SUMMARY
Picornaviruses are small, non-enveloped, single stranded, positive sense RNA viruses which cause multiple diseases including myocarditis/dilated cardiomyopathy, type 1 diabetes, encephalitis, myositis, orchitis and hepatitis. Although picornaviruses directly kill cells, tissue injury primarily results from autoimmunity to self antigens. Viruses induce autoimmunity by: aborting deletion of self-reactive T cells during T cell ontogeny; reversing anergy of peripheral autoimmune T cells; eliminating T regulatory cells; stimulating self-reactive T cells through antigenic mimicry or cryptic epitopes; and acting as an adjuvant for self molecules released during virus infection. Most autoimmune diseases (SLE, rheumatoid arthritis, Grave’s disease) predominate in females, but diseases associated with picornavirus infections predominate in males. T regulatory cells are activated in infected females because of the combined effects of estrogen and innate immunity.
Keywords: Autoimmunity, picornavirus, T regulatory cells, estrogen, sex differences
INFECTION AND AUTOIMMUNITY
Microbial infections are strongly implicated as risk factors for the induction of autoimmunity [1], including such diseases as type 1 diabetes [2], rheumatic heart disease [3], myocarditis [4], multiple sclerosis [5], and rheumatoid arthritis/systemic lupus erythematosis [6], but the precise host and microbial characteristics or conditions required for autoimmunity initiation are poorly understood. Three factors are necessary for the development of an autoimmune disease. These are: 1) the presence of a repertoire of autoreactive lymphocytes; 2) activation of the autoreactive cells; and 3) absence of the normal immunoregulatory mechanisms which suppress autoimmunity [7]. T cells are pivotal to the immune response as these cells directly mediate inflammation through release of chemokines and cytokines, and induce target cell cytotoxicity; and provide B cell help for IgG, IgA, and IgE responses. There are several mechanisms by which infections can lead to autoimmunity.
1. Loss of tolerance
The first mechanism is loss of tolerance. Tolerance is induced either centrally in the thymus during T cell ontogeny or peripherally through anergy or induction of regulatory cells. Self-reactive prothymocytes enter the thymus where high affinity interactions between the T cell receptors on the developing T cells and major histocompatibility complex (MHC) antigen on thymic epithelium initiates clonal deletion of autoreactive T cells through apoptosis. Infections with viruses (HIV, rabies), bacteria (F. turalenesis), parasites (T. cruzi, P. chaubi, S. mansoni, T. spiralis) and fungi (H. capsulatum, P. brasiliensis) cause thymic atrophy by increasing glucorticoid hormone levels which activate caspases 3 and 8[8, 9]. Similarly, infections with coxsackievirus B3, but not with coxsackievirus B1 or other picornaviruses, cause both thymic and peripheral T cell atrophy [10], but in this case glucorticoid hormones may not be involved as adenalectomy failed to prevent thymic involution. In addition to apoptosis of T cells, infection alters intrathymic T cell migration resulting in increased release of immature T cell and self-reactive T cells into the periphery [8]. After leaving the thymus, autoreactive T cells should be subjected to peripheral tolerance. Peripheral tolerance can result either from deletion or anergy of self reactive cells by inappropriate antigen presentation [11]. Anergy is a functional state in which T cell proliferation and cytokine production are suppressed, and is usually attributed to inhibition of signal transduction subsequent to T cell receptor (TCR) and co-stimulatory molecule (CD28) engagement [12]. Anergized T cells show impaired tyrosine kinase phosphorylation of the T cell receptor and blocked phosphorylation of signal kinase (MAPK, ERK, JNK) pathways downstream of the T cell receptor [13, 14]. Anergized cells remain alive for extended periods, but are incapable of responding even when the appropriate antigen is presented by professional antigen presenting cells. Recently, other mechanisms of T cell anergy have been proposed. Studies indicate that the cell cycle inhibitor p27kip1 is increased during anergy and that over-expression of this molecule induces an anergic state [15, 16], although whether p27kip1 induces anergy through prevention of T cell proliferation or through promoting Smad3 dependent transcription is controversial [17]. In addition to activation of downstream kinases, CD28 increases cellular metabolism including glucose and amino acid uptake and protein synthesis through Akt and mTOR (mammalian target of rapamycin) [18]. Blocking cellular metabolism anergizes T cells despite normal engagement of TCR/CD28 and signal transduction [18]. Finally, anergy can be actively induced in T cells through PD-1 (programmed death-1)/PD-L1 interactions. PD-1 is an inhibitory molecule belonging to the CD28 family, which is up-regulated on T cells after antigen stimulation and inhibits T cell proliferation and cytokine production [19]. Furthermore, PD-1/PD-L1 interactions induce T cell anergy though suppression of IL-2 response [20]. PD-1/PD-L1 interactions and T cell anergy are important in myocarditis [21–23]. Mice deficient in PD-1 spontaneously develop myocarditis [22] and treating coxsackievirus B3 infected animals with agonist anti-PD-1 antibody augments both myocardial inflammation and pro-inflammatory cytokine expression [23].
It is unlikely that viral infections rescue anergized autoimmune T cells through inhibition of MAPK/ERK since many virus infections, including picornaviruses, are known to activate these pathways[24, 25]. p38 MAPK activation is necessary for maximal virus production, and most likely is essential for progeny virus release since viral protein synthesis is not affected by inhibition of p38MAPK. The mechanism for virus-induced MAPK/ERK activation during picornavirus infection probably depends upon functional lipid rafts which are required for virus internalization and targeting of the virus to the golgi [26], but are also implicated in MAKP/ERK activation [27]. If viruses are unlikely to rescue anergized autoimmune T cells through suppression of p38MAPK, they might be highly effective in promoting autoimmunity through production of IL-2. High levels of IL-2 reverse T cell anergy and can potentially lead to autoimmunity [28]. Infection of mice with non-myocarditic variants of coxsackievirus B3 induce little IL-2 while infections with myocarditic virus variants stimulate strong IL-2 responses [29]. Injection of exogenous recombinant IL-2 into mice infected with non-pathogenic coxsackievirus B3 restores myocarditis susceptibility suggesting that viral myocarditis requires IL-2 to reverse T cell anergy and that only virus variants capable of promoting good IL-2 responses will induce this disease.
2. Loss of T regulatory cells
Diverse populations of lymphoid cells have the capacity to inhibit immune responses. Although most reports center on CD4+ T regulatory cells, CD8+ T regulatory cells are similar both in their generation and function [30, 31]. With each cell population (CD4+ or CD8+), immunosuppressive cells can be divided into natural and inducible populations.
Natural T regulatory cells arise from the CD4+CD8+ developmental stage by induction of both CD25 and Forkhead box P3 (FoxP3) transcription factor; the latter factor sustaining and stabilizing the regulatory activity of these cells [32]. FoxP3 binds to approximately 700 genes [33]. Among its other functions, FoxP3 blocks the ability of NFAT and NFkB to activate their target genes resulting in transcriptional suppression of cytokine (IL-2, IL-4, IFNγ) expression [34–36]. Generation of the natural T regulatory cells involves CD28, CD40L, and LFA-1 expression on the precursor T cells and CD80, CD86, CD40 and ICAM-1 expression on thymic stroma [37]while IL-2, IL-7 and IL-15 maintain T regulatory cells in the periphery [32, 38]. In contrast to the natural T regulatory cells, inducible T regulatory cells arise in the periphery through antigen activation of naive CD4+ cells [39]. Naïve CD4+ cells stimulated in the presence of TGFβ differentiate into inducible T regulatory cells while naïve CD4+ cells stimulated in the presence of IL-6 and possibly IL-23 differentiate into Th17 cells [39, 40]. IL-23 may not be required for the differentiation of Th17 cells but may be necessary for Th17 cell survival [41]. Th17 cells express retinoic acid orphan receptor-γt transcription factor, IL-17A, IL-17F and IL-22 and increase expression of IL-1, IL-6 and G-CSF and enhance autoimmunity in both humans and animals [40]. Diseases associated with Th17 include rheumatoid arthritis and multiple sclerosis [42]. As with natural T regulatory cells, many inducible T regulatory cells express FoxP3 [31].
Natural T regulatory cells primarily suppress immunity through direct cell-cell contact using CTLA-4 or membrane bound TGFβ [32, 43]. Inducible T regulatory cells can suppress immunity by CTLA-4 as in natural T regulatory cells or through production of IL-10 or TGFβ. T regulatory cells can also inhibit effector T cell responses through metabolic disruption or killing of T cells, alteration of antigen presenting cell function, induction of indolamine 2,3-dioxygenase (IDO), and physical impedance of effector T cell interaction with antigen presenting cells [31].
T regulatory cells have a crucial role in determining myocarditis susceptibility to coxsackievirus B3 infection [44, 45]. Reducing CD80 expression on mast cells and macrophage in virus infected mice results in decreases in CTLA-4 expression and T regulatory cell numbers with subsequent increases in cardiac inflammation [44]. Furthermore, the relative ability of coxsackievirus variants to induce T regulatory cells may be pivotal in whether the infections are pathogenic or non-pathogenic. Studies from this laboratory using two coxsackievirus B3 variants which differ by a single nonconserved amino acid in the VP2 capsid protein [46] show that the non-pathogenic variant induces a potent T regulatory cell (CD4+CD25+FoxP3+) response which is absent during infections with the pathogenic virus [45]. Similar results have been found in coxsackievirus B4 infection where induction of T regulatory cells prevents insulin dependent diabetes [47]. Cytokine responses during infection, involving either IL-13 [48] or TGFβ [47], promote T regulatory cell generation.
In infectious diseases, induction of T regulatory cells might be detrimental as suppression of anti-pathogen immunity could increase microbial replication and direct pathogen induced tissue injury. In this case, induction of T regulatory cells could lead to chronic infections while lack of a T regulatory cell response would allow rapid control and elimination of the infectious agent [49, 50]. However, in coxsackievirus infection, induction of T regulatory cells is not associated with chronic infection [45] [47]. Virus elimination occurs normally in animals having enhanced T regulatory cell responses even though immunopathogenic injury is ablated. In part, suppression of T cell immunity has minimal effect on acute picornavirus infections [51] because T-cell independent responses (including neutralizing antibody [52], RIG-1/MDA-5 helicases and type 1 interferons [53], and nitric oxide [54]) are highly effective in clearing the virus.
3. Antigenic mimicry
Another mechanism for infection induced autoimmunity is antigenic mimicry in which microbial and self-molecules share sufficient similarity to induce cross-reactive immunity [55–57]. Cross-reactive T cells or antibodies between microbes and self antigens are found in various autoimmune diseases including: ankylosing spondylitis, between HLA B27 and Krebsiella pneumonia [58, 59]; myasthenia gravis, between the acetylcholine receptor and herpes simplex virus [60]; type I diabetes, between glutamic acid decarboxylase and human cytomegalovirus [61]; rheumatic heart disease, between the M protein of group A streptococcus and cardiac myosin [62]; multiple sclerosis, between myelin basic protein and Epstein Barr Virus DNA polymerase [63]; and Sjogren’s syndrome, between the Ro60 kD autoantigen in salivary gland and hepatitis C virus [64]. Antigenic mimicry has been implicated between picornaviruses and self molecules in Sjogren’s syndrome [58, 59, 65–67] involving cross-reactivity between coxsackievirus and the Ro/SSA 60 kD autoantigen; in type 1 diabetes [68] between coxsackievirus and the glutamic acid decarboxylase (GAD65) autoantigen [64, 69, 70]; in myocarditis [71] between coxsackievirus and cardiac membrane proteins.
