Abstract
Purpose
We evaluated various preoperative anterior segment parameters measured with a Pentacam rotating Scheimpflug camera and compared them with those of conventional methods. We also evaluated the effect of different parameters on corneal endothelial cells after cataract surgery.
Methods
Pentacam examination was performed in 88 eyes from 88 patients to evaluate central anterior chamber depth (ACDpentacam), nuclear density (Densitometrypentacam), anterior chamber volume (ACV), and lens thickness (LTpentacam). We compared values of ACDpentacam with those of ultrasound (ACDsono) and also compared Densitometrypentacam values with those of Lens Opacities Classification System (LOCS III) classification. We evaluated the effect of the following preoperative values measured with Pentacam on postoperative endothelial cell loss: pupil size measured both preoperatively and before capsulorrhexsis (PupilCCC), amount of viscoelastics, and LT measured by ultrasound (LTsono).
Results
A significant concordance was found between the two grading methods of nuclear opacity: Densitometrypentacam and LOCS III classification (τb = 0.414, p = 0.000). We also found a positive correlation between ACDpentacam and ACDsono (r = 0.823, p = 0.000) and between ACDpentacam and ACV (r = 0.650, p = 0.000). There were significant differences between the results of LTpentacam and LTsono. The final regression model identified Densitometrypentacam, viscoelastics and PupilCCC as independent predictors of decreased postoperative corneal endothelial cell density (CD) at postoperative day 3, and Densitometrypentacam, viscoelastics, and ACV as independent predictors of decreased CD two months postoperatively (p<0.05).
Conclusions
Good agreement was found between all results obtained with the Pentacam and conventional methods except LT. Analyzing anterior chamber parameters preoperatively using Pentacam could be helpful to predict postoperative endothelial cell loss.
Keywords: Anterior segment parameters, Corneal endothelium, Pentacam
The Pentacam (Oculus Inc., Wetzlar, Germany) offers evaluation of the entire anterior segment from the anterior corneal surface to the posterior lens surface using a rotating Scheimpflug camera (Oculus Inc.). The noncontact measuring process takes two seconds and performs 12 to 50 single captures. We evaluated the accordance of various preoperative anterior segment parameters measured by the Pentacam with those of conventional methods, and we also used Pentacam data to predict post-cataract surgery corneal endothelial cell loss.
Materials and Methods
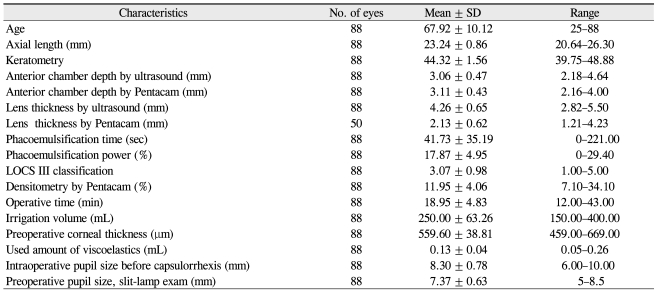
Eighty-eight eyes from 88 patients scheduled for routine cataract surgery were selected prospectively. Baseline patient data are shown in Table 1. Exclusion criteria for the study were eyes with significant corneal opacity, previous intraocular surgery, trauma, glaucoma, uveitis, Fuchs' endothelial dystrophy, other abnormalities that could cause significant endothelial cell impairment independent of surgery, eyes with small pupils that required iris retractors, and eyes with intraoperative complications such as posterior capsule rupture or postoperative complications.
Table 1.
Baseline patient data
LOCS III = Lens Opacities Classification System.
Surgical technique
All surgeries were performed under retrobulbar anesthesia by the same surgeon. A 3.0-mm clear corneal incision was made in the superior quadrant. A capsulorrhexis approximately 5.0 mm in diameter was created with forceps, and cortical cleaving hydrodissection was then performed. The nucleus was emulsified using the stop-and-chop technique. After irrigation and aspiration of the cortex, a foldable acrylic intraocular lens (SN60WF; Alcon, Fort Worth, TX, USA) was implanted in the bag. The same irrigating solution (balanced salt solution [BSS]) and ophthalmic viscoelastics were used in all patients.
