Abstract
BACKGROUND
Prevalence of unhealthy alcohol use among medical inpatients is high.
OBJECTIVE
To characterize the course and outcomes of unhealthy alcohol use, and factors associated with these outcomes.
DESIGN
Prospective cohort study.
PARTICIPANTS
A total of 287 medical inpatients with unhealthy alcohol use.
MAIN MEASURES
At baseline and 12 months later, consumption and alcohol-related consequences were assessed. The outcome of interest was a favorable drinking outcome at 12 months (abstinence or drinking “moderate” amounts without consequences). The independent variables evaluated included demographics, physical/sexual abuse, drug use, depressive symptoms, alcohol dependence, commitment to change (Taking Action), spending time with heavy-drinking friends and receipt of alcohol treatment (after hospitalization). Adjusted regression models were used to evaluate factors associated with a favorable outcome.
KEY RESULTS
Thirty-three percent had a favorable drinking outcome 1 year later. Not spending time with heavy-drinking friends [adjusted odds ratio (AOR) 2.14, 95% CI: 1.14–4.00] and receipt of alcohol treatment [AOR (95% CI): 2.16(1.20–3.87)] were associated with a favorable outcome. Compared to the first quartile (lowest level) of Taking Action, subjects in the second, third and highest quartiles had higher odds of a favorable outcome [AOR (95% CI): 3.65 (1.47, 9.02), 3.39 (1.38, 8.31) and 6.76 (2.74, 16.67)].
CONCLUSIONS
Although most medical inpatients with unhealthy alcohol use continue drinking at-risk amounts and/or have alcohol-related consequences, one third are abstinent or drink “moderate” amounts without consequences 1 year later. Not spending time with heavy-drinking friends, receipt of alcohol treatment and commitment to change are associated with this favorable outcome. This can inform efforts to address unhealthy alcohol use among patients who often do not seek specialty treatment.
KEY WORDS: unhealthy alcohol use, medical inpatients, factors associated with drinking and consequences
INTRODUCTION
Unhealthy alcohol use (alcohol consumption that increases the risk of health consequences and includes abuse and dependence) is a major public health concern1,2. In primary care settings the prevalence of unhealthy alcohol use is 7 to 20% or more, with most people not suffering from alcohol dependence3. However, in medical hospital settings, the proportion of patients with unhealthy alcohol use who meet the criteria for alcohol dependence is high4. For example, in four general hospitals in Germany, Freyer-Adam et al. found that 61% of inpatients with unhealthy alcohol use had alcohol dependence5. In a large urban safety-net hospital in the US (the sample for the current study), the proportion was 77%4,6. As such, the problem of unhealthy alcohol use in inpatient medical settings is likely to differ from that in other (particularly outpatient) health care settings.
In general populations, the natural history of drinking among those with dependence has been well studied, and social and personal factors have been identified as predictors of natural recovery. Epidemiologic studies indicate that there is a substantial proportion of individuals with alcohol dependence who will be in recovery 12 months later7. Age and participation in self-help or treatment affect the course of substance dependence and male gender, depression, heroin and cocaine use, divorce and low level of education are related to worse outcome8. “Resolution” (abstinence for more than 2 years) has been linked to heavier drinking practices and negative life events during the year before the onset of abstinence9.
Nevertheless, the course of drinking and predictors of favorable drinking outcome among medical inpatients are not well known. Describing both consumption and consequence outcomes allows assessment of a range of outcomes among diverse patients. It is of clinical interest among inpatients, especially because some may choose a “moderate” drinking goal during brief counseling sessions, and may do so without negative consequences even if previously diagnosed with dependence. Moderate drinking may be an appropriate goal if patients can do so without consequences.
Understanding the course of unhealthy alcohol use and predictors of favorable consumption and consequence outcomes may help clinicians to tailor advice and treatment planning, and to develop interventions for medical inpatients. The latter is important given the lack of robust evidence for the efficacy of brief interventions in this setting5,10,11.
Therefore, we studied a prospective cohort of medical inpatients with unhealthy alcohol use to determine the course of alcohol use and consequences, and factors associated with favorable drinking outcomes, 1 year after hospitalization. We hypothesized that factors such as male gender, low socio-economic status, depression, physical or sexual abuse, illegal drug use, presence of alcohol dependence and social pressure to drink would be associated with unfavorable outcome, and factors such as readiness to change and receipt of specialized alcohol treatment (including self-help) would be associated with favorable outcome.