When cross-reactive antibodies but not T cells are observed [66, 72], mimicry probably involves the tertiary conformation of the antigens. In contrast, cross-reactive T cell clones [61] usually recognize similar primary amino acid sequences between microbes and self antigens since T cells respond to peptides presented by MHC molecules. Although one often is told that a single T cell clone responds to a specific epitope of 8-20 amino acids presented by a major histocompatibility complex (MHC) molecule [73], in fact, there is significant flexibility in the T cell receptor recognition of the epitope. Subtly altered peptides may partially or fully initiate T cell activation which may lead to cytokine production without T cell proliferation or to anergy [74–76]. Distinct structural characteristics of the epitope determine its ability to functionally interact with the TCR and stimulate immunity [77] so that of the 8-20 amino acids in the total peptide, only amino acids at specific positions will be determinative and substitution of other amino acids at these residues which are equivalent in size and/or polarity can stimulate the same T cell response. Thus, very limited sequence homology between the microbial and self antigens may be required for cross-reactivity [63, 74] increasing the probability for antigenic mimicry.
4. Cryptic epitopes
Cryptic epitopes are immunogenic peptides which are either not generated during normal antigen processing or generated at too low concentrations for effective T cell activation [78]. Low cryptic epitope generation during normal antigen processing may result from cleaving of proteins within potential cryptic epitopes by the proteases normally present in antigen presenting cells. Concentrations of cryptic epitopes might be augmented by increasing the amount of the self protein degraded. Although most cryptic epitopes will still be destroyed, sufficient amounts may escape to allow immune sensitization [78]. Virus-induced ubiquitination of self proteins in infected cells can lead to increased self molecule degradation such as occurs with coxsackieviruses that downregulate cellular cyclin D1 using the ubiquitin-proteosome pathway [79]. Low levels of cryptic epiotpes may also be made more antigenic by increasing efficiency of their presentation to T cells though up-regulation of major histocompatibility complex (MHC) and accessory molecules on antigen presenting cells or by release of pro-inflammatory cytokines required for T cell proliferation [78]. The types of proteases can also vary among distinct antigen presenting cells which might produce distinct peptide repertoires for T cell activation [80]. IFNγ and TNFα exposure alter protease expression in cells and may change the peptides produced [81]. Protein-protein interactions can affect antigen processing. For example, internalization of HIV-CD4 complexes results in cryptic epitope production of the CD4 molecule and autoreactivity [82, 83]. Similarly, antigen-antibody complexes might alter protease access to cleavage sites in antigens during antigen processing [84]. FcR up-take of immune complexes could deliver antigen to different compartments of the endosome pathway which may also alter antigen processing [85]. Finally, virus infections may cause cryptic epitopes generation in self proteins through the action of viral proteases. Many viruses, as well as other infectious agents, code for their own proteases which are necessary for processing of microbial proteins. For example, the picornavirus genome consists of a single strand RNA which contains 5′ and 3′ non-translated regions and a single open reading frame. The open reading frame is translated into a single polyprotein which is processed by viral proteases into at least 11 proteins. Picornavirus proteases not only cleave the viral polyprotein, but also degrade the host eukaryotic initiation factor 4G (eIF-4G) which disrupts the cellular p220 protein cap-dependent binding complex and results in the shutdown of cap-dependent host protein synthesis [86]. This is an important adaptation by the virus which allows it to shut down host cell protein synthesis for maximum progeny virus production. Viral proteases additionally cleave cellular proteins not required for virus replication such as dystrophin, a contractile protein in myocytes [87]. Cleavage of dystrophin itself could result in cardiomyopathy [87], but it is also likely that the viral protease cleaves dystrophin differently than cellular proteases and this could result in cryptic epitope generation.
5. Adjuvants and autoimmunity
Adjuvants are compounds which, when concurrently administered with antigen, substantially enhance the immune response to that antigen [88, 89]. The crucial aspect of a good adjuvant is to rapidly activate the innate immune system to prime antigen presenting cells for antigen up-take, maturation and optimal antigen presentation to the adaptive immune system along with elicitation of pro-inflammatory cytokines [90]. Often, this employs use of microbial components in the adjuvant, such as Mycobacterium, which activate the innate immune system through toll-like receptors (TLR). TLR are type I integral membrane glycoproteins which have extracellular domains with variable numbers of leucine-rich repeat (LRR) motifs and conserved intracellular domains with a homologous Toll/interleukin (IL)-1 response domain [91, 92]. There are 12 TLR in humans and mice which react to different molecular species[41, 91, 93–96]. TLR are pattern recognition receptors (PRR), cellular molecules which recognize pathogen-associated molecular patterns (PAMPs). PAMPs are conserved microbial molecules shared by a diverse population of pathogens and are probably required for microbial infection or replication [91]. The ability of an individual to recognize PAMPs allows a very rapid host response to infection without requiring specificity of the response to a particular infectious agent. TLRs can be expressed either individually or as heterodimers (TLR1/TLR6, TLR1/TLR2 or TLR2/TLR6) [91–93]; and different cells express distinct sets of TLR. For example, plasmacytoid dendritic cells express TLR7 and TLR9 but not TLR3; monocyte-derived dendritic cells express TLR3 but not TLRs7 and 9; CD8+ cells express high levels of TLR3 but very low levels of TLR2 and TLR4; and B cells express high levels of TLR9 and TLR10 [93, 97, 98]. However, TLR expression and functionality is dynamic and can change with the activation state of the cell. TLR2 and TLR4 mRNA and intracellular protein are expressed by naïve CD4+ cells but these TLR proteins are not present on the plasma membrane. After activation, CD4+ cells rapidly express cell-surface TLR2 and TLR4, but only the TLR2 may be functional resulting in IFNγ, IL-2 and TNFα expression [99]. Evidence indicates that both the type and intensity of signal transduction through specific TLRs determine the nature of the adaptive immune response that they promote. TLRs 3, 4, 5 and 9 preferentially activate Th1 responses while TLR2 preferentially induces Th2 immunity [98]. Similarly, while low dose LPS stimulation of TLR4 promotes Th2 response, higher doses of LPS promote Th1 responses. This means that distinct lymphoid cell populations will respond differently in infections depending upon both the TLR ligand(s) of the invading organism and the TLR subsets expressed by the responding lymphoid cells.
Many experimental diseases can be induced either through injection of mice with TLR activating molecules such as double stranded RNA or lipopolysaccharide alone (hepatitis) [100]; or, more often through injection of tissue homogenates/proteins in adjuvant (experimental allergic encephalitis; thyroiditis, myocarditis) [101–103]. This strongly implicates an adjuvant role in induction of various tissue specific autoimmune diseases, at least experimentally, and provides strong circumstantial evidence that a major role for viruses and other microbes in autoimmunity induction is their ability to stimulate strong TLR signals. Infections are often implicated in the induction of autoimmune diseases but the mechanism(s) by which infection results in autoimmunity are controversial [57, 104]. Although the concept of antigenic mimicry has been around for decade, the definitive evidence that this plays a decisive role in autoimmune diseases is still lacking. However, recent studies in coxsackievirus B3 induced myocarditis have shown that TLR4 deficient mice develop significantly less myocarditis demonstrating a pivotal role for TLR signaling in this viral induced disease ([105]; reviewed by Rose [104]). One question might be why TLR4 should be important in coxsackievirus B3 induced myocarditis when this virus is non-enveloped and would therefore lack the classical TLR4 ligand, lipopolysaccharide. However, it is now clear that coxsackievirus proteins can directly bind and activate TLR4 [106]. Also, it is now known that endogenous as well as microbial ligands can activate TLR and that the endogenous ligands may act as “danger” signals to the innate immune system [107–110]. Cardiac myosin has recently been shown to activate TLR2 and to cause cardiac inflammation [110–112]. Furthermore, coxsackievirus infection increases TLR2, 7 and 8 mRNA expression [113]. Since coxsackievirus B3 is lysogenic, it is reasonable to assume that virus-induced death of cardiac myocytes results in release of cardiac myosin peptides and potential activation of TLR2 through this endogenous ligand.
TLR signal transduction can either positively or negatively affect T regulatory cell activity. TLR8-MyD88 signaling suppresses T regulatory cell function, while TLR2 and TLR5 both increase T regulatory cell numbers and activity [41, 114, 115]. How TLR signaling modulates T regulatory cells is complex, but most likely results via alterations in dendritic cell cytokine or accessory molecule expression [116, 117]. Activation of NFkB and production of pro-inflammatory cytokines (IL-1β and TNFα) subsequent to TLR signaling may be crucial in inducing autoimmunity through the effects of these cytokines on antigen presenting cells or directly on T regulatory cells [118, 119]. IL-1β and TNFα promote dendritic cell maturation and migration and also up-regulate expression of CD80 and CD86 [118]. While these effects should enhance immunogenicity of self antigens and promote autoimmunity, they may also alter T regulatory cells. Mice lacking CD80, CD86 and CD40 have fewer T regulatory cells than wild-type mice [115]. Therefore, one might expect that IL-1β and TNFα should enhance T regulatory cell responses because these cytokines increase CD80/CD86 expression. However, TNFα directly interacts with T regulatory cells independent of antigen presenting cells and suppresses their function in hepatitis B virus infections [119]. In contrast to TNFα, IL-2, IL-4 and IL-7, which are also generated from TLR activation, strengthen the T regulatory response [34, 117]. In addition to effects mediated through cytokines, direct TLR signaling in T regulatory cells could modulate immunosuppression [114]. Human T regulatory cells express TLR4, 5 and 8 and do not express TLR7. Other TLR have not been determined. Mouse T regulatory cells express TLR1, 2, 4, 5, 6, 7, and 8 but not TLR3 or 9 [114, 120].
