Abstract
Objectives
The maintenance of infectivity of influenza viruses on the surfaces of personal protective equipment and clothing is an important factor in terms of controlling viral cross-infection in the environment and preventing contact infection. The aim of this study was to determine if laboratory-grown influenza A (H1N1) virus maintained infectivity on the surfaces of personal protective equipment and clothing used in healthcare settings.
Methods
Influenza A virus (0.5 mL) was deposited on the surface of a rubber glove, an N95 particulate respirator, a surgical mask made of non-woven fabric, a gown made of Dupont Tyvek, a coated wooden desk, and stainless steel. Each sample was left for 1, 8, and 24 h, and hemagglutination (HA) and 50% tissue culture infective dose (TCID50)/mL were measured.
Results
The HA titer of this influenza A virus did not decrease in any of the materials tested even after 24 h. The infectivity of influenza A virus measured by TCID50 was maintained for 8 h on the surface of all materials, with the exception of the rubber glove for which virus infectivity was maintained for 24 h.
Conclusions
Our results indicate that the replacement/renewal of personal protective equipment and clothing by healthcare professionals in cases of exposure to secretions and droplets containing viruses spread by patients is an appropriate procedure to prevent cross-infection.
Keywords: Control, Cross-infection, Environment, Infectivity, Influenza
Introduction
Healthcare professionals may be exposed to high doses of influenza viruses during their examination of patients [1]. The healthcare environment is commonly contaminated with secretions and droplets, including viruses spread by patients. It is likely that viruses shed by influenza virus-infected patients are responsible for the maintenance of virus infectivity in the environment [2–5]. Accordingly, measures should be taken to limit influenza virus contamination of the environment to prevent cross-infection among healthcare professionals.
Healthcare professionals use personal protective equipment and clothing to prevent infection [6, 7] that may include any type of clothing, equipment, or respiratory protective device designed to protect against droplet infection [8]. Personal protective equipment and clothing, such as gloves, gowns, surgical masks, and N95 particulate respirators, can prevent direct contact with viruses, but the surface of the equipment may still become contaminated [9–11] with virus particles. Consequently, the inappropriate disposal of such protective equipment and clothing after use may result in inadvertent exposure to virus contamination through contact with the surface of the material. Additionally, people frequently touch their face with their hands [12], which may also result in contact infection.
A number of studies have shown that the influenza virus can maintain infectivity on environmental surfaces. Bean et al. [13] investigated the survival of laboratory-grown influenza A (H1N1) virus on the surfaces of various materials, such as stainless steel, plastic, pajamas, tissue paper, magazines, and a handkerchief. These researchers found that the 50% of the tissue culture infective dose (TCID50) was reduced to below the detection limit on the pajamas, tissue paper, magazines, and a handkerchief after 12 h, while the virus maintained infectivity for 24 h on the plastic and stainless steel surfaces, with the TCID50 falling below the detection limit only after 48 h.
In order to prevent cross-infection via personal protective equipment in healthcare settings, it is necessary to know how long the influenza virus maintains infectivity on the surface of such equipment. However, to the best of our knowledge, there have been very few studies on this aspect of virus infectivity and public healthcare. The aim of this study was to determine both whether influenza viruses maintain infectivity and survive on the surfaces of personal protective equipment in healthcare settings and the appropriate time to replace personal protective equipment.
Materials and methods
In this study we used influenza A (H1N1) virus strain A/PR/8/34 [ATCC VR-95, 1280 hemagglutination (HA) units, 1999-12-10] obtained from allantoic fluid. We conducted a series of experiments designed to assess the duration of the infectivity of influenza A viruses on the surfaces of personal protective equipment in healthcare settings.