METHODS
Data were collected by interview with medical inpatients at an urban academic hospital who were drinking risky amounts of alcohol [>14 standard drinks (14 g of pure alcohol)/week or ≥5 drinks on an occasion for men, >11 drinks/week or ≥4 drinks on an occasion for women and persons aged over 65 years]. This cohort was prospectively followed for 1 year. Subjects were participants in a randomized trial of a single brief motivational interviewing counseling session (compared with no brief motivational counseling); the intervention had no significant effect on drinking or alcohol consequences6.
Research associates approached all patients aged ≥18 whose physicians did not decline the contact. Individuals fluent in English or Spanish who gave consent were asked to complete a screening interview. Eligibility criteria were: currently drinking risky amounts (as above), two contacts to assist follow-up, no plans to move from the area for the next year and a Mini-Mental State Examination score of ≥21. During the screening interview, subjects completed a 1–10 visual analog scale for readiness to change (“How ready are you to change your drinking habits”). Subjects who refused participation were more likely to be Black (45% vs 31%) and to drink greater amounts of alcohol (median 24 vs 18 drinks per week) compared to eligible subjects who enrolled, but were similar regarding readiness to change measured on a 1–10 visual analog scale.
At study entry we assessed demographics, principal admitting and alcohol-attributable medical diagnoses (by medical record review), alcohol use disorder diagnosis [assessed using the Composite International Diagnostic Interview (CIDI) Alcohol Module]12,13, education, homelessness, heroin use, cocaine use, physical or sexual abuse before the age of 18, and whether or not the subject spent time with heavy or problem drinkers (reflecting social pressure to drink). Not spending time with heavy-drinking friends was assessed with the question “How many of the people you spend time with are heavy or problem drinkers?” and later dichotomized into none vs. any. Baseline measures of health-related quality-of-life (QOL) [Short-Form Health Survey, Physical Component Summary (PCS) score]14, depressive symptoms, and readiness to change alcohol use [problem recognition and commitment to change drinking with the “Perception of Problem” (range 10–50) and “Taking Action” (range 6–30) scales, respectively] were also used. These latter two scales were determined based on a factor analysis of the Stages of Change Readiness Treatment and Eagerness Scale (SOCRATES) in this sample15. The Taking Action scale questions assess both actions to facilitate change that already occurred and commitment to change, with a higher score indicating a higher level of having taken action and commitment to change16. At 12 months, receipt of treatment since study entry was assessed by self-report [hospital detoxification, any treatment for alcohol problems (including counseling or therapy), Alcoholics Anonymous meetings, self-help, mutual help or other 12-step programs for alcohol problems or medication prescribed by a physician to prevent them from drinking]. At study entry and 12 months later, we assessed alcohol consumption with a validated 30-day calendar method (Timeline Followback)17 and alcohol-related consequences with the Short Inventory of Problems (SIP)18. The outcome of interest was favorable drinking at 12 months, defined as abstinence or drinking “moderate” amounts [i.e., less than at-risk amounts, defined above except >7 (not 11) drinks per week was the cutoff for women and the elderly] without consequences. The outcome definition was based on a procedure described and validated by Cisler and Zweben19–21 that classified drinkers according to two factors: whether they drank at-risk amounts and whether they experienced alcohol-related consequences. This composite outcome index was created to capture a broader range of clinically relevant outcomes, knowing that patients with unhealthy alcohol use may choose to keep on drinking but at lower levels and without suffering from alcohol-related consequences.
The following factors were tested: education, marital status, homelessness, physical or sexual abuse before the age of 18, heroin or cocaine use, elevated depressive symptoms, presence of alcohol dependence, readiness to change measure, spending time with heavy-drinking friends and receipt of alcohol treatment after hospitalization (evaluated at the 12-month assessment).
Confounders were defined a priori based on literature and clinical experience, and included: age, gender, race/ethnicity, randomization group, PCS and drinking (drinks per day, past 30 days) at study entry. We included a measure of drinking at study entry as a confounder because alcohol consumption level is known to be one of the strongest predictors of subsequent drinking.
