Abstract
To describe an asthma management protocol used in a nurse-staffed pediatric After-Hours Call Center (AHCC) that incorporates severity-based home treatment recommendations and follow-up call assessments. Call records for asthma advice from January 1, 2004 to June 30, 2004 were identified retrospectively and reviewed. Descriptive statistics were used to report patient demographics, frequencies of symptom severity zones (Red, Yellow, or Green) at initial calls, frequencies of call dispositions designating care advice provided (including home treatment recommendations and seeking emergency department [ED] care), and changes in severity zones between initial calls and follow-up calls when nurses reassessed patients after recommended home treatment. During the study period, 3,632 asthma calls (2,439 initial; 1,193 follow-up) were managed by AHCC nurses. Initial calls were classified mostly as Red (28%) or Yellow (42%) severity zones; 27% were Green zone and 3% could not be categorized. Fifty-two percent of initial calls with Red or Yellow severity zones involved home treatment recommendations; 50% of those Red zone and 63% of those Yellow zone calls had improved severity zones at follow-up call assessments. Twenty-eight percent of patients with home treatment recommendations were referred to the ED at the time of follow-up call nurse reassessment. This telephone-based nurse-staffed pediatric acute asthma management protocol includes provision of severity-based home treatment recommendations and follow-up assessments, and improved symptoms for many children with acute exacerbations. This protocol may also be successful in other locations and may improve outcomes, such as reduction in ED visits.
Key words: asthma, child, call center
Introduction
In the United States, over two million children with asthma have at least one exacerbation per year, and more than 700,000 emergency department (ED) visits occur annually for this age group.1 The National Asthma Education and Prevention Program (NAEPP) guidelines recommend early and aggressive treatment of acute symptoms.2 However, many parents of children with asthma lack written action plans or do not refer to them, and they need assistance in recognizing symptom severity and understanding management details.3–10
Call centers staffed by registered nurses (RNs) frequently provide after-hours pediatric advice as an alternative to direct consultation with on-call physicians. Several pediatric studies report that telephone consultation and advice by nurses is safe, effective, and associated with parental satisfaction.11–15 These studies generally describe the advice in disposition categories of urgent referral, see a physician the next day, or provide home care.12 The publications on effectiveness provide no specific information on the approach to asthma calls. The Pediatric After-Hours protocol for an asthma attack (Barton Schmitt, M.D.)16 involves categorization of the episode as mild, moderate, severe, or respiratory arrest imminent. Advice based on severity includes calling 911, going to the ED now, seeing the primary care provider (PCP) within 4 hours, and urgent home treatment when the child has continuous wheezing or coughing and an available short-acting bronchodilator has not yet been used. Urgent home treatment involves the parent giving a short-acting bronchodilator dose immediately and a second dose 20 minutes later. When such home treatment is advised, a follow-up telephone contact after an interval such as 30 minutes depends on the call center–specific protocol for either a nurse to call back to reassess and determine whether the child has improved or a suggestion for the parent to call with a report on the child's response. If the condition is “unchanged or worse,” the family is referred to the ED. If the condition is “improved or resolved,” continued home care advice is provided.
There are no publications of outcomes of advice for such asthma care by telephone, nor any details on parent actions taken in the interim between initial and follow-up calls. This article describes an asthma advice protocol utilized at a nurse-staffed pediatric after-hours call center (AHCC) associated with a tertiary-care university-affiliated urban children's hospital. This protocol is unusual among asthma protocols used by pediatric call centers in that it involves provision of severity-based home treatment recommendations, including permission for the nurse to prescribe use of oral corticosteroids, and follow-up reassessments initiated by the nurse. Our report includes analysis of parent actions regarding the home treatment provided after nurse recommendations for a randomly selected set of calls.
After-Hours Call Center
St. Louis Children's Hospital (SLCH), a tertiary-care university-affiliated children's hospital, has offered an AHCC since 1996. The AHCC is staffed by approximately 60 RNs who provide telephone coverage for calls from 4:30 PM to 8:00 AM Monday through Friday and 24 hours on weekends and holidays. Approximately 65 regional practices including 180 physicians in a 250-mile radius of the hospital utilize the service, and the AHCC receives approximately 85,000 calls annually. The AHCC uses a computerized triage system with advice protocols, and asthma is one of the most common reasons for calls, accounting for up to 10% of calls during seasonal increases.