Intraoperatively, we recorded phacoemulsification time (seconds), phacoemulsification power (%), total operative time (minutes), and amount of BSS irrigating solution (mL) used.
Lens opacity measurement
At the preoperative slit-lamp examination, nuclear opacity was graded from 1 to 6 using the Lens Opacities Classification System (LOCS III) by two observers. We selected data that showed agreement of grading scores between these two observers.
The Pentacam provides an image of nearly the entire lens along with an objective measurement of the lens density in the chosen area, which ranges from 0 to 100. To evaluate the nuclear density via Pentacam, we needed Scheimpflug images and used enhanced densitometry analysis. One observer evaluated the densitometry of the area corresponding to the lens nucleus center two times, and we took the mean value to use as the lens density.
Lens thickness, anterior chamber depth and anterior chamber volume measurement
Applanation ultrasonography (Compact II device, Quantel Medical) was done to evaluate the lens thickness (LTsono, mm), anterior chamber depth (ACD, mm) and anterior chamber volume (ACV, mm3). ACD was defined as the axial distance between the anterior surface of the cornea and the anterior surface of the lens. ACV was calculated from the integration (integral calculus) of the distances between the back surface of the cornea and the iris of the respective lens in a 12-mm diameter around the corneal apex. LT was defined as the axial distance between the anterior chamber surface of the lens and the posterior surface of the lens. All measurements were done by one experienced observer following pupil dilation.
Pentacam was performed to evaluate central ACD (from the epithelium) and lens thickness (LTpentacam). The anterior chamber depth (ACDpentacam) was measured at the apex of the cornea. Pupil dilation was necessary to measure LTpentacam.
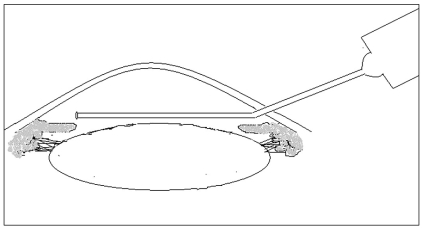
Pupil size and amount of viscoelastics measurement
Preoperatively, the fully dilated pupil size (Pupilpreop) was measured by slit-lamp biomicrosopy after a two-hour instillation of mydriatics (tropicamide 0.5%, phenylephrine hydrochloride 0.5% Mydrin®-P; Santen Pharmaceutical Co., Osaka, Japan). During surgery, the dilated pupil size was measured (PupilCCC) after injection of viscoelastics (sodium hyaluronic acid 1% Hyal 2000; LG life Sciences, Korea) into the anterior chamber using a blunt-ended injection needle of known length before anterior capsulotomy (Fig. 1).
Fig. 1.
Measurement of pupil size a measured before capsulorrhexis (PupilCCC). PupilCCC was measured before capsulorrhexis using a blunt-ended, viscoelastics injection needle of known length.
For capsulorrhexis (CCC), we injected just enough viscoelastics into the anterior chamber to observe a slight backward movement of the lens-iris diaphragm. We then measured the amount of viscoelastics used for CCC by subtracting the amount remaining after CCC from the initial amount.
Endothelial cell evaluation
Corneal endothelial injury associated with phacoemulsification was assessed by specular microscopy in terms of the changes in cell density (CD) and cell morphology.
To evaluate central corneal endothelial cell density, specular microscopy photographs of the central corneal endothelium were taken using a noncontact specular microscope (Nonon Robo, Konan, Japan). We analyzed a minimum of 40 endothelial cells to calculate the endothelial cell density.
Specular microscopic examination, including endothelial cell density (cells/mm2), coefficient of variation (CV) and hexagonality (HA), was performed preoperatively and again at three days and at two months postoperatively.
We calculated the percentage change of CD, CV and HA as follows: percentage change of CD = (preoperative CD-postoperative CD)×100/preoperative CD, percentage change of CV = (preoperative CV-postoperative CV)×100/preoperative CV, and percentage change of HA = (preoperative HA-postoperative HA)×100/preoperative HA.
