Abstract
Background
Venous thromboembolism is common after major trauma. Strategies to prevent fatal pulmonary embolism (PE) are widely utilized, but the incidence and risk factors for fatal PE are poorly understood.
Methods
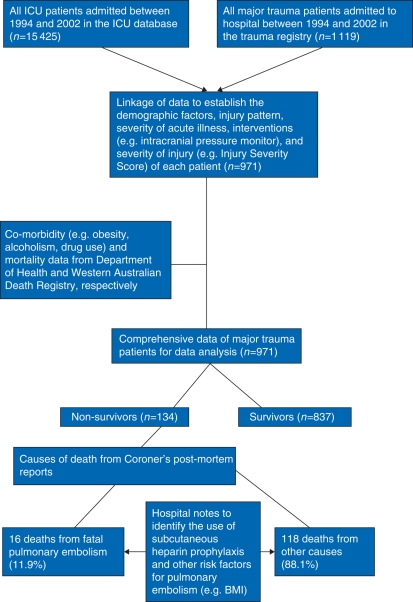
Using linked data from the intensive care unit, trauma registry, Western Australian Death Registry, and post-mortem reports, the incidence and risk factors for fatal PE in a consecutive cohort of major trauma patients, admitted between 1994 and 2002, were assessed. Non-linear relationships between continuous predictors and risk of fatal PE were modelled by logistic regression.
Results
Of the 971 consecutive trauma patients considered in the study, 134 (13.8%) died after their injuries. Fatal PE accounted for 11.9% of all deaths despite unfractionated heparin prophylaxis being used in 44% of these patients. Fatal PE occurred in those who were older (mean age 51- vs 37-yr-old, P=0.01), with more co-morbidities (Charlson's co-morbidity index 1.1 vs 0.2, P=0.01), had a larger BMI (31.8 vs 24.5, P=0.01), and less severe head and systemic injuries when compared with those who died of other causes. Sites of injuries were not significantly related to the risk of fatal PE. Fatal PE occurred much later than deaths from other causes (median 18 vs 2 days, P=0.01), and the estimated attributable mortality of PE was 49% (95% confidence interval 36–62%).
Conclusions
Fatal PE appeared to be a potential preventable cause of late mortality after major trauma. Severity of injuries, co-morbidity, and BMI were important risk factors for fatal PE after major trauma.
Keywords: mortality, prevention, thromboembolism, traumatic injuries
Key points.
Incidence and risk factors for fatal pulmonary embolism (PE) after trauma are poorly understood.
Fatal PE was uncommon but it accounted for a significant proportion of mortality after trauma.
Severity of injuries, co-morbidity and BMI were important risk factors for fatal PE.
More research is needed to assess whether IVC filter is efficacious and cost-effective for patients with these risk factors.
Venous thromboembolism is common after major trauma (>50%) and fatality from pulmonary embolism (PE) approaches 50% in some series.1 The incidence of symptomatic PE after major trauma varies and is very dependent on how the diagnosis is confirmed and probably under-reported in cases of sudden death without an autopsy.2
Evidence suggests that pneumatic lower limb compression devices and low-dose s.c. unfractionated heparin (UFH) prophylaxis are not completely effective in preventing venous thromboembolism.3 Low-molecular-weight heparin (LMWH) is more efficacious than UFH, and although there was no difference in major bleeding in those patients without obvious contraindication, the clinical concern about excessive haemorrhage persists. As such, retrievable inferior vena cava (IVC) filters have been increasingly used in many trauma patients.4,5 The IVC filters are, however, expensive, invasive, and associated with some complications, including erosion of the IVC, inducing thrombosis either above or below the filter, migration of the filter to the right atrium, and tilting or mal-positioning of the filter resulting in ineffective filtering of emboli and fatal PE.6–8 Although IVC filters are now widely used in many trauma patients,9 evidence to support their cost-effectiveness from randomized controlled trials or meta-analyses is sparse.10,11
Fatal PE is an important outcome after major trauma.1 It has been reported to occur at a frequency between 0.4% and 4.2% after major trauma.3,12,13 It is possible that fatal PE occurs more often in patients who have more severe traumatic injuries and some of these patients may die with PE instead of from PE. If most deaths related to PE after major trauma are in fact preventable and the risk factors for this fatal condition can also be identified, selecting high-risk patients for invasive preventive therapy such as IVC filters will be most appropriate. The most appropriate time to insert and remove a retrievable IVC filter in patients after major trauma is also uncertain.14–16
We hypothesized that fatal PE after major trauma is preventable and may be predictable from the characteristics of patients and conducted a nested cohort study to assess its incidence, time of occurrence, and risk factors in a consecutive cohort of major trauma patients who did not receive IVC filters.
