Recently, we described a one-year trial in which cadaver kidneys were assigned with a computerized point system to potential renal recipients on our waiting list.1 Factors weighed included waiting time, tissue matching, medical urgency, and graft preservation times. It has been suggested2 that a modification of this system could be used for equitable allocation of vital extrarenal organs. To assess this possibility, we have examined retrospectively our own experience with liver transplantation over an eight-month period beginning September 1, 1986. From this study, we have concluded that dispersal of livers and hearts can be guided by computer point scoring, but that physician judgment will be a much greater factor in the final decision than with renal transplantation. A proposal will be offered for a prospective trial.
CASE MATERIAL
Between September 1, 1986 and May 1, 1987, 162 primary liver transplantation and 55 retransplantations were performed at the University of Pittsburgh Health Science Center (Table 1), 77 at the Children’s Hospital of Pittsburgh, and 140 at the Presbyterian University Hospital. The mix of recipient blood types was similar to that in the general population (Table 1).
Table 1.
Liver Transplantations Performed Between September 1, 1986 and April 30, 1987
| Primary Grafts | Second Grafts | Third Grafts | Fourth Grafts | |
|---|---|---|---|---|
| Adults | 112 | 22 | 5 | 1 |
| Children | 50 | 23 | 4 | — |
| Total | 162 | 45 | 9 | 1 |
| Recipient blood group | ||||
| Type O | 67 | 25 | 4 | 1 |
| Type A | 72 | 11 | 1 | — |
| Type B | 18 | 6 | 3 | — |
| Type AB | 5 | 3 | 1 | — |
On September 1, 1986, 85 and 57 candidates were on the adult and pediatric lists respectively, for a total of 142. By the end of 8 months, the total had increased to 183, mainly because more adults waiting for O and A livers had been added so rapidly (Table 2).
Table 2.
Numbers of Candidates on the Liver Transplant Waiting List
| Sept. 1, 1986 | April 30, 1987 | Net Gain or Loss | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Recipient Blood Type | O | A | B | AB | O | A | B | AB | O | A | B | AB |
| Pediatric | 33 | 16 | 6 | 2 | 32 | 16 | 7 | 0 | −1 | 0 | +1 | −2 |
| Adult | 43 | 30 | 12 | 0 | 70 | 44 | 11 | 3 | +27 | +14 | −1 | +3 |
| Total | 76 | 46 | 18 | 2 | 102 | 60 | 18 | 3 | +26 | +14 | 0 | +1 |
MEDICAL URGENCY
Different liver diseases have variable profiles and rates of development. However, an accurate and simple six-stage severity scale has been defined by social and vocational invalidism in the first three classes, and by progressive dependence upon increasingly sophisticated hospital resources in the last three classes (Table 3). A more detailed analysis of symptoms, findings, biochemical abnormalities, and complications invariably identifies the same patients as in urgent need of a new liver. Very poor synthetic liver function, jaundice, serious coagulation disorders, hepatorenal syndrome, encephalopathy, ascites, variceal bleeding, wasting, and recurrent bacterial peritonitis are found in varying combinations in patients who become hospital bound.
Table 3.
Status of Prospective Liver Recipients
| Class | Definition |
|---|---|
| 1 | Working, in school, growing infant |
| 2 | Confined to home, self–care, not thriving but stable (infant) |
| 3 | Home, requiring professional care, losing developmental ground (infant) |
| 4 | Hospital bound, not in intensive care unit (ICU) |
| 5 | ICU bound |
| 6 | In ICU, unconscious, ventilator |
NOTE. The classes can be used to calculate medical urgency points (see text).
Table 4 shows the urgency status at the time the 162 transplantations were carried out over an eight-month period. More than two thirds of the operations were performed after the patients had deteriorated to the point of requiring chronic hospitalizaiton; and in 37.7% of the total cases, the recipients had entered the lethal classes 5 and 6 from which even short-term survival was not possible without transplantation.
