Abstract
The fate of 185 cadaveric liver homografts preserved for four to 24 hours with University of Wisconsin (UW) solution was compared with that of 180 grafts preserved for three to 9½ hours with conventional Euro-Collins solution. Although the average preservation time of the UW-preserved livers was almost twice as long as that of the Euro-Collins-preserved livers, the UW-preserved grafts survived at a higher rate; permitted equal patient survival; and had a lower rate of primary nonfunction, a reduced need for retransplantation, and a lower rate of hepatic artery thrombosis. There was no correlation between the time of preservation of UW-preserved grafts up to 24 hours and liver function abnormalities in the first postoperative week. In contrast, livers preserved with Euro-Collins solution for more than five hours had significantly increased perturbations of hepatic function tests. The potential revolutionary effect of the UW solution on liver transplantation is described herein.
In September 1987, Jamieson and Kalayoglu and their associates1,2 at the University of Wisconsin (UW) reported that cold ischemia of canine and human liver homografts could be extended safely to one day with an infusate described by Wahlberg et al3 in experiments on pancreas preservation. The superior qualities of their UW solution were confirmed in our laboratories with liver replacement experiments in dogs (S. Todo, L. Podesta, Y. Ueda, et al, unpublished data, Pittsburgh, Dec 15, 1988) and rats and with an isolated perfusion model in rats.4
Herein, we report our experience with the first 185 human livers preserved with UW solution, with a minimum follow-up of three months after transplantation. The results were compared with those using 180 consecutive grafts that had been infused and preserved with Euro-Collins solution5 during the immediately preceding five-month period.
METHODS
Recipient Case Material
There were 164 patients who received 185 UW-preserved livers between Oct 22, 1987, and March 21, 1988 (Table 1), 21 (12.2%) requiring retransplantation during the observation period of three to eight months. Of the 164 patients, 151 were undergoing primary transplantation. The other 13 had replacement of a graft transplanted in the pre-UW era months to years earlier.
Table 1.
Comparison Between Recipients of UW vs Euro-Collins Preserved Grafts
| Recipient Data | UW Group | Euro-Collins Group |
|---|---|---|
| No. of grafts | 185 | 180 |
| 1st | 151 | 144 |
| 2nd | 27 | 31 |
| 3rd | 7 | 4 |
| 4th | … | 1 |
| No. of patients | 164 | 152 |
| Age, y | 36.5 ± 20.6 | 33.6 ± 20.9 |
| >18, % | 78.1 | 71.8 |
| <18, % | 21.9 | 28.2 |
| Sex, % | ||
| M | 58.5 | 43.5 |
| F | 41.5 | 56.5 |
The 152 retrospective control patients received 180 Euro-Collins-preserved livers between May 22, 1987, and Oct 21, 1987; of these, 28 (18%) required retransplantation. Of these recipients (Table 1), 144 were undergoing primary transplantation while eight had replacement of a liver that had been transplanted before the study period. The recipients in the Euro-Collins group had fewer males (Table 1) than the UW group.
Donor Case Material
The donor populations in the UW and Euro-Collins groups (Table 2) were not different in age, time of hospitalization, cause of death, liver function, cardiovascular and pulmonary status, or incidence of other organ removal.
Table 2.
Comparison of Donors of UW vs Euro-Collins Preserved Grafts
| Donor Data | UW Group | Euro-Collins Group | P* |
|---|---|---|---|
| No. of donors | 185 | 180 | … |
| Age, y | 19.8 ± 12.2 | 17.1 ± 10.5 | NS |
| >18, % | 78.1 | 71.8 | … |
| <18, % | 21.9 | 28.2 | … |
| Method of procurement, % | |||
| Rapid technique | 56.6 | 73.4 | <.05 |
| Regular technique | 38.9 | 25.5 | <.05 |
| Modified technique | 4.4 | 1.1 | NS |
NS indicates not significant.
