Summary
Haematomas in various body organs have been reported following snake bites. We report the case of a post-menopausal woman who presented with a broad ligament haematoma diagnosed two days after a viper bite which required blood transfusion and laparotomy. This rare possibility should be considered in the differential diagnosis of a woman presenting with a lower abdominal or pelvic mass, anaemia and a bleeding diathesis after a snake bite.
Keywords: Snake bite, haematoma, broad ligament
Introduction
Snake bites are common in farming communities. Ophitoxaemia refers to the clinical spectrum which may follow envenomation.1 Snakebites have two major effects. Locally, the venom causes an intense inflammation and destroys by proteolytic enzymes the vascular walls, inducing oedema, sometimes over a large area, often with blood loss. The venom proteins, when in high concentrations in the blood, cause shock, generalised symptoms such as hypotension and abdominal cramps, allergic sensitisation, coagulopathy and, rarely, death.2 Haematological changes - both local as well as systemic - are some of the commonest features of snake bite poisoning. Bleeding may occur from multiple sites3 including gums, injection sites and even as multiple petechiae and purpurae. There may be haematemesis, melaena and haematuria. In addition cerebral haemorrhage and extradural haematoma4 have also been reported. Almost every species of snake can cause renal failure.
In most cases, swelling and oedema resolve within 2 to 3 weeks. In others there may be delayed systemic manifestations. They may occasionally persist up to 3 months and in exceptional circumstances, they may also be permanent. There are records, which suggest that coagulation disturbances and neurotoxicity may persist beyond 3 weeks. Necrosis of the local tissue, resultant gangrene and the consequent cosmetic defects are obvious long term effects of ophitoxaemia. Only 1 in 20 snake bites require active emergency treatment or the administration of antivenom.5
Case Report
A 52 year old post-menopausal woman was admitted to a district hospital four hours after she had been bitten on her left ankle by a viper whilst working on her farm in the late afternoon. She had no cough or external bleeding but her saliva had been streaked with blood. Anti-snake venom was not given because it was unavailable at the time. Management consisted of local wound toileting and bandaging, antibiotics, anti-tetanus prophylaxis and analgesics. There was no collapse or other apparent systemic upset. A lower abdominal mass was noticed two days later. She became pale and was transfused with two units of whole blood. A week after initial admission she was referred to KATH, Kumasi, Ghana, for further management. There was nothing significant in her past medical history.
On review in KATH she was pale, afebrile and not jaundiced. There was no external bleeding and her saliva was clear. Her blood pressure was 120/70 mm.Hg. and pulse 70 beats per minute. Her haemoglobin was 5.4 gm/dl, bleeding time nine minutes (Normal up to 6 minutes): Prothrombin time (PT) 18 seconds (Normal 10 – 14 seconds) and Partial Thromboplastin time (PTT) 60 seconds (Normal 35 – 45 seconds).The clinical and laboratory findings all pointed to a bleeding diathesis6. A lower abdominal mass equivalent to a 16 week gravid uterus was found. An abdominal ultrasound scan revealed a hypoechoic mass in the right adnexa, but the ovary on that side was not visualized. Renal function tests were normal. Her overall clinical condition was stable and the administration of anti-snake venom was considered unnecessary.
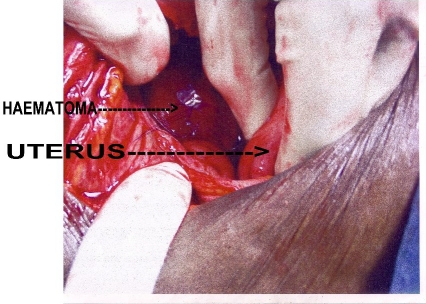
She was transfused with three units of whole blood over the next two days and the Bleeding time, PT and PTT became normal with haemoglobin of 6.0 g/dl. Six more units of whole blood were transfused over the next three days and this brought her haemoglobin up to 12g/dl. The mass remained the same size from the time of admission. An exploratory laparotomy was performed on the 12th day after the snake bite and this revealed a right broad ligament haematoma about 14cm. by12 cm (Figure 1).
Figure 1.
