Course
Postoperatively, patients were managed in the intensive care unit (ICU) in the same manner as liver recipients for ventilatory support, fluid and electrolyte management, and intensive immunosuppressive therapy. Isolated intestinal recipients recovered faster after transplantation and were discharged from the ICU earlier, 6 days vs. 12 days, than those receiving combined or multivisceral grafts because of less operative complexity and better preoperative conditions. Initiation of enteral feeding and discontinuation of TPN were also much faster with isolated intestinal recipients, 9 days vs. 18.5 days, and 30 days vs. 48 days, probably for the same reasons.
Survival
Twenty-four of the 30 recipients (80%) are currently alive for 4 to 32 months after intestinal transplantation. Survival rates for patients receiving an isolated graft, combined grafts, and multivisceral grafts were 78% (7/9), 76% (13/17), and 100% (4/4), respectively.
Of the nine isolated graft recipients, three patients required graft removal due to acute (n = 2) or drug-noncompliant chronic (n = 1) rejection, for which one patient underwent retransplantation and died. Graft survival was 60% (6/10). Graft survival rates for combined and multivisceral grafts were the same as those of the patients.
Mortality
Of the six deaths, three patients died within 3 months after transplantation and the remaining 3 died after 1 year. The early deaths were children receiving combined grafts. Sepsis related to technical failure (intestinal anastomotic leakage, biliary leakage, or hepatic artery thrombosis) was the cause of mortality in all of these early deaths. Of the three late mortalities, one child who received a combined small bowel–liver graft died of lymphoproliferative disease at 13 months. Two adult patients who underwent isolated graft transplantation died, at 12 months from sepsis after graft removal for acute rejection, and at 26 months, also from sepsis after intestinal retransplantation.
Rejection
The overall incidence of acute intestinal rejection was 87.5%. The risk of rejection was high at 75% within 1 month, reduced to 20% at the third month, but increased again after 6 months mostly due to transient reduction of immunosuppression for viral or fungal infection. Chronic rejection was demonstrated histologically in two failed grafts. One graft was removed at 21 months for drug-noncompliant rejection, and the other was removed at 8 months due to rejection induced by withdrawal of immunosuppression for demyelination of the white matter of the brain.
Graft-vs.-host disease has been a threat in intestinal transplantation, but has actually occurred in only one patient (0.03%) in our series (1/30). The patient developed pneumocystis pneumonia and intestinal anastomotic leakage within a week after combined grafting, which compelled a marked reduction in immunosuppression. Graft-vs.-host disease was diagnosed by immunohistologic study of skin biopsies which were taken a day before the patient died, but was not seen in the skin biopsies taken 4 days previously. Cellular or humoral evidence of GVH disease after intestinal transplantation was described in only three patients among past clinical cases.9, 10, 12
Infection
All but two adult patients developed bacterial infection postoperatively. Line sepsis, abdominal wound infection, and peritonitis are major sources of infection. Bacterial translocation was seen in each of two adult and pediatric recipients, and successfully treated by augmentation of immunosuppression and antibiotics. Seven of the 15 adult recipients developed CMV enteritis 1 to 4 months after transplantation, of which 2 had persistent infection. Three of the 15 pediatric recipients developed postoperative lymphoproliferative disease by Epstein-Barr virus infection, and one had a lethal outcome.
Graft Function
Stomal discharge, reflecting resumption of gastrointestinal motility, was seen within 2 to 3 days after transplantation, progressively increased to 1 to 2 L/day, and then became stable at 0.5 to 1.0 L/day after 3 to 6 months. Dysmotility developed postoperatively on both native stomach and transplanted intestine. Delayed gastric emptying was detected by barium study and radioisotope scanning in 75% of the patients within the first 2 months. It resolved spontaneously to 30% at 4 months and 15% by 6 months. The cause of delayed gastric emptying is unclear. More than one half of the recipients had accelerated small-intestine transit time of less than 2 hours by barium study, and a few patients showed prolonged transit time of more than 4 hours. Both abnormalities subsided spontaneously in a majority of the recipients in 6 to 12 months. All but one of the 23 surviving patients with functioning grafts are completely free from TPN (see Table 3). All of them have gained or maintained body weight solely by enteral nutrition. One recipient requires partial TPN support during the night because of very high stomal output. Serum protein and albumin levels of the patients are within normal ranges with satisfactory absorption of FK506 and d-xylose, but 72-hour fecal fat secretions are abnormal in all of the patients, ranging from 2.4% to 88.3%.
