Abstract
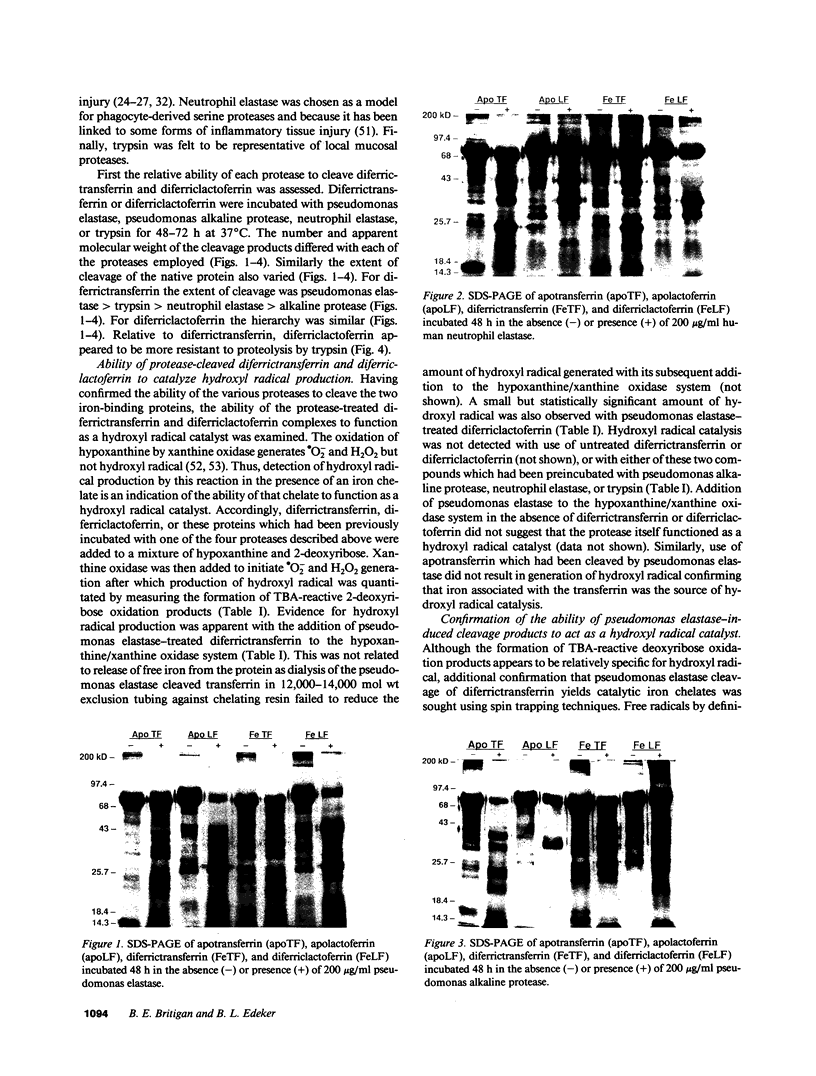
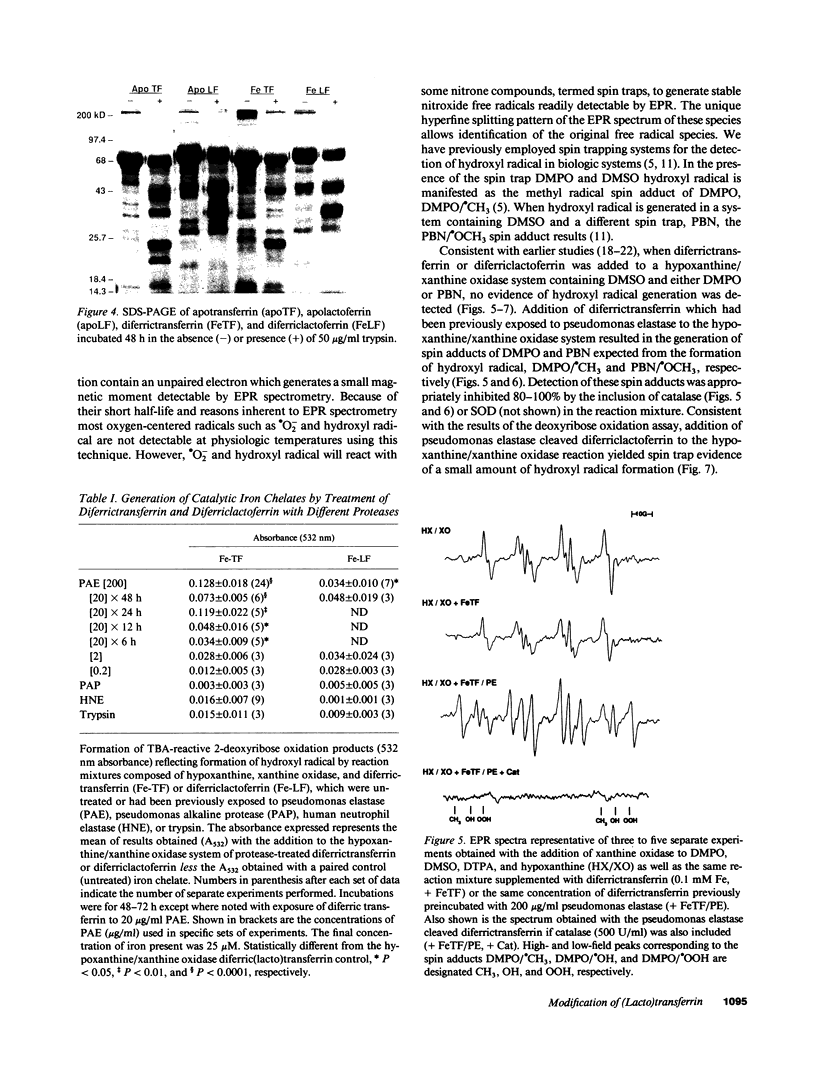
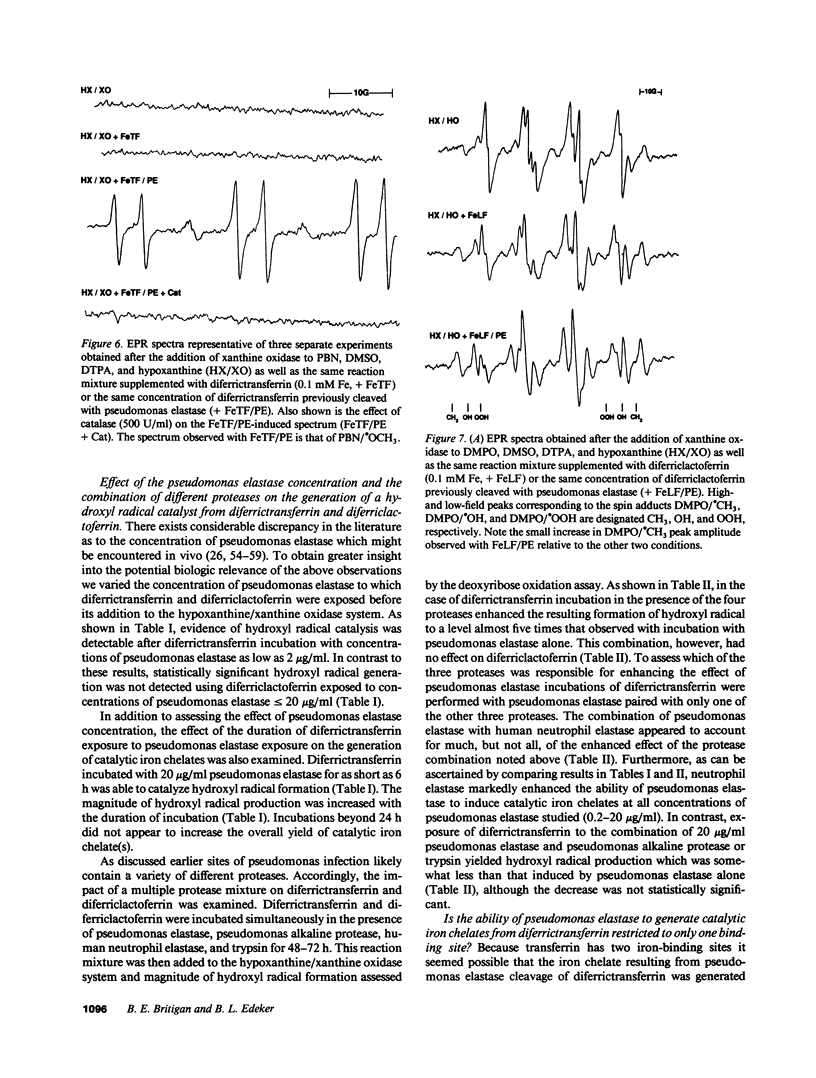
In vivo most extracellular iron is bound to transferrin or lactoferrin in such a way as to be unable to catalyze the formation of hydroxyl radical from superoxide (.O2-) and hydrogen peroxide (H2O2). At sites of Pseudomonas aeruginosa infection bacterial and neutrophil products could possibly modify transferrin and/or lactoferrin forming catalytic iron complexes. To examine this possibility, diferrictransferrin and diferriclactoferrin which had been incubated with pseudomonas elastase, pseudomonas alkaline protease, human neutrophil elastase, trypsin, or the myeloperoxidase product HOCl were added to a hypoxanthine/xanthine oxidase .O2-/H2O2 generating system. Hydroxyl radical formation was only detected with pseudomonas elastase treated diferrictransferrin and, to a much lesser extent, diferriclactoferrin. This effect was enhanced by the combination of pseudomonas elastase with other proteases, most prominently neutrophil elastase. Addition of pseudomonas elastase-treated diferrictransferrin to stimulated neutrophils also resulted in hydroxyl radical generation. Incubation of pseudomonas elastase with transferrin which had been selectively iron loaded at either the NH2- or COOH-terminal binding site yielded iron chelates with similar efficacy for hydroxyl radical catalysis. Pseudomonas elastase and HOCl treatment also decreased the ability of apotransferrin to inhibit hydroxyl radical formation by a Fe-NTA supplemented hypoxanthine/xanthine oxidase system. However, apotransferrin could be protected from the effects of HOCl if bicarbonate anion was present during the incubation. Apolactoferrin inhibition of hydroxyl radical generation was unaffected by any of the four proteases or HOCl. Alteration of transferrin by enzymes and oxidants present at sites of pseudomonas and other bacterial infections may increase the potential for local hydroxyl radical generation thereby contributing to tissue injury.
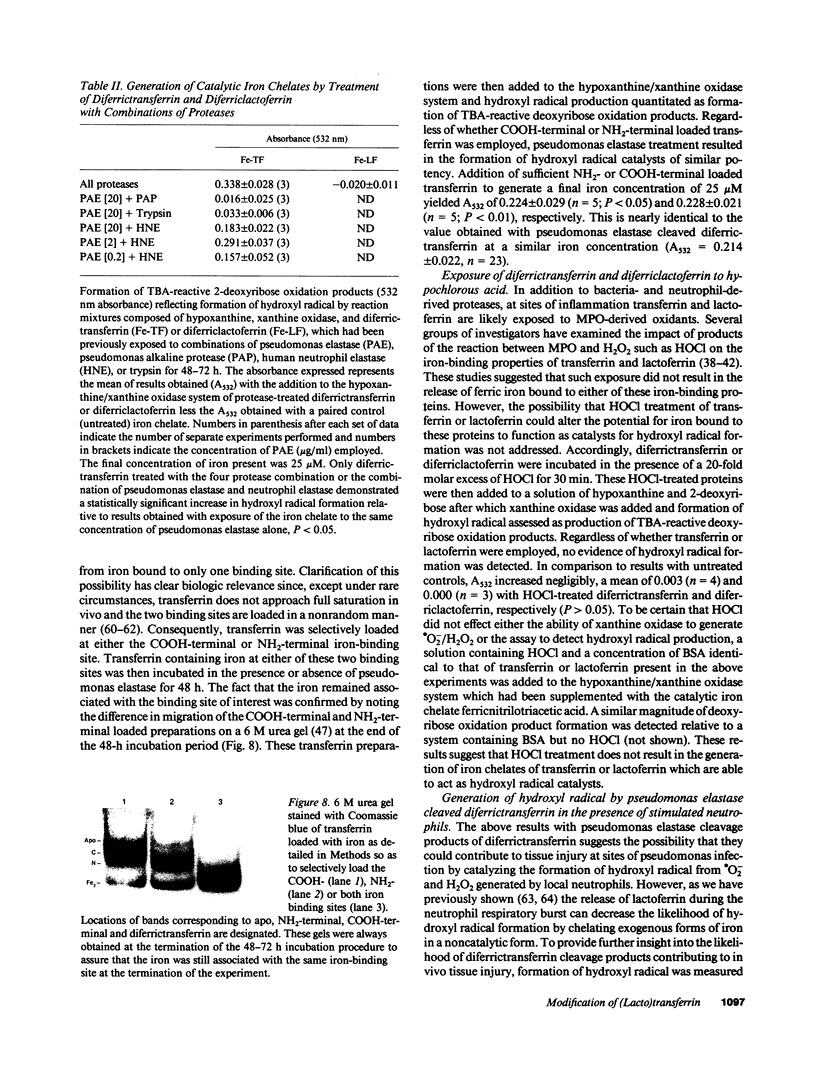
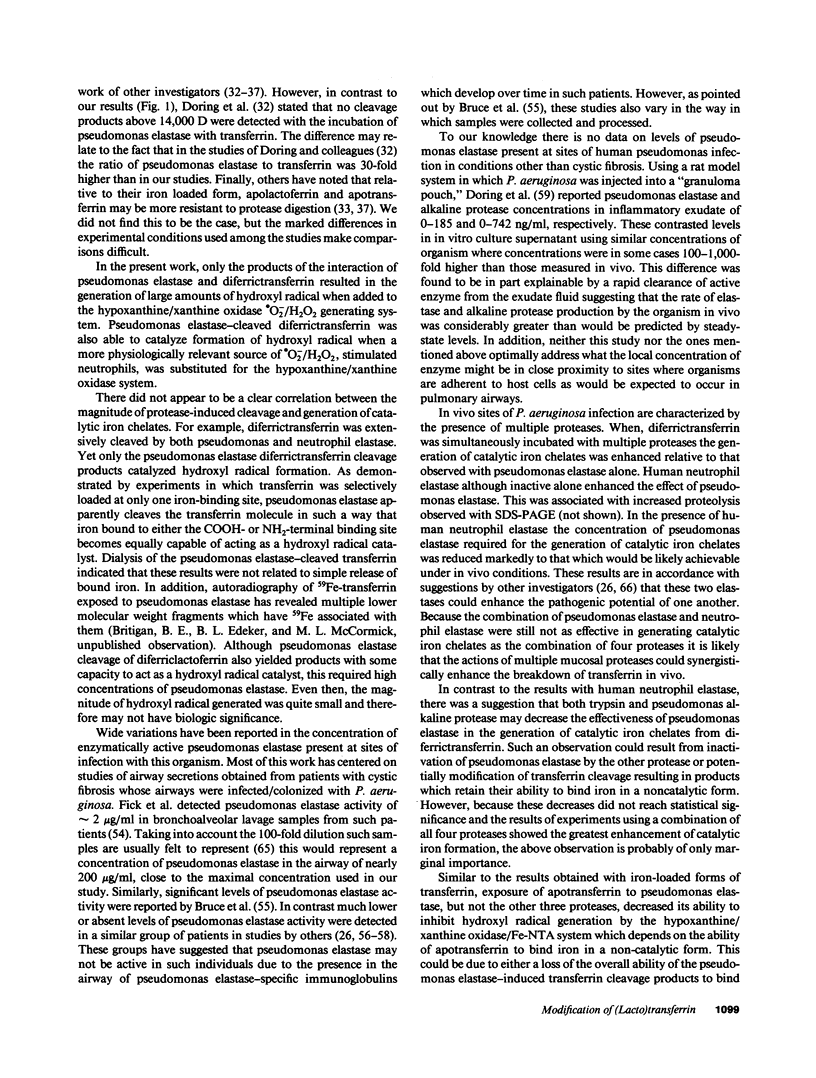
