Abstract
Background
Concomitant with the rise in childhood obesity there has been a significant increase in the number of adolescents with clinical features of insulin resistance and prediabetes. Clinical insulin resistance and prediabetes are likely to progress to type 2 diabetes and early atherosclerosis if not targeted for early intervention. There are no efficacy trials of lifestyle intervention in this group to inform clinical practice. The primary aim of this randomised control trial (RCT) is to determine the efficacy and effectiveness of two different structured lifestyle interventions differing in diet composition on insulin sensitivity, in adolescents with clinical insulin resistance and/or prediabetes treated with metformin.
Methods/design
This study protocol describes the design of an ongoing RCT. We are recruiting 108 (54 each treatment arm) 10 to 17 year olds with clinical features of insulin resistance and/or prediabetes, through physician referral, into a multi-centred RCT. All participants are prescribed metformin and participate in a diet and exercise program. The lifestyle program is the same for all participants except for diet composition. The diets are a high carbohydrate, low fat diet and a moderate carbohydrate, increased protein diet.
The program commences with an intensive 3 month dietary intervention, implemented by trained dietitians, followed by a 3 month intensive gym and home based exercise program, supervised by certified physical trainers. To measure the longer term effectiveness, after the intensive intervention trial participants are managed by either their usual physician or study physician and followed up by the study dietitians for an additional 6 months. The primary outcome measure, change in insulin sensitivity, is measured at 3, 6 and 12 months.
Discussion
Clinical insulin resistance and prediabetes in the paediatric population are rapidly emerging clinical problems with serious health outcomes. With appropriate management these conditions are potentially reversible or at least their progression can be delayed. This research study is the first trial designed to provide much needed data on the effective dietary management for this cohort. This study will inform clinical practice guidelines for adolescents with clinical insulin resistance and may assist in preventing metabolic complications, type 2 diabetes and early cardiovascular disease.
Trial registration
Australian and New Zealand Clinical Trials Registration Number ACTRN12608000416392
Background
Concomitant with the rise in childhood obesity there has been a significant increase in the number of adolescents with clinical signs of insulin resistance and prediabetes [1]. It is essential that adolescents with clinical insulin resistance and prediabetes are targeted for early intervention. Unmanaged, they are likely to progress to type 2 diabetes and early atherosclerosis [2]. Development of type 2 diabetes in young people is of particular concern because complications are common and appear early in the disease [3,4].
Avoidance of progression to type 2 diabetes is of enormous benefit, not only to the individual in terms of increasing life expectancy and quality of life, but also in economic terms to society and health care payers [5]. Evidence, primarily from adult studies, indicates that progression can be reduced by diet, exercise and metformin [5].
Diet
The role of the specific macronutrient content of the diet in the management of insulin resistance in adolescents has not been previously investigated. Most current methods of dietary management focus on weight management and recommend a high carbohydrate, low fat approach [6]. However, a recent systematic review of the dietary management of obesity in children and adolescents concluded: "There is a marked mismatch between the public health importance of childhood obesity and the number and quality of the studies conducted so far to assess dietary interventions for weight reduction in childhood and adolescence, and little evidence to support the current recommendation of a low-fat energy-restricted diet."[7]. The effectiveness of a low fat high carbohydrate dietary pattern over the long term remains uncertain, and despite widespread dissemination of the public health message to adopt a low fat high carbohydrate diet, rates of obesity, insulin resistance, prediabetes and type 2 diabetes continue to climb.
One alternative is a moderate carbohydrate, increased protein diet. In adults, several studies indicate that this diet may enhance weight loss and improve metabolic markers including post prandial glucose levels [8-10]. Not all studies support these findings [11], although, there are several supportive mechanisms proposed. The relative success of lower carbohydrate, higher protein diets has been related to i) an increase in satiety [12,13] ii) effects on thermogenesis, iii) favourable changes in body composition (preserves fat free mass and reduces fat mass)[14]; and iv) decreased energy-efficiency, all of which are related to protein metabolism [15-17]. However, no clinical trial data are available in children and adolescents.
Little is known about the optimal dietary intervention strategy for overweight and obese children and adolescents. Intervention studies have used hypo-caloric diets, with and without energy based food exchange system (for example Traffic Light guides), national dietary guidelines and protein sparing modified fasts, with varying results [18]. However, many inadequately described the details of the prescribed dietary intervention, making replication of the interventions difficult [18]. Structured, restrictive weight management diets have been also been described [19]. While there is general concern that this may be counter productive to the development of healthy eating habits, anecdotally, many young people who have successfully lost weight in our Weight Management Services frequently request dietary prescription. This observation supports the need for high quality studies which includes detailed dietary interventions to inform best practice.
Exercise
Including a physical activity intervention in the management of overweight and obese adolescents is considered to be part of best practice [20]. Physical activity, with or without dietary intervention, is effective in improving body composition and may improve insulin sensitivity and other metabolic markers [21,22]. Most paediatric studies have used aerobic training; however, evidence from two small paediatric studies suggests that resistance training may also be important for improving insulin sensitivity, body composition and fat distribution [23,24].