Statistical analysis
Statistical analysis was performed with the SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). The associations of variables were assessed by Pearson's correlation coefficient and paired t-test. To evaluate the correlation of two methods (LOCS and Pentacam densitometry), we used Kendall's tau-b value.
We selected seven variables (ACDpentacam, ACDsono, Pupilpreop, PupilCCC, LTsono, amount of viscoelastics, and Densitometrypentacam) that could be associated with endothelial cell change.
The univariate associations of the seven variables with the percentage change of CD, CV and HA were evaluated using simple regression analysis. We used a multiple linear regression model to evaluate the impact of various risk factors on CD change alone. The seven variables were entered into this multiple regression analysis. A stepwise regression was used, and a p-value of 0.50 or less was required for a variable to remain in the model.
Results
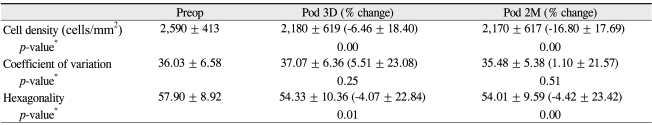
Baseline patient data are shown in Table 1. Changes of CD, CV and HA over time are shown in Table 2. Our data shows the wound-healing process of corneal endothelium after cataract surgery, and we observed CV recovery at two months postoperatively.
Table 2.
Change of endothelial cell density, coefficient of variation and hexagonality over time
Preop=preoperative measurement; Pod 3D = measurement at postoperative 3 day; Pod 2M = measurement at postoperative 2 month.
*Paired t-test, compared with preoperative value at each follow-up.
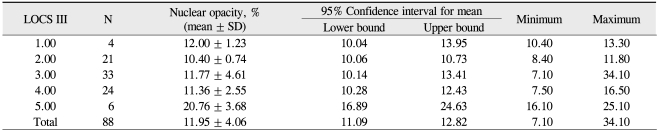
Mean Densitometrypentacam values according to grading by LOCS III classification are shown in Table 3. No eyes in our study had a nuclear opacity grade of 6 by LOCS III classification. A significant degree of concordance was found between Densitometrypentacam and LOCS III classification (τb = 0.414, p = 0.000) for nuclear opacity.
Table 3.
Nuclear opacity measured with Pentacam distribution according to LOCS III classification
LOCS III = Lens Opacities Classification System. τb(Kendall's tau b) = 0.414, p = 0.000.
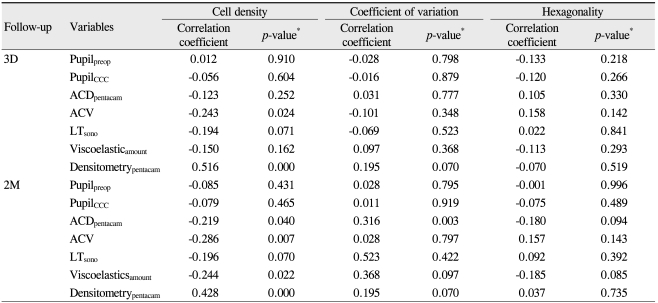
Table 4 summarizes the univariate associations of the seven variables with the percentage of endothelial cell change (CD, CV and HA).
Table 4.
Univariate association of our seven variables with the significance values predicting percentage change of endothelial cell density, coefficient of variation and, hexagonality at postoperative day 3 (3D) and month 2 (2M)
Pupilpreop = pupil size as measured preoperatively; PupilCCC = pupil size a measured before capsulorrhexis; ACDpentacam = anterior chamber depth measured by Pentacam; ACV = anterior chamber volume; LTsono=lens thickness measured by ultrasound; Viscoelasticamount = amount of viscoelastic; Densitometrypentacam = lens opacity measured by Pentacam densitometry.
*p < 0.05, statistically significant.
Univariate analysis demonstrated that ACV and Densitometrypentacam were associated with the percentage decrease of CD at postoperative day 3. ACDpentacam, ACV, amount of viscoelastics, and Densitometrypentacam were associated with the percentage decrease of CD two months postoperatively. ACDpentacam was associated with the percentage change of CV at two months postoperatively.