SEX AND PICORNAVIRUS-INDUCED AUTOIMMUNITY
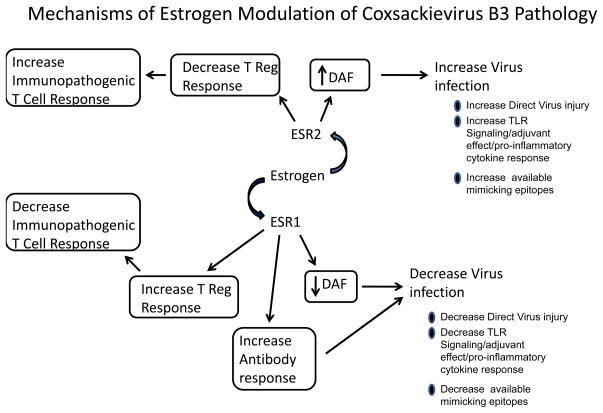
Females are often less susceptible to viral infections than males. This is true for a wide range of viruses including picornaviruses (coxsackievirus, Theiler’s virus, encephalomyocarditis virus), Herpes Simplex virus type 1, HIV, hantaviruses, VSV, and West Nile Virus (see [121]). The reasons why females are less susceptible are complex but most likely relate to the enhanced immune responses occurring in this sex. Estrogen modulates both innate and adaptive immunity. Although some effects of estrogen on immunity are controversial, the following are generally accepted: increasing immunoglobulin synthesis[122]; suppressing both T and B cell lymphopoiesis [123]; enhancing dendritic cell differentiation and antigen presentation[124]; suppressing TNFα and IL-6 expression [125, 126] while increasing IL-4 and IFNγ production [127, 128]; inhibiting B cell apoptosis[129]; and promoting FoxP3+ T regulatory cell development [130–132]. The effects of estrogen on immune responses and cytokine expression can be controversial. Although the majority of studies indicate that estrogen increases IFNγ expression, there are several reports that estrogen either has no effect on IFNγ [127] or decreases its expression [133]. In coxsackievirus B3 infections, estrogen suppresses IFNγ and Th1 responses while promoting IL-4 and Th2 responses [134]. The reason for the divergent effect of estrogen on IFNγ induction during coxsackievirus B3 infection relates to the suppressive effects of this hormone on the virus receptor (discussed below) which restricts virus infection and replication and therefore indirectly affects cytokine and immune responses (see Figure 1). In this case, the effect of estrogen on the immune response becomes secondary to its effects on virus infection.
Figure 1.
Effects of estrogen on innate and adaptive immune responses. Estrogen signals through two receptors (ESR1 and ESR2). ESR1 suppresses expression of one of the two known coxsackievirus B3 receptors, decay accelerating factor (DAF) which will restrict virus infection and replication. Lower virus loads will result in less direct virus mediated injury by reducing numbers of infected cells and will also reduce Toll-like receptor (TLR) signaling which will restrict pro-inflammatory cytokine expression. Reduced virus loads will also decrease the amount of viral epitopes which mimic self molecules and thus prevent induction of autoimmunity through this mechanism. ESR1 also promotes antibody responses and increased virus neutralizing antibody will further inhibit virus infection. Finally signaling through ESR1 promotes T regulatory cell responses which will further suppress immunopathogenic T cell activation. ESR2 has the opposite effects of ESR1 as signaling through this receptor increases virus receptor expression/virus infection and suppresses T regulatory cell response.
Part of the complexity associated with estrogen in viral infections is that this hormone alters both nuclear and non-nuclear signal pathways. There are two known estrogen receptors (ESR1 and ESR2) which bind with equivalent specificity and affinity to estrogen response elements (ERE) in gene promoter regions leading to modulation of gene expression [135]. ESR1 (also known as ERα) and ESR2 (also known as ERβ) have wide tissue distribution with ESR1 primarily found in the uterus, liver, kidney and heart while ESR2 is primarily found in ovary prostate, lung, central nervous system, gastrointestinal tract, and bladder. Lymphocytes, macrophage and dendritic cells co-express both ESR1 and ESR2 [136] but ESR1 primarily controls estrogen modulation of dendritic cell maturation, T cell cytokine production and immunoglobulin response [126, 127, 137, 138]. In contrast, signaling through ESR2 up-regulates inducible nitric oxide synthetase (iNOS) and nitric oxide generation while ESR1 suppresses this response [139]. Several important studies now show that where ESR1 and ESR2 are co-expressed in the same cell, these receptors may exert opposing effects on gene expression and thus counter-balance each other [133, 135]. Since there is clearly differential tissue distribution of the nuclear receptors, it is quite possible for estrogen to have divergent effects depending upon where a virus infection occurs. For example, since ESR1 is more prevalent in heart while ESR2 is more prevent in lung [135], one might expect different estrogen effects in cardiotropic coxsackievirus infection than in influenza virus infections which are restricted to the respiratory tract. Although the genomic effects of estrogen receptors have been most extensively studied, it is now clear that ESR1 can also translocate from the nucleus to the plasma membrane resulting in modulation of intracellular calcium flux and activation of both the MAPK/ERK and PI3K/AKT pathways. Both ESR1 and ESR2 can also bind to mitochondria DNA and modulate mitochondrial respiratory complexes and production of reactive oxygen species [140].
For some viruses and specifically for coxsackieviruses, estrogens can directly affect virus infection and replication independent of its effects on immunity. Viruses use cell surface molecules for attachment to cells and initiation of the infection cycle. At least some molecules used as virus receptors are under estrogen control. These include CXCR4 which can act as a co-receptor for HIV; αvβ3 integrin which acts as a receptor/co-receptor for adenovirus, coxsackievirus A9 and hantavirus [141–145]; and decay accelerating factor (DAF; CD55) which is one of the two known receptors for coxsackieviruses. The other known receptor is coxsackievirus-adenovirus receptor (CAR) [146–148]. Although most coxsackieviruses use both CAR and DAF for optimal infection [149], CAR appears to be the dominant receptor and can lead to infection of cells in tissue culture with little or no DAF involvement [150]. In vivo, receptor usage is more complex and may depend upon the type of cell or tissue infected. Chimeric fusion proteins (DAF-Fc and CAR-Fc) are highly effective in inhibiting coxsackievirus infection in the heart but CAR-Fc alone prevents virus infection of the pancreas indicating that both receptors are required for optimal cardiac infection whereas DAF is not important for infection of the pancreas in the same infected animal [147, 151, 152]. Studies using DAF knockout mice confirm that this receptor is important for myocarditis but not pancreatitis [153]. DAF expression is enhanced by estrogen treatment in a tissue specific manner [154], but only recently has it been shown that ESR1 and ESR2 have opposite effects on DAF expression. ESR1 suppresses and ESR2 increases DAF on lymphoid cells. Increased DAF also correlates to enhanced susceptibility to develop myocarditis (Huber, manuscript in preparation) [155]. The effect of estrogen on DAF expression seems at odds with the resistance of females to coxsackievirus B3 induced myocarditis [155]. The primary function of DAF is to inactivate the C3 component of complement and protect cells from complement mediated lysis [156]. However, DAF has been shown to suppress T cell responses during allogaft rejection [157] and depletion of DAF can promote autoimmunity [158]. The mechanism by which DAF suppresses T cell immunity is not well understood although it apparently requires complement, the natural ligand of DAF. It is not clear whether estrogen also increases CAR expression, although this is quite possible since estrogen inhibits TNFα responses and TNFα and IFNγ both suppress CAR expression [159]. What direct effects modulation of CAR expression might have on innate or adaptive immunity is not clear. However, CAR is a junction adhesion molecule (JAM), proteins which are located in tight junctions and are essential in structural stability of the junction [160, 161]. In addition, JAMs are involved in leukocyte transmigration through endothelial barriers. When endothelial cells are exposed to cytokines, JAMs re-distribute outside of tight junctions and bind to specific leukocytes enabling their transmigration [160]. Since CAR binds immunoglobulin [162], it is probable that this tight junction molecule promotes B cell transmigration. Increasing CAR expression could reinforce tight junction stability and inhibit B cell transmigration into underlying tissues; both effects would result in reduced inflammation.
Substantial evidence indicates that tissue injury in picornavirus infections results from immunopathogenic mechanisms rather than from direct virus induced killing of infected cells. T cell depletion of mice prevents myocarditis, diabetes and demyelinization in coxsackievirus B3 [51], encephalomyocarditis virus [163], and Theiler’s virus [164, 165] infections. In coxsackievirus B3 infections, cytolytic CD8+ T cells reactive to myocyte antigens are the primary mediators of cardiac injury [166–168]. With coxsackievirus induced myocarditis, the basis of the autoimmune response appears to be antigenic mimicry between the virus and cardiac proteins including cardiac myosin [3, 71, 169]. However, the existence of mimicking epitopes is not sufficient for induction of autoimmunity. Variants of coxsackievirus B3 which contain functional mimicking epitopes may not generate autoimmunity unless T regulatory cell responses are prohibited. As indicated above, coxsackievirus B3 infection of female mice fails to generate autoimmunity while male mice are highly susceptible [170, 171]. Sex associated hormones control cardiac pathology since castration of males is protective while restoration of testosterone increases susceptibility [29, 170, 172, 173]. Furthermore, treating male mice with 17-β-estradiol significantly suppresses myocarditis while treatment of females with androgen enhances myocarditis [171]. Estrogen protects against coxsackievirus B3 induced myocarditis and autoimmunity by multiple mechanisms. As discussed above, reduction in virus receptor expression would limit virus load and consequently activation of innate and adaptive immunity. A second mechanism for protection results from the ability of estrogen to promote CD4+CD25+ FoxP3+ T regulatory cell response [45, 174]. In the CVB3 induced myocarditis model, signaling through the ESR1 is responsible for T regulatory cell response while signaling through ESR2 inhibits T regulatory cell activation (Huber manuscript submitted). This observation is consistent with previous published reports showing the same phenomenon [132, 175].
The mechanism(s) for enhanced T regulatory response in females could be quite complex. One possibility might be an inherent increase in FoxP3 expression in females. Mice either lacking FoxP3 or having mutated forms of this transcription factor are highly susceptible to autoimmunity [176]. Although FoxP3 is located on the X chromosome [33], it is unknown whether females inherently express more of this transcription factor than males because of X chromosome inactivation. In placental mammals, the X inactivation center located on the X chromosome contains an Xist RNA gene which triggers chromosome wide gene repression and maintains gene dose balance between males and females [177]. Some genes escape X inactivation [178]. The number of X chromosome genes which escape is not clear but may be as few as 5% of the genes on this chromosome [179]. Whether FoxP3 is one of the few X-linked genes which escapes inactivation and may therefore be expressed at higher levels in females is not known. More likely epigenetic control of FoxP3 expression is more important in T regulatory cell responses. The FoxP3 gene contains 11 coding and 3 non-coding exons, and intronic enhancer, proximal promoter and upstream enhancer region [180]. Various extracellular and intracellular signals modulate FoxP3 expression with TGFβ, IL-2 and IFNγ promoting expression and interferon regulatory factor 1 (IRF-1), IL-6 and IL-4 suppressing expression. In many cases control of FoxP3 transcription depends upon CpG methylation of specific sites in the promoter and intronic enhancer regions. For example, IL-6 induces methylation of FoxP3 through STAT3 dependent mechanisms resulting in suppressed FoxP3 expression. Fully demethylated FoxP3 as found in natural T regulatory cells can result in stable suppressive activity. In contrast, adaptive peripheral T regulatory cells can be more readily re-methylated at the FoxP3 gene leading to loss of suppressive function. Estrogen increases expression of both TGFβ and IFNγ [181] while decreasing expression of IL-6 [182]. Thus, estrogen both provides extracellular stimuli which promote FoxP3 transcription and eliminates Il-6 dependent methylation of the FoxP3 gene.
