Abstract
Bile-duct invasion is rare in patients with hepatocellular carcinoma (HCC). We report a case that received peroral direct cholangioscopy (PDCS)-guided endoscopic biopsy and photodynamic treatment (PDT) for recurrent HCC with intraductal tiny nodular tumor growth. A 64-year-old woman presented with recurrent right upper-quadrant pain. Six months previously she had been diagnosed with HCC with bile-duct invasion in the right anterior segment and had received right anterior segmentectomy. On pathological examination, the margin of resection was clear, but macroscopic bile-duct invasion was noted. On admission, magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography (ERCP) revealed a 0.5-cm-sized polypoid mass at the hilar portion. ERCP-guided biopsy failed, and an ampullary stricture was noted. PDCS-guided endoscopic biopsy was thus performed, and histopathology of the retrieved specimen revealed HCC. The patient submitted to PDT. There was no procedure-related complication. After 1 month of PDT the polypoid lesion and scar change at the hilar lesion had disappeared.
Keywords: Peroral direct cholangioscopy, Photodynamic treatment, Recurrent hepatocellular carcinoma, Intraductal growth
INTRODUCTION
Invasion of blood vessels, particularly the portal vein, is a common feature of hepatocellular carcinoma (HCC), however bile duct invasion is rare. HCC with bile duct invasion is characterized by obstructive jaundice or hemobilia from the tumor thrombi. Hepatectomy is an effective treatment. However, most of this type of patients are inoperable. The alternative treatment strategy is palliative in intent, including transcatheter arterial chemoembolization, and/or radiotherapy.1 Also, percutaneous cholangioscopic ethanol injection or microwave coagulation therapy was reported to control HCC with bile duct invasion.2,3
Recently, a feasibility study and therapeutic case of an ultraslim or standard upper endoscope have been reported for peroral direct cholangioscopy (PDCS) without the use of a mother-baby endoscopic system.4-8 Here, we describe the first report of PDCS-guided endoscopic biopsy and photodynamic therapy (PDT) for recurrent HCC with intraductal tiny nodular tumor growth.
CASE REPORT
A 64-year-old woman presented with recurrent right upper quadrant pain. Six months ago, she was diagnosed with HCC with bile duct invasion in right anterior segment, and right anterior segmentectomy was performed. On pathological examination, grossly 2.2×1.5×1.0 cm sized HCC mainly on intrahepatic duct of segment 8 was noted. However, margin of resection was clear. On this admission, physical examination revealed mild right upper quadrant tenderness. Laboratory findings was as follows: white blood cell count 6,500/mm3, hemoglobin 10.8 g/dL, platelet 195×103/mm3, aspartate aminotransferase 37 IU/L, alanine aminotransferase 65 IU/L, alkaline phosphatase 163 IU/L, gamma glutamyl transpeptidase 94 IU/L, total bilirubin 1.0 mg/dL, prothrombin time 88.5% (1.06 INR) and serum alpha-fetoprotein 3.2 ng/mL. The patient was positive for hepatitis B virus surface antigen. On abdominal CT scan, there was no definite tumor recurrence. Endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) revealed an about 0.5 cm-sized eccentric polypoid mass at hilar portion (Fig. 1A and B). On ERCP, targeted biopsy under fluoroscopic guidance failed. After performing endoscopic papillary balloon dilatation with CRE balloon (12 mm; Boston Scientific, Natick, MA, USA) due to ampullary stricture, therefore, ultraslim upper endoscope (GIF-XP260N; Olympus Optical Co., Ltd., Tokyo, Japan) was inserted into the CBD through the dilated papilla without guidewire assistance. An about 0.5 cm-sized polypoid mass was observed on hilar portion (Fig. 2A), and PDCS-guided endoscopic biopsy was performed at this lesion. Histopathology revealed HCC (Fig. 2B). Considering the hilar location of tiny nodular lesion and the history of previous operation, we decided that local treatment modality such as argon plasma coagulation (APC) or PDT. Due to ampullary stricture, advance of ultraslim upper endoscope to hilar level was difficult. Approximation of APC probe to nodular lesion may therefore not be feasible. The patient received photosensitizer (Photofrin®; Axcan Pharma, Mont-Saint-Hilaire, Quebec, Canada) at a dosage of 2 mg/kg intravenously, and intraluminal photoactivation was performed with a laser quartz fiber bearing a cylindrical diffuser tip (CD 405-30C, 4 cm in length; CeramOptec GmbH, Bonn, Germany) 48 hours later. The fiber was placed at the hilar portion through the working channel of ultraslim upper endoscope. Photoactivation was performed two times at 630 nm using a light dose of 180 J/cm2, fluence of 0.241 W/cm2, and irradiation time of 600 seconds under direct vision and fluoroscopic guidance (Fig. 3). No procedure-related complication was encountered. After 1 month of PDT, direct visualization with ultraslim upper endoscope and balloon occluded cholangiography revealed disappearance of polypoid lesion and scar change at the hilar portion (Figs. 1C, 2C and D). The patient remained well during 5 months of follow-up with no evidence of recurred HCC on imaging study.