Analyses
We used an iterative model-building procedure to identify factors associated with favorable drinking. Each factor of interest was entered in a separate model adjusted for potential confounders (i.e., in “minimally adjusted models”): age, gender, race/ethnicity, randomization group, physical health-related QOL (PCS score), presence of an alcohol-attributable principal diagnosis at hospital admission and drinks per day at study entry. The potential confounders were selected a priori based on literature and clinical experience.
Prior to regression modeling, we assessed bivariate correlations between all independent variables and covariates. To avoid potential collinearity, no pair of variables with Spearman correlation coefficient >0.40 was included in the same model. Because it was correlated with other factors of interest (drinks per day, past 30 days, r = 0.54; alcohol dependence, r = 0.54; receipt of alcohol treatment, r = 0.44; depressive symptoms, r = 0.44), the Perception of Problem (PP) scale was excluded from further analyses. Since other work suggests that the PP scale and other variables reflecting perception of alcohol problems are markers of severity and since the PP scale was correlated with other better markers of severity, we excluded it from further multivariable analyses. We nevertheless report unadjusted models for PP, since measures of perception of alcohol problem are often used in the literature. No other pairs were correlated >0.40. In an unadjusted logistic regression model, subjects in the highest quartile (highest level) of PP had 2.21 (95% CI: 1.07, 4.56) times the odds of an unfavorable drinking outcome compared to the lowest quartile.
Factors significantly associated with the drinking outcome at an alpha level of 0.05 in these “minimally adjusted models” were included together in a single multivariable model along with confounders. Factors that were no longer significant at an alpha level of 0.05 in the multivariable model were removed one at a time to obtain the final model.
All analyses were adjusted for randomization group (i.e., assignment to brief intervention) at baseline. Analyses were performed using SAS software (version 9.1; SAS Institute, Cary, NC).
RESULTS
Of the 5,813 patients screened, 986 were drinking risky amounts. Of these, 462 were not eligible for entry into the cohort, and 183 were eligible but declined. Of the 341 subjects who were eligible and consented to be in the cohort, 287 (84%) had complete data at 12 months and were included in these analyses. The baseline characteristics of the 287 subjects are presented in Table 1. The five most prevalent principal diagnoses at hospital admission were: rule out myocardial infarction (n = 50), pancreatitis (n = 31), cellulitis (n = 20), asthma (n = 19) and pneumonia (n = 19). Subjects who completed the 12-month follow-up did not differ significantly (alpha level 0.05) from those lost to follow-up with respect to the baseline characteristics presented in Table 1.
Table 1.
Characteristics at Study Entry of 287 Medical Inpatients Identified by Screening with Unhealthy Alcohol Use
| Characteristics | |
|---|---|
| Age, mean (SD) | 44.4 (10.6) |
| Female, n (%) | 86 (30) |
| Currently married, n (%) | 32 (11.2) |
| Education (years), mean (SD) | 11.9 (2.5) |
| Homelessness, n (%) | 73 (25) |
| Race/ethnicity | |
| African-American, n (%) | 133 (46) |
| White, n (%) | 108 (38) |
| Hispanic, n (%) | 24 (8) |
| Other, n (%) | 22 (8) |
| DSM IV Alcohol Diagnosis | |
| Alcohol dependence, n (%) | 223 (78) |
| Alcohol abuse, n (%) | 13 (4) |
| No alcohol use disorder diagnosis, n (%) | 51 (18) |
| Alcohol consumption (drinks per day, past 30 days), mean (SD) | 6.8 (8.9) |