Metformin therapy
There are now five randomised control trials (RCTs) [25] that have demonstrated the beneficial effects of metformin in adolescents with insulin resistance and/or prediabetes. These results support previous studies assessing the role of metformin in adolescents with type 2 diabetes, polycystic ovary syndrome and non-alcoholic fatty liver disease [26-28]. The effect of metformin therapy tends to be small. Results from our systematic review and meta-analysis indicate that after 6 months of metformin therapy in children and adolescents with insulin resistance there was a statistically significant mean decrease in fasting insulin, homeostasis model assessment of insulin resistance (HOMA) and body mass index (BMI) of 9.6 microU/ml (95% CI: 6.3 to 13.0) and 2.7 kg/m2 (95% CI: 1.7 to 3.6), respectively, compared to the placebo control group [25]. Results from studies in adults suggest that a lifestyle change with pharmacotherapy exceeds the benefit of either intervention alone [29]. However, no study has evaluated more intensive lifestyle interventions in conjunction with metformin in this target group.
Study Aims
The primary aim of this study is to determine the efficacy of two different structured dietary interventions on insulin sensitivity, in adolescents with clinical evidence of insulin resistance and/or prediabetes treated with metformin. The isocaloric diets are 1) a high carbohydrate, low fat diet and 2) a moderate carbohydrate, increased protein diet.
We hypothesise that the moderate carbohydrate, increased protein diet will be more effective than the high carbohydrate diet in improving insulin sensitivity and metabolic profile in adolescents with clinical features of insulin resistance and/or prediabetes.
Design and Methods
Ethics approval
The study has been reviewed and approved by The Children's Hospital at Westmead (CHW) Human Research Ethics Committee (07/CHW/12), Sydney South West Area Health, Western Zone (08/LPOOL/195) and Sydney South West Area Health Service, Royal Prince Alfred Hospital (08/RPAH/455). Written informed consent from parents and assent from the young people is sought prior to their enrolment in the study.
Design
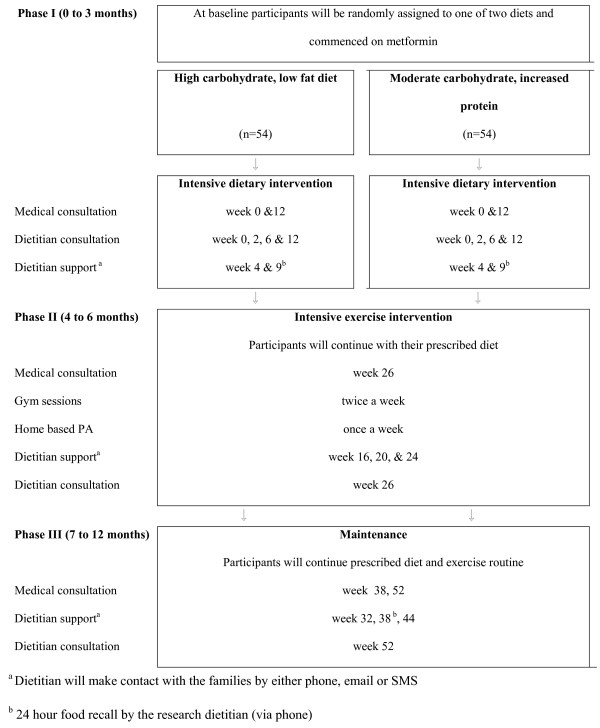
The study is a 12 month RCT, taking place at three tertiary hospitals in Sydney, Australia: CHW (the main study centre), Royal Prince Alfred Hospital and Campbelltown Hospital. The project consists of three phases:
Phase I (0 to 3 months): Intensive structured dietary intervention
Phase II (4 to 6 months): Intensive exercise program
Phase III (7 to 12 months): Maintenance
The overall schedule for the intervention is shown in Figure 1.
Figure 1.
At the commencement of the study the children and adolescents are randomised to one of two diets. All participants are treated with metformin and receive the same overall lifestyle intervention. The only difference between the two treatment arms is the composition of the diet.
Outcome measures
The primary outcome measure is insulin sensitivity. Insulin sensitivity is measured at baseline and after 3 and 12 months at CHW by the whole body insulin sensitivity index derived from an oral glucose tolerance test (OGTT) using the following formula: 10 000/√ ((Fasting insulin × fasting glucose) × (mean 2 hr glucose × mean 2 hr insulin))[30]. The potential confounding variables include adiposity and change in adiposity, pubertal stage, fitness and physical activity and dietary adherence. The secondary outcome measures are metabolic profile indicators including: acanthosis nigricans score, amenorrhoea/oligomenorrhoea, blood pressure, total cholesterol, HDL-cholesterol, triglycerides, waist to height ratio, hs-CRP, adipokines. Changes in outcome measures will be examined over time, as will differences between trial arms.