Right broad ligament haematoma
The uterus and ovaries were atrophic. The intestines and other pelvic organs appeared normal. A stab incision was made on the dome of the mass and enlarged to a diameter of 5cm. Blood clots filling a 500ml kidney dish were evacuated. There were no active bleeding points. A drain was placed into the cavity to monitor any further bleeding. The cavity was partially closed and the abdomen was closed in layers. The rest of her post -operative course was uneventful and she was discharged home on the 8th post-operative day. At post-discharge review two weeks later, she was well and not pale and the lower abdominal mass was absent.
Discussion
This is the first documented broad ligament haematoma following a snake bite in our unit. In this case identification of the snake was easy because other workers on the farm killed the viper and carried it to the hospital. In a study in the Brong Ahafo region of Ghana by Le Visser and Kyei-Faried7 carpet viper was the most common poisonous snake with haemorrhagic syndrome noticed in a majority of cases. Envenomation occurred as evidenced by streaks of blood in the saliva a few hours after the bite. This was followed by a coagulopathy as demonstrated by anaemia and the subsequent laboratory findings. Authors are all uniform in their opinion that delayed onset of signs is rare. In their series of 56 cases, Saini et al8 documented 4 patients who had normal clinical and laboratory coagulation profile at admission shortly following a snake bite, but started bleeding as late as 4–6 days after the bite. The possible explanation for these manifestations is that local blebs constitute a venom depot which is suddenly released into the blood stream, especially when the wound is handled surgically.
Blood changes include anaemia, leucocytosis and thrombocytopenia. Deranged coagulant activity manifested by prolonged clotting time and prothrombin time may also be evident.
In this case anti-venom was not available on presentation at the district hospital. There are specific indications for use of antivenom. Every bite, even if by poisonous species does not merit its use. The need for anti-venom is determined by severity of the envenomation and type of snake involved.9 This caution against the empirical use of antivenom is due to the risk of hypersensitivity reactions.
Therefore, antivenom is indicated only if serious manifestations of envenomation are evident viz. coma, neurotoxicity, hypotension, shock, bleeding, DIC, acute renal failure, rhabdomyolysis and ECG changes. In this environment however, where vipers are the cause of most snake bites, initial treatment should include the administration of anti-snake venom as in the standard treatment guidelines of the Ministry of Health.10
References
- 1.Ophitoxaemia - venomous snake bite. http://www.priory.com/med/ophitoxaemia.htm.
- 2.Petite J. Viper bites: treat or ignore? Swiss Med Wkly. 2005;135:618–625. doi: 10.4414/smw.2005.11198. [DOI] [PubMed] [Google Scholar]
- 3.Warrell DA, Davidson NMcD, Greenwood BM, et al. Poisoning by bites of the saw-scaled or carpet viper (Echis carinatus) in Nigeria. Quart J Med. 1977;46(181):33–62. [PubMed] [Google Scholar]
- 4.Kouyoumdjian JA, Polizelli C, Lobo SM, Guimares SM. Fatal extradural haematoma after snake bite (Bothrops moojeni) Trans R Soc Trop Med Hyg. 1991;85(4):552. doi: 10.1016/0035-9203(91)90257-y. [DOI] [PubMed] [Google Scholar]
- 5.Australian snake bites. Camperdown, Australia 2050: 2003. Medical management of snake bites. http://www.avru.org/health/health_dinax.htlm. [Google Scholar]
- 6.Hantson P, Verhelst D, Wittebole X, et al. Defibrination and systemic bleeding caused by an imported African snakebite. European Journal of Emergency Medicine. 2003 Dec;10(4):349–352. doi: 10.1097/00063110-200312000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Visser LE, Kyei-Faried S. Snake bites: A simple treatment protocol for rural areas. Ghana Med J. 2005;37(2):57–61. [Google Scholar]
- 8.Saini RK, Sharma S, Singh S, Pathania NS. Snake bite poisoning: A preliminary report. J Assoc Phys India. 1984;32(2):195–197. [PubMed] [Google Scholar]
- 9.Jorden RC, Pollack CV., Jr . Bites and Stings. In: Kravis TC, Warner CG, Jacobs LM Jr, editors. Emergency Medicine (A comprehensive review) 3rd Edition. New York 10036, U.S.A.: Raven Press; 1993. pp. 627–649. [Google Scholar]
- 10.Ministry of Health Standard Treatment Guidelines. Ghana: Ministry of Health; 2004. pp. 454–456. [Google Scholar]