Abstract
The transnasal endoscopic examination using an ultraslim upper endoscope may be more comfortable and less stressful than the peroral approach. Transnasal endoscopic retrograde cholangiopancreatography (ERCP), endoscopic nasobiliary drainage, and direct peroral cholangioscopy using an ultraslim upper endoscope have recently been reported. An 82-year-old woman with a previous history of endoscopic sphincterotomy and stone removal was admitted with acute cholangitis. Instead of conventional ERCP, we performed direct transnasal cholangioscopy (TNC) using an ultraslim upper endoscope for biliary decompression and stone removal because of her unstable vital signs. Direct TNC using an ultraslim upper endoscope may be useful in selected patients with biliary disease.
Keywords: Direct transnasal cholangioscopy, Bile duct stone removal, Ultra-slim upper endoscope
INTRODUCTION
Ultra-slim upper endoscopes are available for transnasal esophagogastroduodenoscopy (EGD). The transnasal approach may reduce patient discomfort and cardiovascular stress compared with the peroral approach.1-3 Recently, some investigators introduced direct peroral cholangioscopy (POC) using an ultra-slim upper endoscopes,4-6 and transnasal ERCP and endoscopic nasobiliary drainage (ENBD) have also been reported.7,8 We report the first bile duct stone extraction under direct transnasal cholangioscopy (TNC) after ENBD using an ultra-slim upper endoscope.
CASE REPORT
An 82-year-old woman who had chronic obstructive pulmonary disease was admitted with acute cholangitis caused by common bile duct (CBD) stones. She had undergone ERCP with CBD stone removal after an endoscopic sphincterotomy (EST) two years earlier. Her vital signs included low blood pressure (80/60 mm Hg) and a fever (38.5℃). The laboratory findings were as follows: white blood cell count 17,700/mm3, total/direct bilirubin 5.21/4.43 mg/dL, and alkaline phosphatase 421 IU/L.
We attempted direct cholangioscopy without sedation using an ultra-slim upper endoscope (GIF-XP260N; outer diameter 5.0 mm; instrumental channel diameter 2.0 mm; Olympus, Tokyo, Japan) via a transnasal approach because of the patient's unstable condition. The endoscope was easily advanced into the CBD through the ampullary orifice opened at the previous EST, and stones in the bile duct were observed directly without assistance. A 5 Fr ENBD catheter was inserted into the right intrahepatic duct, and the endoscope was withdrawn using the conventional method. Because the endoscope was inserted via a nasal route, mouth-to-nose transfer of the drainage tube was not required.
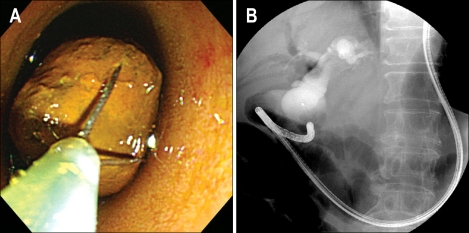
Three days later, her clinical findings had improved, and the serum bilirubin level had normalized. We performed ERCP with a conventional duodenoscope to remove stones. However, we did not continue the procedure because oxygen saturation dropped below 90% during ERCP. On the next day we attempted direct TNC for removal of the stones. After advancing the ultra-slim endoscope into the CBD, the stones were captured directly using a basket (Memory Basket 5FR Soft Wire; Cook Medical, Bloomington, IN, USA) under endoscopic visualization (Fig. 1) and removed from the bile duct. We confirmed that no CBD stone remained under direct endoscopic observation.
Fig. 1.
(A) Endoscopic view showing a common-bile-duct stone captured in a basket under direct endoscopic observation. (B) Cholangiogram showing capture of the stone in a basket.
DISCUSSION
Ultra-slim upper endoscopes were introduced and used widely for unsedated transnasal EGD. The transnasal approach may be more comfortable and less stressful than the peroral approach, and some authors have reported that transnasal EGD is safer than transoral EGD, as it is associated with fewer adverse effects on cardiopulmonary function and is better tolerated by patients.1-3 Recently, direct POC4-6 and transnasal ERCP with ENBD7,8 using an ultra-slim endoscopes have been reported.
Our patient was considered suitable for direct cholangioscopy using an ultra-slim endoscope because she had a previous EST and bile duct dilation, as in reported cases.4-6,8 Moreover, the patient was old and had unstable vital signs. We thought that the transnasal approach would be more comfortable and less invasive than conventional ERCP in this patient. Another advantage of the transnasal approach is that there is no need for mouth-to-nose transfer of a drainage tube when performing ENBD because the scope is inserted via the nose.7,8
Nevertheless, several limitations to the practical utilization of ultra-slim endoscopes for biliary disease should be noted. Reported cholangioscopy or ENBD procedures using ultra-slim endoscopes are limited to patients who have had a previous EST.4-6,8 In addition, special accessories are required to guide the flexible ultra-slim endoscope into the biliary tree from the duodenum.6 Moreover, the use of instruments for diagnostic or therapeutic procedures is restricted because of the small diameter of the instrument channel.
In conclusion, with ongoing instrument development, transnasal endoscopic procedures using ultra-slim endoscopes may prove useful in various biliary diseases, as in our case.
References
- 1.Abe K, Miyaoka M. Trial of transnasal esophagogastroduodenoscopy. Dig Endosc. 2006;18:212–217. [Google Scholar]
- 2.Yagi J, Adachi K, Arima N, et al. A prospective randomized comparative study on the safety and tolerability of transnasal esophagogastroduodenoscopy. Endoscopy. 2005;37:1226–1231. doi: 10.1055/s-2005-921037. [DOI] [PubMed] [Google Scholar]
- 3.Mori A, Ohashi N, Tatebe H, et al. Autonomic nervous function in upper gastrointestinal endoscopy: a prospective randomized comparison between transnasal and oral procedures. J Gastroenterol. 2008;43:38–44. doi: 10.1007/s00535-007-2124-y. [DOI] [PubMed] [Google Scholar]
- 4.Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853–857. doi: 10.1016/j.gie.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 5.Choi HJ, Moon JH, Ko BM, et al. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos) Gastrointest Endosc. 2009;69:935–940. doi: 10.1016/j.gie.2008.08.043. [DOI] [PubMed] [Google Scholar]
- 6.Moon JH, Ko BM, Choi HJ, et al. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos) Gastrointest Endosc. 2009;70:297–302. doi: 10.1016/j.gie.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Mori A, Asano T, Maruyama T, et al. Transnasal ERCP/ENBD using an ultrathin esophagogastroduodenoscope. J Gastroenterol. 2006;41:1237–1238. doi: 10.1007/s00535-006-1911-1. [DOI] [PubMed] [Google Scholar]
- 8.Itoi T, Kawai T, Sofuni A, et al. Efficacy and safety of 1-step transnasal endoscopic nasobiliary drainage for the treatment of acute cholangitis in patients with previous endoscopic sphincterotomy (with videos) Gastrointest Endosc. 2008;68:84–90. doi: 10.1016/j.gie.2007.11.050. [DOI] [PubMed] [Google Scholar]