Since the first human liver transplantation in Denver on March 1, 1963, numerous refinements in surgical techniques and in perioperative care have been made, the mechanism of graft rejection has been more precisely understood, and safer and more effective immunosuppressive agents have been discovered.1–3 Now, in 1987, it is well accepted that liver transplantation is often the only effective therapy for many advanced liver diseases.
We will report here, as a landmark of our continuing efforts, the survival of patients with various end-stage liver diseases after liver transplantation from our own experience in 1,000 hepatic homograft recipients under cyclosporine-steroid therapy.
CASE MATERIALS AND METHODS
Since the introduction of cyclosporine-steroid therapy for our liver recipients in March 1980, 1,000 patients received liver homografts for various end-stage liver diseases by July 1987 at our institutes in Denver (in 1980), in Pittsburgh (since 1981), and Dallas (since 1985).
Of the 1,000 liver recipients, 666 were adults of age 18 years or older, and 334 were children of the ages younger than 18 years. The youngest liver recipient was 26 days old, and the oldest one was 76 years old at the time of transplantation. The numbers of patients in various age groups are listed in Table 1.
Table 1.
Number of Patients in Various Age Groups, and 1- to 5-Year Survival Rates
| Actuarial Survival (%) | ||||||
|---|---|---|---|---|---|---|
| Age (yr) | No. Patients | 1 year | 2 years | 3 years | 4 years | 5 years |
| 0–1 | 30 | 63 | 55 | 49 | 37 | 37 |
| 1–2 | 40 | 66 | 66 | 66 | 66 | 66 |
| 2–3 | 48 | 70 | 68 | 65 | 65 | 65 |
| 3–4 | 35 | 71 | 68 | 68 | 68 | 68 |
| 4–5 | 29 | 58 | 58 | 58 | 58 | 58 |
| 5–10 | 84 | 78 | 74 | 72 | 72 | 68 |
| 10–18 | 68 | 80 | 79 | 76 | 76 | 76 |
| 18–30 | 128 | 77 | 73 | 66 | 58 | 58 |
| 30–40 | 160 | 77 | 75 | 70 | 64 | 60 |
| 40–50 | 209 | 75 | 73 | 70 | 70 | 70 |
| 50–60 | 121 | 76 | 70 | 61 | 61 | 61 |
| 60–70 | 47 | 59 | 56 | 56 | — | — |
| 70 and older | 1 | 100 | — | — | — | — |
The liver diseases of adult recipients and those of pediatric recipients are listed in Table 2 and Table 3, according to the incidence. Three most common liver diseases among adult recipients were (1) postnecrotic cirrhosis (including chronic active hepatitis and cryptogenic cirrhosis), (2) primary biliary cirrhosis, and (3) primary sclerosing cholangitis. Those of pediatric recipients were (1) biliary atresia (including extrahepatic and intrahepatic type, biliary hypoplasia and Alagille’s syndrome), (2) liver-based inborn metabolic errors (alpha-1-antitrypsin deficiency disease, Wilson’s disease, tyrosinemia, and others), and (3) postnecrotic cirrhosis.
Table 2.
Liver Diseases of Adult Recipients
| Disease | No. Patients |
|---|---|
| Cirrhosis (postnecrotic, cryptogenic, alcoholic) | 278 |
| Postnecrotic and cryptogenic | 237 |
| HBsAg positive | 36 |
| Alcoholic | 41 |
| Primary biliary cirrhosis | 165 |
| Primary sclerosing cholangitis | 74 |
| Liver-based inborn metabolic errors | 35 |
| (Alpha-1-antitrypsin deficiency, Wilson’s, etc) | |
| Primary hepatic malignancy | 33 |
| Fulminant hepatic failure | 27 |
| Secondary biliary cirrhosis | 13 |
| Budd-Chiari syndrome | 13 |
| Bile duct cancer | 10 |
| Secondary hepatic malignancy | 7 |
| Others* | 11 |
Cystic fibrosis (3), adenomatosis (2), biliary atresia, cryptococcal cholangitis, congenital hepatic fibrosis, polycystic disease, trauma, lymphoangiomatosis.
Table 3.
Liver Diseases of Pediatric Recipients
| Diseases | No. Patients |
|---|---|
| Biliary atresia | 179 |
| Liver-based inborn metabolic errors | 63 |
| (Alpha-1-antitrypsin deficiency. Wilson’s, etc) | |
| Cirrhosis (postnecrotic and cryptogenic) | 39 |
| Familial cholestatic syndrome | 15 |
| Fulminant hepatic failure | 13 |
| Secondary biliary cirrhosis | 7 |
| Congenital hepatic fibrosis | 7 |
| Primary hepatic malignancy | 3 |
| Budd-Chiari syndrome | 2 |
| Neonatal hepatitis | 2 |
| Others* | 4 |
Primary sclerosing cholangitis, trauma, focal nodular hyperplasia, inflammatory pseudotumor.