Asthma Protocol
The asthma protocol used by this AHCC was adapted from the NAEPP Expert Panel Report 2 section on home treatment during management of acute asthma exacerbations,2 referencing the Pediatric Telephone Protocols (Barton Schmitt, M.D.),16 and with input from the AHCC Physician Advisory Board, members of the Washington University School of Medicine Division of Pediatric Allergy and Pulmonary Medicine, and AHCC staff nurses. This protocol involves evidence-based treatment recommendations and is routinely reviewed and updated. It is used for patients who by parent report have asthma and have previously been treated with albuterol. There are two specific versions of the protocol: “Asthma” for initial calls for the particular exacerbation and “Asthma Follow-Up” for follow-up calls.
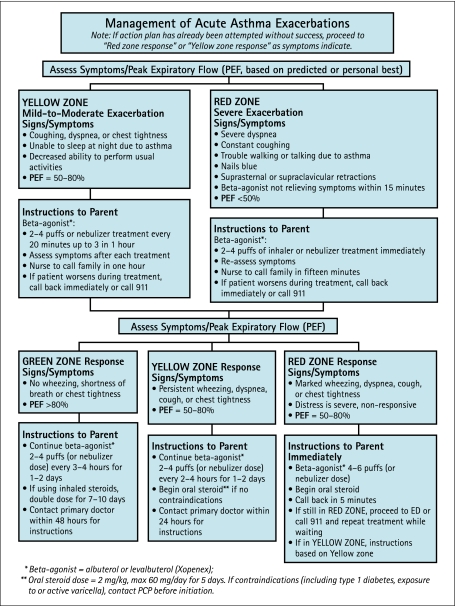
After initial assessments based on symptoms, history, and peak expiratory flow rate results (as appropriate based on age and condition), trained nurses categorize the severity of the exacerbation into one of nine call dispositions that correspond to severity zones (Red, Yellow, or Green) (Table 1) and they advise appropriate management (Fig. 1). For the most severe symptoms, they instruct parents to call 911 or proceed immediately to an ED. For particular patients with moderate-to-severe symptoms and available rescue medicines (albuterol or leval-buterol), they recommend home treatment and call the parents back to reassess after appropriate time intervals. The nurses have standing severity-based orders to instruct parents to administer oral corticosteroids (OCS) if available at home, or they may call pharmacies and prescribe OCS on behalf of participating PCPs. Prior to advising administration of OCS, they inquire regarding contraindications, which would prompt contact with the PCP for discussion. The nurses also have standing orders to similarly prescribe refills for rescue medicine. Ninety-five percent of participating PCPs have approved initiation of available OCS and prescriptions as indicated. Five percent did not sign the standing order document, having specific management requests; calls from patients of these PCPs are referred immediately to the PCPs (the disposition of “Call PCP Now”). For all calls, nurses advise PCP follow-up during regular office hours, and documentation of the call details is faxed to PCPs within 24 hours.
Table 1.
Call Dispositions and Associated Severity Zones
| Disposition | Details | Severity Zone |
|---|---|---|
| Call EMS 911 Now | Severe distress; signs of respiratory or circulatory compromise or mental status change; unable to speak or cry; cyanosis; wheezing or distress due to allergic reaction | Red |
| Go to ED Now | Red zone; <6 months old; OCS started >2 hours ago; leave immediately | Red |
| Emergent Home Treatment with Follow-Up Call | Red zone; >6 months old; OCS started <2 hours ago | Red |
| Urgent Home Treatment with Follow-Up Call | Yellow zone; >6 months old; receiving albuterol every 4 hours for >48 hours; back-to-back treatments and/or OCS may not have been attempted yet | Yellow |
| See Physician Within 1 Hour (or PCP Triage) | Signs of dehydration, fever, or severe chest pain; RN judgment–may recommend leave for ED as soon as possible or within 3-4 hours; RN may page PCP | Yellow |
| See Physician Within 4 Hours (or PCP triage) | ||
| See PCP Within 24 Hours | Yellow zone; >6 months old; not receiving frequent treatments | Yellow |
| See PCP When Office is Open (Within 3 Days) | Green zone and mild symptoms | Green |
| See PCP Within 2 Weeks | Not in an exacerbation but complaining of asthma symptoms interfering with activities or sleep | Green |
| Call PCP Now | Usually Red or Yellow zone; some reasons not related to severity; significant asthma history (intubations, intensive care); significant comorbid factors or other chronic conditions; PCP has not authorized prescription of OCS; child participating in asthma research study | Red or Yellow or Green |
EMS, emergency medical system; ED, emergency department; PCP, primary care physician; OCS, oral corticosteroids.