| SOCRATES | |
| Perception of Problem, mean (SD) | 35.5 (11.1) |
| Taking Action, mean (SD) | 21.2 (5.8) |
| Depressive symptoms (CES-D score ≥16), n (%) | 203 (71) |
| Heroin or cocaine use (past 30 days), n (%) | 74 (26) |
| Physical abuse before age 18, n (%) | 116 (41) |
| Sexual abuse before age 18, n (%) | 66 (23) |
| Not spending time with heavy-drinking friends (less social pressure to drink), n (%) | 84 (29) |
| Alcohol-attributable principal diagnosis at hospital admission, n (%) | 42 (15) |
| Receipt of alcohol treatment including self-help | 127 (44.6) |
Homelessness was defined as more than 1 night spent on the streets or in a shelter over the past 3 months
SOCRATES: Stages of Change Readiness Treatment and Eagerness Scale
DSM IV: Diagnostic and Statistical Manual of Mental Disorders, 4th edn
CES-D: Center for Epidemiologic Studies Depression scale
Alcohol-attributable diagnosis includes any of the following: acute alcoholic cirrhosis of the liver, alcoholic cardiomyopathy, alcoholic gastritis, alcoholic hepatits, alcohol intoxication, alcoholic liver damage, alcoholic fatty liver, alcoholic pellagra, alcoholic polyneurpoathy, alcoholic withdrawal, alcoholic withdrawal convulsion, alcoholic withdrawal delirium, alcoholic withdrawal hallucinosis, other alcoholic psychosis, alcoholic amnestic syndrome, other alcoholic dementia, alcoholic pancreatitis or other diagnoses considered alcohol-attributable by the investigator (e.g., holiday heart, alcoholic ketoacidosis, alcohol-related rhabdomyolisis)
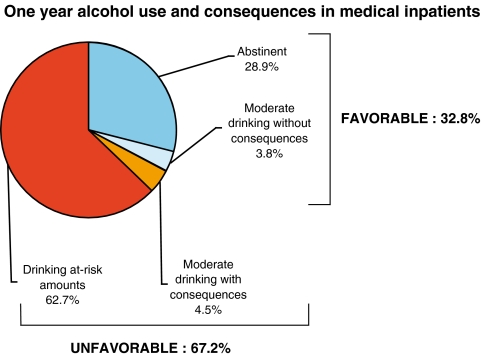
At 12 months, most subjects (63%) were drinking risky amounts, 29% were abstinent, and a few were drinking moderate amounts (with or without consequences) (8%). At 12 months, 33% had a favorable drinking outcome [i.e., they were abstinent (29%) or drinking moderate amounts without consequences (4%)] (Fig. 1).
Figure 1.
Note: Alcohol consumption was assessed with the 30-day Timeline Followback method. Alcohol consequences were assessed with the Short Inventory of Problems (SIP). The SIP is a 15-item questionnaire that assesses, over the past 3 months, the presence of alcohol-related consequences in various dimensions: physical, interpersonal, intrapersonal, impulse control and social responsibility.
Table 2 presents unadjusted logistic regression models for all factors of interest and confounders, and the final model developed from the iterative model building procedure. Elevated depressive symptoms, Taking Action, not spending time with heavy-drinking friends and receipt of alcohol treatment after hospital discharge were associated with a favorable drinking outcome in both unadjusted and “minimally adjusted models.” These four variables were entered simultaneously with the a priori defined potential confounders in an adjusted logistic regression model. The depressive symptom variable was no longer significant in the multivariable model (p = 0.2) and was therefore excluded from the final model. In the final model (Table 2), compared to the first quartile (lowest level) of Taking Action, subjects in the second, third and highest quartile had 3.65 (95% confidence interval, 1.47, 9.02), 3.39 (95% CI 1.38, 8.31) and 6.76 (95% CI 2.74, 16.67) times the odds of a favorable drinking outcome, respectively. Not spending time with heavy-drinking friends [adjusted odds ratio (AOR) 2.14; 95% CI 1.14, 4.00] and receipt of alcohol treatment after hospital discharge during the past year (from baseline to 12-month assessment; AOR 2.16, 95% CI 1.20, 3.87) were associated with a favorable drinking outcome. The Hosmer and Lemeshow chi-square test suggested acceptable model fit of the final logistic regression model (p = 0.73).
Table 2.