CONCLUSION
Viruses, and other microbial infections, have long been associated with autoimmune diseases. Infections can promote autoimmunity through multiple mechanisms and most likely, different mechanisms will be involved with different viruses. In coxsackievirus B3 infections, autoimmunity is the major pathogenic response causing myocarditis. The basis of the autoimmunity is antigenic mimicry between the virus and cardiac proteins, but this antigenic mimicry alone is insufficient for autoimmunity to develop. Environmental factors must be conducive to autoimmune stimulation. These environmental factors include activation of innate immunity, most likely with a strong involvement of toll-like receptor signal transduction, and inhibition of T regulatory cell activation. Although natural T regulatory cells are constitutively present, a potent pro-inflammatory environment could readily negate their immunosuppressive effect and allow autoimmunity induction. Similarly, conditions which strongly favor T regulatory responses might prevent autoimmunity in the face of innate activation. A major difference between males and females infected with coxsackievirus B3 is that the females generate T regulatory cells subsequent to infection which the males lack. The failure of males to develop T regulatory cells probably results first from the potent TNFα and IL-6 responses induced in this sex, both cytokines suppress T regulatory cells. Secondly, increased TGFβ expression in females would promote T regulatory cell development. A second method in which females could suppress immunopathogenic responses is through estrogen induced increases in DAF expression. The role of DAF in coxsackievirus B3 infections is likely to be highly complex as DAF is not only capable of modulating T cell responses but is also one of the known receptors of coxsackievirus B3. Total lack of DAF expression in the heart prevents optimal virus infection of this organ. However, signaling through DAF on T lymphocytes is immunosuppressive. This means that low level expression of DAF should promote coxsackievirus B3 induced myocarditis by allowing virus infection of the cardiac myocytes but that substantial increases in DAF expression caused by estrogen should be immunosuppressive and prevent immunopathogenic, T cell-dependent cardiac injury.
TLRs undoubtedly play a central role in coxsackievirus B3 pathogenicity. Their role is most likely multifactorial as they would promote activation of the autoimmune T cells and simultaneously suppress T regulatory cell responses through production of TNFα and IL-6. Although this investigator has only identified autoimmune T cells which react to mimicking epitopes between coxsackievirus B3 and cardiac antigens, signaling through TLR should also promote autoimmunity to self antigens released during virus induced death of infected cardiocytes in what has been termed an “adjuvant effect”. Similarly, it is very reasonable to assume that cryptic epitope induced autoimmunity could be important in coxsackievirus immunopathology. Although multiple mechanisms for the generation of cryptic epiotpes have been postulated, it seems that a highly probable mechanism, production of unique sets of peptides through microbial protease cleavage of self proteins during infection, is rarely, if ever discussed. The ability of coxsackieviral proteases to efficiently cleave self proteins is well known and it seems probable that viral protease cleavage sites could differ from those of endogenous cellular proteases. Considering the substantial amount of virus protein production, significant levels of cryptic peptides should result during viral replication in cardiocytes. The cryptic epitopes, coupled with the adjuvant effect of infection, should be a potent engine for activation of autoimmune T cells. In infections which fail to induce autoimmunity, presumably factors such as induction of immunosuppressive cytokines, modulation of antigen presenting cells, or induction of T regulatory cells prevent the autoimmune response from occurring.
Future Prospective.
Virus induced autoimmunity clearly occurs both clinically and in experimental disease models. The mechanisms for autoimmunity induction are highly controversial, however, with different investigators proposing various mechanisms even for the same virus. Thus, for coxsackievirus B3, distinct investigators have forwarded adjuvant effect, cryptic epitope and antigenic mimicry as the primary method for eliciting autoimmune responses. In fact, all of these mechanisms can lead to autoimmune T cell activation, but none of these processes will result in autoimmune disease, unless immunosuppression is eliminated. Clinically, understanding how to restore T regulatory cell responses in patients with post-infectious autoimmunity/immunopathology may be more beneficial than specifically defining how activation of autoimmune T cells occurred in the first place. Mechanisms for promoting or eliminating T regulatory cells will differ dramatically depending upon the characteristics of the virus infection and host response to infection. Because different viruses can induce distinct innate responses, it is reasonable to assume that specific conditions favoring immunosuppression in one infection may not exist in another infection. In coxsackievirus B3 infection of mice, sex is a crucial factor promoting T regulatory cell activation but the processes leading to T regulatory cell response are not understood. A major area for future investigation will be to define how why some viruses induce autoimmunity while others do not.
Executive summary.
Infections can stimulate auto-reactive T cell clones by a number of different mechanisms
More than one mechanism for activating auto-reactive T cells may occur in any specific infection
Activating auto-reactive T cells is not sufficient to produce autoimmune disease, however. Elimination of immunosuppression (T regulatory cells) is a necessary element in autoimmunity.
Unlike most autoimmune diseases (SLE, rheumatoid arthritis, Grave’s disease) which predominate in females, autoimmunity subsequent to picornaviruses predominates in males. The reason for this is that estrogen promotes T regulatory cell responses.
Estrogen most likely suppresses immunoregulation by inhibiting IL-6 and TNFα production, both of which prevent FoxP3 expression.
References
- 1.Munz C, Lunemann Jd, Getts Mt, Miller Sd. Antiviral immune responses: Triggers of or triggered by autoimmunity? Nat Rev Immunol. 2009;9(4):246–258. doi: 10.1038/nri2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldberg E, Krause I. Infection and type 1 diabetes mellitus - a two edged sword? Autoimmunity reviews. 2009;8(8):682–686. doi: 10.1016/j.autrev.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 3.Root-Bernstein R, Vonck J, Podufaly A. Antigenic complementarity between coxsackie virus and streptococcus in the induction of rheumatic heart disease and autoimmune myocarditis. Autoimmunity. 2009;42(1):1–16. doi: 10.1080/08916930802208540. [DOI] [PubMed] [Google Scholar]
- 4.Fairweather D, Kaya Z, Shellam Gr, Lawson Cm, Rose Nr. From infection to autoimmunity. J Autoimmun. 2001;16(3):175–186. doi: 10.1006/jaut.2000.0492. [DOI] [PubMed] [Google Scholar]
- 5.Pohl D. Epstein-barr virus and multiple sclerosis. J Neurol Sci. 2009;286(1–2):62–64. doi: 10.1016/j.jns.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 6.Doria A, Canova M, Tonon M, et al. Infections as triggers and complications of systemic lupus erythematosus. Autoimmunity reviews. 2008;8(1):24–28. doi: 10.1016/j.autrev.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 7.Horwitz M, Sarvetnick N. Viruses, host responses, and autoimmunity. Immunol Rev. 1999;169:241–253. doi: 10.1111/j.1600-065X.1999.tb01319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Savino W. The thymus is a common target organ in infectious diseases. PLoS pathogens. 2006;2(6):e62. doi: 10.1371/journal.ppat.0020062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D, Muller N, Mcpherson Kg, Reichardt Hm. Glucocorticoids engage different signal transduction pathways to induce apoptosis in thymocytes and mature t cells. J Immunol. 2006;176(3):1695–1702. doi: 10.4049/jimmunol.176.3.1695. [DOI] [PubMed] [Google Scholar]
- 10.Matteucci D, Toniolo A, Conaldi Pg, Basolo F, Gori Z, Bendinelli M. Systemic lymphoid atrophy in coxsackievirus b3-infected mice: Effects of virus and immunopotentiating agents. J Infect Dis. 1985;151(6):1100–1108. doi: 10.1093/infdis/151.6.1100. [DOI] [PubMed] [Google Scholar]
- 11.D’souza Wn, Lefrancois L. Frontline: An in-depth evaluation of the production of il-2 by antigen-specific cd8 t cells in vivo. Eur J Immunol. 2004;34(11):2977–2985. doi: 10.1002/eji.200425485. [DOI] [PubMed] [Google Scholar]
- 12.Saibil Sd, Deenick Ek, Ohashi Ps. The sound of silence: Modulating anergy in t lymphocytes. Curr Opin Immunol. 2007;19(6):658–664. doi: 10.1016/j.coi.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Adler Hs, Steinbrink K. Map kinase p38 and its relation to t cell anergy and suppressor function of regulatory t cells. Cell Cycle. 2008;7(2):169–170. doi: 10.4161/cc.7.2.5312. [DOI] [PubMed] [Google Scholar]
- 14.Wells Ad. New insights into the molecular basis of t cell anergy: Anergy factors, avoidance sensors, and epigenetic imprinting. J Immunol. 2009;182(12):7331–7341. doi: 10.4049/jimmunol.0803917. [DOI] [PubMed] [Google Scholar]
- 15.Boussiotis Va, Freeman Gj, Taylor Pa, et al. P27kip1 functions as an anergy factor inhibiting interleukin 2 transcription and clonal expansion of alloreactive human and mouse helper t lymphocytes. Nat Med. 2000;6(3):290–297. doi: 10.1038/73144. [DOI] [PubMed] [Google Scholar]
- 16.Wells Ad, Walsh Mc, Sankaran D, Turka La. T cell effector function and anergy avoidance are quantitatively linked to cell division. J Immunol. 2000;165(5):2432–2443. doi: 10.4049/jimmunol.165.5.2432. [DOI] [PubMed] [Google Scholar]