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ambruso D. R., Johnston R. B., Jr Lactoferrin enhances hydroxyl radical production by human neutrophils, neutrophil particulate fractions, and an enzymatic generating system. J Clin Invest. 1981 Feb;67(2):352–360. doi: 10.1172/JCI110042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aruoma O. I., Halliwell B. Superoxide-dependent and ascorbate-dependent formation of hydroxyl radicals from hydrogen peroxide in the presence of iron. Are lactoferrin and transferrin promoters of hydroxyl-radical generation? Biochem J. 1987 Jan 1;241(1):273–278. doi: 10.1042/bj2410273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin D. A., Jenny E. R., Aisen P. The effect of human serum transferrin and milk lactoferrin on hydroxyl radical formation from superoxide and hydrogen peroxide. J Biol Chem. 1984 Nov 10;259(21):13391–13394. [PubMed] [Google Scholar]
- Baldwin D. A., de Sousa D. M. The effect of salts on the kinetics of iron release from N-terminal and C terminal monoferrictransferrins. Biochem Biophys Res Commun. 1981 Apr 30;99(4):1101–1107. doi: 10.1016/0006-291x(81)90732-4. [DOI] [PubMed] [Google Scholar]
- Bannister J. V., Bannister W. H., Hill H. A., Thornalley P. J. Enhanced production of hydroxyl radicals by the xanthine-xanthine oxidase reaction in the presence of lactoferrin. Biochim Biophys Acta. 1982 Mar 15;715(1):116–120. doi: 10.1016/0304-4165(82)90056-3. [DOI] [PubMed] [Google Scholar]
- Bates G. W., Billups C., Saltman P. The kinetics and mechanism of iron (3) exchange between chelates and transferrin. I. The complexes of citrate and nitrilotriacetic acid. J Biol Chem. 1967 Jun 25;242(12):2810–2815. [PubMed] [Google Scholar]
- Bluard-Deconinck J. M., Williams J., Evans R. W., van Snick J., Osinski P. A., Masson P. L. Iron-binding fragments from the N-terminal and C-terminal regions of human lactoferrin. Biochem J. 1978 May 1;171(2):321–327. doi: 10.1042/bj1710321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brines R. D., Brock J. H. The effect of trypsin and chymotrypsin on the in vitro antimicrobial and iron-binding properties of lactoferrin in human milk and bovine colostrum. Unusual resistance of human apolactoferrin to proteolytic digestion. Biochim Biophys Acta. 1983 Sep 13;759(3):229–235. doi: 10.1016/0304-4165(83)90317-3. [DOI] [PubMed] [Google Scholar]