Procurement Techniques
The techniques for multiple organ removal were those originally described6 or were modified with a rapid flush method for unstable donors.7 The rapid method was used more commonly (P<.05) in the Euro-Collins group (Table 2), but in previous studies. it had been shown that the choice of technique did not influence the outcome.8 The hepatic grafts were procured 95.3% of the time in collaboration with host renal teams and with heart teams from specialty centers. Some of these groups insisted on abdominal aortic infusion with lactated Ringer’s solution from the outset, others used different variations of Collins’ solution, and still others had their own mixtures. All of the livers preserved before UW solution became available had a final back table flush with Euro-Collins solution through a portal vein cannula.
For the UW-preserved livers, the procedure was the same except that on the back table, the portal vein was flushed with UW solution using 1.5 L if the donor weighed more than 60 kg, 1 L for livers from smaller donors, and 250 to 500 mL for pediatric cases. About one tenth of the volume of portal vein infusate was given into the hepatic artery.
Recipient Operations and Care
The recipient techniques9 were the same in the control and test cases. Just before revascularizing the new liver, the organ was reperfused with 300 to 500 mL of lactated Ringer’s solution in the Euro-Collins cases to remove air and excess potassium, and with plasmanate in the UW cases. Postoperative immunosuppression was with cyclosporine and low-dose steroids,10 with supplementary monoclonal antilymphocyte (OKT3)11 and/or azathioprine as indicated.
End Points Compared
Comparisons between the Euro-Collins and UW groups included the cold ischemia periods, liver function tests, recipient survival, major complications, incidence of primary nonfunction of the grafts, frequency of hepatic artery thrombosis, and need for retransplantation.
Statistical Analysis
Values were expressed as mean ± SD. Comparisons were with Student’s t test, χ2 test, and linear regression analysis. Actuarial patient survival was calculated by the method of Kaplan-Meier, and the statistical comparisons of patient and graft survival were made by the Mantel-Cox method.
RESULTS
Cold Ischemia Time
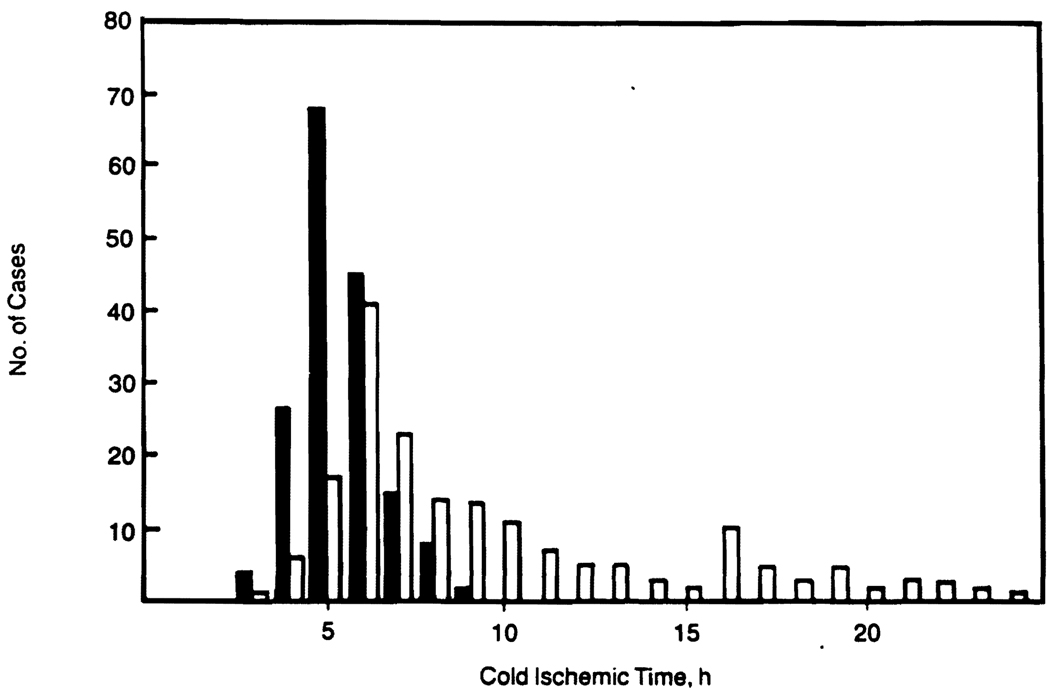
All of the Euro-Collins-preserved livers were revascularized after three to 9½ hours, whereas 81 (44%) of the UW-preserved livers were preserved for longer than 9½hours (Fig 1), with a maximum of 24 hours. The mean cold ischemia time was 5.9 ± 1.4 (SD) hours for the Euro-Collins-preserved livers and 10.1 ± 5.0 (SD) hours for the UW-preserved livers (P<.001).