Participants and recruitment
Approximately 108 (54 in each treatment arm) 10 to 17 year olds with clinical insulin resistance and/or prediabetes are being recruited through doctor referral from the three tertiary hospitals trial sites in Sydney as well as local general practitioner (primary care physician) and paediatrician referral. After a patient has been assessed and identified as meeting the trial criteria the patient and parent or carer is informed about the study by the referring doctor or study physician. If interested in participating, the patient and parent or carer makes phone contact with the research dietitian who explains the study design and sends a parent/carer information sheet and an information sheet for the adolescent detailing the study researchers, intervention, the potential benefits and required commitment and consent form. Once written consent is obtained by the study team the participant is randomised to one of two diets.
Selection criteria
Inclusion criteria
Ten to 17 year olds who are overweight or obese, as defined by the International Obesity TaskForce criteria [31] with either pre type 2 diabetes as defined by the American Diabetes Association [32] and/or clinical insulin resistance are eligble for recruitment. Clinical insulin resistance is defined as overweight or obese and fasting insulin (pmol/L)/glucose (mmol/L) ratio >20 with one or more of the following acanthosis nigricans, polycystic ovarian syndrome (National Institute of Health criteria [33]), hypertension [34], fasting HDL cholesterol < 1.03 mmol/L [35] or fasting triglycerides ≥ 1.7 mmol/L [35].
Exclusion criteria
Type 1 or type 2 diabetes, contraindications to metformin therapy, secondary causes of obesity, psychiatric disturbance, significant mental illness, inability to take part in physical activity, weight loss medications or medications known to cause weight gain, and weight >120 kg, due to technical difficulties with dual energy x-ray absorptiometry machine (DXA). Children and adolescents taking metformin prior to commencement of the study are required to have a three month wash-out period.
Randomisation
Treatment allocation occurs centrally by minimisation [36] with the aid of computer software [37] at CHW. To adjust for potential confounding influences participants are randomised into dietary groups stratified by sex, pubertal stage, categorised by the study physician as either prepubertal or early puberty (Tanner stage 1 and 2) or pubertal (Tanner stage 3, 4 and 5), and BMI status (overweight or obese as defined by the International Obesity TaskForce [31]).
Sample size
The sample size is based on the primary outcome, change in whole body insulin sensitivity index (ISI) between baseline and one year, using means and standard deviations (SD) from our clinical data [38] and are consistent with published data [30]. To have an 80% chance of detecting a significant increase in whole body ISI over a one year period at the two sided 5% level, 43 young people are required in each intervention arm, assuming a clinically significant increase in whole body ISI of 0.8 and an SD of 1.3. The high SD allows for the variation of insulin sensitivity during puberty. To accommodate a 20% dropout rate we will need to recruit 54 in each intervention arm (108 in total). A 20% drop out rate is based on two Australian paediatric weight reduction trials, PEACH and HELPP, which reported a 12% and 18% [39] dropout rate at 12 months. In addition, based on our clinical experience, we anticipate a maximum of 2 or 3 participants may progress to type 2 diabetes. However, treatment for these participants is likely to be consistent with the study intervention.
Interventions
At the commencement of the study all participants are commenced on metformin and randomised to one of two diets. The participants are encouraged to follow their prescribed diet for the duration of the trial.
Metformin
Metformin (Diabex) is dispensed through the pharmacy at CHW and is provided at no cost to all participants. The initial dose is 250 mg twice a day. After the first two weeks this is increased to a final dose of 500 mg twice daily.
Diets
Diet 1 is a high carbohydrate, low fat diet, that is 55-60% carbohydrate (moderate glycaemic load), 30% fat (≤ 10% saturated fat) and 15% protein. Diet 2 is a moderate carbohydrate, increased protein diet, that is 40-45% total energy (moderate glycaemic load), 30% fat (≤ 10% saturated fat), 25-30% protein. Both diets are prescriptive and two different energy levels are prescribed depending upon age: 6,000 to 7,000 kJ (10 to 14 year old) or 7,000 to 8,000 kJ (15 to 17 year old). Representative menus for the two diets are shown in Table 1.
Table 1.
Representative menu for the two diets
| Diet 1 High carbohydrate, low fat | Diet 2 Moderate carbohydrate, increased protein | |
|---|---|---|
| Breakfast | 2 breakfast (Weet-Bix) biscuits | 1 slice of wholemeal toast |
| 200 mL low-fat milk | 1 tsp margarine | |
| 1 tsp honey | 1 egg | |
| 1 piece fruit | 1 piece fruit | |
| Morning Tea | 200 mL low-fat flavoured milk | 200 g low-fat yoghurt |
| 30 g muesli bar | 1 piece fruit | |
| Lunch | 2 slices wholemeal bread | 2 slices wholemeal bread |
| 1 tsp margarine | 1 tsp margarine | |
| Unlimited salad vegetables | 50 g lean meat | |
| 1 piece of fruit | Unlimited salad vegetables | |
| Afternoon tea | 2 slices wholemeal bread toasted | 4 wholegrain cracker biscuits |
| 4 tsp peanut butter | 1 slice reduced fat cheese | |
| Dinner | 1 cup cooked pasta | 150 g beef steak |
| 100 g meat & tomato based sauce | 1 potato mashed | |
| 1 cup (or more) mixed vegetables/salad | 1 cup (or more) mixed vegetables/salad | |
| Supper | 2 scoops low-fat ice cream | 200 mL reduced-fat milk |
| 1 cup strawberries | 1 tbs Milo |
Medical care
Clinical progress is reviewed by the participant's primary referring physician or study physician at 3, 6, 9 and 12 months, unless otherwise indicated. The physician assesses pubertal staging, blood pressure, grading of acanthosis nigricans, menstrual history and metformin dosage/adherence. The physician is blinded to the trial arm of the individual and participants are requested to not inform their physician.