The surfaces used as test materials included a rubber glove, an N95 particulate respirator (Hi-Luck 350; Koken, Tokyo, Japan), a surgical mask made of non-woven fabric, a gown made of Dupont Tyvek, a coated wooden desk, and stainless steel. Tyvek is a material made from 0.5- to 10-μm, very fine, continuous polyethylene fibers bonded together by heat. Being very soft and strong, it is widely used as a material for gowns used by healthcare professionals [14]. A coated wooden desk and stainless steel surface were used as samples for comparison with personal protective equipment. A sample (0.5 mL) of viral suspension containing 103.8 TCID50/mL was deposited on a 3-cm2 area of each test material. A 0.5-mL volume was selected because this volume was the optimal volume for collection with a cotton pad.
The HA and the TCID50/mL were measured at 0 h, immediately after application of the viral suspension, to provide baseline data to monitor the changes over time. Aliquots of influenza A/PR/8/34(H1N1) were deposited and remained on the surface of each material for 0, 1, 8, or 24 h. The temperature of the laboratory was maintained at 25.2°C, and the relative humidity was 55%.
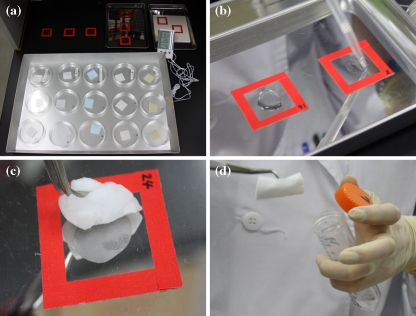
At the specified time periods post-virus application (1, 8, 24 h), a piece of the rubber glove, N95 particulate respirator, surgical mask made of a non-woven fabric, and gown made of Dupont Tyvek were each placed in a separate centrifuge tube containing 5 mL phosphate-buffered saline (PBS). If liquid was left on the coated wooden desk or stainless steel, it was aspirated with a dropper, and the residual liquid was wiped with absorbent cotton. Both the aspirated liquid and the absorbent cotton were also placed in a centrifuge tube containing 5 mL PBS. The solution containing the recovered virus from each material was then mixed for 30 s on a vortex mixer to dislodge any attached test virus. The virus solutions obtained were used for quantification. Figure 1 shows the procedure for recovering the virus on the coated wooden desk and stainless steel surfaces.
Fig. 1.
Methods used for virus inoculation and subsequent virus isolation from various surfaces. a Virus was recovered from a 3-cm2 test piece of a rubber glove, N95 particulate respirator, non-woven surgical mask, and gown made of Dupont Tyvek. A 3-cm2 area of coated wooden desk and stainless steel was enclosed with tape for application of the viral suspension. b The liquid remaining on the coated wooden desk and stainless steel was recovered by aspiration with a dropper. c The residual liquid after aspiration and the dried liquid were recovered by wiping with absorbent cotton. d The liquid thus recovered was placed in a centrifuge tube containing 5 mL phosphate buffered saline, and the resulting solution was mixed for 30 s on a Vortex mixer to wash out the test virus. The virus solutions thus obtained were used as samples for quantification
Determination of HA titer
The recovered virus solution (50 μL) was serially diluted twice with 50 μL veronal-buffered saline (diluent), pH 6.6, and 50 μL of 1% avian erythrocyte solution prepared using the diluent was then added and mixed. The mixture was allowed to stand in a refrigerator before the HA titer was defined as the highest dilution causing agglutination.