- Britigan B. E., Coffman T. J., Buettner G. R. Spin trapping evidence for the lack of significant hydroxyl radical production during the respiration burst of human phagocytes using a spin adduct resistant to superoxide-mediated destruction. J Biol Chem. 1990 Feb 15;265(5):2650–2656. [PubMed] [Google Scholar]
- Britigan B. E., Hassett D. J., Rosen G. M., Hamill D. R., Cohen M. S. Neutrophil degranulation inhibits potential hydroxyl-radical formation. Relative impact of myeloperoxidase and lactoferrin release on hydroxyl-radical production by iron-supplemented neutrophils assessed by spin-trapping techniques. Biochem J. 1989 Dec 1;264(2):447–455. doi: 10.1042/bj2640447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britigan B. E., Pou S., Rosen G. M., Lilleg D. M., Buettner G. R. Hydroxyl radical is not a product of the reaction of xanthine oxidase and xanthine. The confounding problem of adventitious iron bound to xanthine oxidase. J Biol Chem. 1990 Oct 15;265(29):17533–17538. [PubMed] [Google Scholar]
- Britigan B. E., Rosen G. M., Chai Y., Cohen M. S. Do human neutrophils make hydroxyl radical? Determination of free radicals generated by human neutrophils activated with a soluble or particulate stimulus using electron paramagnetic resonance spectrometry. J Biol Chem. 1986 Apr 5;261(10):4426–4431. [PubMed] [Google Scholar]
- Britigan B. E., Rosen G. M., Thompson B. Y., Chai Y., Cohen M. S. Stimulated human neutrophils limit iron-catalyzed hydroxyl radical formation as detected by spin-trapping techniques. J Biol Chem. 1986 Dec 25;261(36):17026–17032. [PubMed] [Google Scholar]
- Bruce M. C., Poncz L., Klinger J. D., Stern R. C., Tomashefski J. F., Jr, Dearborn D. G. Biochemical and pathologic evidence for proteolytic destruction of lung connective tissue in cystic fibrosis. Am Rev Respir Dis. 1985 Sep;132(3):529–535. doi: 10.1164/arrd.1985.132.3.529. [DOI] [PubMed] [Google Scholar]
- Buettner G. R. The reaction of superoxide, formate radical, and hydrated electron with transferrin and its model compound, Fe(III)-ethylenediamine-N,N'-bis[2-(2-hydroxyphenyl)acetic acid] as studied by pulse radiolysis. J Biol Chem. 1987 Sep 5;262(25):11995–11998. [PubMed] [Google Scholar]
- Bullen J. J., Rogers H. J., Griffiths E. Role of iron in bacterial infection. Curr Top Microbiol Immunol. 1978;80:1–35. doi: 10.1007/978-3-642-66956-9_1. [DOI] [PubMed] [Google Scholar]