Associations with Favorable Drinking Outcome 1 Year After General Medical Hospitalization of 287 Patients with Unhealthy Alcohol Use: Unadjusted and Final Logistic Regression Models
| Unadjusted model | Final model | |||
|---|---|---|---|---|
| OR | 95% CI | AOR | 95% CI | |
| Factors of interest | ||||
| Education (for a 1 year difference) | 1.100 | 0.992, 1.219 | ||
| Currently married | 0.651 | 0.280, 1.511 | ||
| Homelessness | 1.475 | 0.843, 2.582 | ||
| Physical or sexual abuse before age 18 | 0.981 | 0.595, 1.616 | ||
| Heroin or cocaine use | 1.088 | 0.619, 1.914 | ||
| Depressive symptoms (CES-D ≥ 16) | 2.224 | 1.211, 4.081 | ||
| Alcohol dependence | 1.294 | 0.700, 2.392 | ||
| Taking Action (lowest quartile = reference group) | ||||
| 2nd quartile | 3.362 | 1.425, 7.930 | 3.645 | 1.473, 9.017 |
| 3rd quartile | 3.222 | 1.376, 7.542 | 3.386 | 1.380, 8.308 |
| Highest (4th) quartile | 6.443 | 2.760, 15.043 | 6.758 | 2.740, 16.667 |
| Not spending time with heavy-drinking friends | 1.896 | 1.109, 3.241 | 2.137 | 1.142, 4.000 |
| Receipt of alcohol treatment in the past 12 months | 1.959 | 1.183, 3.247 | 2.160 | 1.204, 3.874 |
| Possible confounders | ||||
| Age (for a 1-year difference) | 1.003 | 0.980, 1.027 | 0.992 | 0.964, 1.022 |
| Gender (female) | 1.113 | 0.648, 1.911 | 1.043 | 0.569, 1.912 |
| Race/ethnicity (non-white vs white) | 0.842 | 0.505, 1.406 | 0.676 | 0.375, 1.221 |
| Randomization group (intervention) | 0.977 | 0.593, 1.610 | 0.927 | 0.529, 1.625 |
| PCS | 0.987 | 0.959, 1.015 | 0.975 | 0.944, 1.007 |
| Drinking at baseline (drinks per day) | 1.008 | 0.981, 1.035 | 1.003 | 0.973, 1.035 |
| Alcohol-attributable principal diagnosis at hospital admission | 1.727 | 0.857, 3.479 | 2.153 | 1.005, 4.610 |
OR: odds ratio
AOR: adjusted odds ratio
CI: confidence interval
Taking Action: subscale of the Stages of Change Readiness Treatment and Eagerness Scale
CES-D: Center for Epidemiologic Studies Depression Scale
PCS: Physical component summary
DISCUSSION
We investigated unhealthy alcohol use outcomes and factors associated with a favorable drinking outcome (abstinence or moderate drinking without consequences) at 12 months in opportunistically screened medical inpatients who were not necessarily seeking specialty alcohol treatment. Most continued to drink amounts that risk health consequences and/or have such consequences, but one third had a favorable drinking outcome. Abstinence was the most likely favorable drinking outcome. Few were drinking moderate amounts, with or without consequences.
In 1976, Imber et al. studied the natural history of drinking in male general hospital inpatients with alcohol dependence; 19% were abstinent 1 year later22. More than 30 years later, we found a similar though higher proportion of abstinence. The more favorable course might be due to a sample that consisted not only of subjects with alcohol dependence (though absence of alcohol dependence was not predictive of favorable drinking outcome in our sample). In the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), Dawson et al. showed that among individuals with alcohol dependence, a year later, 17.7% were drinking “low-risk” amounts, and 18.2% were abstainers; approximately half of those with a favorable consumption outcome were still drinking7. Similarly, Sobell et al., in two Canadian general population studies of individuals with alcohol dependence, found that low-risk drinking accounted for 40 and 60% of all cases of recovery7,23. Yet in our study, even though some subjects did not have alcohol dependence, favorable drinking outcome most often consisted of abstinence. Although reasons for the different observations are not clear, the setting and severity of the general hospital sample likely account for them in part.
In primary care, where the prevalence of alcohol dependence is lower, a similar proportion of screen-identified patients was not drinking risky amounts 6 months later24. Similarly, in a study of screening and brief intervention conducted among inpatients with unhealthy alcohol use (without dependence), 46% of the controls did not report any alcohol problems 12 months later. On average, they decreased their daily alcohol consumption by 24 g of alcohol (from 70 g). In most brief intervention studies, a substantial decrease in drinking has been observed in the groups that did not receive any intervention10,25–27. The course of unhealthy alcohol use tends to involve self-change with or without formal help, with a substantial proportion of individuals either abstaining or drinking moderate amounts without consequences a year later. These changes take place for individuals in the general population and for individuals that have contacts with the health care system. These changes may be due to self-change, life events and experiences, notably the accumulation of negative events, as well as assessment effects—all things that happen regardless of interventions.