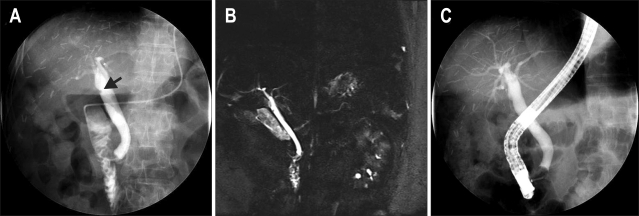
Fig. 1.
(A, B) Endoscopic retrograde cholangiopancreatography (black arrow) and magnetic resonance cholangiopancreatography revealed a 0.5-cm-sized eccentric polypoid lesion at the hilar portion. (C) Follow-up balloon-occluded cholangiography revealed disappearance of the polypoid lesion at the hilar portion.
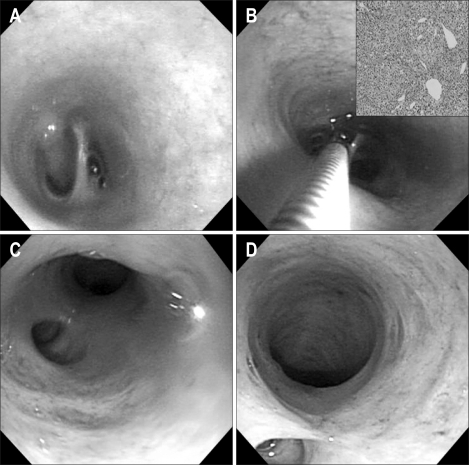
Fig. 2.
(A) Peroral direct cholangioscopic findings demonstrating a 0.5-cm-sized polypoid lesion on the hilar portion. (B) Peroral direct cholangioscopy (PDCS)-guided biopsy specimen of the tiny nodular lesions at the hilar portion. Endoscopic biopsy revealed a hepatocellular carcinoma (H&E stain, ×200; inset). (C, D) Follow-up PDCS with an ultraslim upper endoscope revealed disappearance of the polypoid lesion at the hilar portion.
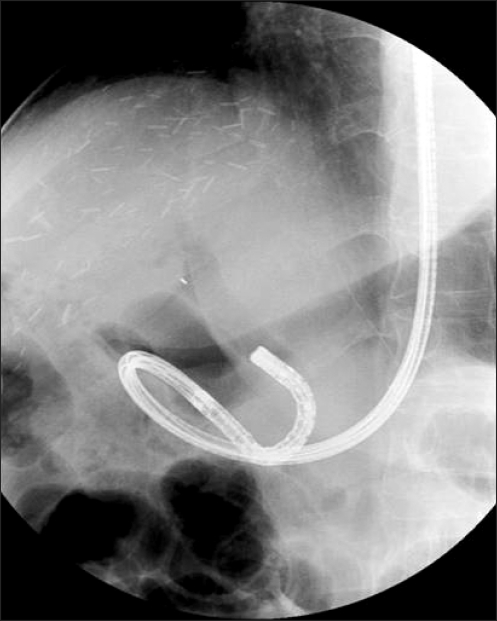
Fig. 3.
Peroral direct cholangioscopy-guided photodynamic treatment was performed using an ultraslim upper endoscope.
DISCUSSION
ERCP guided brushing cytology or biopsy may be standard sampling methods for bile duct lesion. However, yield of cytology and biopsy may be unsatisfactory and precise acquisition of tiny intrabiliary lesion may be difficult.9,10 As in our case, PDCS-guided biopsy under direct vision may be useful for this situation.
To date, percutaneous cholangioscopic ethanol injection or microwave coagulation therapy are the techniques used to control HCC with intraductal tumor or thrombi.2,3 However, cholangioscopic ethanol injection or microwave coagulation therapy required many sessions.3 And a percutaneous approach may require sinus-tract maturation, resulting in delayed management and development of procedure- related complications.11
In previous our study,8 PDCS-guided APC for intrabiliary tumors of the bile duct may be feasible. However, as in the present case, approximation of PDCS-guided APC probe to proximal biliary tract may be difficult according to ampullary stricture. In this situation, PDCS with PDT may have a several advantage. Cylindrical diffuse tip with radio-opaque markers may be feasible for targeting of far distal intrabiliary lesion under direct vision and fluoroscopic guidance. Furthermore, PDT may be safer than APC which may be related to the procedural complications such as bleeding or perforation.12,13 In the present case, there was no procedure-related complication, but PDT related complications were reported such as cholangitis or photosensitivity. Photosensitivity that occurs for 4 to 6 weeks after therapy which may limit quality of life.12 Cholangitis was successfully managed with antibiotics.14
There are several reports that PDT is an effective method for the palliative treatment of un-resectable cholangiocarcinoma. PDT for un-resectable cholangiocarcinoma may increase survival and improve quality of life.12-15 However, as we are aware, there are no report of PDT for HCC with bile duct invasion. Further prospective studies are required to determine the efficacy and safety of PDT for HCC with intrabiliary tumor growth.