The survival data were analyzed as of September 1, 1987, using the method of Kaplan-Meier. The statistical comparisons were made by the methods of Breslow and of Mantel-Cox. The difference was considered as significant when the P value was less than .05.
RESULTS
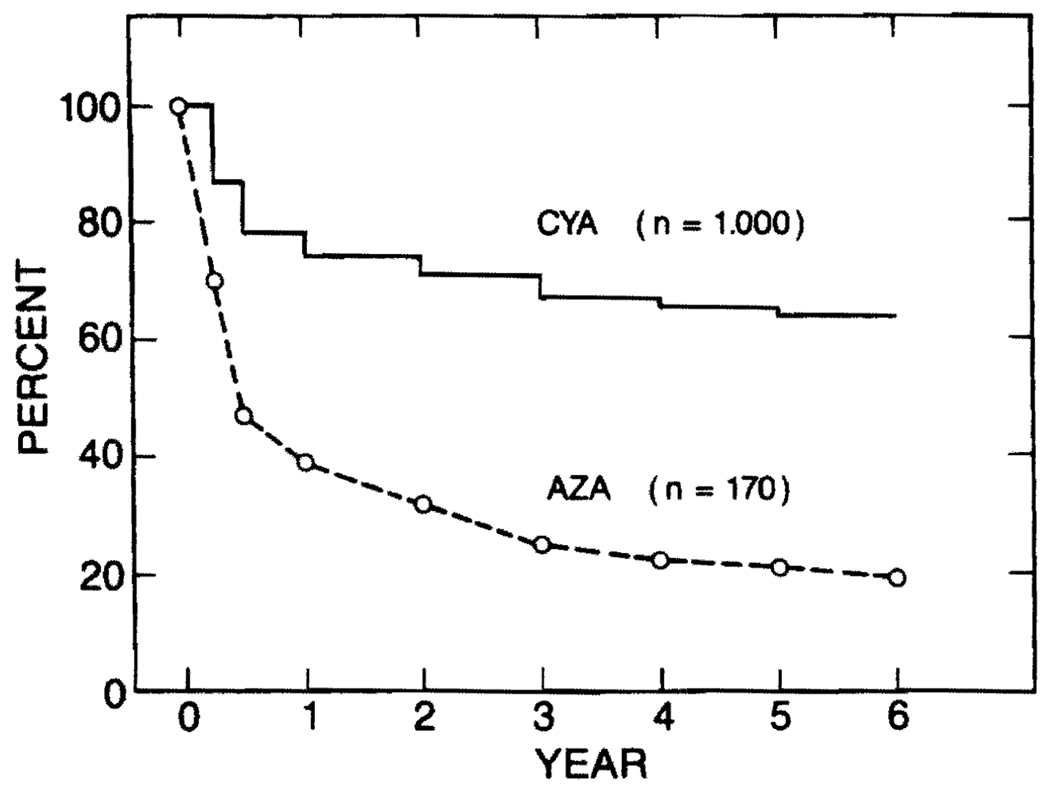
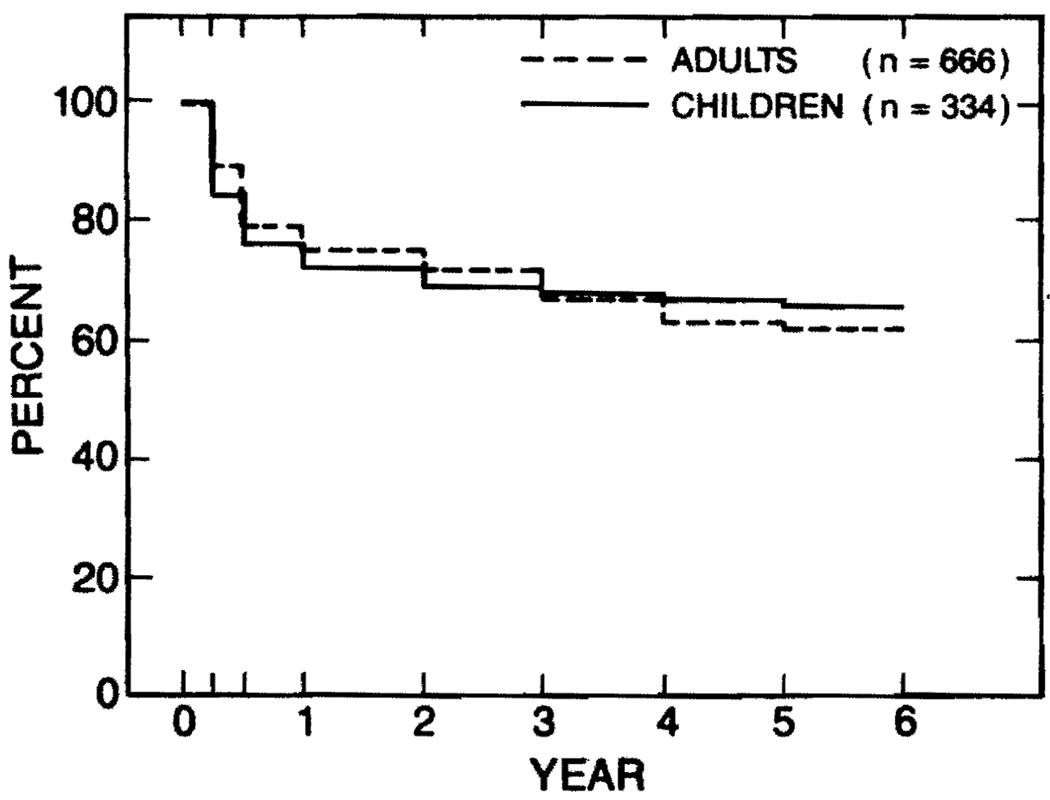
Overall survival rates of the 1,000 recipients treated with cyclosporine-steroid therapy were three times higher than those of 170 patients treated with azathioprine-steroids before 1980. One- to 5-year survival rates were 74%, 71%, 67%, 65%, and 64%, respectively, as shown in Fig 1. Five percent to 10% survival superiority of the pediatric recipients had existed for pediatric recipients during the azathioprine era before 1980. Since 1981, the survival rates of adult and of pediatric recipients are identical under cyclosporine-steroid therapy (Figure 2).