Few studies have investigated the course and factors associated with outcomes of unhealthy alcohol use in medical inpatients. Although people who enroll in trials differ from those who do not, and although assessment effects can affect outcomes, cohorts of subjects from randomized controlled trials can provide some relevant information. In addition, we identified factors associated with favorable drinking outcome: Taking Action (a measure of actions towards facilitation of change and commitment to change, which can be considered a specific subcategory of readiness to change), not spending time with heavy-drinking friends (which can be seen as a proxy measure for the social pressure to drink) and receipt of alcohol treatment over the past 12 months were positively associated with a favorable drinking outcome. Even though usually considered markers of severity or predictors of poor outcome, and contrary to our hypotheses, a diagnosis of alcohol dependence, drug use, low education level and homelessness were not associated with drinking outcome8,28.
These results suggest the importance of commitment to change and action toward facilitation of change as valuable targets for interventions29. As shown in other studies, individuals who tend to have some intention or commitment to reduce their drinking when seen in a hospital will have a better prognosis30. Self-report of receipt of alcohol treatment between study entry and 12 months later was associated with favorable drinking outcome. This supports the current knowledge on treatment efficacy2,31,32. The observed positive predictive effect of not having heavy-drinking friends on favorable drinking outcome is also consistent with studies indicating the negative impact of the social environment on drinking, notably the impact of social pressure to drink and its negative impact on relapse risk33. Our results add to the evidence that the absence of a heavy-drinking social environment is associated with a better drinking prognosis for individuals with unhealthy alcohol use. Future research may explore relationships between alcohol use behaviors and social networks in order to determine if the same social network effects found in tobacco cessation can be identified for alcohol use34.
The fact that factors usually considered predictors of poor outcome in outpatients (i.e., diagnosis of alcohol dependence, drug use, low education level, homelessness, childhood physical or sexual abuse) were not associated with drinking outcomes in our study is of interest. This may have been due to a lack of power, or alternatively to intrinsic differences in hospitalized patients and ambulatory patients with unhealthy alcohol use. Specifically, our study of hospitalized patients may have examined a more homogeneous and sicker population than usually enrolled in general population studies. Individuals with less severe social and health problems tend to access the health care system less and were therefore less likely to be included in our study. Notably, the present study showed a high prevalence of alcohol dependence among individuals with unhealthy alcohol use (i.e., most patients who screened positive had alcohol dependence). Even though the prevalence of dependence is usually high in screen-positive hospitalized patients, the fact that the study population was recruited at an urban safety net hospital may explain an even higher prevalence. Nevertheless, our findings suggest that these poor prognostic factors should not be seen as insurmountable obstacles when addressing unhealthy alcohol use among medical inpatients.
Study limitations should be considered when interpreting our findings. First, we evaluated the course of unhealthy alcohol use in a sample of subjects that was included in a randomized trial. It is unlikely that the intervention affected our results since we controlled for it in analyses and the trial had negative results. The subjects agreed to participate in a study in which they could receive alcohol counseling. This might have resulted in a selection of individuals more prone to behavior change or more motivated to change; however, it might also have led to selection of patients who were interested in counseling because they thought they could not change without it. Subjects who refused participation were similar to subjects who participated regarding readiness to change completed during the screening interview. Study subjects may also have had courses not representative of natural history due to assessment effects. If this is the case, then the course of unhealthy alcohol use in medical inpatients would be even worse than what we observed. Second, our study was able to identify associations over time but was not designed to study causation. This study is a secondary observational analysis, thus observed associations may not be causal and analyses may be underpowered. The latter may explain why some factors were not significantly associated with drinking outcome, though despite this possibility, other potentially useful and easily assessable clinical factors were associated with outcome. Third we grouped together various treatment modalities and are therefore not able to distinguish between them, though all are known to have efficacy31. The present cohort was followed for 12 months. This could be seen as short with regard to drinking outcomes. Our results should be replicated in cohorts with longer follow-up and with multiple assessment time points. Nevertheless, the literature suggests that 12-month outcomes are indicative of longer term functioning35,36.