Phase 1: Intensive structured dietary intervention (0 to 3 months)
Phase I assesses the impact of the macronutrient content of the diet on insulin sensitivity. The trial dietitian (lifestyle coach) delivers a standardised intervention to both trial arms, which utilises a prescribed meal plan and coaching model. Participants are not given the macronutrient content of the diets; they have been simply told that they will be randomised to one of two diets and they are given a meal plan, titled 'My Meal Plan'. The meal plans take into consideration adolescent food preferences, with the aim of weight loss. The coaching framework provides a theoretical basis for a number of key psychological variables which are important in achieving dietary compliance, lifestyle change and sustainable weight loss, such as self efficacy, stage of change intervention, autonomy, assuming responsibility, self monitoring, goal setting, accountability and self directed behaviour change[21,40].
During Phase I, food consistent with the prescribed diet plans and equating to approximately 25% of the participants energy requirements is given to the families. During this phase physical activity advice is standardised and delivered by the trial dietitian. The advice is consistent with Australian recommendations for children and adolescents including promoting an increase in incidental activity, a decrease in sedentary behaviour and an increase in active transport [41].
During this phase the participants and at least one parent/carer are expected to attend four face to face meetings with the dietitian as outlined in Figure 1. In addition to the face to face contact the dietitian also makes contact with the participant using either phone, email or text message, depending on the preference of the participant. This contact is aimed at the participant to assist with motivation and answer questions. It may or may not involve the parent/carer.
Phase II: Intensive exercise program (4 to 6 months)
Phase II assesses the impact of a supervised, general exercise program on the treatment effect of diet and metformin. All participants receive an exercise program as well as nutrition coaching, as outlined in Figure 1. The exercise program is conducted in small groups for 1 hour, twice a week for 12 weeks in a commercial gym, Fitness First. Participants are given free access to Fitness First gyms in the geographic area in which they live. The gym program consists of a circuit training program with an age-appropriate mix of resistance exercises and aerobic stations conducted by a qualified physical trainer. In addition to the gym program participants are encouraged to exercise once a week at home. During this phase the trial dietitian offers support to the participants every 4 weeks, Figure 1.
Phase III: Maintenance (7 to 12 months)
During Phase III participants are managed by their usual physician or study physician and followed up by the trial dietitian as indicated in Figure 1. They are encouraged to continue with their diet and exercise regimens and metformin (if required).
Training the dietitians (lifestyle coaches)
Two dietitians are employed to specifically to work on this trial. Training of these dietitians to deliver the interventions is provided by two other experienced dietitians (SB/KC) with expertise in lifestyle counselling in children and adolescents with insulin resistance and prediabetes. Training includes shadowing in the hospital setting in order to gain experience and supervision is received on a regular basis, approximately 6 weekly intervals, as per department guidelines for training of dietitians.
Blinding
Assessors of the main outcome measures are blinded to treatment allocation. These include the two trial clinical nurse consultants responsible for undertaking the OGTTs and anthropometric measures, the technician who takes the dual energy x-ray absorptiometry (DXA) measurements and the primary and study physicians.
Measurements
Details of measurements are outlined below and the measurement schedule is shown in Table 2.
Table 2.
RESIST Measurement Schedule
| Measurement | Baseline | 3 months | 6 months | 9 months | 12 months |
|---|---|---|---|---|---|
| Clinical Assessment | |||||
| Anthropometry | ✓ | ✓ | ✓ | ✓ | |
| Blood pressure | ✓ | ✓ | ✓ | ✓ | |
| Pubertal staging | ✓ | ✓ | ✓ | ✓ | |
| Acanthosis nigricans grading | ✓ | ✓ | ✓ | ✓ | |
| Body composition | |||||
| Dual energy x-ray absorptiometry | ✓ | ✓ | ✓ | ||
| Metabolic Measures | |||||
| Oral glucose tolerance test | ✓ | ✓ | ✓ | ||
| Fasting blood sample | ✓ | ✓ | ✓ | ✓ | |
| Urine sample (spot) | ✓ | ✓ | ✓ | ✓ | |
| Diet: Self monitoring, intake and questionnaires | |||||
| Dietary checklist and questionnaires | ✓ | ✓ | ✓ | ||
| 24 hour recall | ✓ | ✓ | ✓ | ✓ | |
| Physical activity, sedentary behaviour and fitness | |||||
| CLASS questionnaire | ✓ | ✓ | ✓ | ✓ | |
| Fitness testing | ✓ | ✓ | ✓ | ||
| Metformin adherence | |||||
| Pill count | ✓ | ✓ | ✓ | ✓ |
Clinical Assessment
Family background and family medical history
Demographic and family medical history information is collected at baseline by the study physician.