Methods
After obtaining approval from the Confidential Health Information Committee and hospital ethics committee, the clinical data of all major trauma patients who were admitted to the Intensive Care Unit of Royal Perth Hospital in Western Australia, between 1994 and 2002, were linked to the trauma registry, death registry, and state hospital morbidity databases. This study period was chosen because IVC filters and routine duplex-Doppler ultrasonography were not used for the trauma patients during the study period. Information on the precise causes of death and on the use of UFH prophylaxis before death were obtained from the Coroner's post-mortem reports and hospital notes, respectively. Royal Perth Hospital is a tertiary hospital in Western Australia and is the state's designated trauma centre. In this study centre, all deaths related to major trauma were referred to the Coroner's office for post-mortem examination to determine the cause(s) of death.
Statistical analysis
The data analysed included patients' age, sex, severity of injury as measured by Acute Physiology and Chronic Health Evaluation [APACHE],17 Injury Severity Score, and details of the severity of head injuries including computed tomographic (CT) findings of the brain,18 Charlson's co-morbidity index,19 interventions such as intracranial pressure monitor, pattern of injuries, the use of s.c. UFH prophylaxis, and BMI.
Categorical variables were analysed by χ2 test, and continuous variables with a near normal distribution and variables with skewed distributions [standard deviation (sd) >50% mean] were analysed by t-test and the Mann–Whitney test, respectively. Multivariate logistic regression was used to assess the associations between multiple predictors and risk of fatal PE. The predicted risk of death of each patient in this cohort was estimated by a combination of the APACHE II-predicted mortality, Injury Severity Score, and details of the severity of head injuries such as pupillary response to light, motor response, and CT findings of the brain.18
Attributable mortality of PE was estimated by the difference in the predicted risk of death between those who died from PE and other causes. We used a four-knot restricted cubic spline function, a technique very similar to polynomial function, to allow non-linearity of continuous predictors in the multivariate analysis.20 All statistical tests were performed by SPSS (version 13.0, IL, USA) and S-Plus (version 8.0, Insightful Corp., Seattle, WA, USA) and P-value <0.05 was regarded as significant.
Results
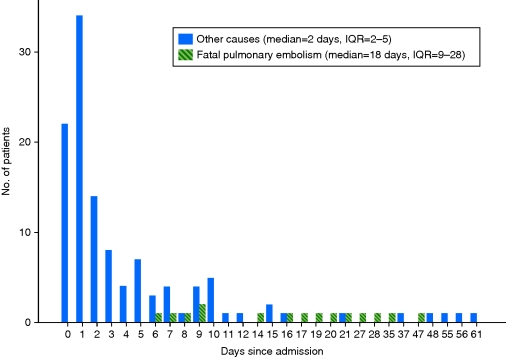
Of the 971 consecutive major trauma patients included in the study, 134 patients (13.8%) died during their hospital stay after the injury. Fatal PE accounted for a total of 16 deaths [11.9%, 95% confidence interval (CI) 8–19%] despite s.c. UFH being used in 44% of these patients. LMWH was not used in this cohort of patients. One other patient also had a small subsegmental PE in the post-mortem examination, but the PE was judged not to be the cause of death by the Coroner. Most patients with fatal PE were treated as having deteriorating sepsis, without considering PE as a diagnosis, before they died. The incidence of fatal PE in the whole cohort was about 1.6% (95% CI 1.0–2.7%; Fig. 1). The median time of fatal PE after the injury was 18 days [mean 39, inter-quartile range (IQR) 9–28] which was much later than other causes of death (median 2, mean 7, IQR 2–5; Fig. 2). The other main causes of death were severe traumatic brain injury, uncontrolled haemorrhage from multiple injuries, and infection leading to multiple organ failure.