This study has notable strengths. We used a large prospective sample identified by screening patients in a general health care setting, with a high follow-up rate. Prospective observational studies are the ideal approach to studying the outcomes and their predictors. Our subjects were well-characterized using validated assessments. We also used a composite outcome of drinking and consequences that has been validated and that has clinical significance20,21.
Our results bring additional information to clinicians treating medical inpatients, a population where unhealthy alcohol use is common. In this setting, one third of the patients will be abstinent a year later. Thus, some optimism regarding the natural history of alcohol use in this population is reasonable. Our results also suggest that homelessness, drug use and depressive symptoms, usually considered markers of severity or predictors of poor outcome, may not have a large negative impact on drinking outcome in medical inpatients. The presence of these markers should not prevent clinicians from addressing unhealthy alcohol use and should not lead them (or their patients) to have a pessimistic view of the drinking prognosis.
The factors identified as being associated with favorable outcome could be useful for clinicians, since they are potentially amenable to change with clinician assistance. Clinicians should therefore be encouraged to target commitment to change in their discussions with patients and help them to take actions towards change. Similarly, linking medical inpatients with unhealthy alcohol use to alcohol treatment and encouraging changes in their social environment to decrease the social pressure to drink may increase the likelihood of a favorable outcome. Since abstinence was the most likely favorable outcome, clinicians should suggest to patients in this setting that abstinence should remain the preferred treatment goal. Clinicians should also keep in mind that factors usually seen as predictive of poor outcomes may not be obstacles among medical inpatients to the degree they may be in other populations of patients with unhealthy alcohol use.
Acknowledgements
Sources of funding Nicolas Bertholet was supported by the Swiss National Science Foundation and Fondation Suisse de Recherche sur l’Alcool. The randomized trial was supported by the National Institute on Alcohol Abuse and Alcoholism (a grant to Boston Medical Center, Dr. Richard Saitz, Principal Investigator, grant R01 AA 12617).
Conflict of interest None disclosed
References
- 1.Rehm J, Room R, Monteiro M, et al. Alcohol as a risk factor for global burden of disease. Eur Addict Res. 2003;9:157–64. doi: 10.1159/000072222. [DOI] [PubMed] [Google Scholar]
- 2.Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005;352:596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- 3.Broadening the base of treatment for alcohol for alcohol problem. Washington, DC: National Academy Press; 1990. [PubMed] [Google Scholar]
- 4.Saitz R, Freedner N, Palfai TP, Horton NJ, Samet JH. The severity of unhealthy alcohol use in hospitalized medical patients. The spectrum is narrow. J Gen Intern Med. 2006;21:381–5. doi: 10.1111/j.1525-1497.2006.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freyer-Adam J, Coder B, Baumeister SE, et al. Brief alcohol intervention for general hospital inpatients: A randomized controlled trial. Drug Alcohol Depend. 2008;93:233–43. doi: 10.1016/j.drugalcdep.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Saitz R, Palfai TP, Cheng DM, et al. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized, controlled trial. Ann Intern Med. 2007;146:167–76. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- 7.Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- 8.Moss HB, Chen CM, Yi HY. Subtypes of alcohol dependence in a nationally representative sample. Drug Alcohol Depend. 2007;Dec 1;91(2–3):149–58 [DOI] [PMC free article] [PubMed]
- 9.Tucker JA, Vuchinich RE, Rippens PD. Different variables are associated with help-seeking patterns and long-term outcomes among problem drinkers. Addict Behav. 2004;29:433–9. doi: 10.1016/j.addbeh.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Daeppen JB, Gaume J, Bady P, et al. Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: a randomized controlled clinical trial. Addiction. 2007;102:1224–33. doi: 10.1111/j.1360-0443.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 11.Emmen MJ, Schippers GM, Bleijenberg G, Wollersheim H. Effectiveness of opportunistic brief interventions for problem drinking in a general hospital setting: systematic review. BMJ. 2004;328:318. doi: 10.1136/bmj.37956.562130.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robins LN, Wing J, Wittchen HU, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45:1069–77. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 13.WHO. Composite International Diagnostic Interview (CIDI)(Core Version 2.0). Geneva, Swtizerland: World Health Organization; 1996.