Table 4.
Candidate Status at Time of 162 Transplantations
| Urgency Class | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Primary grafts | ||||||
| Pediatric | 0.0% | 0.0% | 70.8% | 14.6% | 14.6% | 0.0% |
| Adult | 0.0% | 0.9% | 28.6% | 42.9% | 18.7% | 8.9% |
| Retransplants | ||||||
| Pediatric | 0.0% | 0.0% | 11.1% | 18.5% | 22.2% | 48.2% |
| Adult | 0.0% | 0.0% | 0.0% | 14.3% | 21.4% | 64.3% |
| Total | 0.0% | 0.5% | 32.0% | 29.8% | 18.6% | 19.1% |
The high rate of emergency transplantation reflected our long-held position that the sickest patients should be treated first. As a result, some reasonable candidates in classes 2, 3, or 4 were forced to wait until they deteriorated into classes 5 and 6 before action was taken. Forty-six patients who were on the waiting list on September 1, 1986, or who were entered during the next 8 months, died in the waiting period (Table 5), invariably with complications of hepatic failure. Usually, infectious complications of the lung or elsewhere had supervened, interdicting last minute attempts at emergency liver replacement. In most such instances, the patients were referred very late in the course of their disease; but some were among those who deteriorated while waiting.
Table 5.
Deaths of Patients Waiting for Liver Transplantation Between September 1, 1986 and April 30, 1987
| Died | |
|---|---|
| Pediatric | 13/118 = 11.02% |
| Adults | 33/273 = 12.1% |
| Total | 46/391 = 11.76% |
PROPOSED PRINCIPLES INVOLVED IN EQUITABLE ALLOCATION
Regional Primacy
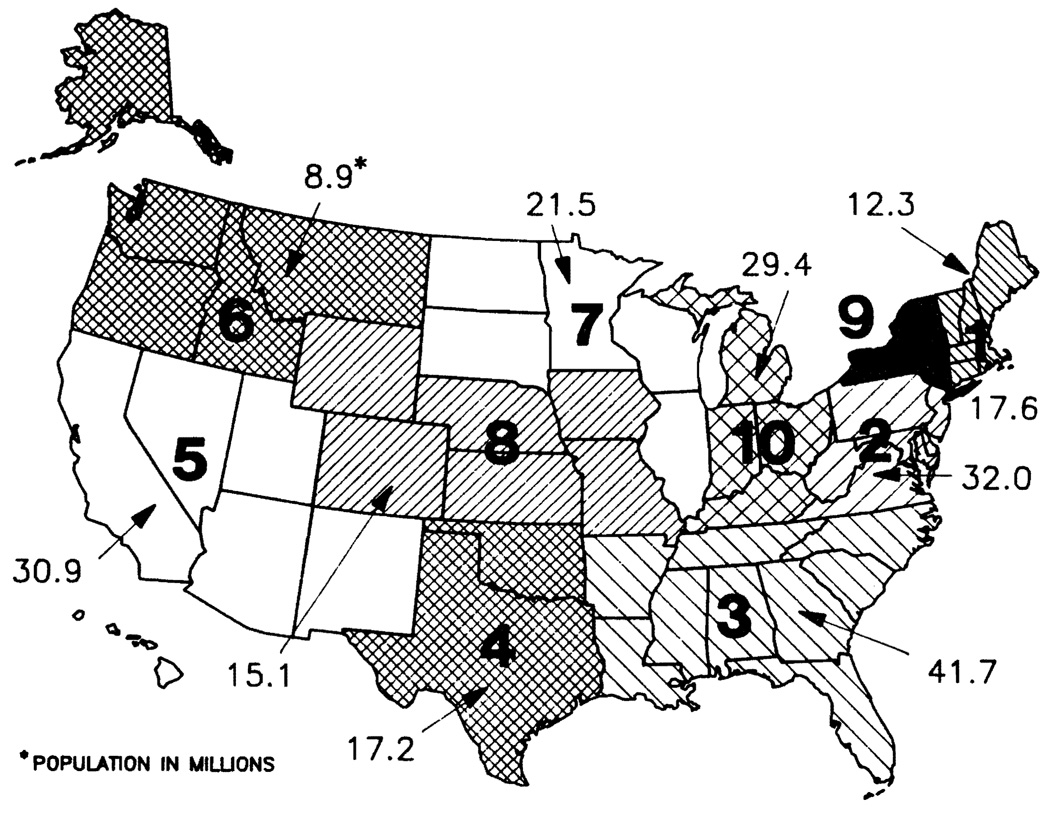
Development of a national network for equitable allocation of organs has become the contractual legal obligation of the United Network for Organ Sharing (UNOS), a previously private and voluntary organization. UNOS consists of ten regions with the geographic confines and population bases shown in Fig 1. Within each region, procurement organizations already exist with service areas that range from large to small both geographically and in terms of population. The heterogeneity of these areas within regions precludes the imposition of a uniform administrative structure upon all.