Fig. 1.
Flow chart for asthma management (yellow and red zone calls). PCP, primary care provider.
For the “Emergent Home Treatment with Follow-Up Call” disposition, nurses instruct parents to administer single doses of rescue medicine (2–4 puffs of metered-dose-inhaler with valved holding chamber or usual nebulizer dose) and begin OCS if available. The nurses call back after approximately 15 minutes to assess response to treatment. If Red zone symptoms persist, they instruct parents to proceed immediately to an ED or call 911.
For the “Urgent Home Treatment with Follow-Up Call” disposition, nurses instruct parents to administer up to three doses of rescue medicine during 1 hour and they call back after approximately 1 hour to reassess. Parents are to assess symptoms after each treatment; if symptoms worsen, they are to call back immediately or call 911. If the nurses find that the response to rescue medicine is good (Green zone), they advise continuation of short-acting bronchodilator doses every 3–4 hours for 24–48 hours, doubling of inhaled corticosteroids (ICS) for 7–10 days (if already prescribed and available), and contacting the PCP within 48 hours (doubling of ICS was included in the protocol at the time of the study, but was removed during the most recent protocol review based on the most recent NAEPP Expert Panel Report).17 If the nurses find that response to treatment is incomplete (Yellow zone), they advise continuation of rescue medicine every 2–4 hours, beginning OCS, and contacting the PCP within 24 hours. If the response is poor (Red zone), nurses instruct parents to proceed immediately to an ED or call 911.
The process involves dialogue between the nurses and parents. Nurses may decide not to recommend home management based on their judgment of the child's severity and the parents' capability of carrying out and comfort with following the plan.
Materials and Methods
Study Design
This descriptive study involved retrospective review of call records for asthma in the AHCC database during a 6-month period (January 1, 2004–June 30, 2004). The university Human Research Protection Office affiliated with the study hospital approved this study.
Demographics
Demographic information routinely collected by the AHCC includes date of birth, gender, and location (zip code), but not race or ethnicity. The study hospital is located within St. Louis City and serves the metropolitan area; zip codes were categorized based on proximity to the hospital as urban, suburban, and rural. Demographics were compared among initial call severity zones.
Severity Zones and Home Treatment Recommendations
Severity zones (Red, Yellow, or Green) were based on assigned call dispositions (Table 1). Most calls were managed by the nurses without input by the PCPs at the time of the call. Reasons for “Call PCP Now” designation are given in Table 1, and most were related to individual PCP preference to be involved in decision making.
The numbers of calls for a particular exacerbation varied depending on initial dispositions. If the initial call involved immediate ED referral or emergency medical services activation or did not involve home treatment recommendation and nurse follow-up call, no follow-up calls were expected, and final disposition was the same as initial calls. If calls were assigned dispositions involving home treatment recommendations and nurse follow-up call, at least two total calls were expected, with final dispositions assigned during final follow-up calls.
The AHCC database is not designed to specifically link initial and follow-up calls. In practice, upon completion of an initial call, the nurse has the option to place the completed call in a “call-back” queue. For the purpose of this study, follow-up calls were linked to initial calls within the database by identifying duplications of names and dates of birth that occurred within 12 hours of initial calls (a time interval presumed to include all necessary follow-up calls). Twenty-four percent of initial calls expected to have follow-ups were not able to be linked to any follow-up calls, perhaps because no follow-up calls occurred due to inability to re-contact parents, possibly because they had sought ED care, or because of human error in logging calls or incorrect disposition assignments.