Fig 1.
Overall actuarial survival rates of 1,000 patients treated with cyclosporine-steroid therapy in comparison with overall actual survival rates of 170 patients treated with azathioprine-steroids therapy.
Fig 2.
Nearly identical survival rates between 666 adult recipients and 334 pediatric recipients since 1980.
The survival rates of various age groups of recipients were compared in Table 1. The survival rates of children under the age of 1 year and those of adults aged 60 years or older were significantly lower than overall survival rates of pediatric and adult recipients, respectively.
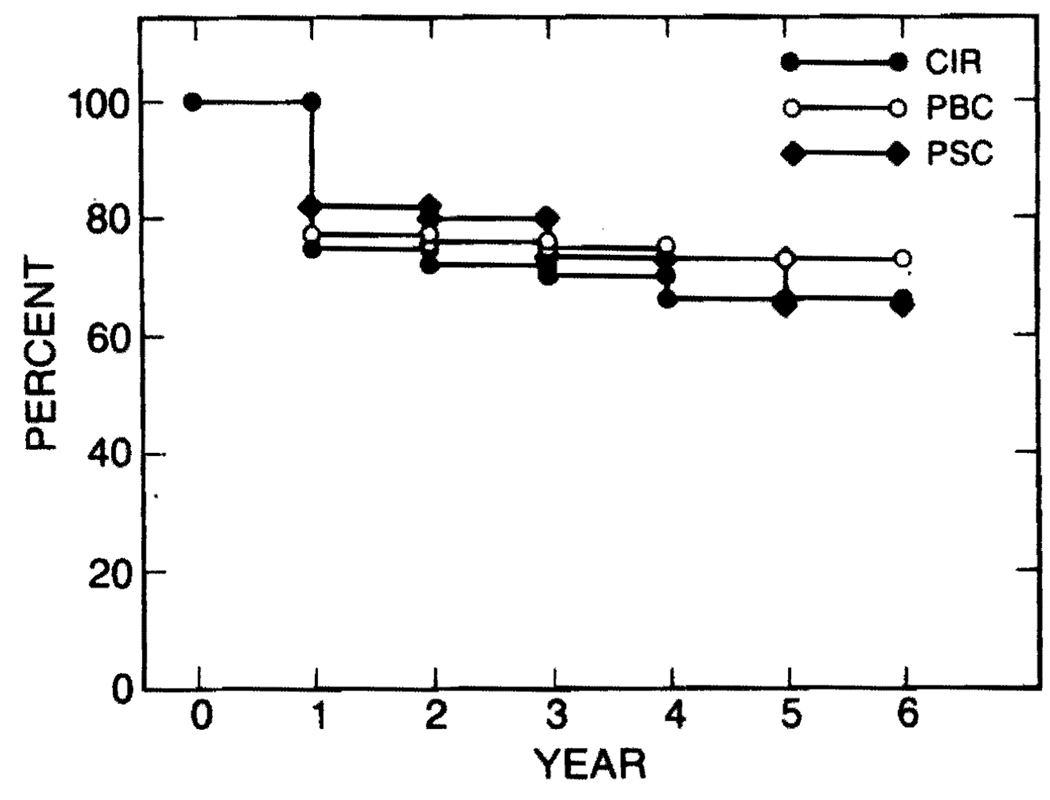
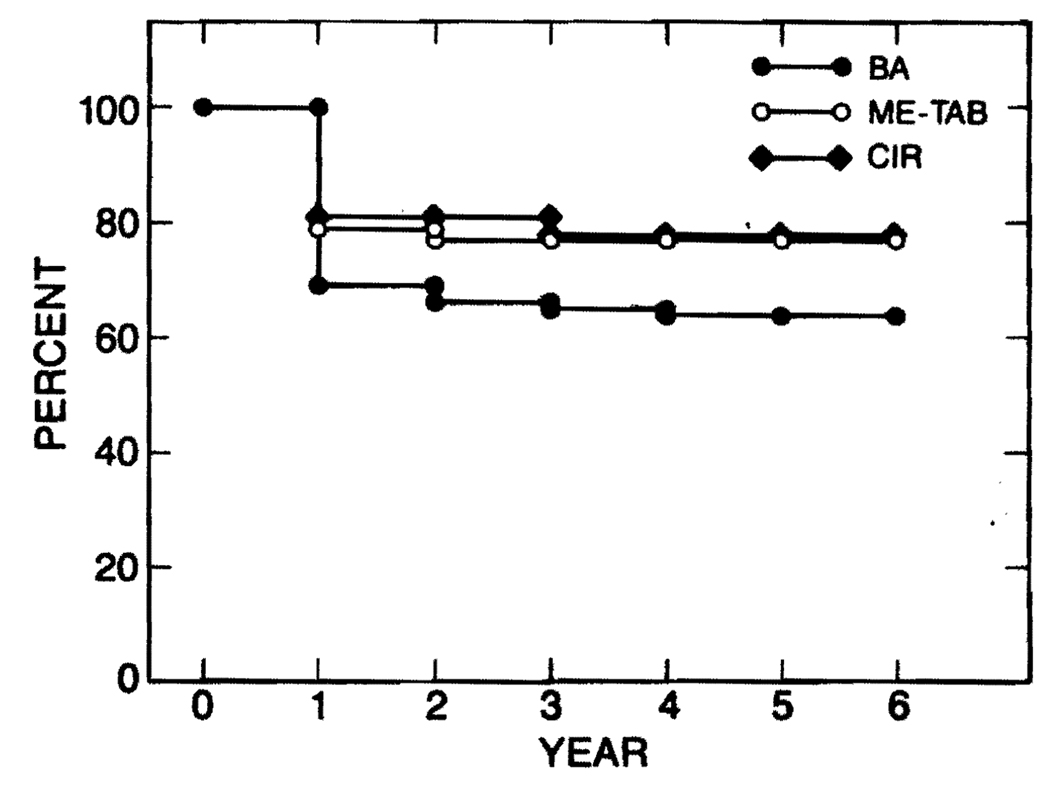
The survival rates were compared among three most common liver diseases of adult recipients (Fig 3) and among those of pediatric recipients with different diseases (Fig 4). Survival rates of adult recipients who had postnecrotic or cryptogenic cirrhosis, those with primary biliary cirrhosis, and those of primary sclerosing cholangitis were nearly identical (Fig 3). In pediatric recipients, survival rates of children with biliary atresia, those of liver-based inborn metabolic errors, and those of postnecrotic or cryptogenic cirrhosis were also similar (Fig 4).
Fig 3.
Survival comparison among adult recipients with three most common diseases (postnecrotic cirrhosis, primary biliary cirrhosis, and primary sclerosing cholangitis) did not show any statistical difference.
Fig 4.
Survival rates of pediatric recipients with liver-based inborn metabolic errors were nearly identical to those with postnecrotic or cryptogenic cirrhosis. Survival rates of children with biliary atresia were slightly lower than the other two diseases, but the difference was not statistically different.