Fig 1.
UNOS regions. Note that Hawaii is in region 5.
However, each of the regions is large enough to serve as a self-contained unit within the confederation of ten. When organs become available within a region, responsibility for the equitable allocation process will begin with the area procurement agency. The first option for liver distribution should be within the area of procurement, using the point system to identify the appropriate recipients from the pool of candidates. Areas within a given region may already have organ sharing arrangements which can be perpetuated or improved, providing the point system is used to identify the recipients within the consortium arrangement. Livers still unused after the local possibilities are exhausted will be offered to all qualified liver transplant centers in the region, once more using the point system. Area and regional computer facilities will expedite the process.
By giving the local areas and the region the first option for use, two noteworthy objectives are met. First, the local incentives for effective organ procurement will be retained, driven by the knowledge that patients on area and regional waiting lists can be expected to benefit preferentially from regional efforts. Second, the average duration of ischemia will be kept to a minimum by preferential local and regional utilization. The latter consideration is of the utmost practical importance, as emphasized by Rapaport,2 since the acceptable limit of preservation ischemia for the liver is so short.
At the same time, wastage of organs will be avoided by promptly entering the livers not used in the originating region into a national reservoir and by allocating these organs to recipients in the other nine regions, according to the same point system used locally and regionally. This will be done through the UNOS national computer which will have records of all candidates in the United States.
It is probable that Canada can be recruited into the plan, treating that country as region 11. The principle of regional primacy would allow Canada the autonomy which its sovereign status requires for development of its own national sharing plan, but with provision to send out superfluous livers, or with organ flow in the opposite direction, to receive these from the United States under reasonable and defined guidelines. Since Canada and the United States have been historical partners in organ sharing, provisions to encourage collaboration will be of the greatest importance. The possibility must be left open of creating liaisons to other countries, especially Mexico.
Physician Responsibility
When a liver is offered in a local area, regionally, or nationally, the decision whether to use the organ will remain the prerogative of the transplant surgeon and/or physician responsible for the care of the patient. This will allow those entrusted with the treatment of the recipient to exercise their best judgment about the suitability of the organ being offered for their specific patient, and to be faithful to their personal or programatic philosophy about such controversial matters as the importance of ABO matching, preformed antibody index, permissible limits of cold ischemia, and anatomic anomalies of the donor or recipient liver. In addition, the prospective recipient’s medical condition at that moment can be given proper consideration in the decision whether to proceed. If a negative decision about the use of a donor liver is made for a given recipient, all that will be required is a physician notation for the UNOS record about why a liver was passed up.
Physicians will be urged to explain this system to their patients since the success of the system will depend upon its openness. All patients on the list (or their familes) should be able to know where they stand on the list, if there are unusual difficulties that make finding a suitable liver difficult, if they have been passed over, and if so, why and by whom.