- 17.Li L, Iwamoto Y, Berezovskaya A, Boussiotis Va. A pathway regulated by cell cycle inhibitor p27kip1 and checkpoint inhibitor smad3 is involved in the induction of t cell tolerance. Nat Immunol. 2006;7(11):1157–1165. doi: 10.1038/ni1398. [DOI] [PubMed] [Google Scholar]
- 18.Zheng Y, Delgoffe Gm, Meyer Cf, Chan W, Powell Jd. Anergic t cells are metabolically anergic. J Immunol. 2009;183(10):6095–6101. doi: 10.4049/jimmunol.0803510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Riley Jl. Pd-1 signaling in primary t cells. Immunol Rev. 2009;229(1):114–125. doi: 10.1111/j.1600-065X.2009.00767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chikuma S, Terawaki S, Hayashi T, et al. Pd-1-mediated suppression of il-2 production induces cd8+ t cell anergy in vivo. J Immunol. 2009;182(11):6682–6689. doi: 10.4049/jimmunol.0900080. [DOI] [PubMed] [Google Scholar]
- 21.Grabie N, Gotsman I, Dacosta R, et al. Endothelial programmed death-1 ligand 1 (pd-l1) regulates cd8+ t-cell mediated injury in the heart. Circulation. 2007;116(18):2062–2071. doi: 10.1161/CIRCULATIONAHA.107.709360. [DOI] [PubMed] [Google Scholar]
- 22.Lucas Ja, Menke J, Rabacal Wa, Schoen Fj, Sharpe Ah, Kelley Vr. Programmed death ligand 1 regulates a critical checkpoint for autoimmune myocarditis and pneumonitis in mrl mice. J Immunol. 2008;181(4):2513–2521. doi: 10.4049/jimmunol.181.4.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seko Y, Yagita H, Okumura K, Azuma M, Nagai R. Roles of programmed death-1 (pd-1)/pd-1 ligands pathway in the development of murine acute myocarditis caused by coxsackievirus b3. Cardiovasc Res. 2007;75(1):158–167. doi: 10.1016/j.cardiores.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Si X, Luo H, Morgan A, et al. Stress-activated protein kinases are involved in coxsackievirus b3 viral progeny release. J Virol. 2005;79(22):13875–13881. doi: 10.1128/JVI.79.22.13875-13881.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luo H, Yanagawa B, Zhang J, et al. Coxsackievirus b3 replication is reduced by inhibition of the extracellular signal-regulated kinase (erk) signaling pathway. J Virol. 2002;76(7):3365–3373. doi: 10.1128/JVI.76.7.3365-3373.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Triantafilou K, Triantafilou M. Lipid-raft-dependent coxsackievirus b4 internalization and rapid targeting to the golgi. Virology. 2004;326(1):6–19. doi: 10.1016/j.virol.2004.04.051. [DOI] [PubMed] [Google Scholar]
- 27.Triantafilou K, Triantafilou M. Lipid raft microdomains: Key sites for coxsackievirus a9 infectious cycle. Virology. 2003;317(1):128–135. doi: 10.1016/j.virol.2003.08.036. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz Rh. T cell anergy. Annu Rev Immunol. 2003;21:305–334. doi: 10.1146/annurev.immunol.21.120601.141110. [DOI] [PubMed] [Google Scholar]
- 29.Huber S, Polgar J, Schultheiss P, Schwimmbeck P. Augmentation of pathogenesis of coxsackievirus b3 infections in mice by exogenous administration of interleukin-1 and interleukin-2. J Virol. 1994;68:195–206. doi: 10.1128/jvi.68.1.195-206.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suzuki M, Konya C, Goronzy Jj, Weyand Cm. Inhibitory cd8+ t cells in autoimmune disease. Hum Immunol. 2008;69(11):781–789. doi: 10.1016/j.humimm.2008.08.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mellanby Rj, Thomas Dc, Lamb J. Role of regulatory t-cells in autoimmunity. Clin Sci (Lond) 2009;116(8):639–649. doi: 10.1042/CS20080200. [DOI] [PubMed] [Google Scholar]
- 32.Wing K, Sakaguchi S. Regulatory t cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol. 11(1):7–13. doi: 10.1038/ni.1818. [DOI] [PubMed] [Google Scholar]
- 33.Zheng Y, Rudensky Ay. Foxp3 in control of the regulatory t cell lineage. Nat Immunol. 2007;8(5):457–462. doi: 10.1038/ni1455. [DOI] [PubMed] [Google Scholar]
- 34.Thornton Am, Piccirillo Ca, Shevach Em. Activation requirements for the induction of cd4+cd25+ t cell suppressor function. Eur J Immunol. 2004;34(2):366–376. doi: 10.1002/eji.200324455. [DOI] [PubMed] [Google Scholar]
- 35.Rudensky Ay, Gavin M, Zheng Y. Foxp3 and nfat: Partners in tolerance. Cell. 2006;126(2):253–256. doi: 10.1016/j.cell.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Torgerson Tr, Genin A, Chen C, et al. Foxp3 inhibits activation-induced nfat2 expression in t cells thereby limiting effector cytokine expression. J Immunol. 2009;183(2):907–915. doi: 10.4049/jimmunol.0800216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sakaguchi S. Naturally arising foxp3-expressing cd25+cd4+ regulatory t cells in immunological tolerance to self and non-self. Nat Immunol. 2005;6(4):345–352. doi: 10.1038/ni1178. [DOI] [PubMed] [Google Scholar]
- 38.Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory t cells and immune tolerance. Cell. 2008;133(5):775–787. doi: 10.1016/j.cell.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 39.Weaver Ct, Hatton Rd. Interplay between the th17 and treg cell lineages: A (co-)evolutionary perspective. Nat Rev Immunol. 2009;9(12):883–889. doi: 10.1038/nri2660. [DOI] [PubMed] [Google Scholar]
- 40.Peck A, Mellins Ed. Breaking old paradigms: Th17 cells in autoimmune arthritis. Clin Immunol. 2009;132(3):295–304. doi: 10.1016/j.clim.2009.03.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Rf, Miyahara Y, Wang Hy. Toll-like receptors and immune regulation: Implications for cancer therapy. Oncogene. 2008;27(2):181–189. doi: 10.1038/sj.onc.1210906. [DOI] [PubMed] [Google Scholar]
- 42.Crome Sq, Wang Ay, Levings Mk. Translational mini-review series on th17 cells: Function and regulation of human t helper 17 cells in health and disease. Clin Exp Immunol. 159(2):109–119. doi: 10.1111/j.1365-2249.2009.04037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oida T, Xu L, Weiner Hl, Kitani A, Strober W. Tgf-beta-mediated suppression by cd4+cd25+ t cells is facilitated by ctla-4 signaling. J Immunol. 2006;177(4):2331–2339. doi: 10.4049/jimmunol.177.4.2331. [DOI] [PubMed] [Google Scholar]
- 44.Frisancho-Kiss S, Nyland Jf, Davis Se, et al. Cutting edge: T cell ig mucin-3 reduces inflammatory heart disease by increasing ctla-4 during innate immunity. J Immunol. 2006;176(11):6411–6415. doi: 10.4049/jimmunol.176.11.6411. [DOI] [PubMed] [Google Scholar]
- 45.Huber Sa, Feldman Am, Sartini D. Coxsackievirus b3 induces t regulatory cells, which inhibit cardiomyopathy in tumor necrosis factor-alpha transgenic mice. Circ Res. 2006;99(10):1109–1116. doi: 10.1161/01.RES.0000249405.13536.49. [DOI] [PubMed] [Google Scholar]
- 46.Knowlton Ku, Jeon Es, Berkley N, Wessely R, Huber S. A mutation in the puff region of vp2 attenuates the myocarditic phenotype of an infectious cdna of the woodruff variant of coxsackievirus b3. J Virol. 1996;70(11):7811–7818. doi: 10.1128/jvi.70.11.7811-7818.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richer Mj, Straka N, Fang D, Shanina I, Horwitz Ms. Regulatory t-cells protect from type 1 diabetes after induction by coxsackievirus infection in the context of transforming growth factor-beta. Diabetes. 2008;57(5):1302–1311. doi: 10.2337/db07-1460. [DOI] [PubMed] [Google Scholar]
- 48.Cihakova D, Barin Jg, Afanasyeva M, et al. Interleukin-13 protects against experimental autoimmune myocarditis by regulating macrophage differentiation. Am J Pathol. 2008;172(5):1195–1208. doi: 10.2353/ajpath.2008.070207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taylor Bc, Zaph C, Troy Ae, et al. Tslp regulates intestinal immunity and inflammation in mouse models of helminth infection and colitis. J Exp Med. 2009;206(3):655–667. doi: 10.1084/jem.20081499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Majlessi L, Lo-Man R, Leclerc C. Regulatory b and t cells in infections. Microbes Infect. 2008;10(9):1030–1035. doi: 10.1016/j.micinf.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 51.Woodruff J, Woodruff J. Involvement of t lymphocytes in the pathogenesis of coxsackievirus b3 heart disease. J Immunol. 1974;113:1726–1734. [PubMed] [Google Scholar]
- 52.Juleff N, Windsor M, Lefevre Ea, et al. Foot-and-mouth disease virus can induce a specific and rapid cd4+ t-cell-independent neutralizing and isotype class-switched antibody response in naive cattle. J Virol. 2009;83(8):3626–3636. doi: 10.1128/JVI.02613-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang Jp, Cerny A, Asher Dr, Kurt-Jones Ea, Bronson Rt, Finberg Rw. Mda5 and mavs mediate type i interferon responses to coxsackie b virus. J Virol. 84(1):254–260. doi: 10.1128/JVI.00631-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zaragoza C, Ocampo C, Saura M, et al. The role of inducible nitric oxide synthase in the host response to coxsackievirus myocarditis. Proc Natl Acad Sci U S A. 1998;95(5):2469–2474. doi: 10.1073/pnas.95.5.2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fujinami Rs, Oldstone Mb. Amino acid homology between the encephalitogenic site of myelin basic protein and virus: Mechanism for autoimmunity. Science. 1985;230(4729):1043–1045. doi: 10.1126/science.2414848. [DOI] [PubMed] [Google Scholar]
- 56.Fujinami Rs, Oldstone Mb. Molecular mimicry as a mechanism for virus-induced autoimmunity. Immunologic research. 1989;8(1):3–15. doi: 10.1007/BF02918552. [DOI] [PubMed] [Google Scholar]
- 57.Rose Nr, Mackay Ir. Molecular mimicry: A critical look at exemplary instances in human diseases. Cell Mol Life Sci. 2000;57(4):542–551. doi: 10.1007/PL00000716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Benoist C, Mathis D. Autoimmunity provoked by infection: How good is the case for t cell epitope mimicry? Nat Immunol. 2001;2(9):797–801. doi: 10.1038/ni0901-797. [DOI] [PubMed] [Google Scholar]