Determination of virus infectivity titer (TCID50)
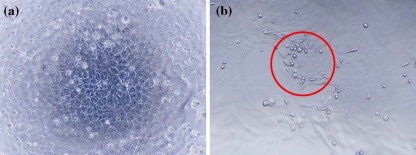
Virus preparations recovered from various surfaces were serially diluted tenfold in PBS. The diluted virus solutions were used to inoculate Madin–Darby canine kidney (MDCK) cells cultured in medium [Dulbecco’s modified Eagle’s medium supplemented with 5% fetal bovine serum (FBS) and containing 100 IU/mL penicillin and 100 mg/mL streptomycin) in 96-well plates and incubated for 3 days in a 5% CO2 incubator at 37°C. After incubation, the cells in each well were examined by light microscopy to observe any cytopathic effect (CPE) caused by virus infection. The TCID50 was determined as the dilution of sample at which the virus infected 50% of the MDCK cells in the wells to cause CPE. Since the influenza virus is able to infect MDCK cells, the appearance of CPE was considered to be specifically caused by influenza virus infection. The appearance of normal MDCK cells is shown in Fig. 2a, while cells showing typical CPE due to virus proliferation are shown in Fig. 2b. The TCID50 was determined on the basis of the number of CPE-positive wells to calculate the infectivity titer of the test virus (TCID50/mL) and calculated using the Reed–Muench formula [15].
Fig. 2.
Cytopathic effect (CPE) observed in influenza virus-inoculated Madin–Darby canine kidney (MDCK) cells. a Normal, uninfected MDCK cells, b MDCK cells showing cell rounding consistent with the CPE observed with influenza virus proliferation
Results
The HA titer of the influenza virus solution was determined to be 64 for all samples at 0 h, immediately after the application of virus suspensions onto the surface of each material. At 1, 8, and 24 h post-virus application, the HA titer on the surface of all samples was 32, demonstrating that the HA titer of the influenza virus remained stable over time without any marked decrease, irrespective of the material.
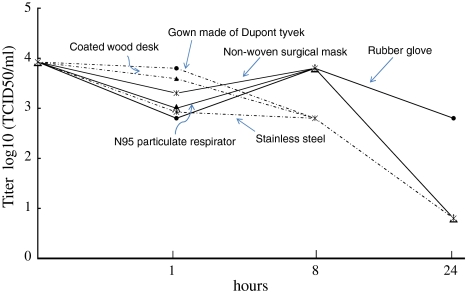
The TCID50/mL of the solution of influenza virus was 103.8 for all samples of the virus recovered at 0 h, immediately after application of the virus suspension. At 1, 8, and 24 h post-virus application, the TCID50/mL of the virus suspension on the surface of the rubber glove was 102.8. In comparison, the TCID50/mL of the virus suspension on the N95 particulate respirator surface was 103.0 after 1 h, increasing to 103.8 after 8 h, before decreasing to 100.8 after 24 h. Similar to the N95 particulate respirator surface, the mask made of a non-woven fabric had a TCID50/mL of 100.8 after 24 h. Virus survival on the Tyvek surface was determined to be 102.8 TCID50/mL after 8 h and 100.8 after 24 h. On the surface of the coated desk, the TCID50/mL was 103.6 after 1 h, 102.8 after 8 h, and 100.8 after 24 h. The TCID50/mL on the stainless steel surface was 102.8 after 8 h and 100.8 after 24 h. Figure 3 shows a summary of the changes in TCID50/mL for the influenza virus suspension allowed to stand on the surface of each material for the specified periods.
Fig. 3.
The value of 50% tissue culture infective dose (TCID50) of influenza virus recovered from various surfaces after 0, 1, 8, and 24 h exposure. The detection limit of the TCID50 assay was determined to be 0.8 log10 TCID50/mL
Discussion
The aim of this study was to assess the time course of changes in influenza virus infectivity on personal protective equipment used in healthcare settings. The results demonstrate that the virus TCID50 was relatively stable at a certain level on the surface of personal protective equipment after 8 h. However, after 24 h, while the HA titer remained at a relatively stable level in all samples, the TCID50 decreased to below the detection limit in all samples except the rubber glove.
The stability of the HA titer after 24 h seems to be explained by the inherent properties of virus-associated carbohydrates and proteins. Hemagglutinin, found on the surface of the influenza virus, is composed of sialic acid-binding polysaccharides [16] and carbohydrates resistant to heat and dryness. Since the HA assay detects the red blood cell agglutinating ability of hemagglutinin, regardless of the presence of infectious influenza virus, the assay was able to detect HA even after 24 h. In contrast, virus-associated proteins necessary for the infectivity of influenza virus are susceptible to heat and dryness, and this susceptibility is likely to be the reason why the virus infectivity, as determined by TCID50, was reduced over time.