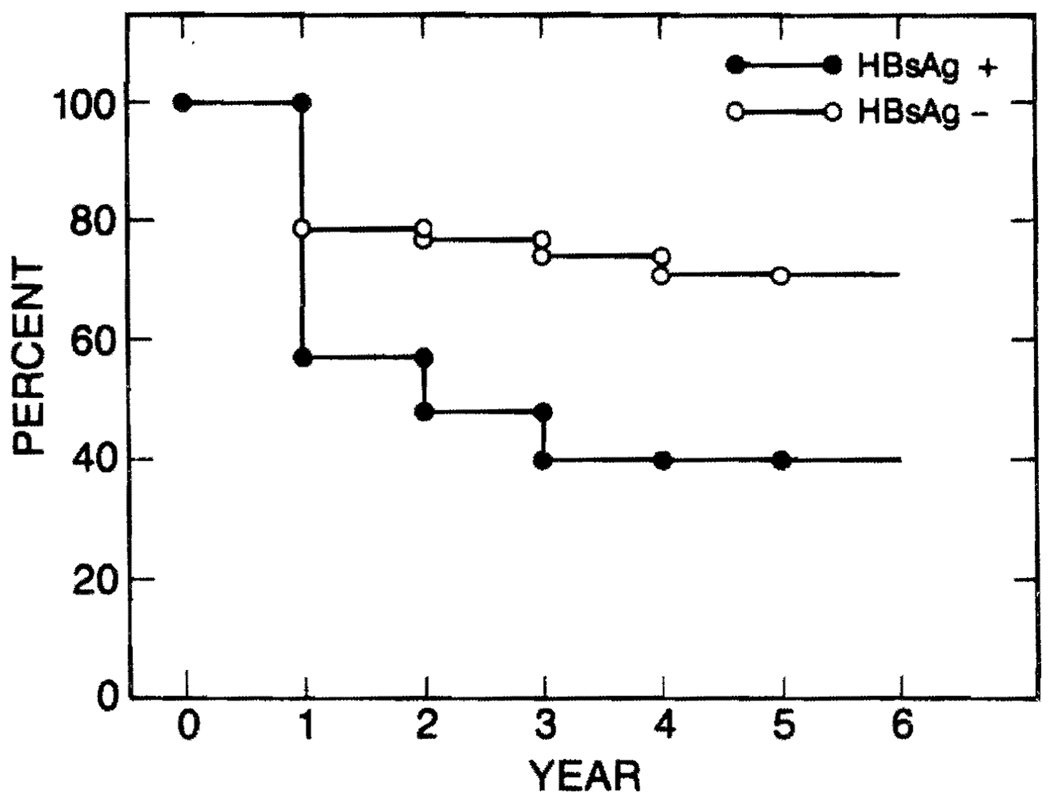
The influence of hepatitis B antigen (HBsAg) upon survival after liver transplantation and the recurrence of hepatitis B in the graft liver were studied. Among 276 recipients who had postnecrotic or cryptogenic cirrhosis, 36 patients were positive for HBsAg and the remaining 240 were negative for HBsAg before transplantation. One- to 5-year survival rates of B virus carriers were 57%, 48%, 40%, 40%, and 40%, and those without the carrier state were 78%, 77%, 74%, 71 %, and 71 %. Thus, survival rates of the patients with HBsAg were significantly worse than those of the patients without HBsAg (Fig 5).
Fig 5.
Survival rates of patients with HBsAg-positive, postnecrotic cirrhosis were significantly lower than those with HBsAg-negative postnecrotic cirrhosis.
Recurrence of hepatitis B was examined among 24 patients who had had HBsAg-positive postnecrotic cirrhosis before transplantation and who survived more than 3 months after transplantation. Five of the 24 patients died between 4 and 15 months, and four of the five died because of recurrent hepatitis B. Eleven of the 24 patients are alive between 6 months and 6 years with or after recovery from hepatitis B recurrence. Eight of the 24 patients are alive without recurrence between 4 and 12 months. Only one patient has become HBsAg negative after transplantation during a short observation period of 7 months. This patient had perioperative alpha interferon therapy.