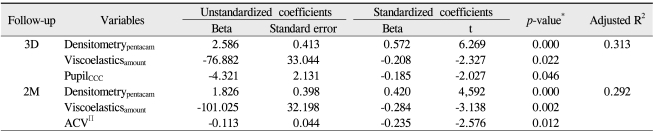
A multiple linear regression analysis was performed to identify the best set of independent predictors for the percentage decrease of CD. These data are shown in Table 5. The final model identified Densitometrypentacam, viscoelastics and PupilCCC as independent predictors of decreased CD at postoperative day 3 (adjusted R2 = 31.3%) and Densitometrypentacam, viscoelastics and ACV as independent predictors of decreased CD at two months postoperatively (adjusted R2 = 29.2%).
Table 5.
Final stepwise, multiple regression model for predicting percentage change of endothelial cell density at postoperative day 3 (3D) and month 2 (2M)
Densitometrypentacam = lens opacity measured by Pentacam densitometry; Viscoelasticsamount = amount of viscoelastics; PupilCCC = pupil size as measured before capsulorrhexis; ACVΠ = anterior chamber volume.
*p < 0.05, statistically significant.
We found that intraoperative PupilCCC increased after injection of viscoelastics. However, we cannot compare these two values directly because PupilCCC was measured intraoperatively at the papillary plane by an injection needle of known length, and Pupilpreop was measured using the slit-lamp biomicroscopy scale.
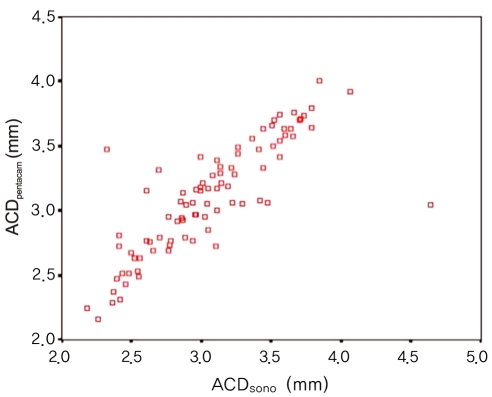
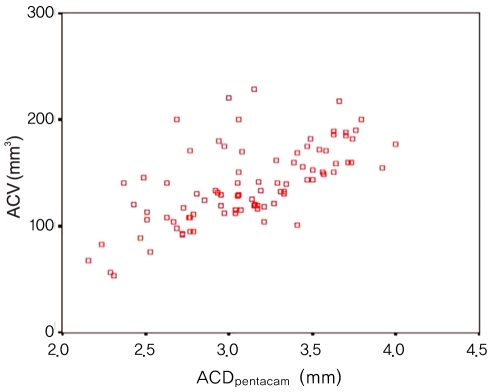
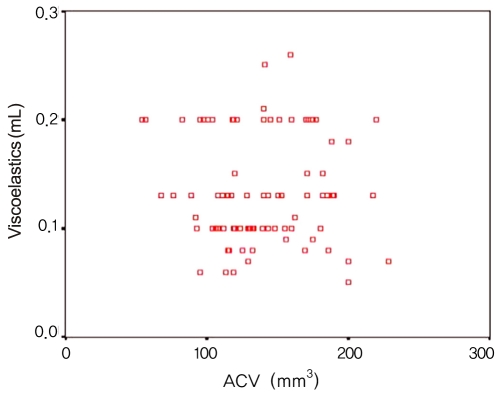
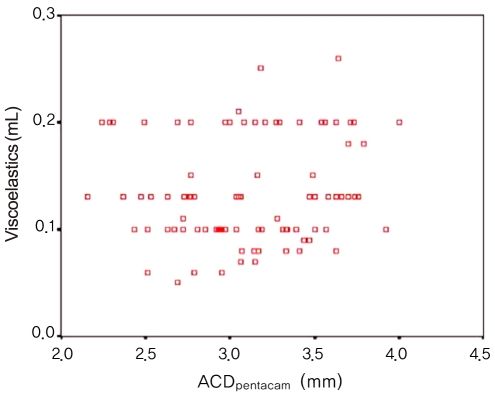
Fig. 2 shows the correlation plot between ACDpentacam and ACDsono (r = 0.823. p = 0.000). Fig. 3 shows the correlation between ACDpentacam and ACV (r = 0.650, p = 0.000). Fig. 4 shows the correlation between ACV and amount of viscoelastic (viscoelasticamount; r = -0.021, p = 0.85). Fig. 5 shows the correlation between ACDpentacam and viscoelasticamount (r = 0.123, p = 0.253).