Fig 1.
Duration of cold ischemia time and number of cases in UW (open bars) and Euro-Collins (solid bars) groups.
Graft Function
On the basis of previously published gross anatomic criteria and color,8,12 the UW-preserved livers were grossly superior. They reperfused immediately with institution of portal inflow and almost always made bile. The clinical impression was that cardiovascular instability and coagulopathies were uncommon compared with the retrospective experience with Euro-Collins-preserved livers.
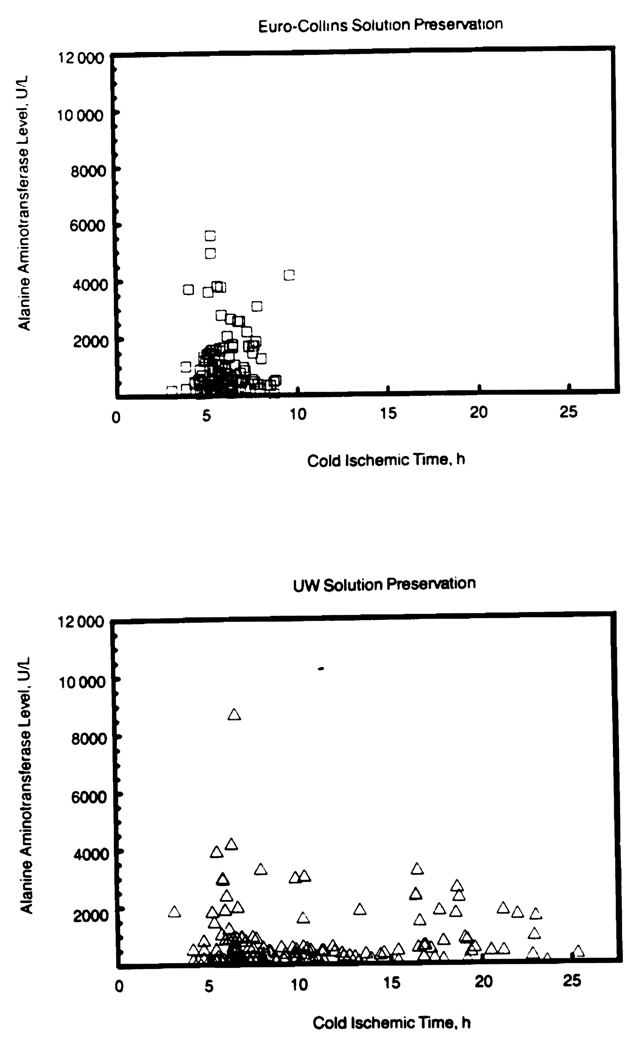
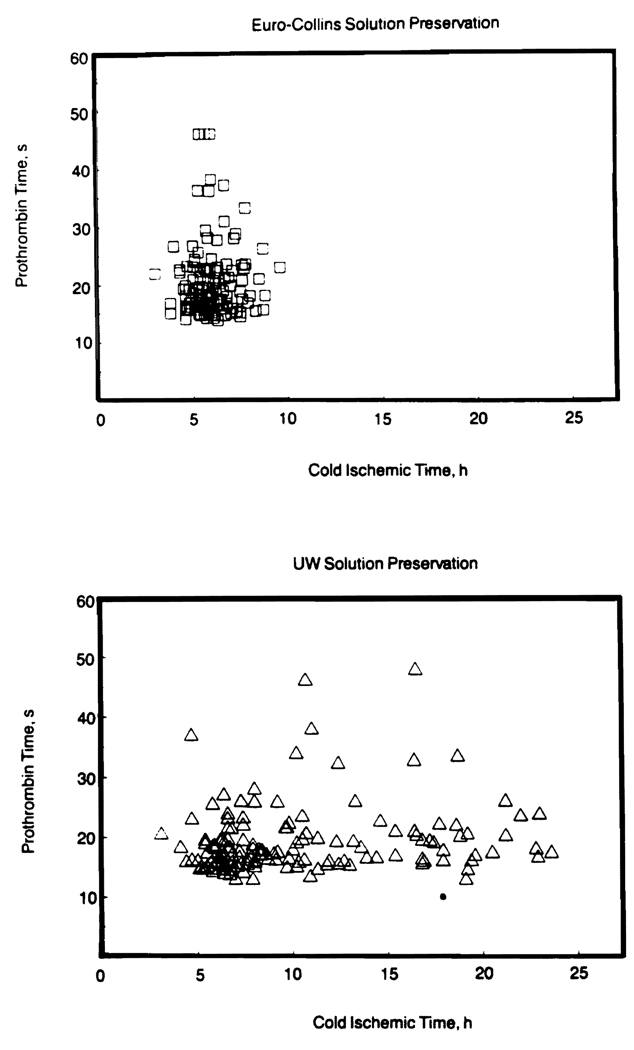
Although the UW livers were preserved longer, the maximum increases in serum aspartate aminotransferase and serum alanine aminotransferase in the first week were no greater than with the Euro-Collins-preserved livers (Fig 2). The same was true for maximum prothrombin time in the first week (Fig 3). Serum bilirubin values during the first four hours were almost identical with values of UW-preserved and Euro-Collins-preserved livers.
Fig 2.
Highest serum alanine aminotransferase values in first postoperative week after transplantation of livers preserved with UW (bottom) and Euro-Collins (top) solutions for variable periods of time.
Fig 3.
Highest prothrombin time values in first postoperative week alter transplantation of livers preserved with UW (bottom) and Euro-Collins (top) solutions for variable periods of time.