- Clark R. A., Pearson D. W. Inactivation of transferrin iron binding capacity by the neutrophil myeloperoxidase system. J Biol Chem. 1989 Jun 5;264(16):9420–9427. [PubMed] [Google Scholar]
- Coffman T. J., Cox C. D., Edeker B. L., Britigan B. E. Possible role of bacterial siderophores in inflammation. Iron bound to the Pseudomonas siderophore pyochelin can function as a hydroxyl radical catalyst. J Clin Invest. 1990 Oct;86(4):1030–1037. doi: 10.1172/JCI114805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diguiseppi J., Fridovich I. Ethylene from 2-keto-4-thiomethyl butyric acid: the Haber-Weiss reaction. Arch Biochem Biophys. 1980 Dec;205(2):323–329. doi: 10.1016/0003-9861(80)90114-9. [DOI] [PubMed] [Google Scholar]
- Dunn M. M., Dunne M., Kamp D. W. Polymorphonuclear leukocyte- and Pseudomonas aeruginosa-induced damage to a human pulmonary epithelial cell line. J Infect Dis. 1990 Jul;162(1):172–177. doi: 10.1093/infdis/162.1.172. [DOI] [PubMed] [Google Scholar]
- Döring G., Dalhoff A., Vogel O., Brunner H., Dröge U., Botzenhart K. In vivo activity of proteases of Pseudomonas aeruginosa in a rat model. J Infect Dis. 1984 Apr;149(4):532–537. doi: 10.1093/infdis/149.4.532. [DOI] [PubMed] [Google Scholar]
- Döring G., Pfestorf M., Botzenhart K., Abdallah M. A. Impact of proteases on iron uptake of Pseudomonas aeruginosa pyoverdin from transferrin and lactoferrin. Infect Immun. 1988 Jan;56(1):291–293. doi: 10.1128/iai.56.1.291-293.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esparza I., Brock J. H. The effect of trypsin digestion on the structure and iron-donating properties of transferrins from several species. Biochim Biophys Acta. 1980 Apr 25;622(2):297–307. doi: 10.1016/0005-2795(80)90040-9. [DOI] [PubMed] [Google Scholar]
- Evans R. W., Williams J. Studies of the binding of different iron donors to human serum transferrin and isolation of iron-binding fragments from the N- and C-terminal regions of the protein. Biochem J. 1978 Aug 1;173(2):543–552. doi: 10.1042/bj1730543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fick R. B., Jr, Naegel G. P., Squier S. U., Wood R. E., Gee J. B., Reynolds H. Y. Proteins of the cystic fibrosis respiratory tract. Fragmented immunoglobulin G opsonic antibody causing defective opsonophagocytosis. J Clin Invest. 1984 Jul;74(1):236–248. doi: 10.1172/JCI111407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fick R. B., Jr Pathogenesis of the pseudomonas lung lesion in cystic fibrosis. Chest. 1989 Jul;96(1):158–164. doi: 10.1378/chest.96.1.158. [DOI] [PubMed] [Google Scholar]