Acknowledgments
Supported by Research Grants from the Veterans Administration and Project Grant No. DK-29961 from the National Institutes of Health, Bethesda, Maryland.
Contributor Information
Satoru Todo, Associate Professor of Surgery, Pittsburgh Transplantation Institute, University of Pittsburgh School of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Andreas Tzakis, Associate Professor of Surgery, Pittsburgh Transplantation Institute, University of Pittsburgh School of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Kareem Abu-Elmagd, Assistant Professor of Surgery, Pittsburgh Transplantation Institute, University of Pittsburgh School of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Jorge Reyes, Assistant Professor of Surgery, Pittsburgh Transplantation Institute, University of Pittsburgh School of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Thomas E. Starzl, Professor of Surgery, Pittsburgh Transplantation Institute, University of Pittsburgh School of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
References
- 1.Carrel A. La technique opératoire des anastomoses vasculaires et la transplantation des viscères. Lyon MEO. 1902;98:859–864. [Google Scholar]
- 2.Lillehei RC, Goott B, Miller FA. The physiological response of the small bowel of the dog to ischemia including prolonged in vitro preservation of the bowel with successful replacement and survival. Ann Surg. 1959;150:543–560. doi: 10.1097/00000658-195910000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Starzl TE, Kaupp HA., Jr Mass homotransplantation of abdominal organs in dogs. Surg Forum. 1960;11:28–30. [PMC free article] [PubMed] [Google Scholar]
- 4.Monchik GJ, Russell PS. Transplantation of small bowel in the rat: Technical and immunological considerations. Surgery. 1971;70:693–702. [PubMed] [Google Scholar]
- 5.Lillehei RC, Idezuki Y, Feemster JA, et al. Transplantation of stomach, intestine and pancreas: Experimental and clinical observations. Surgery. 1967;62:721–741. [PubMed] [Google Scholar]
- 6.Okumura M, Fujimura I, Ferrari AA, et al. Transplante de intestino delgado: Apresentacao de um caso. Rev Hosp Clin Fac Med Sao Paulo. 1969;2D:39–54. [PubMed] [Google Scholar]
- 7.Olivier CL, Rettori R, Olivier CH, et al. Homotransplantation orthotopique de l’intestin grêle et des colons droit et transverse chez l’homme. J Chir (Paris) 1969;98:323–330. [PubMed] [Google Scholar]
- 8.Alican F, Hardy JD, Cayirli M, et al. Intestinal transplantation: Laboratory experience and report of a clinical case. Am J Surg. 1971;121:105–107. doi: 10.1016/0002-9610(71)90092-4. [DOI] [PubMed] [Google Scholar]
- 9.Fortner JG, Sichuk G, Litwin SD, et al. Immunological responses to an intestinal allograft with HL-A-identical donor-recipient. Transplantation. 1972;14:531–535. doi: 10.1097/00007890-197211000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Cohen Z, Silverman RE, Wassef R, et al. Small intestinal transplantation using cyclosporine: Report of a case. Transplantation. 1986;42:613. doi: 10.1097/00007890-198612000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Starzl TE, Rowe M, Todo S, et al. Transplantation of multiple abdominal viscera. JAMA. 1989;26:1449–1457. [PMC free article] [PubMed] [Google Scholar]
- 12.Grant D, Wall W, Mimeault R, et al. Successful small-bowel/liver transplantation. Lancet. 1990;335:181–184. doi: 10.1016/0140-6736(90)90275-a. [DOI] [PubMed] [Google Scholar]