In the UW group, the time of preservation had no demonstrable adverse effects up to 24 hours (Figs 2 and 3). In contrast, grafts preserved for more than five hours with Euro-Collins solution had significant increases in serum aspartate aminotransferase and serum alanine aminotransferase levels (P<.05), as well as greater prolongation of prothrombin time.
Patient Survival
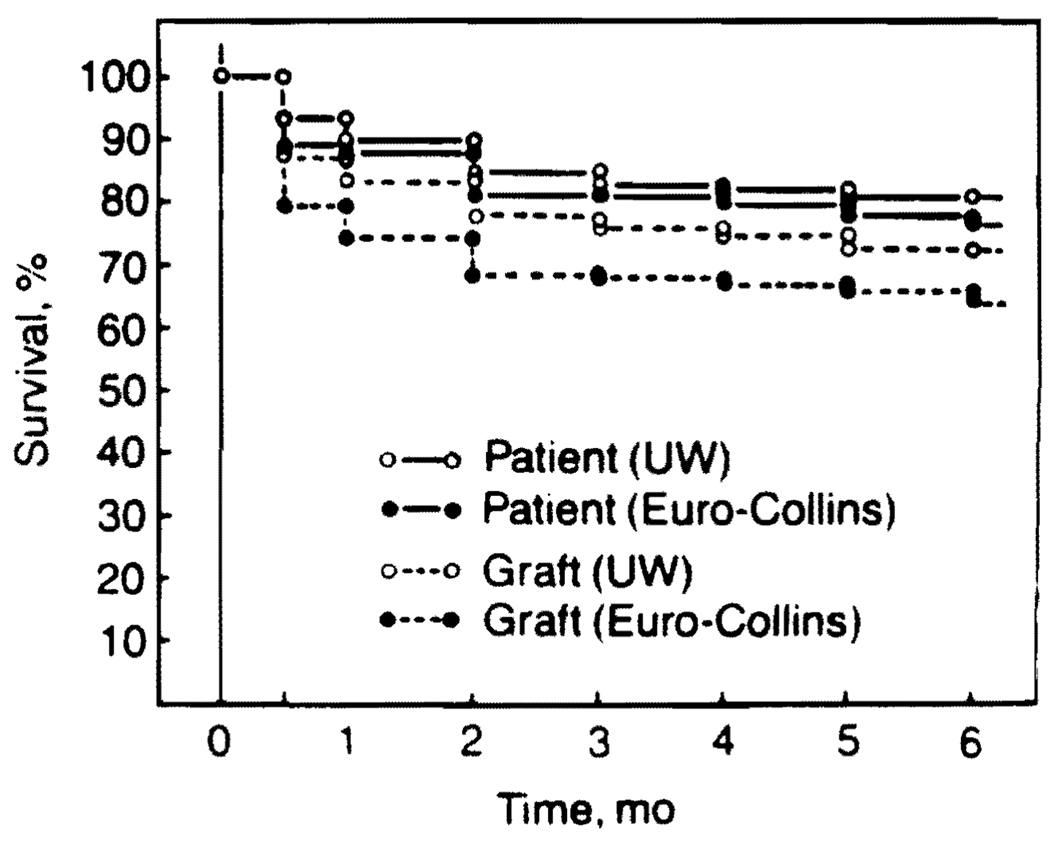
After primary transplantation, the patient survival curves were nearly identical with the UW vs Euro-Collins groups, with actual survival at three months of 83% and 81%, respectively, and an actuarial six-month survival of 81% and 77%. respectively (Fig 4).
Fig 4.
Patient and graft survival in UW and Euro-Collins groups.
The patients who had retransplantations with UW-preserved livers had a slightly better survival for three months than the recipients whose retransplant grafts were preserved with Euro-Collins solution.
Causes of Patient Death
Sepsis from viral, bacterial, and fungal infection was the leading cause of death in both study groups. Primary graft nonfunction was responsible for six patient deaths in the Euro-Collins group compared with one in the UW group.
Graft Survival
Graft survival in 151 primary transplant recipients in the UW group and 144 primary recipients in the Euro-Collins group are shown in Fig 4. The actual graft survival at three months was 76% using UW-preserved livers vs 68% using Euro-Collins-preserved livers and actuarial six-month survival was 73% vs 65%, respectively (P<.09).
Causes of Retransplantation