Patient Free Choice and Rights
It should be the responsibility of UNOS to make public the regional and national locations of liver transplantation programs, and the program directors. In this way, prospective recipients can develop options to area or regional care if that is what they or their families desire.
If such patient choice is not made explicit in a national program that stresses regionalization, a dehumanizing element can be introduced unconsciously into captive practices that are engendered by stipulated monopolies. For example, prospective recipients on a liver waiting list may feel that they cannot be demanding, express dissatisfaction, or deviate in any way from docile behavior for fear of jeopardizing their candidacy. There are few things more degrading to patients than to be treated as custodial cases. In the event that there is high patient dissatisfaction in a given area or region, the consequent shrinkage of the recipient waiting lists would diminish the consumption of organs in that region and result in the shipment of left-over organs to other localities to which migration of recipients could occur.
FACTORS IN POINT SCORE
Preliminary Stratification
Size
The acceptable donor size for each individual patient should be determined by the responsible recipient surgeon. Normal liver size in the human is about 2.4% of body weight; but the liver size in the end stage hepatic diseases may be decreased, increased, or normal. Precise estimates of liver size can be obtained with ultrasonography or computerized axial tomography (CAT).4 With this information a donor size range appropriate for the individual recipient can be stipulated for listing locally, regionally, or nationally.
Cytotoxic antibody crossmatch
In the previously described renal allocation plan,1 a negative cytotoxic crossmatch connoting the absence of antidonor cytotoxic antibodies was a necessary condition for candidacy for local kidneys or for kidneys shipped in from outside regions. The presence of a positive crossmatch in liver cases has not significantly influenced the outcome.5 Thus, this test is not used to cull recipients from candidacy for a given donor.
ABO Points
Under ordinary circumstances, the donor and recipient should be of the same ABO type. Thus, liver candidates are listed under blood groups O, A, B, or AB. Nevertheless, it is known3 that livers can be transplanted, although somewhat less successfully, from donors with different but compatible blood types (eg, O to A) and from incompatible donors (eg, A to O). Therefore, transplantation is not precluded under the latter circumstances. However, removal of credit points for failure to achieve ABO identity will make it more difficult to obtain the organs.
Recipients with the same ABO type as the donor arc awarded ten points. Those with compatible but not identical types are given five points, and those with incompatible types are given no points. In the example shown in Table 6 in which the donor was O blood type, the recipients given five points were A, B, or AB.
Table 6.
Liver Transplantation Candidate Selection
| Patient | Days Waiting |
Rank Order* |
Points for Waiting |
ABO Match Points |
Urgency | Donor Distance Points |
Location Patient Waiting |
Recipient Distance Points |
Total Points |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Class | Points | |||||||||