Fig. 2.
Correlation of anterior chamber depth (mm) by Pentacam (ACDpentacam) and ultrasound (ACDsono) (r = 0.822, p < 0.05).
Fig. 3.
Correlation between anterior chamber depth (ACD) measured by Pentacam (ACDpentacam) and anterior chamber volume (ACV) (r = 0.650, p = 0.000).
Fig. 4.
Correlation between anterior chamber volume (ACV) and injected amount of viscoelastics before capsulorrhexis (r = -0.021, p = 0.850).
Fig. 5.
Correlation between anterior chamber depth by Pentacam (ACDpentacam) and injected amount of viscoelastics before capsulorrhexis (r = 0.123, p = 0.253).
Discussion
The Pentacam allows evaluation of the entire anterior segment from the anterior corneal surface to the posterior lens surface using a rotating Scheimpflug camera [1-7]. The noncontact measuring process takes two seconds and performs 12 to 50 single captures. The Pentacam has various functions, including the ability to measure ACV and nuclear density, which can be expressed as continuous numeric data. Until now, we could only evaluate nuclear opacity by categorizing with systems such as LOCS classification [7-9]. The Scheimpflug image provides the basis for objective, precise quantification of lens opacity [7]. The lens density is standardized from 0 to 100. Therefore, 0 means the lens shows no clouding, and 100 means the lens is completely opaque (Pentacam instruction manual, Oculus Inc.). Although we observed lens opacities from of LOCS III classification 1 to 5 in our study, we only obtained a relatively small range of Densitometrypentacam values from 7.10 to 34.10%. We might have subjectively overestimated the lens opacity using the LOCS III classification.
Since Densitometrypentacam data are not categorical data like LOCS classifications, we could more easily access statistical analysis using the former data type. We found a significant concordance between the LOCS III and Densitometrypentacam methods.
Anterior chamber values are necessary for calculating intraocular lens power when planning surgical procedures. Precise anterior chamber measurements are essential for performing exact biometry and for surgical planning [5,6].
Several methods for measuring the anterior chamber depth are available [5,6,10]. The Pentacam and standard ultrasound devices define ACD as the distance between the anterior surface of the cornea and the anterior surface of the lens.
Ultrasound devices have become the most commonly used methods to measure ACD. Contact devices such as the ultrasound have disadvantages, including corneal indentations, the risk for corneal abrasions and infections, off-axis measurement, and possible precorneal echo spikes [10]. Pentacam imaging is a relatively new, noncontact automatic optical technique in ophthalmology. Although different methods to determine ACD may yield significantly different results [3,10], mean ACD measurements of the Pentacam and ultrasound were significantly correlated in our study (r = 0.823, p = 0.000), a finding that was similar to previous reports [2,6].
The Pentacam can evaluate ACV as well as ACD [4,5]. Both our study and previous reports found a good correlation between ACD and ACV (r = 0.650) [1,5].
We tried to evaluate LT using the Pentacam (LTpentacam) and to compare these values with those obtained by ultrasound (LTsono) in 50 eyes. There was a significant difference between LT measured by Pentacam (mean ± SC, 2.13 ± 0.62) and by ultrasound (mean ± SD, 4.42 ± 0.79) (paired t-test, p<0.05). The Pentacam LT values in our study were lower than other reports [11,12] and it was impossible to constantly measure LTpentacam correctly. We suspect that this is because the posterior surface of the lens cannot be precisely determined with Scheimpflug imaging, which depends on pupil dilation. Previous reports have emphasized pupil dilation for measuring LTpentacam (Pentacam instruction manual). Based on this information, we used the value of LTsono to evaluate the effect on postoperative endothelial cell loss.