Surgical masks and N95 particulate respirators are made from non-woven fabric and are used by healthcare professionals during patient examinations [9, 17, 18] or by patients to prevent transmission of a virus [19, 20]. In our experiments, the virus maintained infectivity on the surfaces of the surgical mask and the N95 particulate respirator for at least 8 h. There have been no reports to date on the maintenance of infectivity of the influenza virus on non-woven fabric surface. However, Bean et al. [13] reported that the TCID50 on the surface of a handkerchief and pajamas decreased to below the detection limit in 12 h.
We considered that a virus would dry on the Tyvek surface, a material used to manufacture medical gowns because these materials do not absorb water. We observed that under our experimental conditions, the virus maintained its infectivity for at least 8 h, but it was below the detection limit after 24 h.
In our study, a coated wooden desk and stainless steel were used as samples for comparison with personal protective equipment. In healthcare settings, these materials may be contaminated by droplets containing pathogens from patients [11]. These materials, as well as Tyvek, do not absorb water. We found that the influenza virus maintained infectivity for at least 8 h post-virus application on the surface of these materials, without showing any decrease in TCID50, subsequently falling to below the detection limit in 24 h. This finding suggests that the virus did not maintain its infectivity for 24 h, which is consistent with the results obtained from the samples of personal protective equipment. According to Bean et al. [13], a laboratory-grown influenza A virus (A/H1N1) maintained infectivity for at least 24 h on the surface of stainless steel at a temperature between 27.8 and 28.3°C and 35–40% relative humidity, and TCID50 reached the detection limit in 48 h. During our study, the temperature of the laboratory was maintained at 25.2°C and 55% relative humidity. This humidity was slightly higher than that in the study conducted by Bean et al. [13] and was less favorable for infectivity of the influenza virus [21, 22].
Rubber gloves are recommended as a standard public health precaution [23, 24] and are used for almost all procedures in healthcare settings [25]. Under the conditions of this study, the TCID50 on the surface of the rubber glove remained at a relatively stable level for at least 24 h post-virus application. Future studies should focus on whether a virus maintains its infectivity for more than 24 h on the surface of rubber gloves under the same conditions. One possible mechanism for the infectivity of the virus being maintained on the rubber glove is that the surface of the rubber glove was hydrophobically treated, while the other samples were hydrophilic. The virus solution formed water droplets on the rubber glove and, as a result, the droplets became embedded in the protein of the egg used to proliferate the laboratory-grown influenza virus, consequently protecting the virus from drying out.
It is clear from the results of our studies that influenza virus contained in droplets is able to maintain its infectivity on the surface of personal protective equipment as well as on a coated wooden desk and stainless steel in medical settings for at least 8 h. However, on the surface of rubber gloves, the virus can maintain its infectivity for the relatively long time of 24 h. Accordingly, healthcare professionals should renew/replace personal protective equipment if they have been exposed to droplets from patients with influenza [26, 27]; however, in practice, personal protective equipment cannot be replaced for each patient. For example, during the severe acute respiratory syndrome (SARS) panademic, personal protective equipment could not be replaced for each patient for the simple reason that there was a shortage in the supply of such equipment and clothing [28]. However, our findings suggest that caring for patients without an renewal or replacement of protective equipment may be responsible for cross-infection of influenza virus and, therefore, that a frequent replacement of personal protective equipment for each patient would prevent cross-infection. Since we have shown that the influenza virus maintains infectivity for at least 8 h on almost all surfaces, the disposal of personal protective equipment to prevent cross-infection after possible exposure to influenza virus is an important healthcare procedure.