Fig 1.
Linkage of different data sources to obtain comprehensive information on the study trauma patients.
Fig 2.
The timing of fatal pulmonary embolism and other causes of death after major trauma. IQR, inter-quartile range.
More than 50% of the patients who died from fatal PE had chest and head injuries (Table 1). When compared with patients who died from other causes, the patients who died from fatal PE were older, with more co-morbidities especially chronic obstructive pulmonary disease and liver disease, had a higher BMI (mean 31.8 vs 24.5), and less severe head and systemic injuries (Table 1). The predicted mortality rates of the patients who had fatal PE were much lower than the patients who died from other causes (18% vs 67%), suggesting that a significant number of deaths due to fatal PE were preventable. The attributable mortality of PE, estimated by the difference in the predicted mortality rates of the patients who died from fatal PE and other causes, was 49% (95% CI 36–62%).
Table 1.
Characteristics of deaths due to fatal PE and other causes. APACHE, Acute Physiology and Chronic Health Evaluation; COPD, chronic obstructive pulmonary disease; sd, standard deviation; IQR, inter-quartile range; ICP, intracranial pressure; ISS, Injury Severity Score. #P-values generated by the Mann–Whitney test
| Variable | Fatal PE (n=16) | Other causes (n=118) | P-value |
|---|---|---|---|
| Age (yr) (range) | 51.3 (21–92) | 36.7 (13–90) | 0.018 |
| Male [no. (%)] | 12 (75) | 85 (72) | 1.000 |
| Head injuries [no. (%)] | 9 (56.3) | 116 (89.8) | 0.002 |
| ICP monitor [no. (%)] | 6 (37.5) | 91 (77.1) | 0.002 |
| Chest injuries [no. (%)] | 10 (62.5) | 74 (62.7) | 1.000 |
| Lower limb long-bone fractures [no. (%)] | 3 (18.8) | 28 (23.7) | 1.000 |
| Spinal fractures [no. (%)] | 5 (31.3) | 28 (23.7) | 0.541 |
| Abdominal injuries [no. (%)] | 3 (18.8) | 27 (22.9) | 1.000 |
| Pelvic fractures [no. (%)] | 3 (18.8) | 24 (20.3) | 1.000 |
| BMI (sd) (median, IQR) | 31.8 (4.0) (31.2, 29–35) | 24.5 (4.1) (24.0, 21–26) | 0.001 |
| ISS (sd) | 27.8 (9.4) | 38.2 (11.9) | 0.001 |
| Prophylactic heparin [no. (%)] | 7 (43.8) | 12 (0.9) | 0.001 |
| Charlson's index (sd) (median, IQR) | 1.1 (2.2) (0, 0–2) | 0.2 (0.6) (0, 0–0) | 0.003# |
| Past medical conditions [no. (%)] | |||
| COPD | 3 (19) | 1 (1) | 0.005 |
| Cerebrovascular disease | 2 (13) | 3 (3) | 0.108 |
| Hypertension | 0 (0) | 1 (1) | 1.000 |
| Congestive heart failure | 0 (0) | 2 (2) | 1.000 |
| Any tumour | 1 (6) | 0 (0) | 0.119 |
| Liver disease | 2 (13) | 1 (1) | 0.038 |