| EB | 550 | 23 | 8.213 | 5 | 6 | 24 | 0 | PUH | 6 | 43.213 |
| RF | 100 | 7 | 2.500 | 10 | 6 | 24 | 0 | PUH | 6 | 42.500 |
| KF | 368 | 20 | 7.142 | 10 | 4 | 16 | 0 | PUH | 6 | 39.142 |
| CE | 284 | 17 | 6.071 | 10 | 4 | 16 | 0 | PUH | 6 | 38.071 |
| RW | 913 | 28 | 9.999 | 10 | 3 | 12 | 0 | KY | 5 | 36.999 |
| JS | 529 | 21 | 7.499 | 10 | 3 | 12 | 0 | OH | 5 | 34.499 |
| DB | 913 | 28 | 9.999 | 10 | 2 | 8 | 0 | NJ | 5 | 32.999 |
| DO | 261 | 15 | 5.357 | 10 | 3 | 12 | 0 | NJ | 5 | 32.357 |
| SN | 319 | 19 | 6.785 | 10 | 3 | 12 | 0 | FL | 2 | 30.785 |
| CB | 143 | 10 | 3.571 | 10 | 3 | 12 | 0 | PA | 5 | 30.571 |
| HC | 53 | 4 | 1.428 | 10 | 3 | 12 | 0 | Pittsburgh | 6 | 29.428 |
| LB | 312 | 18 | 6.428 | 10 | 2 | 8 | 0 | WV | 5 | 29.428 |
| DG | 121 | 9 | 3.214 | 10 | 3 | 12 | 0 | GA | 3 | 28.214 |
| NC | 268 | 16 | 5.714 | 5 | 3 | 12 | 0 | OH | 5 | 27.714 |
| NS | 536 | 22 | 7.856 | 10 | 1 | 4 | 0 | PA | 5 | 26.856 |
| MD | 219 | 12 | 4.285 | 5 | 3 | 12 | 0 | WV | 5 | 26.285 |
| EB | 193 | 11 | 3.928 | 5 | 3 | 12 | 0 | NY | 5 | 25.928 |
| HB | 2 | 1 | 0.357 | 10 | 3 | 12 | 0 | GA | 3 | 25.357 |
| BB | 60 | 5 | 1.786 | 10 | 2 | 12 | 0 | CA | 0 | 23.786 |
| SL | 881 | 25 | 8.928 | 5 | 1 | 4 | 0 | VA | 5 | 22.928 |
| ML | 254 | 13 | 4.642 | 5 | 2 | 8 | 0 | PA | 5 | 22.642 |
| CK | 613 | 24 | 8.570 | 5 | 1 | 4 | 0 | PA | 5 | 22.570 |
| JP | 913 | 28 | 9.999 | 5 | 1 | 4 | 0 | AR | 3 | 21.999 |
| PL | 109 | 8 | 2.857 | 5 | 3 | 12 | 0 | OK | 2 | 21.B57 |
| IF | 88 | 6 | 2.143 | 5 | 3 | 12 | 0 | FL | 2 | 21.143 |
| DD | 18 | 3 | 1.071 | 10 | 2 | 8 | 0 | WA | 0 | 19.071 |
| PL | 254 | 14 | 4.999 | 5 | 1 | 4 | 0 | PA | 5 | 18.999 |
| GH | 17 | 2 | 0.714 | 10 | 1 | 4 | 0 | GA | 3 | 17.714 |
Abbreviations: PUH, Presbyterian University Hospital; other location abbreviations indicate states.
Highest number = longest wait
Time Waiting
Recipients are listed in order of their acceptance to candidacy by the local selection committee, thereby automatically establishing a rank order waiting list. The person waiting the longest is given ten points, the patient in the middle of the rank order is awarded five points, and those with the shortest waits receive the lowest scores (Table 6).
Medical Urgency
For each patient, medical urgency is determined for class 1 (least urgent) to class 6, determined by the criteria shown in Table 3 and discussed earlier. Four points are given for each level of urgency. Thus, a patient in class 1 should get four points and someone in class 6 would receive twenty-four points. Examples are shown with an actual recent case in Table 6.
Logistic (Distance) Factors
Short duration of preservation time, the practicality of coordinating the complex transplantation process, and the cost of these arrangements are roughly proportional to how far the donors and recipients are from the transplant center involved. Thus, logisitc points are granted both for the donor and recipient.
The donor points are the same for all candidates at a given transplant center for the liver from that donor (Table 7). If a donor is within 50 miles of the transplant center involved, 12 logistic points are given to all potential recipients. For each succeeding 500 mile radius, two points are removed (Table 7). Thus, ten points would be given if a donor were 400 miles away, and eight points if the distance were 600 miles. Beyond 2500 miles, no points are given (Table 7).
Table 7.