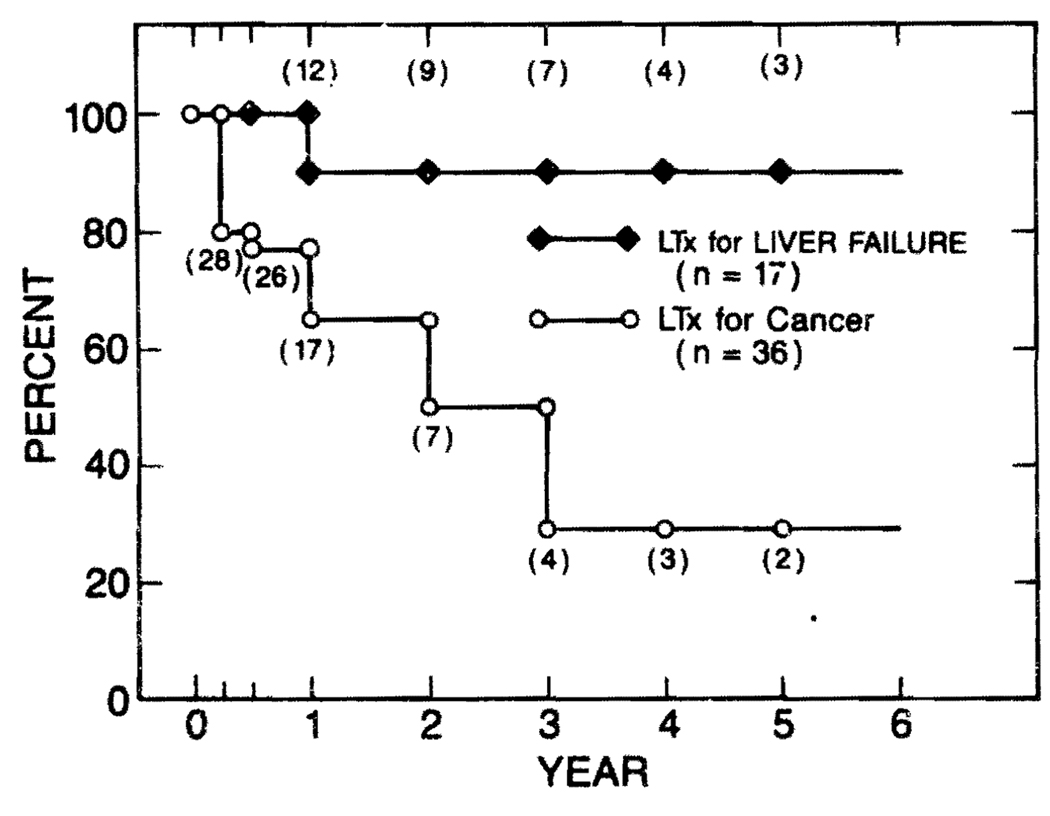
Fifty-three of the 1,000 patients received liver transplantation in the presence of primary hepatic malignancy other than bile duct carcinoma. Transplantation for 36 of these 53 patients was primarily to treat advanced hepatic malignancy that could not be resected by conventional techniques of subtotal hepatectomy. Eighteen of the 36 patients had hepatoma, eight had fibrolamellar hepatoma, eight had epitheloid hemangioendothelioma, one had cholangiosarcoma, and another had angiosarcoma.
For 17 of the 53 patients, liver transplantation was primarily to treat liver failure, and the malignant neoplasm in the diseased liver could have been resected by subtotal hepatectomy, if the liver was not terminally diseased. Fifteen of these 17 patients had hepatoma, one had fibrolamellar hepatoma and another had mixed cholangiohepatoma.
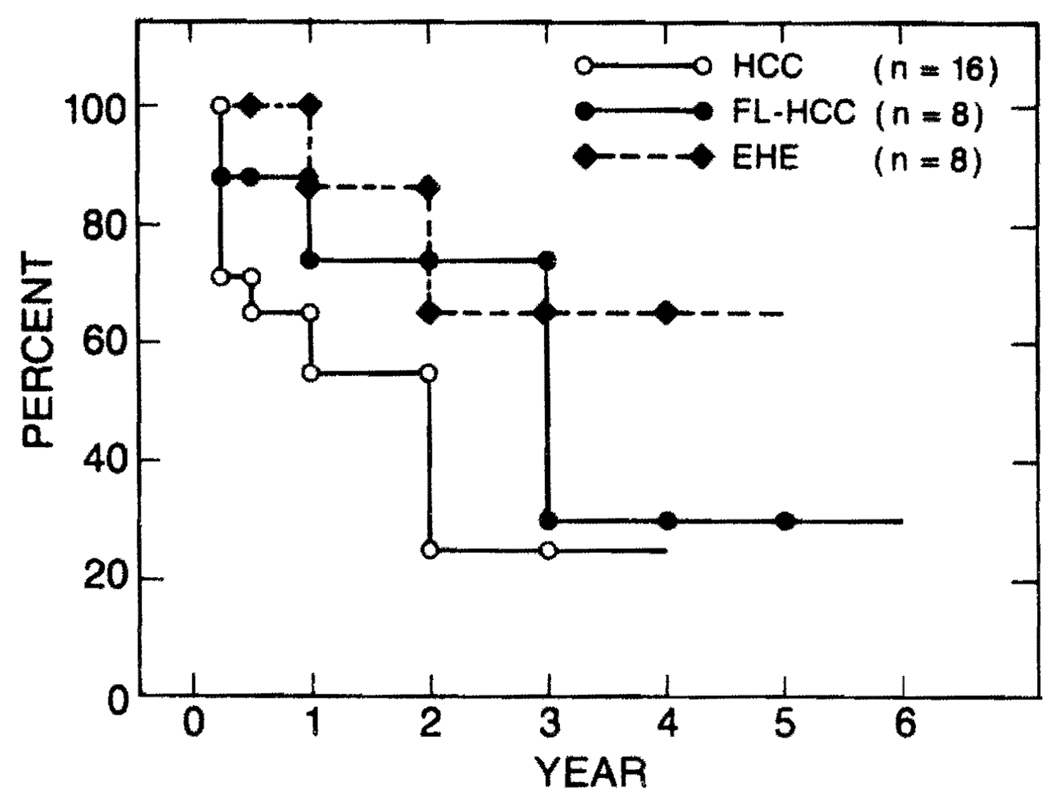
One- to 5-year survival rates of the 36 patients who received liver graft for the principal indication of malignancy were 65%, 50%, 29%, 29%, and 29%, respectively (Fig 6). The survival rates of 18 patients with hepatoma were lower than those of eight patients with fibrolamellar hepatoma and those of eight patients with epitheloid hemangioendothelioma (Fig 7).