Anthropometry
Weight and height are measured using standard procedures [42]. For weight a single measurement, measured to the nearest 0.1 kg, is recorded and used for data analysis. Height is measured twice, to the nearest 0.1 cm, and the average value is used for data analysis. Waist circumference is measured to the nearest 0.1 cm using a flexible steel tape. The waist is defined as the horizontal distance around the umbilicus using the left hand under technique. The average of three measurements will be used for data analysis. Waist to height ratio will be used as a measure of central adiposity [43].
Pubertal status
Pubertal status is categorised according to the Tanner Scale after assessment by the study physician [44].
Blood Pressure
Blood pressure is measured using an automated blood pressure monitor (Dinamap 1846 SX) according to standard procedures [45].
Acanthosis nigricans
Acanthosis nigricans in the axilla and neck is graded by the study physicians using the Burke scale [46].
Body composition
Dual energy x-ray absorptiometry (DXA)
DXA (Prodigy, Lunar-GE, Madison, WI USA) equipped with propriety software version 8.6 is used to measure body composition. The manufacturer recommended scan mode (as determined by height and weight) is used for total body mass measurements. When possible, standard positioning techniques is used. Where the participant width exceeds maximum scan width, subjects are "mummy wrapped", with arms placed in a lateral position to reduce subject width. Scans are analysed using manufacturer recommended techniques. In subjects where delineation of body subregions is compromised due to overlapping of tissue from two regions, lines are positioned midway through the intersection of the two regions.
Metabolic measures
OGTT
An OGTT is performed after an overnight fast. The dose of glucose is 1.75 g/kg of body weight to a maximum of 75 g. Plasma glucose and insulin is sampled every 30 minutes for 2 hours as previously described [38].
Blood samples
In addition to glucose and insulin, blood drawn at time 0 (OGTT) is analysed using standard techniques for full blood count, lipids (total cholesterol, HDL-C, triglycerides,), hs-CRP, oestradiol, testosterone, sex hormone binding globulin, lactate, hepatic transaminases (alanine aminotransferase, gamma-glutamyl transferase), renal function tests (urea, electrolytes, and creatinine). Blood (plasma and serum) is stored at -80°C in the Institute of Endocrinology and Diabetes, CHW for future analysis of homocystine (plasma), adipokines and vitamin B12.
Urine samples
Spot urine samples are collected and analysed for albumin to creatinine ratio using standard techniques.
Diet: Self monitoring, intake and eating behaviours
Diet checklist
Seven day diet checklists are completed by the participants for self monitoring, with assistance from the parent or guardian if required. The checklists were adapted from those used in previous studies [9].
Dietary 24 hour recall
Dietary intake is assessed using a methodology adapted from USDA five pass method as used in the 2007 Australian National Children's Nutrient and Physical Activity Survey [47]. In brief, at each time point (weeks 9, 12, 26, 38 and 52) food and beverage intake is measured using a three pass 24 hour dietary recall. To assist with estimation of portion sizes a food model book is provided with picture guides of common household measures and life size images, plates, bowls, glasses and amorphous dishes.
Eating behaviour
Eating behaviour is assessed by the Eating Pattern Inventory for Children [48].
Qualitative aspects of the diet
Qualitative aspects of the diet including, perceptions of cost, satiety, ease of compliance are assessed by a locally developed questionnaire. This questionnaire is completed by the parent or guardian.
Physical activity, sedentary behaviour and fitness
Physical activity and sedentary behaviour
The Children's Leisure Activities Study Survey (CLASS) is completed by the participant with assistance from the parent or guardian if required. CLASS assesses a range of physical activity and sedentary behaviours. CLASS has been validated for use among children, and used by adolescents aged 13-16 years in the Nepean Study [49]
Fitness
Assessment of aerobic fitness is performed using a Bruce treadmill protocol and breath by breath gas analysis. VO2 peak (maximal oxygen uptake) is expressed relative to body mass [50].
Metformin compliance
Metformin adherence is assessed by pill counts by the clinical trials pharmacist at CHW.
Data analysis
Data analyses will be carried out according to a pre-established plan, with the primary analysis based on intention to treat and with statistical support from the Clinical Epidemiology Unit, CHW. Analysis will be undertaken blinded, at the end of each phase of intervention. Generalised linear models using a repeated measures option will be used to assess differences in continuous variables between baseline and follow up by treatment group after adjusting for baseline covariates if necessary [51]. Mixed models will also be used to investigate changes over time. The mixed models procedure will take into account within subject correlations and missing data points. A time by group interaction will be included to investigate whether rates of change of adiposity and other primary outcomes are significantly different between the two study groups. In addition, the proportions of young people who were successful in decreasing adiposity will be compared between groups and the result expressed as number-needed-to-treat.