- Goldstein W., Döring G. Lysosomal enzymes from polymorphonuclear leukocytes and proteinase inhibitors in patients with cystic fibrosis. Am Rev Respir Dis. 1986 Jul;134(1):49–56. doi: 10.1164/arrd.1986.134.1.49. [DOI] [PubMed] [Google Scholar]
- Greenwald R. A., Rush S. W., Moak S. A., Weitz Z. Conversion of superoxide generated by polymorphonuclear leukocytes to hydroxyl radical: a direct spectrophotometric detection system based on degradation of deoxyribose. Free Radic Biol Med. 1989;6(4):385–392. doi: 10.1016/0891-5849(89)90084-1. [DOI] [PubMed] [Google Scholar]
- Gutteridge J. M., Paterson S. K., Segal A. W., Halliwell B. Inhibition of lipid peroxidation by the iron-binding protein lactoferrin. Biochem J. 1981 Oct 1;199(1):259–261. doi: 10.1042/bj1990259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliwell B., Aruoma O. I., Wasil M., Gutteridge J. M. The resistance of transferrin, lactoferrin and caeruloplasmin to oxidative damage. Biochem J. 1988 Nov 15;256(1):311–312. doi: 10.1042/bj2560311a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliwell B., Gutteridge J. M. Formation of thiobarbituric-acid-reactive substance from deoxyribose in the presence of iron salts: the role of superoxide and hydroxyl radicals. FEBS Lett. 1981 Jun 15;128(2):347–352. doi: 10.1016/0014-5793(81)80114-7. [DOI] [PubMed] [Google Scholar]
- Holder I. A. Experimental studies of the pathogenesis of infections due to Pseudomonas aeruginosa: effect of treatment with protease inhibitors. Rev Infect Dis. 1983 Nov-Dec;5 (Suppl 5):S914–S921. doi: 10.1093/clinids/5.supplement_5.s914. [DOI] [PubMed] [Google Scholar]
- Jackson A. H., Hill S. L., Afford S. C., Stockley R. A. Sputum sol-phase proteins and elastase activity in patients with cystic fibrosis. Eur J Respir Dis. 1984 Feb;65(2):114–124. [PubMed] [Google Scholar]
- Kaur H., Fagerheim I., Grootveld M., Puppo A., Halliwell B. Aromatic hydroxylation of phenylalanine as an assay for hydroxyl radicals: application to activated human neutrophils and to the heme protein leghemoglobin. Anal Biochem. 1988 Aug 1;172(2):360–367. doi: 10.1016/0003-2697(88)90456-3. [DOI] [PubMed] [Google Scholar]