A randomly selected subset of approximately 15% of records for initial calls involving home treatment recommendations (“Emergent Home Treatment with Follow-Up Call” or “Urgent Home Treatment with Follow-Up Call” dispositions) and their linked follow-up calls were hand-audited to verify accuracy of change in severity zone as discerned from examination of dispositions in the database and to collect information about available home medications and parent self-reported adherence to treatment recommendations.
Emergency Department Visits and Hospitalizations
In order to obtain some limited information about ED visits and hospitalizations occurring after AHCC calls, the study hospital medical records database was reviewed for asthma visits identified by the 493. XX diagnosis code (International Classification of Diseases, [ICD]-9). We hypothesized that the hospitalization rate for children seeking ED care after an AHCC call would not be greater than the overall asthma-related hospitalization rate. The asthma-related hospitalization rate for children who had AHCC calls during the twenty-four hours preceding the ED visit was compared to that of all children with ED asthma visits during the study period. SLCH accounts for 70% of all asthma-related hospitalizations among children in the St. Louis metropolitan area, the area from which approximately 75% of call calls originated.
Statistical Analysis
The SAS version 9.1.3 statistical software (SAS Institute, Inc., Cary, NC) was used for data analysis. Data are reported as mean (standard deviation) for continuous variables and as number (percentage) for categorical variables. Proportions were compared between groups using independent t-tests for continuous data and either χ2 or Fisher's exact tests for categorical or nominal data. P-values <0.05 were considered statistically significant.
Results
Child Demographics
During the 6-month study period, 3,632 calls for asthma advice for 2,003 children were managed by AHCC nurses; this total included 2,439 initial and 1,193 follow-up calls. The median number of initial calls/child was 1 (range = 1–7); 83% of children had only 1 initial call, 12% had 2, and 5% had 3 or more. Fifty-nine percent of calls involved male and 36% involved female children; 5% were missing information about gender. Mean age was 5.4 ± 4.3 years. Twelve percent of children were from urban zip codes, 61% were from suburban zip codes, and 25% were from rural zip codes. Demographics were similar according to initial call severity zone (Table 2).
Table 2.
Demographics According to Initial Severity Zone
| Red | Yellow | Green | |
|---|---|---|---|
| Age, years | n = 688 | n = 1027 | n = 656 |
| Mean (SD) | 5.17 ± 4.23 | 5.88 ± 4.45 | 5.01 ± 4.12 |
| Gender | n = 649 | n = 977 | n = 633 |
| Male | 405 (62%) | 593 (61%) | 394 (62%) |
| Female | 244 (38%) | 384 (39%) | 239 (38%) |
| Zip code | n = 688 | n = 1027 | n = 656 |
| Urban | 66 (9%) | 157 (15%) | 73 (11%) |
| Suburban | 438 (64%) | 619 (60%) | 398 (61%) |
| Rural | 171 (25%) | 236 (23%) | 178 (27%) |
| Missing | 13 (2%) | 15 (2%) | 7 (1%) |
SD, standard deviation.
Severity Zones and Home Treatment Recommendations
Among all initial calls, Red zone severity was assigned for 688 (28%), with advice to call 911 or immediately proceed to ED for 208, and “Emergent Home Treatment with Follow-Up Call” dispositions for 324. The remaining 156 had the disposition of “Call PCP Now.” Yellow zone severity was assigned for 1,027 (42%) of initial calls, with “Urgent Home Treatment with Follow-Up Call” dispositions for 948. The remaining 79 Yellow zone calls involved recommendations to be evaluated by a physician within 1 or 4 hours or their PCP within 24 hours or “Call PCP Now.” Green zone severity was assigned for 656 (27%) initial calls, during which parents were counseled about asthma and advised to follow up with the PCP. Three percent of initial calls could not be categorized into one of the three severity zones due to missing data.
Among initial calls with Red zone designation and “Emergent Home Treatment with Follow-Up Call” disposition, 37% improved (8% to Yellow zone and 29% to Green zone), 33% had no change in zone, and 30% had missing follow-up data (Table 3). Among initial calls with Yellow zone designation and “Urgent Home Treatment with Follow-Up Call” disposition, 72% improved to Green zone, 4% worsened to Red zone, 2% had no change, and 22% had missing follow-up data (Table 3). If it is assumed that those calls with missing information about follow-up calls did not improve, 37% with “Emergent Home Treatment with Follow-Up Call” dispositions and 72% with “Urgent Home Treatment with Follow-Up Call” dispositions had improvement in severity zones, and the overall improvement rate was 63% among calls with home treatment recommendations.