Points Awarded for Proximity of Donor and Recipient to Center Where Transplant Is to Be Performed
| Distance From Center (miles) | Points From Donor | Points From Recipient |
|---|---|---|
| 0–50 | 12 | 6 |
| 50–500 | 10 | 5 |
| 500–1000 | 8 | 4 |
| 1000–1500 | 6 | 3 |
| 1500–2000 | 4 | 2 |
| 2000–2500 | 2 | 1 |
| >2500 | 0 | 0 |
Mileage points also are given to recipients for the proximity of their holding area to the transplant center; but the scale is only half as generous. Patients living locally are given six points, and for every 500 mile increment away from Pittsburgh (or whatever the transplant center is) one point is subtracted (Table 7). Zero points are given for patients whose place of waiting is greater than 2500 miles away from their transplant center (Table 7).
EXAMPLE OF POINT SYSTEM USE
On May 1, 1987, a young woman of O blood type who weighed 130 pounds was pronounced brain dead in Portland, Oregon. A need for the liver was not identified on the West Coast and the liver was offered to the Pittsburgh program. Twenty-eight recipients on the Pittsburgh waiting list were in the 125 to 135 pound weight range which was selected for purposes of illustration. Because of the location of the donor, no logistic points were given to the recipients for donor distance; but a full range of zero to six points was given because of varying proximity of the recipients to Pittsburgh. Seventeen of the 28 candidates who were O blood type were given ten points for blood group identity, and the other 11 were given five points for ABO compatibility. ABO incompatibility was not a possible condition since O blood group humans are universal tissue donors.6
Medical urgency points were highly variable, but the two most seriously ill patients with class 6 medical urgency were at the top of the list. Patients 3 and 4 whose urgency status was class 4 were not far behind in total points; their candidacy was advanced by their location in Pittsburgh and by long waiting times.
Physician judgment governed the final decision to treat the second patient on the list. The reason was that the number one candidate was of a different blood type (A) than the donor, a situation that depreciates survival by about 10%.3 The matter became moot because permission for donation was withdrawn in Oregon. An A donor was found within 24 hours for the first choice, and one day later, an O liver was found for the second patient.
DISCUSSION
The concept of the point system for liver allocation is the same as that already proposed for kidneys,1,2 but with a far greater emphasis on medical urgency and logistic factors. Nevertheless, the waiting time can be influential, especially when a patient’s condition deteriorates while waiting if this fact is recorded with a class change in medical urgency. A sliding scale is thereby created in which it is progressively easier to obtain a liver as the disease becomes worse, and as the time waiting is prolonged.
The Pittsburgh liver transplantation program has been a good workshop to develop a plan for national allocation of extrarenal organs. The waiting list has been large enough so that usually there have been multiple candidates of appropriate size for a given liver. The potential recipients have come from all parts of the continental United States and beyond its borders, making it possible to examine the relationship between regional, national, and international obligations in the context of organ supply. Finally, we have trained most of the teams doing liver transplantation in North America and have had a consequent special interest in promulgating, not restricting, the orderly application of this revolutionary development in hepatology.
The allocation plan for livers that we are proposing does not provide impractical answers to questions about organ distribution or impose unsound or unethical practices. It is based on the principles of ultimate physician responsibility for decisions involving individual patient care, regional primacy for organ use, and protection of patients’ rights including free selection of services.
Of these principles, physician responsibility may be the most important. It was astonishing in the 8 months which were examined how often last minute decisions were required because of unexpected findings at the donor operation or because of volatile circumstances with the recipient candidate whose condition sometimes changed from hour to hour. The plan does not require blind adherence to a formula, but only a sensible explanation if the guidelines that translate into point totals are not followed.
Regional primacy as a principle of organ allocation will have a major impact upon the eventual shape of the national network. If the regions are to be meaningful, they will have to be the same for all organs. Although an argument could be made even now to divide the excessively large region 3 into two separate parts, those regions already delineated by UNOS (Fig 1) should be retained for the moment. Otherwise, frantic efforts during the next year or so are apt to be made to gerrymander functional procurement regions for specific organs by agreements between procurement organizations, surgical groups, or other interested parties. If these efforts were to succeed, the effect could be enforced movement of recipients to centers which have successfully negotiated agreements counter to the spirit of the 1984 and 1986 Organ Transplantation Acts.