| Alcoholism | 1 (6) | 4 (3) | 0.476 |
| Drug use | 0 (0) | 3 (3) | 1.000 |
| Diabetes mellitus | 0 (0) | 3 (3) | 1.000 |
| Renal disease | 1 (6) | 0 (0) | 0.119 |
| Depression | 1 (6) | 2 (2) | 0.319 |
| APACHE II-predicted mortality [% (sd)] (median, IQR) | 15.4 (13.4) (14, 4–19) | 32.0 (16.8) (28, 20–45) | 0.001# |
| Head injury prediction model mortality risk [% (sd)] (median, IQR) | 23.4 (16.1) (22, 7–35) | 51.4 (23.2) (56, 38–70) | 0.001# |
| Predicted mortality by combining ISS, APACHE II risk, and head injury prediction model risk [% (sd)] (median, IQR) | 17.8 (22.9) (8, 4–22) | 66.6 (32.3) (79, 43–94) | 0.001# |
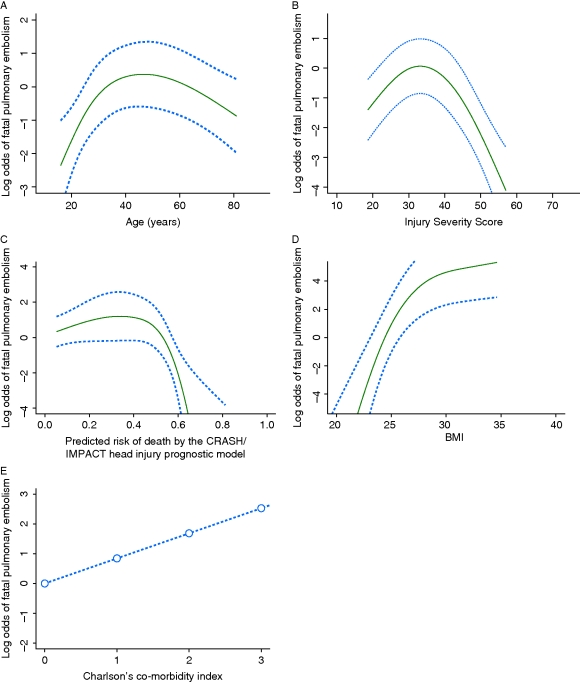
Age, Injury Severity Score, and severity of head injury showed a triphasic relationship with the risk of fatal PE (Fig. 3a–c), and this was different from the relatively linear relationship between the risk of fatal PE and BMI (Fig. 3d) or co-morbidity (Fig. 3e).
Fig 3.
Relationship between risk of fatal pulmonary embolism and (a) age, (b) Injury Severity Score, (c) severity of head injury, (d) BMI, and (e) Charlson's co-morbidity index after adjusting for other covariates (dotted lines signify CI).
Discussion
Our results showed that fatal PE was relatively uncommon after major trauma (1.6%), but it accounted for about 11.9% of all deaths. We estimated that about 50% of the deaths from fatal PE were preventable. Severity of injuries, co-morbidities, and BMI were important risk factors for fatal PE.
The incidence of fatal PE in our cohort was comparable with other reports.3,12,13 Although fatal PE was relatively uncommon, it accounted for a significant proportion of deaths (11.9%). Our results showed that many patients who died from fatal PE did not have very severe injuries; the predicted risks of mortality were much lower than those who died from other causes (Table 1). The estimated attributable mortality of PE suggested that about half of the deaths from fatal PE were potentially preventable. UFH prophylaxis, although only used in less than half of the patients with fatal PE, was not very effective in preventing fatal PE in our cohort, a finding similar to some other reports.3 The American College of Chest Physicians has recently strongly recommended LMWH prophylaxis (Grade 1A) for venous thromboembolism prophylaxis after major trauma. Our data support this recommendation because UFH was not very effective in preventing fatal PE and the medium time to fatal PE after the injury (18 days) was long after the injury when LMWH may be safely commenced.