- 59.Stathopoulou Ea, Routsias Jg, Stea Ea, Moutsopoulos Hm, Tzioufas Ag. Cross-reaction between antibodies to the major epitope of ro60 kd autoantigen and a homologous peptide of coxsackie virus 2b protein. Clin Exp Immunol. 2005;141(1):148–154. doi: 10.1111/j.1365-2249.2005.02812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schwimmbeck Pl, Dyrberg T, Drachman Db, Oldstone Mb. Molecular mimicry and myasthenia gravis. An autoantigenic site of the acetylcholine receptor alpha-subunit that has biologic activity and reacts immunochemically with herpes simplex virus. J Clin Invest. 1989;84(4):1174–1180. doi: 10.1172/JCI114282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hiemstra Hs, Schloot Nc, Van Veelen Pa, et al. Cytomegalovirus in autoimmunity. T cell crossreactivity to viral antigen and autoantigen glutamic acid decarboxylase. Proc Natl Acad Sci U S A. 2001;98(7):3988–3991. doi: 10.1073/pnas.071050898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cunningham M, Hall N, Krisher K, Spanier A. A study of anti-group a streptococcal monoclonal antibodies crossreactive with myosin. J Immunol. 1986;136:293. [PubMed] [Google Scholar]
- 63.Wucherpfennig K, Strominger J. Molecular mimicry in t cell-mediated autoimmunity: Viral peptides activate human t cell clones specific for myelin basic protein. Cell. 1995;80:695–705. doi: 10.1016/0092-8674(95)90348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lonnrot M, Hyoty H, Knip M, et al. Antibody cross-reactivity induced by the homologous regions in glutamic acid decarboxylase (gad65) and 2c protein of coxsackievirus b4. Childhood diabetes in finland study group. Clin Exp Immunol. 1996;104(3):398–405. doi: 10.1046/j.1365-2249.1996.60771.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Triantafyllopoulou A, Moutsopoulos Hm. Autoimmunity and coxsackievirus infection in primary sjogren’s syndrome. Ann N Y Acad Sci. 2005;1050:389–396. doi: 10.1196/annals.1313.090. [DOI] [PubMed] [Google Scholar]
- 66.Triantafyllopoulou A, Tapinos N, Moutsopoulos Hm. Evidence for coxsackievirus infection in primary sjogren’s syndrome. Arthritis Rheum. 2004;50(9):2897–2902. doi: 10.1002/art.20463. [DOI] [PubMed] [Google Scholar]
- 67.Youinou P, Pers Jo, Saraux A, Pennec Yl. Viruses contribute to the development of sjogren’s syndrome. Clin Exp Immunol. 2005;141(1):19–20. doi: 10.1111/j.1365-2249.2005.02827.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elfaitouri A, Berg Ak, Frisk G, Yin H, Tuvemo T, Blomberg J. Recent enterovirus infection in type 1 diabetes: Evidence with a novel igm method. J Med Virol. 2007;79(12):1861–1867. doi: 10.1002/jmv.21008. [DOI] [PubMed] [Google Scholar]
- 69.Maclaren Nk, Alkinson Ma. Insulin-dependent diabetes mellitus: The hypothesis of molecular mimicry between islet cell antigens and microorganisms. Molecular medicine today. 1997;3(2):76–83. doi: 10.1016/s1357-4310(96)10056-3. [DOI] [PubMed] [Google Scholar]
- 70.Vreugdenhil Gr, Batstra Mr, Aanstoot Hj, Melchers Wj, Galama Jm. Analysis of antibody responses against coxsackie virus b4 protein 2c and the diabetes autoantigen gad(65) J Med Virol. 1999;59(2):256–261. [PubMed] [Google Scholar]
- 71.Maisch B, Bauer E, Cirsi M, Kocksiek K. Cytolytic cross-reactive antibodies directed against the cardiac membrane and viral proteins in coxsackievirus b3 and b4 myocarditis. Circulation. 1993;87(Suppl IV):49–65. [PubMed] [Google Scholar]
- 72.Maclaren N, Alkinson M. Insulin-dependent diabetes mellitus: The hypthesis of molecular mimicry between islet cell antigens and microorganisms. Molecular medicine today. 1997;3:76–83. doi: 10.1016/s1357-4310(96)10056-3. [DOI] [PubMed] [Google Scholar]
- 73.Babbitt Bp, Allen Pm, Matsueda G, Haber E, Unanue Er. Binding of immunogenic peptides to ia histocompatibility molecules. Nature. 1985;317(6035):359–361. doi: 10.1038/317359a0. [DOI] [PubMed] [Google Scholar]
- 74.Evavold B, Sloan-Lancaster J, Wilson K, Rothbard J, Allen P. Specific t cell recognition of minimally homologous peptides. Evidence for multiple endogenous ligands. Immunity. 1995;2:655. doi: 10.1016/1074-7613(95)90010-1. [DOI] [PubMed] [Google Scholar]
- 75.Sloan-Lancaster J, Allen Pm. Altered peptide ligand-induced partial t cell activation: Molecular mechanisms and role in t cell biology. Annu Rev Immunol. 1996;14:1–27. doi: 10.1146/annurev.immunol.14.1.1. [DOI] [PubMed] [Google Scholar]
- 76.Sloan-Lancaster J, Evavold Bd, Allen Pm. Induction of t-cell anergy by altered t-cell-receptor ligand on live antigen-presenting cells. Nature. 1993;363(6425):156–159. doi: 10.1038/363156a0. [DOI] [PubMed] [Google Scholar]
- 77.Kersh Gj, Allen Pm. Structural basis for t cell recognition of altered peptide ligands: A single t cell receptor can productively recognize a large continuum of related ligands. J Exp Med. 1996;184(4):1259–1268. doi: 10.1084/jem.184.4.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lanzavecchia A. How can cryptic epitopes trigger autoimmunity? J Exp Med. 1995;181(6):1945–1948. doi: 10.1084/jem.181.6.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Luo H, Zhang J, Dastvan F, et al. Ubiquitin-dependent proteolysis of cyclin d1 is associated with coxsackievirus-induced cell growth arrest. J Virol. 2003;77(1):1–9. doi: 10.1128/JVI.77.1.1-9.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vidard L, Rock Kl, Benacerraf B. Heterogeneity in antigen processing by different types of antigen-presenting cells. Effect of cell culture on antigen processing ability. J Immunol. 1992;149(6):1905–1911. [PubMed] [Google Scholar]
- 81.Gresser O, Weber E, Hellwig A, Riese S, Regnier-Vigouroux A. Immunocompetent astrocytes and microglia display major differences in the processing of the invariant chain and in the expression of active cathepsin l and cathepsin s. Eur J Immunol. 2001;31(6):1813–1824. doi: 10.1002/1521-4141(200106)31:6<1813::aid-immu1813>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 82.Salemi S, Caporossi Ap, Boffa L, Longobardi Mg, Barnaba V. Hivgp120 activates autoreactive cd4-specific t cell responses by unveiling of hidden cd4 peptides during processing. J Exp Med. 1995;181(6):2253–2257. doi: 10.1084/jem.181.6.2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sattentau Qj, Moore Jp, Vignaux F, Traincard F, Poignard P. Conformational changes induced in the envelope glycoproteins of the human and simian immunodeficiency viruses by soluble receptor binding. J Virol. 1993;67(12):7383–7393. doi: 10.1128/jvi.67.12.7383-7393.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Simitsek Pd, Campbell Dg, Lanzavecchia A, Fairweather N, Watts C. Modulation of antigen processing by bound antibodies can boost or suppress class ii major histocompatibility complex presentation of different t cell determinants. J Exp Med. 1995;181(6):1957–1963. doi: 10.1084/jem.181.6.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Driessen C, Lennon-Dumenil Am, Ploegh Hl. Individual cathepsins degrade immune complexes internalized by antigen-presenting cells via fcgamma receptors. Eur J Immunol. 2001;31(5):1592–1601. doi: 10.1002/1521-4141(200105)31:5<1592::AID-IMMU1592>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 86.Gauntt C, Sakkinen P, Rose N, Huber S. Picornaviruses: Immunopathology and autoimmunity. In: Cunningham M, Fujinami R, editors. Effects of microbes on the immune system. Lippincott-Raven Publishers; Philadelphia: 2000. pp. 313–329. [Google Scholar]
- 87.Badorff C, Lee Gh, Lamphear Bj, et al. Enteroviral protease 2a cleaves dystrophin: Evidence of cytoskeletal disruption in an acquired cardiomyopathy. Nat Med. 1999;5(3):320–326. doi: 10.1038/6543. [DOI] [PubMed] [Google Scholar]
- 88.O’hagan Dt, Valiante Nm. Recent advances in the discovery and delivery of vaccine adjuvants. Nat Rev Drug Discov. 2003;2(9):727–735. doi: 10.1038/nrd1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Marrack P, Mckee As, Munks Mw. Towards an understanding of the adjuvant action of aluminium. Nat Rev Immunol. 2009;9(4):287–293. doi: 10.1038/nri2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Allison Ac. Immunological adjuvants and their modes of action. Arch Immunol Ther Exp (Warsz) 1997;45(2–3):141–147. [PubMed] [Google Scholar]
- 91.Abreu Mt, Arditi M. Innate immunity and toll-like receptors: Clinical implications of basic science research. J Pediatr. 2004;144(4):421–429. doi: 10.1016/j.jpeds.2004.01.057. [DOI] [PubMed] [Google Scholar]
- 92.Means Tk, Golenbock Dt, Fenton Mj. The biology of toll-like receptors. Cytokine & growth factor reviews. 2000;11(3):219–232. doi: 10.1016/s1359-6101(00)00006-x. [DOI] [PubMed] [Google Scholar]
- 93.Netea Mg, Van Der Meer Jw, Kullberg Bj. Toll-like receptors as an escape mechanism from the host defense. Trends in microbiology. 2004;12(11):484–488. doi: 10.1016/j.tim.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 94.O’neill La. Tlrs. Professor mechnikov, sit on your hat. Trends in immunology. 2004;25(12):687–693. doi: 10.1016/j.it.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 95.Lauw Fn, Caffrey Dr, Golenbock Dt. Of mice and man: Tlr11 (finally) finds profilin. Trends in immunology. 2005;26(10):509–511. doi: 10.1016/j.it.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 96.Hasan U, Chaffois C, Gaillard C, et al. Human tlr10 is a functional receptor, expressed by b cells and plasmacytoid dendritic cells, which activates gene transcription through myd88. J Immunol. 2005;174(5):2942–2950. doi: 10.4049/jimmunol.174.5.2942. [DOI] [PubMed] [Google Scholar]
- 97.Pulendran B. Variegation of the immune response with dendritic cells and pathogen recognition receptors. J Immunol. 2005;174(5):2457–2465. doi: 10.4049/jimmunol.174.5.2457. [DOI] [PubMed] [Google Scholar]
- 98.Netea Mg, Van Der Meer Jw, Sutmuller Rp, Adema Gj, Kullberg Bj. From the th1/th2 paradigm towards a toll-like receptor/t-helper bias. Antimicrobial agents and chemotherapy. 2005;49(10):3991–3996. doi: 10.1128/AAC.49.10.3991-3996.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liew Fy, Komai-Koma M, Xu D. A toll for t cell costimulation. Annals of the rheumatic diseases. 2004;63(Suppl 2):ii76–ii78. doi: 10.1136/ard.2004.028308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dong Z, Wei H, Sun R, Tian Z. The roles of innate immune cells in liver injury and regeneration. Cell Mol Immunol. 2007;4(4):241–252. [PubMed] [Google Scholar]