Table 3.
Changes in Severity Zones at Follow-Up Calls for Initial Calls with Dispositions of “Emergent Home Treatment with Follow-Up Call” (Red Zone) or “Urgent Home Treatment with Follow-Up Call” (Yellow Zone)
| No. (%) | ||
|---|---|---|
| Red zone (n = 324) | Red-Red | 107 (33%) |
| Red-Yellow | 25 (8%) | |
| Red-Green | 94 (29%) | |
| Missing data for follow-up calls | 98 (30%) | |
| Yellow zone (n = 948) | Yellow-Red | 37 (4%) |
| Yellow-Yellow | 15 (2%) | |
| Yellow-Green | 686 (72%) | |
| Missing data for follow-up calls | 210 (22%) |
One-hundred-seventy-two sets of initial calls with dispositions of “Emergent Home Treatment with Follow-Up Call” or “Urgent Home Treatment with Follow-Up Call” and their linked follow-up calls were randomly selected for hand-audit. Five were excluded due to the following reasons: (1) initial Green zone with no home treatment, (1) unable to locate corresponding database file, and (3) children with a second call during the study period. Results of analysis of the remaining 167 are reported in Table 4. Seventy-eight percent of children were reported to have received albuterol during the preceding 24 hours and 20% were reported to have OCS available at home. At the time of the follow-up calls by the nurses, 95% of children were reported to have received treatments as recommended by the nurses (range of albuterol treatments = 2–7) and 16% were reported to have received OCS. Overall, 50% of Red zone calls and 63% of Yellow zone calls had improvement in severity zones. Twenty-eight percent of the hand-audited calls involved referral to the ED upon follow-up reassessment by the nurses.
Table 4.
Details of Hand-Audited Initial Calls with Initial Call Dispositions of “Emergent Home Treatment with Follow-Up Call” (Red Zone) or “Urgent Home Treatment with Follow-Up Call” (Yellow Zone) and Linked Follow-Up Calls
| n = 167 | |
|---|---|
| Initial call severity zone | |
| Red zone | 78 (47%) |
| Yellow zone | 89 (53%) |
| Any albuterol treatments given during previous 24 hours | 131 (78%) |
| Number of albuterol treatments, mean (standard deviation) | 1.2 (0.5) |
| Oral steroids given during previous 24 hours | 12 (7%) |
| Oral steroids currently available in home | 33 (20%) |
| Number of calls (initial to final)-median (IQR), range | 2 (1), 2–7 |
| Number of albuterol treatments given since initial call-mean (SD) | 2.2 (1) |
| Oral steroids given since initial call | 27 (16%) |
| Treatments given as recommended | 158 (95%) |
| Referred to an emergency department during follow-up call | 47 (28%) |
| Initial-to-final severity zone change | |
| Red-Red | 39 (50%) |
| Red-Yellow | 15 (19%) |
| Red-Green | 24 (31%) |
| Yellow-Red | 4 (4%) |
| Yellow-Yellow | 29 (33%) |
| Yellow-Green | 56 (63%) |
IQR, interquartile range; SD, standard deviation.
Emergency Department Visits and Hospitalizations
During the study period, 203 children with AHCC calls had asthma-related ED visits at the study hospital within 24 hours of their calls; 31/203 (15.3%) (95% confidence interval [CI] 10.6%, 21.0%) were hospitalized. The overall asthma-related hospitalization rate during the study period was similar: 649/4,541 (14.3%) (95% CI 13.3%, 15.3%).
Discussion
This article describes a nurse-staffed pediatric acute asthma management protocol of an AHCC associated with a university-affiliated tertiary-care children's hospital. Using this protocol, trained nurses provide symptom- and severity-based advice for parents of children with acute exacerbations, often recommending home treatment and providing follow-up assessments of response to treatment and determination of final disposition.