In the long run, the practice of regional primacy for organ allocation theoretically should result in the largest, or at least the most numerous, liver transplant centers being in the most heavily populated regions. If this does not occur, it will be an expression of dissatisfaction by the recipients who will have joined the waiting lists in other regions, thereby reducing organ consumption in the original region, and creating a draw on spill-over organs from that region. Then, centers of genuine excellence in smaller population areas can build their own lists and compete with the traditional tools of quality service and the improvements of care that can be engendered by effective research and development programs.
The efficient and fair deployment of such livers in other regions using the point system will go a long way toward correcting a potential peril of creating limited numbers of potentially monopolistic regional recipient centers as has been proposed by a number of planning agencies, but opposed by Rapaport.2
It will never be possible to impose detailed candidacy criteria upon recipient health care teams. Some programs may systematically exclude candidates because of age, advanced disease, extrahepatic complications of end stage liver disease, previous abdominal operations, history of alcohol or substance abuse, or other factors which are known or assumed to degrade results. Then, patients may be deprived of the right to be treated near their own homes.7 Even worse, the insurance carriers in that region, including government agencies, may refuse to allow treatment outside the region on grounds of certified noncandidacy. The free movement of these patients to programs willing to care for them should not be inhibited, since artificial livers are not available as an option to liver replacement. The only alternative is death.
The same allocation plan used for livers should be applicable for heart programs, the only difference being in the classification of medical urgency (Table 8). For highly sensitized potential heart recipients with cytotoxic antibodies against a significant percent of the human population, a negative cytotoxic cross with donor lymphocytes may be required before proceeding with transplantation. Otherwise, the same computer scoring could be used as that for the liver.
Table 8.
Medical Urgency Used for Heart Recipients
| Class | Definition |
|---|---|
| 1 | Working |
| 2 | Home bound, self–care |
| 3 | Home bound with attendant |
| 4 | Hospital bound |
| 5 | Hospital bound, intravenous inotropic drugs |
| 6 | Mechanical assist devices for survival |
SUMMARY
A national plan is proposed for the equitable allocation of extrarenal organs, with particular reference to the liver. The principles of the plan include preferential use of the organs in the local and regional area of procurement, with national listing of the organs left over after the original cut. At each of the local, regional, and national levels, the allocation is based on total points awarded for medical urgency, time waiting, blood group conformity, and physical location of both donor and recipient. The plan, which should be applicable as well for allocation of hearts, is compatible with international sharing with nearby countries such as Canada.
Acknowledgments
Supported by Research Grants from the Veterans Administration and Project Grant No. AM-29961 from the National Institutes of Health, Bethesda, MD.
REFERENCES
- 1.Starzl TE, Hakala T, Tzakis A, et al. JAMA. 1987;257:3073. [PMC free article] [PubMed] [Google Scholar]
- 2.Rapaport FT. JAMA. 1987;257:3118. [PubMed] [Google Scholar]
- 3.Gordon RD, Iwatsuki S, Esquivel CO, et al. Surgery. 1986;100:342. [PubMed] [Google Scholar]
- 4.Van Thiel DH, Hagler NG, Schade RR, et al. Gastroenterology. 1985;88:1812. doi: 10.1016/0016-5085(85)90005-8. [DOI] [PubMed] [Google Scholar]
- 5.Gordon RD, Fung JJ, Markus B, et al. Surgery. 1986;100:705. [PMC free article] [PubMed] [Google Scholar]
- 6.Starzl TE. Experience in Renal Transplantation. Philadelphia: Saunders; 1964. p. 37.p. 249.p. 317. [Google Scholar]
- 7.Lundberg GD. JAMA. 1983;250:2966. [PubMed] [Google Scholar]