There were 17 retransplantations (11.3%) among the 151 patients who received primary liver transplantation in the UW group, while in the Euro-Collins group there were 29 retransplantations (20%) (Table 3). The number of hepatic artery thromboses was reduced significantly in the UW group (P<.05), as well as the incidence of primary graft nonfunction and rejection. The three primarily nonfunctioning grafts in the UW group (Table 3) had cold ischemia times of four hours and 41 minutes, five hours and 30 minutes, and 22 hours and 58 minutes. Thus, there was no relationship in the UW cases that required retransplantation between the length of cold ischemia times and the occurrence of primary graft nonfunction.
Table 3.
Causes of Retransplantation After Primary Grafting
| Patient Information | UW Group | Euro-Collins Group | P* |
|---|---|---|---|
| No. of patients | 151 | 144 | … |
| No. of retransplants | 17 (11.3%) | 29 (20%) | <.1 |
| Hepatic artery thrombosis | 7 | 18 | <.05 |
| Primary nonfunction | 3 | 5 | NS |
| Rejection | 1 | 4 | NS |
| Other causes of retransplantation | 6 | 2 | NS |
NS indicates not significant.
Duration of Hospital Stay
The mean duration of hospital stay of patients in the UW group was 37.7 ± 20.8 (SD) days, and that of all patients in the Euro-Collins group was 40.9 ± 23.9 (SD) days. The mean length of stay in the intensive care unit was 8.7 ± 10.6 days in the UW group and 8.8 ± 14.5 (SD) days in the Euro-Collins group (P value, not significant).