The majority of asthma calls to the AHCC were for symptoms corresponding to Red and Yellow zone severities. More than half of initial calls involved nurse-directed home treatment recommendations and nurse reassessments during follow-up calls. Over 60% of children were improved at the time of follow-up call reassessments after home treatment, including 37% of initial Red zone and 72% of initial Yellow zone calls. These improvement rates were substantiated by the detailed hand-audit, which also revealed that most parents (95%) reported administering treatments as recommended. Overall, less than one third of initial Red or Yellow zone severity calls involving home treatment were referred to the ED at the time of reassessment. These results suggest that the nurses' assessments, dispositions, and home care recommendations were appropriate, and that many children benefited from this directed home treatment.
Although this descriptive study was not designed to evaluate a reduction in ED visits, the fact that the majority of children had improvement in severity zones after home treatment suggests that some ED visits may have been avoided as a result of this directed home management. Our data for ED visits within 24 hours after AHCC calls are limited because they only involved visits to the study hospital, and children may have had care at other area EDs. Two-hundred-three children with AHCC calls during the study period (8% of all initial calls) had ED visits at the study hospital within 24 hours of an AHCC call, and the hospitalization rate from the ED was similar to that for all children with asthma-related ED visits during the study period.
In addition to recommending home treatment with inhaled short-acting β-agonist medication, this protocol also includes recommendations to begin OCS for selected patients, consistent with NAEPP guidelines recommending OCS for patients with acute exacerbations who have incomplete responses to initial inhaled β-agonists.2,3 OCS are associated with reduced hospitalization rates for acute asthma exacerbations and are recommended to be administered as soon as possible for moderate and severe acute exacerbations.18 Ninety-five percent of PCP subscribers to the AHCC allow the RNs to telephonically prescribe OCS and refill β-agonist prescriptions on their behalf. In the sample included in this review, 16% of children were reported to have received OCS during the interval between the initial and follow-up calls. Although the data were not analyzed regarding improvement according to receipt of OCS, it is possible that this evidence-based clinical practice may prevent ED visits and hospitalizations.
This descriptive study has some limitations. This was a retrospective review of a computerized protocol database designed for clinical use. Some data were recoverable with difficulty from free text fields, and some data were missing. Because of this, a hand-audit of randomly selected records was completed and verified the general results. The data collected by the AHCC are parental report with inherent limitations and were not verified by direct examination of patients. The AHCC is affiliated with an urban children's hospital that treats approximately 60,000 patients per year in the emergency department and serves a metropolitan area of nearly 2.8 million people. The AHCC collects limited demographic information, and the study population involves mainly suburban and rural patients. These factors may limit generalizability to other groups of patients.
The AHCC is a resource not only for parents of children with asthma but also for PCPs who appreciate that their patients receive appropriate assessment and timely management. Both parents and PCPs consistently report high satisfaction with the care delivered by the AHCC. This acute asthma management protocol includes evidence-based treatment recommendations, is endorsed by local asthma specialists, and is subject to ongoing quality assessment. Despite the limitations in this review, these results substantiate the protocol design and use.
In conclusion, this telephone-based pediatric acute asthma management protocol involves evidence-based recommendations and follow-up assessments, and the results of this review suggest that most children experiencing this nurse-directed home management have improvement after the recommended treatment. It is possible that this protocol may result in improved asthma-related outcomes beyond the telephone calls, including fewer acute-care visits to PCPs and EDs, and it may be successful in other cities.
Acknowledgments
This study was funded by a grant from the National Heart Lung Blood Institute (HL 072919).
Disclosure Statement
No competing financial interests exist.