- Klebanoff S. J., Hamon C. B. Role of myeloperoxidase-mediated antimicrobial systems in intact leukocytes. J Reticuloendothel Soc. 1972 Aug;12(2):170–196. [PubMed] [Google Scholar]
- Kreger A. S. Pathogenesis of Pseudomonas aeruginosa ocular diseases. Rev Infect Dis. 1983 Nov-Dec;5 (Suppl 5):S931–S935. doi: 10.1093/clinids/5.supplement_5.s931. [DOI] [PubMed] [Google Scholar]
- Laemmli U. K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970 Aug 15;227(5259):680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- Legrand D., Mazurier J., Montreuil J., Spik G. Structure and spatial conformation of the iron-binding sites of transferrins. Biochimie. 1988 Sep;70(9):1185–1195. doi: 10.1016/0300-9084(88)90184-8. [DOI] [PubMed] [Google Scholar]
- Leibman A., Aisen P. Distribution of iron between the binding sites of transferrin in serum: methods and results in normal human subjects. Blood. 1979 Jun;53(6):1058–1065. [PubMed] [Google Scholar]
- MacGillivray R. T., Mendez E., Shewale J. G., Sinha S. K., Lineback-Zins J., Brew K. The primary structure of human serum transferrin. The structures of seven cyanogen bromide fragments and the assembly of the complete structure. J Biol Chem. 1983 Mar 25;258(6):3543–3553. [PubMed] [Google Scholar]
- Makey D. G., Seal U. S. The detection of four molecular forms of human transferrin during the iron binding process. Biochim Biophys Acta. 1976 Nov 26;453(1):250–256. doi: 10.1016/0005-2795(76)90270-1. [DOI] [PubMed] [Google Scholar]
- Mohammed J. R., Mohammed B. S., Pawluk L. J., Bucci D. M., Baker N. R., Davis W. B. Purification and cytotoxic potential of myeloperoxidase in cystic fibrosis sputum. J Lab Clin Med. 1988 Dec;112(6):711–720. [PubMed] [Google Scholar]
- Motohashi N., Mori I. Superoxide-dependent formation of hydroxyl radical catalyzed by transferrin. FEBS Lett. 1983 Jun 27;157(1):197–199. doi: 10.1016/0014-5793(83)81144-2. [DOI] [PubMed] [Google Scholar]
- Nauseef W. M. Posttranslational processing of a human myeloid lysosomal protein, myeloperoxidase. Blood. 1987 Oct;70(4):1143–1150. [PubMed] [Google Scholar]
- Oe H., Takahashi N., Doi E., Hirose M. Effects of anion binding on the conformations of the two domains of ovotransferrin. J Biochem. 1989 Nov;106(5):858–863. doi: 10.1093/oxfordjournals.jbchem.a122942. [DOI] [PubMed] [Google Scholar]