Discussion
Clinical insulin resistance and prediabetes in the paediatric population are rapidly emerging clinical problems with serious health outcomes. With appropriate management these conditions are potentially reversible or at least their progression can be delayed. This research study is the first trial designed to provide definitive data on the effective dietary management for this cohort. This is crucial information to prevent metabolic complications, type 2 diabetes and early cardiovascular disease.
Funding
Diabetes Australia Research Trust 2008, BUPA Health Foundation Australia Pty Limited (formerly MBF Foundation) 2008 to 2011, Heart Foundation (#G 08 S 3758), 2009 to 2010. Sarah Garnett is supported by a National Health and Medical Research Council Australian Clinical Research Fellowship (#457225).
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SPG, CTC, LAB participated in all aspects of the conception, design and funding of the study. MN participated in all aspects of the design of the study, with particular emphasis on design of the dietary intervention, and funding. KS, HJW, SS, GRA, MRK, SD provided medical expertise and design of the study. RP and CB were responsible for the development of the exercise intervention and testing. SB, KC and LH were responsible for the development of the dietary intervention. GH was responsible for the methodology of the 24 hour recall. All authors were responsible for drafting the manuscript and have read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Sarah P Garnett, Email: sarahg@chw.edu.au.
Louise A Baur, Email: louiseb3@chw.edu.au.
Manny Noakes, Email: Manny.Noakes@csiro.au.
Katharine Steinbeck, Email: kates@chw.edu.au.
Helen J Woodhead, Email: Helen.Woodhead@sesiahs.health.nsw.gov.au.
Susie Burrell, Email: susieb2@chw.edu.au.
Kerryn Chisholm, Email: kerryn@chw.edu.au.
Carolyn R Broderick, Email: carolyb2@chw.edu.au.
Robert Parker, Email: robertp@chw.edu.au.
Sukanya De, Email: sukayad@chw.edu.au.
Shubha Shrinivasan, Email: shubhas@chw.edu.au.
Lori Hopley, Email: lori.hopley@newcastle.edu.au.
Gilly Hendrie, Email: Gilly.Hendrie@csiro.au.
Geoffrey R Ambler, Email: geoffa@chw.edu.au.
Michael R Kohn, Email: michaek2@chw.edu.au.
Chris T Cowell, Email: chrisc@chw.edu.au.
Acknowledgements
We would like to thank FitnessFirst for use of the gym facilities, the physical trainers who are volunteering their time to train the participants and Alphapharm for providing metformin. We would also like to thank the food companies that are donating food to the study, which include the Australian Egg Corporation, George Weston, Simplot Australia Propriety Limited, Unilever Australia Limited and Meat and Livestock Australia.
References
- Washington RL. The Metabolic Syndrome - no longer an adult disease. J Pediatr. 2008;152:A1. [Google Scholar]
- Weiss R, Taksali SE, Tamborlane WV, Burgert TS, Savoye M, Caprio S. Predictors of changes in glucose tolerance status in obese youth. Diabetes Care. 2005;28:902–909. doi: 10.2337/diacare.28.4.902. [DOI] [PubMed] [Google Scholar]
- Eppens MC, Craig ME, Jones TW, Silink M, Ong S, Ping YJ. Type 2 diabetes in youth from the Western Pacific region: glycaemic control, diabetes care and complications. Curr Med Res Opin. 2006;22:1013–1020. doi: 10.1185/030079906X104795. [DOI] [PubMed] [Google Scholar]
- Ettinger LM, Freeman K, DiMartino-Nardi JR, Flynn JT. Microalbuminuria and abnormal ambulatory blood pressure in adolescents with type 2 diabetes mellitus. J Pediatr. 2005;147:67–73. doi: 10.1016/j.jpeds.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Alberti KG, Zimmet P, Shaw J. International Diabetes Federation: a consensus on Type 2 diabetes prevention. Diabet Med. 2007;24:451–463. doi: 10.1111/j.1464-5491.2007.02157.x. [DOI] [PubMed] [Google Scholar]
- Australian Government, Department of Health and Aging. Guidelines for the Management of Overweight and Obesity in Children and Adolescents Part 5 - Conventional Weight-management Strategies. http://www.health.gov.au/internet/main/publishing.nsf/Content/893169B10DD846FCCA256F190003BADA/$File/children_part5.pdf Accessed 2006.