Fig 6.
Survival rates of patients who received transplantation for primary liver malignancy were poor. However, survival rates of patients who had transplantation primarily for liver failure and whose advanced cirrhosis contained small malignancies were excellent.
Fig 7.
Survival rates of patients with hepatoma (HCC) were significantly lower than those with fibrolamellar hepatoma (FL-HCC) and those with epitheloid hemangioendothelioma (EHE).
Recurrence of primary hepatic malignancy after liver transplantation was examined among 27 of the 36 patients, who survived more than 6 months. Tumor recurrence was observed in 13 of the 27 6-month survivors. Seven of 11 patients with hepatoma had tumor recurrence, and three of which occurred within 1 year. Three of seven patients with fibromellar hepatoma had recurrence. All of the recurrences were diagnosed more than a year after transplantation. Similarly, the two (of eight) patients with epitheloid hemangioendothelioma had recurrences more than a year after transplantation. One patient with cholangiocarcinoma died from metastases 31 months after transplantation, 8 months after tumor recurrence.
Of the 17 patients who received liver grafts primarily for liver failure and whose livers harbored hepatic malignancy, only one died from recurrence of hepatoma. The remaining 16 patients are alive, free of tumor between 3 months to 6 years. The chronic survival of 17 of 17 patients, with only one late death, is noteworthy.
There were ten recipients who had carcinoma of the bile duct. In eight patients bile duct carcinoma was associated with primary sclerosing cholangitis, and in the remaining two patients the lesions were the so-called Klatskin tumors. One patient with a Klatskin tumor died within a month from transplant complications, and another died from recurrence 8 months after transplantation. Of the eight patients who had bile duct carcinoma associated with sclerosing cholangitis, one died from transplant complications within 1 month, four patients died from tumor recurrence in 4, 12, 14, and 16 months after transplantation, and three patients were alive free of tumor in 12, 13, and 14 months. No patient with bile duct carcinoma has lived 2 years after transplantation in this series.
There were seven patients who received liver transplantation for secondary hepatic malignancy. Three of the seven patients died. The first patient with carcinoid tumor of the small intestine died from transplant complications within three months, the second patient with carcinoid tumor of the small intestine and adenocarcinoma of the bile duct died in 6 months from recurrence of the bile duct cancer, and the third patient with adenocarcinoma of unknown primary site died from recurrence 21 months after transplantation. The remaining four of the seven patients are alive and free of tumor. One patient with glucagonoma, which was initially diagnosed as a hepatoma with lymphnode metastasis, is alive after 21 months, and another patient with glucagonoma is alive 10 months after transplantation. One patient with gastrinoma is alive free of tumor in 2 months. One patient with leiomyosarcoma of the small intestine is alive, but with recurrent tumor after 15 months.
DISCUSSION
Our first comprehensive report on liver transplantation using cyclosporine-steroid therapy in 1982 involved only 67 patients (41 adults and 26 children), but it had already predicted a vast improvement of survival after liver transplantation. The article had a strong influence upon the practice of hepatology.1 Five years later, this report, involving 1,000 patients, confirms the earlier assessment. The survival rates of 74% at 1 year and 64% at 5 years are convincing enough to consider liver transplantation as an ultimate therapy for various end-stage liver diseases. Unless agents that are more effective and safer than cyclosporine are used, further significant improvement of overall survival may not be expected, because liver transplantation will be applied for patients of even higher risk than now. However, substantial improvements can be achieved in some areas.
The survival rates after liver transplantation among children under 1 year of age are lower than those of older children. One of the main reasons for this is technical difficulty due to the small structures. The incidence of hepatic arterial thrombosis is higher in this age group than older age groups. Further technical refinements, intraoperative use of electromagnetic flow-meters, restricted use of perioperative coagulation factors and a proper anticoagulation therapy will reduce the incidence of technical failures. The lack of small sized pediatric organ donor is another reason of lower survival rates in this age group. Public education to raise awareness of urgent need of organ donation must be continued. Reduced size liver grafting, such as left lateral segment of a larger liver into a small pediatric recipient, can be carried out without significant additional risk as reported in this forum. This approach should decrease the waiting period for a proper donor organ, and thus the operation can be performed before an infant becomes too sick to have a successful transplantation.