This study has a number of limitations. First, the experiments were only conducted at one specific temperature and 55% relative humidity. This experiment should be conducted under various conditions of low temperatures and low humidity, such as those found during winter when an influenza pandemic is likely to break out. The second limitation is that our experiments did not assess the time course of changes in virus infectivity between 8 and 24 h. Therefore, the possibility cannot be ruled out that infectivity was lost in <24 h. The third limitation is that our experiments used a laboratory-grown influenza A virus, while a previous study conducted to assess the infectivity of the influenza virus showed that influenza virus mixed with human mucus maintained its infectivity on the surfaces of banknotes up to 17 days [29]. On the basis of this latter finding, we hope to investigate the infectivity of dried influenza virus or droplets mixed with mucus on the surfaces of personal protective equipment. Since the amount of virus in droplets emitted from patients with influenza has not been reported in the literature, it is unknown whether the amount of virus in such droplets is equivalent to that in the virus solution used in our experiments. This issue remains to be elucidated in future studies. Further studies involving a larger number of samples are required to assess the validity of this study.
In conclusion, the appropriate exchange of personal protective equipment in cases of exposure to secretions and droplets, including viruses spread by patients, should be encouraged among healthcare professionals to prevent cross-infection of the influenza virus.
Acknowledgments
We thank Tomomi Yoshida of Kitasato University School of Allied Health Sciences for her editorial assistance and all of the people who cooperated in the study. This study was supported by the Kitasato Research Center of Environmental Sciences.
References
- 1.Swaminathan A, Martin R, Gamon S, Aboltins C, Athan E, Braitberg G, et al. Personal protective equipment and antiviral drug use during hospitalization for suspected avian or pandemic influenza. Emerg Infect Dis. 2007;13:1541–1547. doi: 10.3201/eid1310.070033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.West K. Infection-control basics. A common sense review for EMS personnel. J Emerg Med Serv. 2002;27:115–125. [PubMed] [Google Scholar]
- 3.Barker J, Stevens D, Bloomfield SF. Spread and prevention of some common viral infections in community facilities and domestic homes. J Appl Microbiol. 2001;91:7–21. doi: 10.1046/j.1365-2672.2001.01364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cowling BJ, Chan KH, Fang VJ, Cheng CK, Fung RO, Wai W, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a randomized trial. Ann Intern Med. 2009;151:437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Novel influenza A (H1N1) virus infections among health-care personnel-United States, April–May 2009. MMWR Morb Mortal Wkly Rep. 2009;58:641–645. [PubMed] [Google Scholar]
- 6.Phin NF, Rylands AJ, Allan J, Edwards C, Enstone JE, Nguyen-Van-Tam JS. Personal protective equipment in an influenza pandemic: a UK simulation exercise. J Hosp Infect. 2009;71:15–21. doi: 10.1016/j.jhin.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Daugherty EL, Perl TM, Needham DM, Rubinson L, Bilderback A, Rand CS. The use of personal protective equipment for control of influenza among critical care clinicians: a survey study. Crit Care Med. 2009;37:1210–1216. doi: 10.1097/CCM.0b013e31819d67b5. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation in the United States—early, targeted, layered use of nonpharmaceutical interventions. Available at: http://www.pandemicflu.gov/plan/community/community_mitigation.pdf. Accessed 30 Aug 2009.