- Gibson LJ, Peto J, Warren JM, dos Santos Silva I. Lack of evidence on diets for obesity for children: a systematic review. Int J Epidemiol. 2006;35:1544–1552. doi: 10.1093/ije/dyl208. [DOI] [PubMed] [Google Scholar]
- Krieger JW, Sitren HS, Daniels MJ, Langkamp-Henken B. Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: a meta-regression 1. Am J Clin Nutr. 2006;83:260–274. doi: 10.1093/ajcn/83.2.260. [DOI] [PubMed] [Google Scholar]
- Noakes M, Keogh JB, Foster PR, Clifton PM. Effect of an energy-restricted, high-protein, low-fat diet relative to a conventional high-carbohydrate, low-fat diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr. 2005;81:1298–1306. doi: 10.1093/ajcn/81.6.1298. [DOI] [PubMed] [Google Scholar]
- McMillan-Price J, Petocz P, Atkinson F, O'neill K, Samman S, Steinbeck K, Caterson I, Brand-Miller J. Comparison of 4 diets of varying glycemic load on weight loss and cardiovascular risk reduction in overweight and obese young adults: a randomized controlled trial. Arch Intern Med. 2006;166:1466–1475. doi: 10.1001/archinte.166.14.1466. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noakes M. The role of protein in weight management. Asia Pac J Clin Nutr. 2008;17(Suppl 1):169–171. [PubMed] [Google Scholar]
- Bowen J, Noakes M, Clifton PM. Appetite regulatory hormone responses to various dietary proteins differ by body mass index status despite similar reductions in ad libitum energy intake. J Clin Endocrinol Metab. 2006;91:2913–2919. doi: 10.1210/jc.2006-0609. [DOI] [PubMed] [Google Scholar]
- Leidy HJ, Carnell NS, Mattes RD, Campbell WW. Higher protein intake preserves lean mass and satiety with weight loss in pre-obese and obese women. Obesity (Silver Spring) 2007;15:421–429. doi: 10.1038/oby.2007.531. [DOI] [PubMed] [Google Scholar]
- Westerterp-Plantenga MS, Luscombe-Marsh N, Lejeune MP, Diepvens K, Nieuwenhuizen A, Engelen MP, Deutz NE, Azzout-Marniche D, Tome D, Westerterp KR. Dietary protein, metabolism, and body-weight regulation: dose-response effects. Int J Obes (Lond) 2006;30(Suppl 3):S16–S23. doi: 10.1038/sj.ijo.0803487. [DOI] [Google Scholar]
- Blaak EE Prevention and treatment of obesity and related complications: a role for protein? Int J Obes (Lond) 200630Suppl 3S24–S27. 10.1038/sj.ijo.080348816570101 [DOI] [Google Scholar]
- Astrup A. Carbohydrates as macronutrients in relation to protein and fat for body weight control. Int J Obes (Lond) 2006;30(Suppl 3):S4–S9. doi: 10.1038/sj.ijo.0803485. [DOI] [Google Scholar]
- Collins CE, Warren J, Neve M, McCoy P, Stokes BJ. Measuring effectiveness of dietetic interventions in child obesity: a systematic review of randomized trials. Arch Pediatr Adolesc Med. 2006;160:906–922. doi: 10.1001/archpedi.160.9.906. [DOI] [PubMed] [Google Scholar]
- Sothern, Udall JN Jr, Suskind RM, Vargas A, Blecker U. Weight loss and growth velocity in obese children after very low calorie diet, exercise, and behavior modification. Acta Paediatr. 2000;89:1036–1043. doi: 10.1080/713794562. [DOI] [PubMed] [Google Scholar]
- Oude LH, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, Summerbell CD. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009. [DOI] [PubMed]
- The Diabetes Prevention (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz ML, Shaibi GQ, Weigensberg MJ, Spruijt-Metz D, Ball GD, Goran MI. Pediatric obesity and insulin resistance: chronic disease risk and implications for treatment and prevention beyond body weight modification. Annu Rev Nutr. 2005;25:435–468. doi: 10.1146/annurev.nutr.25.050304.092625. [DOI] [PubMed] [Google Scholar]
- Shaibi GQ, Cruz ML, Ball GD, Weigensberg MJ, Salem GJ, Crespo NC, Goran MI. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc. 2006;38:1208–1215. doi: 10.1249/01.mss.0000227304.88406.0f. [DOI] [PubMed] [Google Scholar]
- Bell LM, Watts K, Siafarikas A, Thompson A, Ratnam N, Bulsara M, Finn J, O'Driscoll G, Green DJ, Jones TW, Davis EA. Exercise alone reduces insulin resistance in obese children independently of changes in body composition. J Clin Endocrinol Metab. 2007;92:4230–4235. doi: 10.1210/jc.2007-0779. [DOI] [PubMed] [Google Scholar]
- Quinn SM, Baur LA, Garnett SP, Cowell CT. Treatment of clinical insulin resistance in children: a systematic review. Obes Rev. 2010;11:722–730. doi: 10.1111/j.1467-789X.2009.00697.x. [DOI] [PubMed] [Google Scholar]
- Jones KL, Arslanian S, Peterokova VA, Park JS, Tomlinson MJ. Effect of metformin in pediatric patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2002;25:89–94. doi: 10.2337/diacare.25.1.89. [DOI] [PubMed] [Google Scholar]