- 13.McAlister V, Wall W, Ghent C, et al. Successful small intestine transplantation. Transplant Proc. 1992;24:1236–1237. [PubMed] [Google Scholar]
- 14.Tattersall C, Gebel H, Haklin M, et al. Lymphocyte responsiveness after irradiation in canine and human intestinal allografts. Curr Surg. 1989;46:16–19. [PubMed] [Google Scholar]
- 15.Revillon Y, Jan D, Goulet O, et al. Small bowel transplantation in seven children: Preservation technique. Transplant Proc. 1991;23:2350–2351. [PubMed] [Google Scholar]
- 16.Hansmann ML, Deltz E, Gundlach M, et al. Small bowel transplantation in a child. Am J Clin Pathol. 1989;920:686–692. doi: 10.1093/ajcp/92.5.686. [DOI] [PubMed] [Google Scholar]
- 17.Deltz E, Schroeder P, Gebhardt H, et al. Successful clinical small bowel transplantation: Report of a case. Clin Transplant. 1989;3:89–91. [Google Scholar]
- 18.Grant D, Sommerauer J, Mimeault R, et al. Treatment with continuous high dose intravenous cyclosporine following intestinal transplantation: A case report. Transplantation. 1989;48:151–152. doi: 10.1097/00007890-198907000-00036. [DOI] [PubMed] [Google Scholar]
- 19.Wallander J, Ewald U, Lackgren G, et al. Extreme short bowel syndrome in neonates: An indication for small bowel transplantation. Transplant Proc. 1992;24:1230–1235. [PubMed] [Google Scholar]
- 20.Goulet O, Revillon Y, Brousse N, et al. Successful small bowel transplantation in an infant. Transplantation. 1992;53:940–943. doi: 10.1097/00007890-199204000-00046. [DOI] [PubMed] [Google Scholar]
- 21.Calne RY, Sells RA, Pena, et al. Induction of immunological tolerance by porcine liver allografts. Nature. 1969;223:472–476. doi: 10.1038/223472a0. [DOI] [PubMed] [Google Scholar]
- 22.Kamada N, Davies HS, Wight D, et al. Liver transplantation in the rat: Biochemical and histological evidence of complete tolerance induction in non-rejector strains. Transplantation. 1983;35:304–311. [PubMed] [Google Scholar]
- 23.Todo S, Tzakis AG, Abu-Elmagd K, et al. Cadaveric small bowel and small bowel-liver transplantation in humans. Transplantation. 1992;53:369–376. doi: 10.1097/00007890-199202010-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Todo S, Tzakis AG, Abu-Elmagd K, et al. Intestinal transplantation in composite visceral grafts or alone. Ann Surg. 1992;216:223–234. doi: 10.1097/00000658-199209000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murase N, Demetris AJ, Matsuzaki T, et al. Long survival in rats after multivisceral versus isolated small bowel allotransplantation under FK506. Surgery. 1991;110:87–98. [PMC free article] [PubMed] [Google Scholar]
- 26.Yoshimi F, Nakamura K, Zhu Y, et al. Canine total orthotopic small bowel transplantation under FK506. Transplant Proc. 1991;23:3240–3242. [PMC free article] [PubMed] [Google Scholar]
- 27.Starzl TE, Todo S, Thomson AW, et al., editors. Proceedings of the First International Congress on FK506. Transplant Proc. 1991;23:2709–3375. [Google Scholar]
- 28.Mughal M, Irving M. Home parenteral nutrition in the United Kingdom and Ireland. Lancet. 1986;2:383–387. doi: 10.1016/s0140-6736(86)90065-6. [DOI] [PubMed] [Google Scholar]
- 29.Howard L, Heaphey L, Fleming CR, et al. Four years of North American Registry home parenteral nutrition outcome data and their implications for patient management. JPEN. 1991;15:384–393. doi: 10.1177/0148607191015004384. [DOI] [PubMed] [Google Scholar]