References
- 1.Akinbami L. Centers for Disease Control and Prevention National Center for Health Statistics. The state of childhood asthma, United States, 1980–2005. Adv Data. 2006;3811:24. [PubMed] [Google Scholar]
- 2.National Asthma Education and Prevention Program. Expert panel report 2: Guidelines for the diagnosis and management of asthma. Bethesda, MD: National Institutes of Health, National Heart Lung Blood Institute; Apr, 1997. publication no. 97-4051. [Google Scholar]
- 3.Butz AM. Huss K. Mudd K. Donithan M. Rand C. Bollinger ME. Asthma management practices at home in young inner-city children. J Asthma. 2004;41:433–444. doi: 10.1081/jas-120033985. [DOI] [PubMed] [Google Scholar]
- 4.Scarfone RJ. Zorc JJ. Capraro GA. Patient self-management of acute asthma; adherence to national guidelines a decade later. Pediatrics. 2001;108:1332–1338. doi: 10.1542/peds.108.6.1332. [DOI] [PubMed] [Google Scholar]
- 5.Butz AM. Syron L. Johnson B. Spaulding J. Walker M. Bollinger ME. Home-based asthma self-management education for inner city children. Public Health Nurs. 2005;22:189–199. doi: 10.1111/j.0737-1209.2005.220302.x. [DOI] [PubMed] [Google Scholar]
- 6.Reeves MJ. Bohm SR. Korzeniewski SJ. Brown MD. Asthma care and management before an emergency department visit in children in western Michigan: How well does care adhere to guidelines? Pediatrics. 2006;117:S118–S126. doi: 10.1542/peds.2005-2000I. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein JA. Lozano P. Farber HJ. Miroshnik I. Lieu TA. Underuse of controller medications among Medicaid-insured children with asthma. Arch Pediatr Adolesc Med. 2002;156:562–567. doi: 10.1001/archpedi.156.6.562. [DOI] [PubMed] [Google Scholar]
- 8.Fernands AK. Mallmann F. Steinhorst AM. Nogueira FL. Avila EM. Saucedo DZ, et al. Characteristics of acute asthma patients attended frequently compared with those attended only occasionally in an emergency department. J Asthma. 2003;40:683–690. doi: 10.1081/jas-120023487. [DOI] [PubMed] [Google Scholar]
- 9.Lieu TA. Quesenberry CP. Capra AM. Sorel ME. Martin KE. Mendoza GR. Outpatient management practices associated with reduced risk of pediatric asthma hospitalization and emergency department visits. Pediatrics. 1997;100:334–341. doi: 10.1542/peds.100.3.334. [DOI] [PubMed] [Google Scholar]
- 10.Warman KL. Silver EJ. McCourt MP. Stein RE. How does home management of asthma exacerbations by parents of inner-city children differ from NHLBI guideline recommendations? National Heart, Lung, and Blood Institute. Pediatrics. 1999;103:422–427. doi: 10.1542/peds.103.2.422. [DOI] [PubMed] [Google Scholar]
- 11.Lattimer V. George S. Thompson F. Thomas E. Mullee M. Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: Randomized controlled trial. The South Wiltshire Out of Hours Project (SWOOP) Group. BMJ. 1998;317:1054–1059. doi: 10.1136/bmj.317.7165.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kempe A. Dempsey C. Whitefield J. Bothner J. MacKenzie T. Poole S. Appropriateness of urgent referrals by nurses at a hospital-based pediatric call center. Arch Pediatr Adolesc Med. 2000;154:355–360. doi: 10.1001/archpedi.154.4.355. [DOI] [PubMed] [Google Scholar]
- 13.Frisbee SJ. Malloy M. Meurer JR. Kuhagen KA. Kini NM. Urban Wisconsin pediatric patients using an after-hours telephone triage service: Outcomes and compliance. WMJ. 2001;100:55–58. [PubMed] [Google Scholar]
- 14.Lee TJ. Baraff LJ. Buzy J. Johnson D. Woo H. Does telephone triage delay significant medical treatment? Advice nurse service vs on-call pediatricians. Arch Pediatr Adolesc Med. 2003;157:635–641. doi: 10.1001/archpedi.157.7.635. [DOI] [PubMed] [Google Scholar]
- 15.Kempe A. Luberti AA. Hertz AR. Sherman HB. Amin D. Dempsey C, et al. Delivery of pediatric after-hours care by call centers: A multicenter study of parental perceptions and compliance. Pediatrics. 2001;108:E111. doi: 10.1542/peds.108.6.e111. [DOI] [PubMed] [Google Scholar]
- 16.Schmitt BD. Pediatric telephone protocols: After hours version. Mesa, AZ: LVM Systems; 1994–2008. Asthma attack protocol. [Google Scholar]
- 17.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma—Summary report 2007. J Allergy Clin Immunol. 2007;120:S94–S138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 18.Rowe BH. Spooner C. Ducharme FM. Bretzlaff JA. Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001;1:CD002178. doi: 10.1002/14651858.CD002178. [DOI] [PubMed] [Google Scholar]