- 14.Ware JE, Jr, Sherbourne CD. Thirty-six item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Bertholet N, Dukes K, Horton NJ, Palfai TP, Pedley A, Saitz R. Factor structure of the SOCRATES questionnaire in hospitalized medical patients. Addict Behav. 2009;34:568–72. doi: 10.1016/j.addbeh.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bertholet N, Cheng DM, Palfai TP, Samet JH, Saitz R. Does readiness to change predict subsequent alcohol consumption in medical inpatients with unhealthy alcohol use? Addict Behav. 2009;34:636–40. doi: 10.1016/j.addbeh.2009.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sobell LC, Sobell MB. Alcohol Timeline Followback (TLFB) Users’ Manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- 18.Miller WR, Tonigan J, Longabaugh R. The Drinker Inventory of Consequences (DrInC). An Instrument for Assessing Adverse Consequences of Alcohol Abuse. Test Manual. 4 vol. Bethesda: NIH; 1995.
- 19.Zweben A, Cisler R. Composite outcome measures in alcoholism treatment research: problems and potentialities. Subst Use Misuse. 1996;31:1783–805. doi: 10.3109/10826089609064001. [DOI] [PubMed] [Google Scholar]
- 20.Zweben A, Cisler RA. Clinical and methodological utility of a composite outcome measure for alcohol treatment research. Alcohol Clin Exp Res. 2003;27:1680–5. doi: 10.1097/01.ALC.0000091237.34225.D7. [DOI] [PubMed] [Google Scholar]
- 21.Cisler RA, Zweben A. Development of a composite measure for assessing alcohol treatment outcome: operationalization and validation. Alcohol Clin Exp Res. 1999;23:263–71. [PubMed] [Google Scholar]
- 22.Imber S, Schultz E, Funderburk F, Allen R, Flamer R. The fate of the untreated alcoholic. Toward a natural history of the disorder. J Nerv Ment Dis. 1976;162:238–47. doi: 10.1097/00005053-197604000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72. doi: 10.2105/AJPH.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertholet N, Horton NJ, Saitz R. Changes in readiness and drinking in primary care patients with unhealthy alcohol use. Alcoholism Clin Exp Res. 2007;Blackwell. [DOI] [PubMed]
- 25.Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–95. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 26.Kaner EF, Beyer F, Dickinson HO et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007:CD004148. [DOI] [PubMed]
- 27.D'Onofrio G, Pantalon MV, Degutis LC, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann Emerg Med. 2008;51:742–750. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gilman SE, Breslau J, Conron KJ, Koenen KC, Subramanian SV, Zaslavsky AM. Education and race-ethnicity differences in the lifetime risk of alcohol dependence. J Epidemiol Community Health. 2008;62:224–30. doi: 10.1136/jech.2006.059022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71:862–78. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- 30.Daeppen JB, Bertholet N, Gmel G, Gaume J. Communication during brief intervention, intention to change, and outcome. Subst Abus. 2007;28:43–51. doi: 10.1300/J465v28n03_05. [DOI] [PubMed] [Google Scholar]
- 31.Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–77. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 32.Anton RF, O'Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295:2003–17. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- 33.Zywiak WH, Stout RL, Longabaugh R, Dyck I, Connors GJ, Maisto SA. Relapse-onset factors in Project MATCH: the Relapse Questionnaire. J Subst Abuse Treat. 2006;31:341–5. doi: 10.1016/j.jsat.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358:2249–58. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maisto SA, Clifford PR, Stout RL, Davis CM. Drinking in the year after treatment as a predictor of 3-year outcomes. J Stud Alcohol. 2006;67:823–32. doi: 10.15288/jsa.2006.67.823. [DOI] [PubMed] [Google Scholar]
- 36.Maisto SA, Clifford PR, Stout RL, Davis CM. Moderate drinking in the first year after treatment as a predictor of 3-year outcomes. J Stud Alcohol Drugs. 2007;68:419–27. doi: 10.15288/jsad.2007.68.419. [DOI] [PubMed] [Google Scholar]