COMMENT
The first step in the development of liver graft preservation was core cooling by infusion of chilled lactated Ringer’s solution into the portal vein.13 Today, core cooling is the first step in the preservation of all whole-organ grafts, and this is most often done in situ by some variant of the technique described by Marchioro et al14 for the continuous hypothermic perfusion of cadaveric livers and kidneys long before the acceptance of brain death conditions. Ackerman and Snell15 and Merkel et al16 popularized in situ cooling of cadaveric kidneys with cold electrolyte solutions infused into the distal aorta. An extension of this technique has allowed removal of all thoracic and abdominal organs, including the liver, without jeopardizing any of the individual organs.6
Extension of the safe period of the liver beyond that provided by initial cooling has followed one of two prototype strategies. One approach was to provide a limited and continuous circulation ex vivo. This was first done successfully with a perfusate that was primed with blood and oxygenated within a hyperbaric oxygen chamber.17 The alternative strategy for the preservation of kidneys, livers, and other organs has been called the slush techniquc, with the instillation of special solutions5,18 and subsequent refrigeration. The introduction of the UW solution1,2 has been the first major development in liver preservation since the description of the slush techniques by Benichou et al5 and Wall et al.18
The remarkable effectiveness of the UW solution has revolutionized liver transplantation at almost every level. The enhanced margin of safety has permitted more effective use of organs that can be stored safely while waiting for operating room facilities or personnel to become available. It has allowed procurement of grafts from cities once considered too distant, from as far as across the Atlantic Ocean. It has changed the way in which the recipient operation is approached. In the past, the donor and the recipient operations were closely coordinated to shorten the ischemic interval to a minimum. Now, the graft usually is brought back to Pittsburgh and submitted to close scrutiny before the recipient is taken to the operating room. If desirable, there is ample time for detailed histopathologic studies of graft biopsy specimens. Finally, the greatly increased margin of safe time can be invested in the performance of a more perfect recipient hepatectomy, better hemostasis before the graft is sewn in, and even leisurely removal of a part of the homograft if a size discrepancy exists between the graft and the hepatic fossa in which it is to be placed.
It is ironic that the advantages of the UW solution are so obvious while the explanations for its efficacy are so obscure. In experiments on pancreas transplantation, Wahlberg et al3 noted that the weight gain commonly seen in organs preserved by past slush techniques was avoided with their solution. The same observations have been made with livers (S. Todo, L. Podesta, Y. Ueda, et al, unpublished data, Pittsburgh, Dec 15, 1988). Minimizing “water logging” of the endothelium of the microvasculature could explain the significant reduction of hepatic artery thrombosis with the use of the UW fluid. Whatever the rationale may be for the effectiveness of the UW solution.19 inhibition of cell swelling during cold storage would appear to be particularly important.
Acknowledgments
This study was supported by research grants from the Veterans Administration and project grant AM 29961 from the National Institutes of Health, Bethesda, Md.
Many members of the surgical faculty and the faculty of the School of Pharmacy contributed to this study. Particularly noteworthy were Andreas Tzakis, MD; Raman Venkataramanan, MD; Luis Mieles, MD; Velma Scantlebury, MD; Leonard Makowka, MD, PhD; Andrei Stieber, MD; Babu Koneru, MD; Wallis Marsh, MD; and Shunzaburo Iwatsuki, MD.