- Lord JM, Flight IH, Norman RJ. Metformin in polycystic ovary syndrome: systematic review and meta-analysis. BMJ. 2003;327:951–953. doi: 10.1136/bmj.327.7421.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwimmer JB, Middleton MS, Deutsch R, Lavine JE. A phase 2 clinical trial of metformin as a treatment for non-diabetic paediatric non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2005;21:871–879. doi: 10.1111/j.1365-2036.2005.02420.x. [DOI] [PubMed] [Google Scholar]
- Freemark M. Pharmacotherapy of childhood obesity: an evidence-based, conceptual approach. Diabetes Care. 2007;30:395–402. doi: 10.2337/dc06-1569. [DOI] [PubMed] [Google Scholar]
- Yeckel CW, Weiss R, Dziura J, Taksali SE, Dufour S, Burgert TS, Tamborlane WV, Caprio S. Validation of insulin sensitivity indices from oral glucose tolerance test parameters in obese children and adolescents. J Clin Endocrinol Metab. 2004;89:1096–1101. doi: 10.1210/jc.2003-031503. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008;31(Suppl 1):S55–S60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- Azziz R. Controversy in clinical endocrinology: diagnosis of polycystic ovarian syndrome: the Rotterdam criteria are premature. J Clin Endocrinol Metab. 2006;91:781–785. doi: 10.1210/jc.2005-2153. [DOI] [PubMed] [Google Scholar]
- Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics. 1996;98:649–658. [PubMed] [Google Scholar]
- Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes. 2007;8:299–306. doi: 10.1111/j.1399-5448.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- Altman DG, Bland JM. Treatment allocation by minimisation. BMJ. 2005;330:843. doi: 10.1136/bmj.330.7495.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Royston P, Day S. Minim: allocation by minimisation in clinical trials. 2008. http://www-users.york.ac.uk/~mb55/guide/minim.htm
- Garnett SP, Srinivasan S, Birt SG, Ambler GR, Lawrie EA, Cowell CT, Craig ME. Evaluation of glycaemic status in young people with clinical insulin resistance; fasting glucose, fasting insulin or an oral glucose tolerance test? Clin Endocrinol (Oxf) 2010;72(4):475–80. doi: 10.1111/j.1365-2265.2009.03677.x. [DOI] [PubMed] [Google Scholar]
- Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: a randomized, controlled trial. Pediatrics. 2007;119:517–525. doi: 10.1542/peds.2006-1746. [DOI] [PubMed] [Google Scholar]
- Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Australian Government, Department of Health and Aging. Australia's physical activity recommendations for 12-18 year olds. http://www.health.gov.au/internet/main/publishing.nsf/Content/phd-physical-activity-youth-pdf-cnt.htm Accessed 2008.
- Norton K, Olds T, (editors) Anthropometrica. Sydney: University of NSW Press; 1996. [Google Scholar]
- Garnett SP, Baur LA, Cowell CT. Waist-to-height ratio: a simple option for determining excess central adiposity in young people. Int J Obes (Lond) 2008;32:1028–1030. doi: 10.1038/ijo.2008.51. [DOI] [PubMed] [Google Scholar]
- Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett SP, Baur LA, Srinivasan S, Lee JW, Cowell CT. Body mass index and waist circumference in midchildhood and adverse cardiovascular disease risk clustering in adolescence. Am J Clin Nutr. 2007;86:549–555. doi: 10.1093/ajcn/86.3.549. [DOI] [PubMed] [Google Scholar]
- Srinivasan S, Ambler GR, Baur LA, Garnett SP, Tepsa M, Yap F, Ward GM, Cowell CT. Randomized controlled trial of metformin for obesity and insulin resistance in children and adolescents - improvement in body composition and fasting insulin. J Clin Endocrinol Metab. 2006. [DOI] [PubMed]
- Australian Government, Department of Health and Ageing. 2007 Australian National Children's Nutrition and Physical Activity Survey. http://www.health.gov.au/internet/main/publishing.nsf/Content/phd-physical-activity-youth-pdf-cnt.htm Accessed 2008.
- Schacht M, Richter-Appelt H, Schulte-Markwort M, Hebebrand J, Schimmelmann BG. Eating Pattern Inventory for Children: a new self-rating questionnaire for preadolescents. J Clin Psychol. 2006;62:1259–1273. doi: 10.1002/jclp.20300. [DOI] [PubMed] [Google Scholar]
- Telford A, Salmon J, Jolley D, Crawford D. Reliability and validity of physical activity questionnaires for children: the Children's Leisure Activities Study Survey (CLASS) Pediatr Exerc Sci. 2004;16:64–79. doi: 10.1123/pes.21.3.339. [DOI] [PubMed] [Google Scholar]
- Unnithan VB, Murray LA, Timmons JA, Buchanan D, Paton JY. Reproducibility of cardiorespiratory measurements during submaximal and maximal running in children. Br J Sports Med. 1995;29:66–71. doi: 10.1136/bjsm.29.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers AJ, Altman DG. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]