- 101.Li Y, Heuser Js, Kosanke Sd, Hemric M, Cunningham Mw. Protection against experimental autoimmune myocarditis is mediated by interleukin-10-producing t cells that are controlled by dendritic cells. Am J Pathol. 2005;167(1):5–15. doi: 10.1016/S0002-9440(10)62948-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang Y, Afanasyeva M, Hill Sl, Kaya Z, Rose Nr. Nasal administration of cardiac myosin suppresses autoimmune myocarditis in mice. J Am Coll Cardiol. 2000;36(6):1992–1999. doi: 10.1016/s0735-1097(00)00939-6. [DOI] [PubMed] [Google Scholar]
- 103.Taneja V, Hansen J, Smart M, Griffiths M, Luthra H, David C. Expression of h-2e molecule mediates protection to collagen induced arthritis in hla-dq8 transgenic mice: Role of cytokines. International Immunol. 1997;9:1213–1219. doi: 10.1093/intimm/9.8.1213. [DOI] [PubMed] [Google Scholar]
- 104.Rose Nr. The adjuvant effect in infection and autoimmunity. Clin Rev Allergy Immunol. 2008 doi: 10.1007/s12016-007-8049-7. [DOI] [PubMed] [Google Scholar]
- 105.Frisancho-Kiss S, Davis Se, Nyland Jf, et al. Cutting edge: Cross-regulation by tlr4 and t cell ig mucin-3 determines sex differences in inflammatory heart disease. J Immunol. 2007;178(11):6710–6714. doi: 10.4049/jimmunol.178.11.6710. [DOI] [PubMed] [Google Scholar]
- 106.Triantafilou K, Triantafilou M. Coxsackievirus b4-induced cytokine production in pancreatic cells is mediated through toll-like receptor 4. J Virol. 2004;78(20):11313–11320. doi: 10.1128/JVI.78.20.11313-11320.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Avalos Am, Busconi L, Marshak-Rothstein A. Regulation of autoreactive b cell responses to endogenous tlr ligands. Autoimmunity. 2009 doi: 10.3109/08916930903374618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Drexler Sk, Foxwell Bm. The role of toll-like receptors in chronic inflammation. Int J Biochem Cell Biol. 2009 doi: 10.1016/j.biocel.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 109.Abdollahi-Roodsaz S, Joosten La, Koenders Mi, Van Den Brand Bt, Van De Loo Fa, Van Den Berg Wb. Local interleukin-1-driven joint pathology is dependent on toll-like receptor 4 activation. Am J Pathol. 2009;175(5):2004–2013. doi: 10.2353/ajpath.2009.090262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang P, Cox Cj, Alvarez Km, Cunningham Mw. Cutting edge: Cardiac myosin activates innate immune responses through tlrs. J Immunol. 2009;183(1):27–31. doi: 10.4049/jimmunol.0800861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Boyd Jh, Mathur S, Wang Y, Bateman Rm, Walley Kr. Toll-like receptor stimulation in cardiomyoctes decreases contractility and initiates an nf-kappab dependent inflammatory response. Cardiovasc Res. 2006;72(3):384–393. doi: 10.1016/j.cardiores.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 112.Zhu X, Bagchi A, Zhao H, et al. Toll-like receptor 2 activation by bacterial peptidoglycan-associated lipoprotein activates cardiomyocyte inflammation and contractile dysfunction. Crit Care Med. 2007;35(3):886–892. doi: 10.1097/01.CCM.0000256723.37586.A2. [DOI] [PubMed] [Google Scholar]
- 113.Xu J, Yang Y, Wang C, Jiang B. Rotavirus and coxsackievirus infection activated different profiles of toll-like receptors and chemokines in intestinal epithelial cells. Inflamm Res. 2009;58(9):585–592. doi: 10.1007/s00011-009-0022-x. [DOI] [PubMed] [Google Scholar]
- 114.Sutmuller Rp, Morgan Me, Netea Mg, Grauer O, Adema Gj. Toll-like receptors on regulatory t cells: Expanding immune regulation. Trends in immunology. 2006;27(8):387–393. doi: 10.1016/j.it.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 115.Sakaguchi S, Setoguchi R, Yagi H, Nomura T. Naturally arising foxp3-expressing cd25+cd4+ regulatory t cells in self-tolerance and autoimmune disease. Curr Top Microbiol Immunol. 2006;305:51–66. doi: 10.1007/3-540-29714-6_3. [DOI] [PubMed] [Google Scholar]
- 116.Lehner T. Special regulatory t cell review: The resurgence of the concept of contrasuppression in immunoregulation. Immunology. 2008;123(1):40–44. doi: 10.1111/j.1365-2567.2007.02780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Harnaha J, Machen J, Wright M, et al. Interleukin-7 is a survival factor for cd4+ cd25+ t-cells and is expressed by diabetes-suppressive dendritic cells. Diabetes. 2006;55(1):158–170. [PubMed] [Google Scholar]
- 118.Jonuleit H, Knop J, Enk Ah. Cytokines and their effects on maturation, differentiation and migration of dendritic cells. Arch Dermatol Res. 1996;289(1):1–8. doi: 10.1007/s004030050144. [DOI] [PubMed] [Google Scholar]
- 119.Stoop Jn, Woltman Am, Biesta Pj, et al. Tumor necrosis factor alpha inhibits the suppressive effect of regulatory t cells on the hepatitis b virus-specific immune response. Hepatology. 2007;46(3):699–705. doi: 10.1002/hep.21761. [DOI] [PubMed] [Google Scholar]
- 120.Liu G, Zhang L, Zhao Y. Modulation of immune responses through direct activation of toll-like receptors to t cells. Clin Exp Immunol. doi: 10.1111/j.1365-2249.2010.04091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Klein Sl, Huber SA. Sex differences in susceptibility to viral infection. In: Klein Slar CW, editor. Sex hormones and immunity to infection. Springer Verlag; Berlin, Germany: 2010. [Google Scholar]
- 122.Smithson G, Couse J, Lubahn D, Korach K, Kincade P. The role of estrogen receptors and androgen receptors in sex steroid regulation of b lymphocytes. J Immunol. 1998;161:27–34. [PubMed] [Google Scholar]
- 123.Islander U, Erlandsson Mc, Hasseus B, et al. Influence of oestrogen receptor alpha and beta on the immune system in aged female mice. Immunology. 2003;110(1):149–157. doi: 10.1046/j.1365-2567.2003.01704.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Paharkova-Vatchkova V, Maldonado R, Kovats S. Estrogen preferentially promotes the differentiation of cd11c+ cd11b(intermediate) dendritic cells from bone marrow precursors. J Immunol. 2004;172(3):1426–1436. doi: 10.4049/jimmunol.172.3.1426. [DOI] [PubMed] [Google Scholar]
- 125.Ito A, Bebo Bf, Jr, Matejuk A, et al. Estrogen treatment down-regulates tnf-alpha production and reduces the severity of experimental autoimmune encephalomyelitis in cytokine knockout mice. J Immunol. 2001;167(1):542–552. doi: 10.4049/jimmunol.167.1.542. [DOI] [PubMed] [Google Scholar]
- 126.Li J, Mcmurray Rw. Effects of estrogen receptor subtype-selective agonists on immune functions in ovariectomized mice. Int Immunopharmacol. 2006;6(9):1413–1423. doi: 10.1016/j.intimp.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 127.Lambert Kc, Curran Em, Judy Bm, Milligan Gn, Lubahn Db, Estes Dm. Estrogen receptor alpha (eralpha) deficiency in macrophages results in increased stimulation of cd4+ t cells while 17beta-estradiol acts through eralpha to increase il-4 and gata-3 expression in cd4+ t cells independent of antigen presentation. J Immunol. 2005;175(9):5716–5723. doi: 10.4049/jimmunol.175.9.5716. [DOI] [PubMed] [Google Scholar]
- 128.Karpuzoglu-Sahin E, Hissong Bd, Ansar Ahmed S. Interferon-gamma levels are upregulated by 17-beta-estradiol and diethylstilbestrol. J Reprod Immunol. 2001;52(1–2):113–127. doi: 10.1016/s0165-0378(01)00117-6. [DOI] [PubMed] [Google Scholar]
- 129.Grimaldi Cm, Cleary J, Dagtas As, Moussai D, Diamond B. Estrogen alters thresholds for b cell apoptosis and activation. J Clin Invest. 2002;109(12):1625–1633. doi: 10.1172/JCI14873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Polanczyk Mj, Hopke C, Huan J, Vandenbark Aa, Offner H. Enhanced foxp3 expression and treg cell function in pregnant and estrogen-treated mice. J Neuroimmunol. 2005;170(1–2):85–92. doi: 10.1016/j.jneuroim.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 131.Polanczyk Mj, Jones Re, Subramanian S, et al. T lymphocytes do not directly mediate the protective effect of estrogen on experimental autoimmune encephalomyelitis. Am J Pathol. 2004;165(6):2069–2077. doi: 10.1016/S0002-9440(10)63257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tai P, Wang J, Jin H, et al. Induction of regulatory t cells by physiological level estrogen. Journal of cellular physiology. 2008;214(2):456–464. doi: 10.1002/jcp.21221. [DOI] [PubMed] [Google Scholar]
- 133.Liu Hy, Buenafe Ac, Matejuk A, et al. Estrogen inhibition of eae involves effects on dendritic cell function. Journal of neuroscience research. 2002;70(2):238–248. doi: 10.1002/jnr.10409. [DOI] [PubMed] [Google Scholar]
- 134.Schwartz J, Sartini D, Huber S. Myocarditis susceptibility in female mice depends upon ovarian cycle phase at infection. Virology. 2004;330(1):16–23. doi: 10.1016/j.virol.2004.06.051. [DOI] [PubMed] [Google Scholar]
- 135.Matthews J, Gustafsson Ja. Estrogen signaling: A subtle balance between er alpha and er beta. Molecular interventions. 2003;3(5):281–292. doi: 10.1124/mi.3.5.281. [DOI] [PubMed] [Google Scholar]
- 136.Scariano Jk, Emery-Cohen Aj, Pickett Gg, Morgan M, Simons Pc, Alba F. Estrogen receptors alpha (esr1) and beta (esr2) are expressed in circulating human lymphocytes. Journal of receptor and signal transduction research. 2008;28(3):285–293. doi: 10.1080/10799890802084614. [DOI] [PubMed] [Google Scholar]
- 137.Carreras E, Turner S, Paharkova-Vatchkova V, Mao A, Dascher C, Kovats S. Estradiol acts directly on bone marrow myeloid progenitors to differentially regulate gm-csf or flt3 ligand-mediated dendritic cell differentiation. J Immunol. 2008;180(2):727–738. doi: 10.4049/jimmunol.180.2.727. [DOI] [PubMed] [Google Scholar]
- 138.Douin-Echinard V, Laffont S, Seillet C, et al. Estrogen receptor alpha, but not beta, is required for optimal dendritic cell differentiation and [corrected] cd40-induced cytokine production. J Immunol. 2008;180(6):3661–3669. doi: 10.4049/jimmunol.180.6.3661. [DOI] [PubMed] [Google Scholar]
- 139.Tsutsumi S, Zhang X, Takata K, et al. Differential regulation of the inducible nitric oxide synthase gene by estrogen receptors 1 and 2. J Endocrinol. 2008;199(2):267–273. doi: 10.1677/JOE-07-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Klinge Cm. Estrogenic control of mitochondrial function and biogenesis. J Cell Biochem. 2008;105(6):1342–1351. doi: 10.1002/jcb.21936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kubarek L, Jagodzinski Pp. Epigenetic up-regulation of cxcr4 and cxcl12 expression by 17 beta-estradiol and tamoxifen is associated with formation of DNA methyltransferase 3b4 splice variant in ishikawa endometrial adenocarcinoma cells. FEBS letters. 2007;581(7):1441–1448. doi: 10.1016/j.febslet.2007.02.070. [DOI] [PubMed] [Google Scholar]