Because the absolute incidence of fatal PE was relatively low among all trauma patients (1.6%) and the attributable mortality of PE was about 50%, the crude mortality of the whole cohort would only reduce slightly from 13.8% to 13.0% even if all PE were prevented by IVC filters. These results suggested that the estimated number of IVC filters needed to prevent one fatal PE was relatively large (mean 125, 95% CI 100–167). Even if IVC filters were used only for patients who survived the first 3 days after the injury (n=900), the number needed to prevent one fatal PE was still large (mean 113, 95% CI 90–154). The non-linear relationship between the severity of injuries and fatal PE suggested that a very selective approach to use IVC filters to prevent fatal PE after major trauma was needed. When the severity of injuries was either very mild or extreme, patients were more likely to survive without fatal PE or die directly from the injuries, respectively (Fig. 3b and c). Therefore, an expensive and invasive preventive therapy such as IVC filter is likely to be most cost-effective if it is used for those with severe injuries that are compatible with survival (e.g. Injury Severity Score between 20 and 45) or practically those who survive the first few days after their severe injuries but have ongoing contraindications to initiation of LMWH. In patients with severe head injury who have contraindications to LMWH but are likely to survive with a favourable neurological outcome (e.g. predicted risk <70%),21 an early placement of an IVC filter may be the most effective measure to prevent fatal PE.
Our results showed that BMI and Charlson's co-morbidity index were important risk factors for fatal PE after major trauma. These findings were consistent with the literature on PE in patients without trauma. Various abnormalities of haemostasis have been reported in obesity, including increased platelet aggregability, circulating mircoparticles, and reduced fibrinolysis, resulting in increased risk of venous thromboembolism.22 Co-morbidity may increase the risk of fatal PE by either an increased risk of venous thromboembolism (e.g. chronic obstructive airway disease)23–25 or a reduced haemodynamic tolerance to a submassive PE (e.g. heart failure).25 Trauma patients with co-morbidities and an increased BMI may benefit most from early initiation of LMWH or placement of an IVC filter if they have contraindications to LMWH.
This study has some limitations. Firstly, fatal PE was relatively uncommon in our cohort of patients and hence the results were imprecise. Secondly, this was a single-centre study and our results may not be applicable to other centres. Because fatal PE is relatively rare after major trauma, a multicentre study will significantly increase the power of the study and external validity. A prospective multicentre observational study will, however, need a significant amount of funding to allow collection of comprehensive data from a large number of trauma patients, and mandatory post-mortem examinations for all deaths after major trauma may not be feasible at all study centres. Thirdly, because of the retrospective nature of the study, we could not ascertain the use of pneumatic compression devices in our patients and this may have confounded our results.26 Finally, our study period was relatively long; medical practice such as the early use of CT pulmonary angiography or early mobilization after damage control surgery might have changed the pattern of fatal PE during the study period.
In spite of these limitations, this study has some strengths when compared with previous studies on PE after major trauma. Firstly, we used autopsy-proven PE as a study endpoint instead of clinical diagnosis which tends to underestimate the true incidence of fatal PE.9,13 Even in a recent report on PE after major trauma, an autopsy was used to confirm fatal PE in only 23% of the deaths.16 Secondly, we have included a comprehensive assessment of risk factors for fatal PE. Some of these risk factors for fatal PE, such as BMI and co-morbidity, have not been thoroughly assessed in patients after major trauma.9 Finally, we have modelled the non-linear relationships between these risk factors and fatal PE; these results may be useful for clinicians to choose appropriate patients for an IVC filter or design a randomized controlled study to assess the cost-effectiveness of IVC filters. In the most recent audit of our trauma patients in 2007 and 2008, LMWH prophylaxis was still not used, but 40 IVC filters (7.4%), 18 CT pulmonary angiography (3.4%), and 11 duplex-Doppler ultrasonography (2%) were used for a total of 538 trauma patients. Of these 538 trauma patients, a total of eight patients had CT pulmonary angiography-confirmed PE (1.5%), another seven patients had duplex-Doppler-confirmed deep vein thrombosis (1.3%), and one patient, with a BMI of 40, died from fatal PE (0.2%). These recent data together with the results of the present study suggest that a combination of early diagnosis and the selective use of IVC filters may be useful in reducing the incidence of fatal PE.