- 9.Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowell SF, Simmerman JM, Erdman DD, Wu JS, Chaovavanich A, Javadi M, et al. Severe acute respiratory syndrome coronavirus on hospital surfaces. Clin Infect Dis. 2004;39:652–657. doi: 10.1086/422652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Booth TF, Kournikakis B, Bastien N, Ho J, Kobasa D, Stadnyk L, et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis. 2005;191:1472–1477. doi: 10.1086/429634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicas M, Best D. A study quantifying the hand-to-face contact rate and its potential application to predicting respiratory tract infection. J Occup Environ Hyg. 2008;5:347–352. doi: 10.1080/15459620802003896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bean B, Moore BM, Sterner F, Peterson LR, Gerding DN, Balfour HH., Jr Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146:47–51. doi: 10.1093/infdis/146.1.47. [DOI] [PubMed] [Google Scholar]
- 14.DuPont Medical Fabrics. Advances in medical fabrics technology improve protection for patients and healthcare professionals. Fabric technology helps protect patients and healthcare workers. Advancing world health. DuPont Medical Fabrics, 2003. Available at: http://www2.dupont.com/Medical_Fabrics/en_US/pdf/AdvancingWorldHealth.pdf. Accessed 30 Aug 2009.
- 15.Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 16.Mahy BWJ, van Regenmortel M. Encyclopedia of virology. vol. 5, 3rd ed. Amsterdam: Elsevier; 2008.
- 17.Qian Y, Willeke K, Grinshpun SA, Donnelly J, Coffey CC. Performance of N95 respirators: filtration efficiency for airborne microbial and inert particles. Am Ind Hyg Assoc J. 1998;59:128–132. doi: 10.1080/15428119891010389. [DOI] [PubMed] [Google Scholar]
- 18.Possamai MA. SARS and health worker safety: lessons for influenza pandemic planning and response. Healthc Pap. 2007;8:18–28. doi: 10.12927/hcpap.2007.19354. [DOI] [PubMed] [Google Scholar]
- 19.MacIntyre CR, Cauchemez S, Dwyer DE, Seale H, Cheung P, Browne G, et al. Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis. 2009;15:233–241. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau JT, Kim JH, Tsui HY, Griffiths S. Anticipated and current preventive behaviors in response to an anticipated human-to-human H5N1 epidemic in the Hong Kong Chinese general population. BMC Infect Dis. 2007;7:18–29. doi: 10.1186/1471-2334-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harper GJ. Airborne micro-organisms: survival tests with four viruses. J Hyg (Lond) 1961;59:479–486. doi: 10.1017/S0022172400039176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Australian Government Department of Health. Australian Government Department of Health and ageing guidelines for the prevention and control of influenza outbreaks in residential care facilities for public health units in Australia. Australian Government Department of Health, 2005.
- 24.World Health Organization. World Health Organization infection control recommendations for avian influenza in health-care facilities. (Amended 13 April 2008). Available at: http://www.who.int/csr/disease/avian_influenza/guidelines/aidememoireinfcont/en/index.html. Accessed 30 Aug 2009.
- 25.Muto CA, Sistrom MG, Strain BA, Farr BM. Glove leakage rates as a function of latex content and brand: caveat emptor. Arch Surg. 2000;135:982–985. doi: 10.1001/archsurg.135.8.982. [DOI] [PubMed] [Google Scholar]
- 26.UK Department of Health/UK Health Protection Agency. Pandemic influenza: guidance for infection control in critical care. Department of Health, UK. 2008. Available at: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_084179.pdf. Accessed 30 Aug 2009.
- 27.Sehulster L, Chinn RY. Centers for Disease Control and Prevention. Guidelines for environmental infection control in health-care facilities: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) MMWR Recomm Rep. 2003;52:1–42. [PubMed] [Google Scholar]
- 28.Tan NC, Goh LG, Lee SS. Family physicians’ experiences, behaviour, and use of personal protection equipment during the SARS outbreak in Singapore: do they fit the Becker Health Belief Model? Asia Pac J Public Health. 2006;18(3):49–56. doi: 10.1177/10105395060180030901. [DOI] [PubMed] [Google Scholar]
- 29.Thomas Y, Vogel G, Wunderli W, Sute P, Witschi M, Koch D, et al. Survival of influenza virus on banknotes. Appl Environ Microbiol. 2008;74:3002–3007. doi: 10.1128/AEM.00076-08. [DOI] [PMC free article] [PubMed] [Google Scholar]