The survival rates of patients older than 60 years old are also lower than those of younger adults. Further experience in selecting elderly candidates will establish more accurate criteria of adequate cardiovascular, pulmonary, and neurologic functions for liver transplantation.
There were no statistical differences in survival rates among the most common diseases in adult recipients (postnecrotic cirrhosis, primary biliary cirrhosis, and primary sclerosing cholangitis) and among those in pediatric recipients (biliary atresia, liver-based inborn metabolic errors, and postnecrotic cirrhosis). However, slightly lower survival rates among children with biliary atresia are directly or indirectly caused by an unsuccessful portoenterostomy and unwise attempts of its revision before transplantation. Although many children with extrahepatic biliary atresia have been saved by portoenterostomy when it was done by proper technique while the liver was still relatively normal, there are many other unfortunate children whose condition deteriorated rather rapidly because of unsuccessful attempts of the operation. It is not unusual that a child had had several abdominal operations, such as attempts of portoenterostomy, revisions of enterostomy, drainage of abdominal abscesses, and operations for bowel obstruction before transplantation. It is also not unusual that children with intrahepatic atresia or other nonextrahepatic type of biliary atresia, such as Alagille’s syndrome, had a portoenterostomy and that children with well established cirrhosis and portal hypertension have received the operation. The portoenterostomy should only be performed by experienced surgeons at the institutes where jaundice-free success rate has been more than 70%. As liver transplantation has become a practical option for children with biliary atresia, indications of portoenterostomy and its rare revision must be strictly followed.
The survival rates of patients with hepatitis B surface antigen positive cirrhosis were significantly lower than those of patients with HBsAg-negative postnecrotic cirrhosis. Recurrence of viral hepatitis B was a general rule despite our efforts at perioperative use of anti-hepatitis B immunoglobulin therapy and ongoing alpha interferon therapy. The recurrence of hepatitis B was the direct or indirect cause of death in four of five late deaths among the 36 patients. It is worthwhile to note that 12 of the 36 patients died within 3 months from various complications related to transplantation, but not from recurrence of hepatitis B. Actually, this high early mortality among chronic hepatitis B virus carriers influenced the survival rates more significantly than the mortality related to recurrent hepatitis B. Immunologic impairment of chronic HBsAg carriers could play a significant role in early mortality. Thus, further investigations are needed not only for antiviral therapy, but also for the means to decrease early mortality that was probably not directly related to hepatitis B virus.
Recurrence of hepatic malignancy after transplantation resulted in lower survival rates of patients who received liver grafts for cancer than those of patients without hepatic malignancy. However, the mere presence of a small, incidental hepatic malignancy in the advanced cirrhosis did not influence the survival rates. When liver transplantation was performed to treat a large hepatocellular carcinoma that could not be resected by a conventional technique of subtotal hepatectomy, the tumor all too frequently recurred within 1 year. For the last few years, adjuvant chemotherapy with adriamycin has been applied for these patients as soon as the condition of the patients and the graft became stable, usually 1 or 2 months after transplantation. During this small and short exercise, there has been at least no significant adverse effects of adjuvant chemotherapy. Safer and more effective adjuvant chemotherapy and/or immunotherapy are needed to prevent tumor recurrence. The prognosis of fibrolamellar hepatoma and epitheloid hemangioendothelioma are better than that of hepatoma, as indicated by better survival rates, and later and lower incidence of recurrence.
In this series of 1,000 patients, there has been no 2-year survivor who had bile duct cancer. The recurrence of the tumor within a year has been frequent. The facts that bile duct cancer was found in eight of 81 patients with primary sclerosing cholangitis (10% incidence) and that the survival of these eight patients was extremely poor strongly indicate the need of earlier transplantation for the patients with long standing sclerosing cholangitis.
In general, metastatic liver tumors constitute a poor indication for liver transplantation. However, over the years, seven such patients had liver replacement accidentally or knowingly because of an unusually indolent clinical course. The survival rates of these highly selected patients were better than generally expected, particularly if the metastases are from pancreatic islet tumors and from carcinoid tumors.
Acknowledgments
Supported by research grants from the Veterans Administration and Project Grant No. AM 29961 from the National Institutes of Health, Bethesda, MD.
REFERENCES
- 1.Starzl TE, Iwatsuki S, Van Thiel DH, et al. Hepatology. 1982;2:614. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffith BP, Shaw BW, Jr, Hardesty RL, et al. Surg Gynecol Obstet. 1985;160:66. [PMC free article] [PubMed] [Google Scholar]
- 3.Starzl TE, Iwatsuki S, Esquivel CO, et al. Semin Liver Dis. 1985;5:349. doi: 10.1055/s-2008-1040632. [DOI] [PMC free article] [PubMed] [Google Scholar]