In our study, LTsono showed a distribution of 2.82 to 5.50 with a mean value of 4.26 ± 0.66 mm, which is comparable to findings of other reports [11,12]. Jivrajka et al. [12] reported that LT tended to be thicker in older patients and in shorter eyes. In our study, LTsono showed no correlation with axial length (r = -0.035, p = 0.748) and had only a weak correlation with age (r = 0.203, p = 0.058). We found that LTpentacam was unsuitable for determining true lens thickness.
Several studies that evaluated the percentage of endothelial cell loss after phacoemulsification have been published [13-15]. The average loss reported after phacoemulsification varies between 4% and 25% [13]. In our study, the percentage loss of endothelial cell density at two months postoperatively was about 16%. Operative factors possibly associated with corneal endothelial injury include ultrasound energy, turbulence of the irrigating solution, instrument contact, air bubbles, touch by nucleus fragment, axial length, phacoemulsification time, nucleus grade, anterior chamber depth, and age [13-15]. Recent advances in endocapsular phacoemulsification procedures, instruments and viscoelastic substances appear to have helped decrease the degree of endothelial damage. At first, we intended to evaluate the relationship between seven anterior segment parameters and three endothelial cell indices (CD, CV and HA), but we did not observe a correlation between either anterior segment parameters and CV or anterior segment parameters and HA, except for the relationship between ACD and CV at two months postoperatively (Table 4). Therefore, we evaluated the correlation between anterior segment parameters and CD alone in our final regression model (Table 5).
We expected that the amount of injected viscoelastics required for adequate lens-iris diaphragm backward movement (and thus for safe capsulorrhexis) would be correlated with ACV or ACDpentacam. However, there was no correlation between ACV and viscoelasticamount (r = -0.021, p = 0.85) or between ACDpentacam and viscoelasticamount (r = 0.123, p = 0.253). We suspected the reason is that viscoelasticamount use involves pushing back the lens-iris diaphragm for adequate capsulotomy, which is also affected by zonular laxity and posterior (vitreous) pressure of each patient during surgery, not only by the real total ACV. In our study, the amount of viscoelastics used was a factor affecting endothelial cell density at both three days and two months postoperatively. Additionally, small pupils are an added risk with any technique for cataract extraction [16,17].
Although the endocapsular technique remains popular, anterior chamber phacoemulsification may be more advantageous in specific cases, such as those with lens subluxation, unstable zonules or extremely hard nuclei. In these cases, there is less risk of injury to the posterior capsule if the procedure is performed in the anterior chamber [18]. Also, in small-pupil phacoemulsification, a method can be used that manipulates part of the lens into the anterior chamber through the pupil to maintain the pupil in a semidilated state [19]. Therefore, in small pupil phacoemulsification, pupil size can be a factor that affects corneal endothelial cells.
Although we cannot compare PupilCCC and Pupilpreop directly due to different measuring scales, our results showed that PupilCCC (rather than Pupilpreop) could have an effect on postoperative endothelial cell density.