- Penner M. H., Yamasaki R. B., Osuga D. T., Babin D. R., Meares C. F., Feeney R. E. Comparative oxidations of tyrosines and methionines in transferrins: human serum transferrin, human lactotransferrin, and chicken ovotransferrin. Arch Biochem Biophys. 1983 Sep;225(2):740–747. doi: 10.1016/0003-9861(83)90085-1. [DOI] [PubMed] [Google Scholar]
- Pier G. B. Pulmonary disease associated with Pseudomonas aeruginosa in cystic fibrosis: current status of the host-bacterium interaction. J Infect Dis. 1985 Apr;151(4):575–580. doi: 10.1093/infdis/151.4.575. [DOI] [PubMed] [Google Scholar]
- Pou S., Cohen M. S., Britigan B. E., Rosen G. M. Spin-trapping and human neutrophils. Limits of detection of hydroxyl radical. J Biol Chem. 1989 Jul 25;264(21):12299–12302. [PubMed] [Google Scholar]
- Reynolds H. Y. Bronchoalveolar lavage. Am Rev Respir Dis. 1987 Jan;135(1):250–263. doi: 10.1164/arrd.1987.135.1.250. [DOI] [PubMed] [Google Scholar]
- Root R. K., Cohen M. S. The microbicidal mechanisms of human neutrophils and eosinophils. Rev Infect Dis. 1981 May-Jun;3(3):565–598. doi: 10.1093/clinids/3.3.565. [DOI] [PubMed] [Google Scholar]
- Suter S., Schaad U. B., Roux L., Nydegger U. E., Waldvogel F. A. Granulocyte neutral proteases and Pseudomonas elastase as possible causes of airway damage in patients with cystic fibrosis. J Infect Dis. 1984 Apr;149(4):523–531. doi: 10.1093/infdis/149.4.523. [DOI] [PubMed] [Google Scholar]
- Suter S., Schaad U. B., Tegner H., Ohlsson K., Desgrandchamps D., Waldvogel F. A. Levels of free granulocyte elastase in bronchial secretions from patients with cystic fibrosis: effect of antimicrobial treatment against Pseudomonas aeruginosa. J Infect Dis. 1986 May;153(5):902–909. doi: 10.1093/infdis/153.5.902. [DOI] [PubMed] [Google Scholar]
- Suter S. The imbalance between granulocyte neutral proteases and antiproteases in bronchial secretions from patients with cystic fibrosis. Antibiot Chemother (1971) 1989;42:158–168. doi: 10.1159/000417616. [DOI] [PubMed] [Google Scholar]
- Thomas M. J., Shirley P. S., Hedrick C. C., DeChatelet L. R. Role of free radical processes in stimulated human polymorphonuclear leukocytes. Biochemistry. 1986 Dec 2;25(24):8042–8048. doi: 10.1021/bi00372a037. [DOI] [PubMed] [Google Scholar]