- 30.Dowling RH. Small bowel adaptation and its regulation. Scand J Gastroenterol. 1982;17 suppl 74:53–74. [PubMed] [Google Scholar]
- 31.Willmore DW. Factors correlating with a successful outcome following extensive intestinal resection in newborn infants. J Pediatr. 1972;80:88–95. doi: 10.1016/s0022-3476(72)80459-1. [DOI] [PubMed] [Google Scholar]
- 32.Postuma R, Morez S, Friesen F. Extreme short bowel syndrome in an infant. J Pediatr Surg. 1983;18:264–268. doi: 10.1016/s0022-3468(83)80096-7. [DOI] [PubMed] [Google Scholar]
- 33.Stokes MA, Irving MH. Mortality in patients on home parenteral nutrition. JPEN. 1989;13:172–175. doi: 10.1177/0148607189013002172. [DOI] [PubMed] [Google Scholar]
- 34.Grosfeld JL, Rescoria FJ, West KW. Short bowel syndrome in infancy and childhood: Analysis of survival in 60 patients. Am J Surg. 1986;151:41–46. doi: 10.1016/0002-9610(86)90009-7. [DOI] [PubMed] [Google Scholar]
- 35.Wolfe BM, Beer WH, Hayashi JT, et al. Experience with home parenteral nutrition. Am J Surg. 1983;146:7–14. doi: 10.1016/0002-9610(83)90251-9. [DOI] [PubMed] [Google Scholar]
- 36.Thompson JS, Rikkers LF. Surgical alternatives for the short bowel syndrome. Am J Gastroenterol. 1987;82:97–104. [PubMed] [Google Scholar]
- 37.Starzl TE, Todo S, Tzakis A, et al. The many faces of multivisceral transplantation. Surg Gynecol Obstet. 1991;172:335–344. [PMC free article] [PubMed] [Google Scholar]
- 38.Casavilla A, Selby R, Abu-Elmagd K, et al. Logistics and technique for combined hepatic-intestinal retrieval. Ann Surg. 1992;216:85–89. doi: 10.1097/00000658-199211000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Belzer FO, Southard JH. Principles of solid-organ preservation by cold storage. Transplantation. 1988;45:673–676. doi: 10.1097/00007890-198804000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Taguchi T, Zorychta E, Guttman FM. Evaluation of UW solution for preservation of small intestinal transplant in the rat. Transplantation. 1992;53:1202–1205. doi: 10.1097/00007890-199206000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Burgmann H, Reckendorfer H, Sperlich M, et al. Small bowel tissue high-energy phosphate alterations during hypothermic storage using different protecting solutions. Eur Surg Res. 1992;24:84–88. doi: 10.1159/000129192. [DOI] [PubMed] [Google Scholar]
- 42.Hamamoto I, Merhav H, Zhu Y, et al. Lipid peroxidation, brush border, and neutrophil enzyme activity after small bowel preservation: A comparison of preservation solutions. Transplant Proc. 1992;24:1095. [PMC free article] [PubMed] [Google Scholar]
- 43.Tzakis A, Todo S, Reyes J, et al. Piggyback orthotopic intestinal transplantation. Surg Gynecol Obstet. 1993;176:297–298. [PMC free article] [PubMed] [Google Scholar]
- 44.Tzakis A, Todo S, Starzl TE. Orthotopic liver transplantation with preservation of the inferior vena cava. Ann Surg. 1989;210:649–652. doi: 10.1097/00000658-198911000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Starzl TE, Porter KA, Francavilla A. The Eck fistula in animals and humans. Curr Probl Surg. 1983;20:692–745. doi: 10.1016/s0011-3840(83)80010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takaya S, Bronsther O, Iwaki Y, et al. The adverse impact on liver transplantation of using positive cytotoxiC crossmatch donors. Transplantation. 1992;53:400–406. doi: 10.1097/00007890-199202010-00026. [DOI] [PMC free article] [PubMed] [Google Scholar]