In summary, fatal PE appeared to be a potential preventable cause of late mortality after major trauma. Severity of injuries, co-morbidity, and BMI were important risk factors for fatal PE. More research is needed to assess whether the selective use of IVC filter is efficacious and cost-effective for patients with these risk factors and contraindications to LMWH prophylaxis.
Conflict of interest
None declared.
Funding
We would like to thank BUPA and Medical Research Foundation of Royal Perth Hospital in funding the data linkage process involved in this study. No funding was received from National Institutes of Health, Wellcome Trust, and Howard Hughes Medical Institute.
References
- 1.Rogers FB, Cipolle MD, Velmahos G, et al. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002;53:142–64. doi: 10.1097/00005373-200207000-00032. doi:10.1097/00005373-200207000-00032. [DOI] [PubMed] [Google Scholar]
- 2.Rogers FB, Shackford SR, Ricci MA, et al. Prophylactic vena cava filter insertion in selected high-risk orthopaedic trauma patients. J Orthop Trauma. 1997;11:267–72. doi: 10.1097/00005131-199705000-00006. doi:10.1097/00005131-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Rosenthal D, McKinsey JF, Levy AM, et al. Use of the Greenfield filter in patients with major trauma. Cardiovasc Surg. 1994;2:52–5. [PubMed] [Google Scholar]
- 4.Shackford SR, Cook A, Rogers FB, et al. The increasing use of vena cava filters in adult trauma victims: data from the American College of Surgeons National Trauma Data Bank. J Trauma. 2007;63:764–9. doi: 10.1097/01.ta.0000240444.14664.5f. doi:10.1097/01.ta.0000240444.14664.5f. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman JA, Kinney TB, Streiff MB, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. Surg Obes Relat Dis. 2006;2:200–12. doi: 10.1016/j.soard.2006.03.009. doi:10.1016/j.soard.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Sing RF, Rogers FB, Novitsky YW, et al. Optional vena cava filters for patients with high thromboembolic risk: questions to be answered. Surg Innov. 2005;12:195–202. doi: 10.1177/155335060501200303. doi:10.1177/155335060501200303. [DOI] [PubMed] [Google Scholar]
- 7.Rogers FB, Strindberg G, Shackford SR, et al. Five-year follow-up of prophylactic vena cava filters in high-risk trauma patients. Arch Surg. 1998;133:406–11. doi: 10.1001/archsurg.133.4.406. [DOI] [PubMed] [Google Scholar]
- 8.Stawicki SP, Sims CA, Sharma R, et al. Vena cava filters: a synopsis of complications and related topics. J Vasc Access. 2008;9:102–10. [PubMed] [Google Scholar]
- 9.Knudson MM, Ikossi DG, Khaw L, et al. Thromboembolism after trauma: an analysis of 1602 episodes from the American College of Surgeons National Trauma Data Bank. Ann Surg. 2004;240:490–6. doi: 10.1097/01.sla.0000137138.40116.6c. discussion 496–8. doi:10.1097/01.sla.0000137138.40116.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cherry RA, Nichols PA, Snavely TM, et al. Prophylactic inferior vena cava filters: do they make a difference in trauma patients? J Trauma. 2008;65:544–8. doi: 10.1097/TA.0b013e31817f980f. doi:10.1097/TA.0b013e31817f980f. [DOI] [PubMed] [Google Scholar]