- 142.Wickham Tj, Mathias P, Cheresh Da, Nemerow Gr. Integrins alpha v beta 3 and alpha v beta 5 promote adenovirus internalization but not virus attachment. Cell. 1993;73(2):309–319. doi: 10.1016/0092-8674(93)90231-e. [DOI] [PubMed] [Google Scholar]
- 143.Roivainen M, Piirainen L, Hovi T, et al. Entry of coxsackievirus a9 into host cells: Specific interactions with alpha v beta 3 integrin, the vitronectin receptor. Virology. 1994;203(2):357–365. doi: 10.1006/viro.1994.1494. [DOI] [PubMed] [Google Scholar]
- 144.Li Cf, Ross Fp, Cao X, Teitelbaum Sl. Estrogen enhances alpha v beta 3 integrin expression by avian osteoclast precursors via stabilization of beta 3 integrin mrna. Molecular endocrinology (Baltimore, Md. 1995;9(7):805–813. doi: 10.1210/mend.9.7.7476964. [DOI] [PubMed] [Google Scholar]
- 145.Gavrilovskaya In, Shepley M, Shaw R, Ginsberg Mh, Mackow Er. Beta3 integrins mediate the cellular entry of hantaviruses that cause respiratory failure. Proc Natl Acad Sci U S A. 1998;95(12):7074–7079. doi: 10.1073/pnas.95.12.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bergelson Jm, Modlin Jf, Wieland-Alter W, Cunningham Ja, Crowell Rl, Finberg Rw. Clinical coxsackievirus b isolates differ from laboratory strains in their interaction with two cell surface receptors. J Infect Dis. 1997;175(3):697–700. doi: 10.1093/infdis/175.3.697. [DOI] [PubMed] [Google Scholar]
- 147.Goodfellow Ig, Evans Dj, Blom Am, et al. Inhibition of coxsackie b virus infection by soluble forms of its receptors: Binding affinities, altered particle formation, and competition with cellular receptors. J Virol. 2005;79(18):12016–12024. doi: 10.1128/JVI.79.18.12016-12024.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Shafren D. Viral cell entry induced by cross-linked decay-accelerating factor. J Virol. 1998;72:9407–9412. doi: 10.1128/jvi.72.11.9407-9412.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Selinka Hc, Wolde A, Sauter M, Kandolf R, Klingel K. Virus-receptor interactions of coxsackie b viruses and their putative influence on cardiotropism. Medical microbiology and immunology. 2004;193(2–3):127–131. doi: 10.1007/s00430-003-0193-y. [DOI] [PubMed] [Google Scholar]
- 150.Pasch A, Kupper Jh, Wolde A, Kandolf R, Selinka Hc. Comparative analysis of virus-host cell interactions of haemagglutinating and non-haemagglutinating strains of coxsackievirus b3. J Gen Virol. 1999;80 ( Pt 12):3153–3158. doi: 10.1099/0022-1317-80-12-3153. [DOI] [PubMed] [Google Scholar]
- 151.Yanagawa B, Spiller Ob, Choy J, et al. Coxsackievirus b3-associated myocardial pathology and viral load reduced by recombinant soluble human decay-accelerating factor in mice. Lab Invest. 2003;83(1):75–85. doi: 10.1097/01.lab.0000049349.56211.09. [DOI] [PubMed] [Google Scholar]
- 152.Yanagawa B, Spiller Ob, Proctor Dg, et al. Soluble recombinant coxsackievirus and adenovirus receptor abrogates coxsackievirus b3-mediated pancreatitis and myocarditis in mice. J Infect Dis. 2004;189(8):1431–1439. doi: 10.1086/382598. [DOI] [PubMed] [Google Scholar]
- 153.Huber S, Song Wc, Sartini D. Decay-accelerating factor (cd55) promotes cd1d expression and vgamma4+ t-cell activation in coxsackievirus b3-induced myocarditis. Viral Immunol. 2006;19(2):156–166. doi: 10.1089/vim.2006.19.156. [DOI] [PubMed] [Google Scholar]
- 154.Song Wc, Deng C, Raszmann K, et al. Mouse decay-accelerating factor: Selective and tissue-specific induction by estrogen of the gene encoding the glycosylphosphatidylinositol-anchored form. J Immunol. 1996;157(9):4166–4172. [PubMed] [Google Scholar]
- 155.Lyden D, Olszewski J, Feran M, Job L, Huber S. Coxsackievirus b3-induced myocarditis. Effects of sex steroids on viremia and infectivity of cardiocytes. Am J Pathol. 1987;126:432–438. [PMC free article] [PubMed] [Google Scholar]
- 156.Sun X, Funk Cd, Deng C, Sahu A, Lambris Jd, Song Wc. Role of decay-accelerating factor in regulating complement activation on the erythrocyte surface as revealed by gene targeting. Proc Natl Acad Sci U S A. 1999;96(2):628–633. doi: 10.1073/pnas.96.2.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Liu J, Miwa T, Hilliard B, et al. The complement inhibitory protein daf (cd55) suppresses t cell immunity in vivo. J Exp Med. 2005;201(4):567–577. doi: 10.1084/jem.20040863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Miwa T, Maldonado Ma, Zhou L, et al. Deletion of decay-accelerating factor (cd55) exacerbates autoimmune disease development in mrl/lpr mice. Am J Pathol. 2002;161(3):1077–1086. doi: 10.1016/S0002-9440(10)64268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Vincent T, Pettersson Rf, Crystal Rg, Leopold Pl. Cytokine-mediated downregulation of coxsackievirus-adenovirus receptor in endothelial cells. J Virol. 2004;78(15):8047–8058. doi: 10.1128/JVI.78.15.8047-8058.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ostermann G, Weber Ks, Zernecke A, Schroder A, Weber C. Jam-1 is a ligand of the beta(2) integrin lfa-1 involved in transendothelial migration of leukocytes. Nat Immunol. 2002;3(2):151–158. doi: 10.1038/ni755. [DOI] [PubMed] [Google Scholar]
- 161.Lisewski U, Shi Y, Wrackmeyer U, et al. The tight junction protein car regulates cardiac conduction and cell-cell communication. J Exp Med. 2008;205(10):2369–2379. doi: 10.1084/jem.20080897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Carson Sd, Chapman Nm. Coxsackievirus and adenovirus receptor (car) binds immunoglobulins. Biochemistry. 2001;40(48):14324–14329. doi: 10.1021/bi015571y. [DOI] [PubMed] [Google Scholar]
- 163.Haynes M, Huber S, Craighead J. Helper-inducer t lymphocytes mediate diabetes in emc-infected balb/cbyj mice. Diabetes. 1987;36:877–881. doi: 10.2337/diab.36.7.877. [DOI] [PubMed] [Google Scholar]
- 164.Miller S, Vanderlugt C, Begolka W, et al. Persistent infection with theiler’s virus leads to cns autoimmunity via epitope spreading. Nat Med. 1997;3:1133–1136. doi: 10.1038/nm1097-1133. [DOI] [PubMed] [Google Scholar]
- 165.Olson Jk, Ercolini Am, Miller Sd. A virus-induced molecular mimicry model of multiple sclerosis. Curr Top Microbiol Immunol. 2005;296:39–53. doi: 10.1007/3-540-30791-5_3. [DOI] [PubMed] [Google Scholar]
- 166.Huber S. T cells in coxsackievirus induced myocarditis. Viral Immunology. 2004;17:152–164. doi: 10.1089/0882824041310667. [DOI] [PubMed] [Google Scholar]
- 167.Huber S, Lodge P. Coxsackievirus b3 myocarditis in balb/c mice. Evidence for autoimmunity to myocyte antigens. Am J Path. 1984;116:21. [PMC free article] [PubMed] [Google Scholar]
- 168.Huber Sa, Sartini D, Exley M. Vgamma4(+) t cells promote autoimmune cd8(+) cytolytic t-lymphocyte activation in coxsackievirus b3-induced myocarditis in mice: Role for cd4(+) th1 cells. J Virol. 2002;76(21):10785–10790. doi: 10.1128/JVI.76.21.10785-10790.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Huber S, Gauntt C. Antigenic mimicry between self and coxsackievirus protein leads to both humoral and cellular autoimmunity to heart proteins. ASM Press; 2000. p. 51. [Google Scholar]
- 170.Huber S, Job L, Auld K. Influence of sex hormones on coxsackie b3 virus infection in balb/c mice. Cell Immunol. 1982;67(173–189):173–179. doi: 10.1016/0008-8749(82)90210-6. [DOI] [PubMed] [Google Scholar]
- 171.Huber S, Kupperman J, Newell M. Hormonal regulation of cd4+ t-cell responses in coxsackievirus b3-induced myocarditis in mice. J Virol. 1999;73:4689–4695. doi: 10.1128/jvi.73.6.4689-4695.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Huber S, Pfaeffle B. Differential th1 and th2 cell responses in male and female balb/c mice infected with coxsackievirus group b type 3. J Virol. 1994;68:5126–5132. doi: 10.1128/jvi.68.8.5126-5132.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Huber Sa, Pfaeffle B. Differential th1 and th2 cell responses in male and female balb/c mice infected with coxsackievirus group b type 3. J Virol. 1994;68(8):5126–5132. doi: 10.1128/jvi.68.8.5126-5132.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Huber Sa. Coxsackievirus b3-induced myocarditis: Infection of females during the estrus phase of the ovarian cycle leads to activation of t regulatory cells. Virology. 2008;378(2):292–298. doi: 10.1016/j.virol.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Offner H, Polanczyk M. A potential role for estrogen in experimental autoimmune encephalomyelitis and multiple sclerosis. Ann N Y Acad Sci. 2006;1089:343–372. doi: 10.1196/annals.1386.021. [DOI] [PubMed] [Google Scholar]
- 176.Ziegler Sf. Foxp3: Of mice and men. Annu Rev Immunol. 2006;24:209–226. doi: 10.1146/annurev.immunol.24.021605.090547. [DOI] [PubMed] [Google Scholar]
- 177.Wutz A. Xist function: Bridging chromatin and stem cells. Trends Genet. 2007;23(9):457–464. doi: 10.1016/j.tig.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 178.Shapiro Lj, Mohandas T, Weiss R, Romeo G. Non-inactivation of an x-chromosome locus in man. Science. 1979;204(4398):1224–1226. doi: 10.1126/science.156396. [DOI] [PubMed] [Google Scholar]
- 179.Disteche Cm, Filippova Gn, Tsuchiya Kd. Escape from x inactivation. Cytogenet Genome Res. 2002;99(1–4):36–43. doi: 10.1159/000071572. [DOI] [PubMed] [Google Scholar]
- 180.Lal G, Bromberg Js. Epigenetic mechanisms of regulation of foxp3 expression. Blood. 2009;114(18):3727–3735. doi: 10.1182/blood-2009-05-219584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Salem Ml. Estrogen, a double-edged sword: Modulation of th1- and th2-mediated inflammations by differential regulation of th1/th2 cytokine production. Curr Drug Targets Inflamm Allergy. 2004;3(1):97–104. doi: 10.2174/1568010043483944. [DOI] [PubMed] [Google Scholar]
- 182.Ray P, Ghosh Sk, Zhang Dh, Ray A. Repression of interleukin-6 gene expression by 17 beta-estradiol: Inhibition of the DNA-binding activity of the transcription factors nf-il6 and nf-kappa b by the estrogen receptor. FEBS letters. 1997;409(1):79–85. doi: 10.1016/s0014-5793(97)00487-0. [DOI] [PubMed] [Google Scholar]