In summary, PDCS-guided biopsy and PDT by using an ultraslim upper endoscope may be a feasible, effective alternative management for recurrent HCC with intraductal tiny nodular tumor growth.
References
- 1.Qin LX, Tang ZY. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003;9:385–391. doi: 10.3748/wjg.v9.i3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seki T, Kubota Y, Wakabayashi M, et al. Percutaneous transhepatic microwave coagulation therapy for hepatocellular carcinoma proliferating in the bile duct. Dig Dis Sci. 1994;39:663–666. doi: 10.1007/BF02088358. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto H, Hayakawa N, Nagino M, Kamiya J, Nimura Y. Percutaneous transheptic cholangioscopic ethanol injection for intrabiliary tumor thrombi due to hepatocellular carcinoma. Endoscopy. 1999;31:204–206. doi: 10.1055/s-1999-13671. [DOI] [PubMed] [Google Scholar]
- 4.Brauer BC, Fukami N, Chen YK. Direct cholangioscopy with narrow-band imaging, chromoendoscopy, and argon plasma coagulation of intraductal papillary mucinous neoplasm of the bile duct (with videos) Gastrointest Endosc. 2008;67:574–576. doi: 10.1016/j.gie.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 5.Choi HJ, Moon JH, Ko BM, et al. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos) Gastrointest Endosc. 2009;69:935–940. doi: 10.1016/j.gie.2008.08.043. [DOI] [PubMed] [Google Scholar]
- 6.Han JH, Park do H, Moon SH, et al. Peroral direct cholangioscopic lithotripsy with a standard upper endoscope for difficult bile duct stones (with videos) Gastrointest Endosc. 2009;70:183–185. doi: 10.1016/j.gie.2008.09.042. [DOI] [PubMed] [Google Scholar]
- 7.Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853–857. doi: 10.1016/j.gie.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 8.Park do H, Park BW, Lee HS, et al. Peroral direct cholangioscopic argon plasma coagulation by using an ultraslim upper endoscope for recurrent hepatoma with intraductal nodular tumor growth (with videos) Gastrointest Endosc. 2007;66:201–203. doi: 10.1016/j.gie.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 9.Ferrari Júnior AP, Lichtenstein DR, Slivka A, Chang C, Carr-Locke DL. Brush cytology during ERCP for the diagnosis of biliary and pancreatic malignancies. Gastrointest Endosc. 1994;40(2 Pt 1):140–145. doi: 10.1016/s0016-5107(94)70155-5. [DOI] [PubMed] [Google Scholar]
- 10.Harewood GC, Baron TH, Stadheim LM, Kipp BR, Sebo TJ, Salomao DR. Prospective, blinded assessment of factors influencing the accuracy of biliary cytology interpretation. Am J Gastroenterol. 2004;99:1464–1469. doi: 10.1111/j.1572-0241.2004.30845.x. [DOI] [PubMed] [Google Scholar]
- 11.Shim CS, Neuhaus H, Tamada K. Direct cholangioscopy. Endoscopy. 2003;35:752–758. doi: 10.1055/s-2003-41580. [DOI] [PubMed] [Google Scholar]
- 12.Baron TH. Photodynamic therapy: standard of care for palliation of cholangiocarcinoma? Clin Gastroenterol Hepatol. 2008;6:266–267. doi: 10.1016/j.cgh.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Kahaleh M, Mishra R, Shami VM, et al. Unresectable cholangiocarcinoma: comparison of survival in biliary stenting alone versus stenting with photodynamic therapy. Clin Gastroenterol Hepatol. 2008;6:290–297. doi: 10.1016/j.cgh.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Harewood GC, Baron TH, Rumalla A, et al. Pilot study to assess patient outcomes following endoscopic application of photodynamic therapy for advanced cholangiocarcinoma. J Gastroenterol Hepatol. 2005;20:415–420. doi: 10.1111/j.1440-1746.2005.03582.x. [DOI] [PubMed] [Google Scholar]
- 15.Berr F, Wiedmann M, Tannapfel A, et al. Photodynamic therapy for advanced bile duct cancer: evidence for improved palliation and extended survival. Hepatology. 2000;31:291–298. doi: 10.1002/hep.510310205. [DOI] [PubMed] [Google Scholar]