- 11.Young T, Tang H, Aukes J, et al. Vena caval filters for the prevention of pulmonary embolism. Cochrane Database Syst Rev. 2007:CD006212. doi: 10.1002/14651858.CD006212.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Knudson MM, Lewis FR, Clinton A, et al. Prevention of venous thromboembolism in trauma patients. J Trauma. 1994;37:480–7. doi: 10.1097/00005373-199409000-00025. doi:10.1097/00005373-199409000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Khansarinia S, Dennis JW, Veldenz HC, et al. Prophylactic Greenfield filter placement in selected high-risk trauma patients. J Vasc Surg. 1995;22:231–5. doi: 10.1016/s0741-5214(95)70135-4. discussion 23523–6 doi:10.1016/S0741-5214(95)70135-4. [DOI] [PubMed] [Google Scholar]
- 14.Hope WW, Demeter BL, Newcomb WL, et al. Postoperative pulmonary embolism: timing, diagnosis, treatment, and outcomes. Am J Surg. 2007;194:814–8. doi: 10.1016/j.amjsurg.2007.08.014. doi:10.1016/j.amjsurg.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Stefanidis D, Paton BL, Jacobs DG, et al. Extended interval for retrieval of vena cava filters is safe and may maximize protection against pulmonary embolism. Am J Surg. 2006;192:789–94. doi: 10.1016/j.amjsurg.2006.08.046. doi:10.1016/j.amjsurg.2006.08.046. [DOI] [PubMed] [Google Scholar]
- 16.Sing RF, Camp SM, Heniford BT, et al. Timing of pulmonary emboli after trauma: implications for retrievable vena cava filters. J Trauma. 2006;60:732–4. doi: 10.1097/01.ta.0000210285.22571.66. discussion 734–5. doi:10.1097/01.ta.0000210285.22571.66. [DOI] [PubMed] [Google Scholar]
- 17.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. doi:10.1097/00003246-198510000-00009. [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. doi:10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165. doi: 10.1371/journal.pmed.0050165. doi:10.1371/journal.pmed.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Regression Modeling Strategies. New York: Springer; 2001. Harrell FE Jr. [Google Scholar]
- 21.Honeybul S, Ho KM, Lind CR, et al. The retrospective application of a prediction model to patients who have had a decompressive craniectomy for trauma. J Neurotrauma. 2009;26:2179–83. doi: 10.1089/neu.2009.0989. doi:10.1089/neu.2009.0989. [DOI] [PubMed] [Google Scholar]
- 22.Stein PD, Goldman J. Obesity and thromboembolic disease. Clin Chest Med. 2009;30:489–93. doi: 10.1016/j.ccm.2009.05.006. doi:10.1016/j.ccm.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Rizkallah J, Man SF, Sin DD. Prevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2009;135:786–93. doi: 10.1378/chest.08-1516. doi:10.1378/chest.08-1516. [DOI] [PubMed] [Google Scholar]
- 24.Ortel TL. Acquired thrombotic risk factors in the critical care setting. Crit Care Med. 2010;38:S43–S50. doi: 10.1097/CCM.0b013e3181c9ccc8. [DOI] [PubMed] [Google Scholar]
- 25.Laporte S, Mismetti P. Epidemiology of thrombotic risk factors: the difficulty in using clinical trials to develop a risk assessment model. Crit Care Med. 2010;38:S10–S17. doi: 10.1097/CCM.0b013e3181c9cc3b. [DOI] [PubMed] [Google Scholar]
- 26.Eppsteiner RW, Shin JJ, Johnson J, et al. Mechanical compression versus subcutaneous heparin therapy in postoperative and posttrauma patients: a systematic review and meta-analysis. World J Surg. 2010;34:10–9. doi: 10.1007/s00268-009-0284-z. doi:10.1007/s00268-009-0284-z. [DOI] [PubMed] [Google Scholar]