Reterences
- 1.Jamieson NV, Sundberg R, Lindell S, et al. Successful 24- to 30-hour preservation of the canine liver: A preliminary report. Transplant proc. 1988;20:945–947. [Google Scholar]
- 2.Kalayoglu M, Sollinger WH, Stratta RJ, et al. Extended preservation of the liver for clinical transplantation. Lancet. 1988;1:617–619. doi: 10.1016/s0140-6736(88)91416-x. [DOI] [PubMed] [Google Scholar]
- 3.Wahlberg JA, Love R, Landegaard L, et al. Seventy-two-hour preservation of the canine pancreas. Transplantation. 1987;43:5–8. doi: 10.1097/00007890-198701000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Ontell SJ, Makowka L, Ove P, et al. Improved hepatic function in the 24 hour preserved rat liver with UW-lactobionate solution and SRI 63–441. Gastroenterology. 1988;5:1617–1624. doi: 10.1016/s0016-5085(88)80086-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benichou J, Halgrimson CG, Weil R, III, et al. Canine and human liver preservation for six to 18 hours by cold infusion. Transplantation. 1977;24:407–411. doi: 10.1097/00007890-197712000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starzl TE, Hakala TR, Shaw BW, Jr, et al. A flexible procedure for multiple cadaveric organ procurement. Surg Gynecol Obstet. 1984;158:223–230. [PMC free article] [PubMed] [Google Scholar]
- 7.Starzl TE, Miller C, Broznick B, et al. An improved technique for multiple organ harvesting. Surg Gynecol Obatet. 1987;165:343–348. [PMC free article] [PubMed] [Google Scholar]
- 8.Miller C, Mazzaferro V, Makowka L, et al. Rapid flush technique for donor hepatectomy: Safety and efficacy of an improved method of liver recovery for transplantation. Transplant proc. 1988;20:948–950. [PMC free article] [PubMed] [Google Scholar]
- 9.Starzl TE, Iwatsuki S, Esquivel CO, et al. Refinements in the surgical technique of liver transplantation. Semin Liv Dis. 1985;6:349–356. doi: 10.1055/s-2008-1040632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Starzl TE, Klintmalm GBG, Porter KA, et al. Liver transplantation with use of cyclosporin A and prednisone. N Engl J Med. 1981;305:266–269. doi: 10.1056/NEJM198107303050507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fung JJ, Demetris AJ, Porter KA, et al. Use of OKT3 with cyclosporine and steroids for reversal of acute kidney and liver allograft rejection. Nephron. 1987;96:19–33. doi: 10.1159/000184431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Makowka L, Gordon RD, Thdo S, et al. Analysis of donor criteria for the prediction of outcome in clinical liver transplantation. Transplant Proc. 1987;19:2378–2382. [PMC free article] [PubMed] [Google Scholar]
- 13.Starzl TE, Kaupp HA, Jr, Brock DR, et al. Reconstructive problems in canine liver homotransplantation with special reference to the postoperative role of hepatic venous flow. Surg Gynecol Obstet. 1960;111:733–743. [PMC free article] [PubMed] [Google Scholar]
- 14.Marchioro TL, Huntley RT, Waddell WR, et al. Extracorporeal perfusion for obtaining postmortem homografts. Surgery. 1963;54:900–911. [PMC free article] [PubMed] [Google Scholar]
- 15.Ackerman JR, Snell ME. Cadaveric renal transplantation. Br J Urol. 1968;40:515–621. doi: 10.1111/j.1464-410x.1968.tb11842.x. [DOI] [PubMed] [Google Scholar]
- 16.Merkel FK, Jonasson O, Bergan JJ. Procurement of cadaver donor organs: Evisceration technique. Transplant Proc. 1972;4:585–589. [PubMed] [Google Scholar]
- 17.Brettschneider L, Daloze PM, Huguet C, et al. The use of combined preservation techniques for extended storage of orthotopic liver homografts. Surg GYnecol Obstet. 1968;126:263–274. [PMC free article] [PubMed] [Google Scholar]
- 18.Wall WJ, Calne RY, Herbertson BM, et al. Simple hypothermic preservation for transporting human livers long distances for transplantation. Transplantation. 1977;23:210–216. doi: 10.1097/00007890-197703000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Belzer FO, Southard JG. Principles of solid-organ preservation by cold storage. Transplantation. 1988;45:673–676. doi: 10.1097/00007890-198804000-00001. [DOI] [PubMed] [Google Scholar]