We concluded that preoperative values measured by Pentacam were suitable for measuring all anterior segment parameters except LT, and anterior segment values measured by Pentacam were good predictors for postoperative endothelial cell loss.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ucakhan OO, Gesoglu P, Ozkan M, Kanpolat A. Corneal elevation and thickness in relation to the refractive status measured with the Pentacam Scheimpflug system. J Cataract Refract Surg. 2008;34:1900–1905. doi: 10.1016/j.jcrs.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Park JY, Kim SY, Jung MS. Comparison of corneal thickness and anterior chamber depth measured with Orbscan, Pentacam, and Ultrasound Pachymetry. J Korean Ophthalmol Soc. 2009;50:664–669. [Google Scholar]
- 3.Shin YJ, Kim NH, Kim DH. Comparison of Pentacam with Orbscan. J Korean Ophthalmol Soc. 2007;48:637–641. [Google Scholar]
- 4.Kwon SM, Oh HC, Lee DJ, et al. Comparison of anterior segment parameters in angle-closure glaucoma using Scheimpflug camera. J Korean Ophthalmol Soc. 2009;50:128–134. [Google Scholar]
- 5.Rabsilber TM, Khoramnia R, Auffarth GU. Anterior chamber measurements using Pentacam rotating Scheimpflug camera. J Cataract Refract Surg. 2006;32:456–459. doi: 10.1016/j.jcrs.2005.12.103. [DOI] [PubMed] [Google Scholar]
- 6.Nemeth G, Vajas A, Kolozsvari B, et al. Anterior chamber depth measurements in phakic and pseudophakic eyes: Pentacam versus ultrasound device. J Cataract Refract Surg. 2006;32:1331–1335. doi: 10.1016/j.jcrs.2006.02.057. [DOI] [PubMed] [Google Scholar]
- 7.Pei X, Bao Y, Chen Y, Li X. Correlation of lens density measured using the Pentacam Scheimpflug system with the Lens Opacities Classification System III grading score and visual acuity in age-related nuclear cataract. Br J Ophthalmol. 2008;92:1471–1475. doi: 10.1136/bjo.2007.136978. [DOI] [PubMed] [Google Scholar]
- 8.Kubo E, Kumamoto Y, Tsuzuki S, Akagi Y. Axial length, myopia, and the severity of lens opacity at the time of cataract surgery. Arch Ophthalmol. 2006;124:1586–1590. doi: 10.1001/archopht.124.11.1586. [DOI] [PubMed] [Google Scholar]
- 9.Chylack LT, Jr, Wolfe JK, Singer DM, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111:831–836. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 10.Koranyi G, Lydahl E, Norrby S, Taube M. Anterior chamber depth measurement: a-scan versus optical methods. J Cataract Refract Surg. 2002;28:243–247. doi: 10.1016/s0886-3350(01)01039-2. [DOI] [PubMed] [Google Scholar]
- 11.Hoffer KJ. Axial dimension of the human cataractous lens. Arch Ophthalmol. 1993;111:914–918. doi: 10.1001/archopht.1993.01090070032014. [DOI] [PubMed] [Google Scholar]
- 12.Jivrajka R, Shammas MC, Boenzi T, et al. Variability of axial length, anterior chamber depth, and lens thickness in the cataractous eye. J Cataract Refract Surg. 2008;34:289–294. doi: 10.1016/j.jcrs.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Walkow T, Anders N, Klebe S. Endothelial cell loss after phacoemulsification: relation to preoperative and intraoperative parameters. J Cataract Refract Surg. 2000;26:727–732. doi: 10.1016/s0886-3350(99)00462-9. [DOI] [PubMed] [Google Scholar]
- 14.Hayashi K, Hayashi H, Nakao F, Hayashi F. Risk factors for corneal endothelial injury during phacoemulsification. J Cataract Refract Surg. 1996;22:1079–1084. doi: 10.1016/s0886-3350(96)80121-0. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien PD, Fitzpatrick P, Kilmartin DJ, Beatty S. Risk factors for endothelial cell loss after phacoemulsification surgery by a junior resident. J Cataract Refract Surg. 2004;30:839–843. doi: 10.1016/S0886-3350(03)00648-5. [DOI] [PubMed] [Google Scholar]
- 16.Cho YK, Kim EC, Kim MS. The surgical results of phacoemulsification cataract surgery according to pupil size. J Korean Ophthalmol Soc. 2007;48:761–767. [Google Scholar]
- 17.Gimbel HV. Nucleofractis phacoemulsification through a small pupil. Can J Ophthalmol. 1992;27:115–119. [PubMed] [Google Scholar]
- 18.Alio JL, Mulet ME, Shalaby AM, Attia WH. Phacoemulsification in the anterior chamber. J Cataract Refract Surg. 2002;28:67–75. doi: 10.1016/s0886-3350(01)01018-5. [DOI] [PubMed] [Google Scholar]
- 19.Fine IH, Packer M, Hoffman RS. Phacoemulsification in the presence of a small pupil. In: Steinert RF, editor. Cataract surgery: technique, complication and management. 2nd ed. Philadelphia: Saunders; 2004. pp. 211–222. [Google Scholar]