- Ward P. A., Till G. O., Kunkel R., Beauchamp C. Evidence for role of hydroxyl radical in complement and neutrophil-dependent tissue injury. J Clin Invest. 1983 Sep;72(3):789–801. doi: 10.1172/JCI111050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss S. J., Lampert M. B., Test S. T. Long-lived oxidants generated by human neutrophils: characterization and bioactivity. Science. 1983 Nov 11;222(4624):625–628. doi: 10.1126/science.6635660. [DOI] [PubMed] [Google Scholar]
- Weiss S. J. Oxygen, ischemia and inflammation. Acta Physiol Scand Suppl. 1986;548:9–37. [PubMed] [Google Scholar]
- Weiss S. J. Tissue destruction by neutrophils. N Engl J Med. 1989 Feb 9;320(6):365–376. doi: 10.1056/NEJM198902093200606. [DOI] [PubMed] [Google Scholar]
- Williams J., Moreton K. The distribution of iron between the metal-binding sites of transferrin human serum. Biochem J. 1980 Feb 1;185(2):483–488. doi: 10.1042/bj1850483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winterbourn C. C. Lactoferrin-catalysed hydroxyl radical production. Additional requirement for a chelating agent. Biochem J. 1983 Jan 15;210(1):15–19. doi: 10.1042/bj2100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winterbourn C. C., Molloy A. L. Susceptibilities of lactoferrin and transferrin to myeloperoxidase-dependent loss of iron-binding capacity. Biochem J. 1988 Mar 1;250(2):613–616. doi: 10.1042/bj2500613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winterbourn C. C. Myeloperoxidase as an effective inhibitor of hydroxyl radical production. Implications for the oxidative reactions of neutrophils. J Clin Invest. 1986 Aug;78(2):545–550. doi: 10.1172/JCI112607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray W., Boulikas T., Wray V. P., Hancock R. Silver staining of proteins in polyacrylamide gels. Anal Biochem. 1981 Nov 15;118(1):197–203. doi: 10.1016/0003-2697(81)90179-2. [DOI] [PubMed] [Google Scholar]
- Wretlind B., Pavlovskis O. R. Pseudomonas aeruginosa elastase and its role in pseudomonas infections. Rev Infect Dis. 1983 Nov-Dec;5 (Suppl 5):S998–1004. doi: 10.1093/clinids/5.supplement_5.s998. [DOI] [PubMed] [Google Scholar]
- Zweier J. L., Wooten J. B., Cohen J. S. Studies of anion binding by transferrin using carbon-13 nuclear magnetic resonance spectroscopy. Biochemistry. 1981 Jun 9;20(12):3505–3510. doi: 10.1021/bi00515a031. [DOI] [PubMed] [Google Scholar]