Abstract
People aged 80 or older are the fastest growing population in high-income countries. One of the most common causes of death among the elderly is the cardiovascular disease (CVD). Lipid-lowering treatment is common, e.g. one-third of 75–84-year-old Swedes are treated with statins [ 3]. The assumption that hypercholesterolaemia is a risk factor at the highest ages seems to be based on extrapolation from younger adults. A review of observational studies shows a trend where all-cause mortality was highest when total cholesterol (TC) was lowest (‘a reverse J-shaped’ association between TC and all-cause mortality). Low TC (<5.5 mmol/l) is associated with the highest mortality rate in 80+-year olds. No clear optimal level of TC was identified. A review of the few randomised controlled trials including 80+-year olds did not provide evidence of an effect of lipid-lowering treatment on total mortality in 80+-year-old people. There is not sufficient data to recommend anything regarding initiation or continuation of lipid-lowering treatment for the population aged 80+, with known CVD, and it is even possible that statins may increase all-cause mortality in this group of elderly individuals without CVD.
Keywords: cholesterol, aged, 80+-year olds, lipid-lowering treatment and all-cause mortality, elderly
Introduction
The fastest growing part of the population in high-income countries is people aged 80 or older. In Japan, the probability of living from 80 to 90 now exceeds 50% for women [1]. One of the most common causes of death among the elderly is cardiovascular disease (CVD), and a common general assumption is that different CVD risk factors (hypertension, smoking, diabetes, BMI, hypercholesterolaemia) remain risk factors at the highest ages. For hypertension, this assumption was confirmed by the HYVET study, which showed better survival when treated with anti-hypertensive drugs in the elderly [2].
High cholesterol is a well-documented risk factor among middle-aged and ‘young elderly’ (people aged 60–70), and statins (lipid-lowering treatment) are one of the most common prescription drugs in high-income countries. One-third of people aged 75–84 are treated with statins in the Swedish population [3], and there is no reason to believe that this prevalence of statin treatment should be much different in other high-income countries. Within a few years, the ‘young elderly’ patients treated with statins will belong to the population of 80+-year olds, and a key question is whether they should continue the lipid-lowering treatment at the highest ages and whether treatment should be initiated among 80+-year olds.
The association between total cholesterol (TC) and mortality among people aged 65 and above has previously been reviewed [4–7]. Although few studies in these reviews included participants older than 80 years, they concluded that high-risk elderly should be treated with statins [4–7]. A meta-analysis based on observational studies included 70–89-year-old participants, focused as the previous reviews on CVD mortality, found low TC associated with a low ischaemic heart disease mortality and a high non-vascular mortality, but no association with total mortality was described [8]. In 2004, Anum and Adera reviewed observational studies regarding the association between TC and coronary heart disease (CHD) mortality in persons aged 65 and above. A positive association between TC and CHD mortality was found in men, but no association with all-cause mortality was found in either gender [9]. A possible inverse relationship between TC and all-cause mortality in 80+-year-old men was suggested, but only three studies regarding the 80+-year olds and all-cause mortality were included in this review [9].
Among 80+-year olds, the cause of death is less certain than among middle-aged and young elderly, due to multi-morbidity. Therefore, the focus of this review of 80+-year olds is total mortality. CVD mortality is less reliably measured than total mortality, and although CVD mortality is the most common cause of death in this age group, it is expected to be detectable in total mortality, if any association between TC and CVD mortality is present. A new review with focus on all-cause mortality's association with TC among 80+-year olds is needed.
The aim of this review of recent studies was to shed light on the following questions.
What is the optimal level of cholesterol in the 80+-year olds for total mortality?
Should lipid-lowering treatment among 80+-year-old patients be initiated and continued?
What is the optimal level of cholesterol in the 80+-year-olds for total mortality?
To answer this question, we included observational studies based on the search strategy described in Figure 1.
Figure 1.
Search strategy and selection criteria.
TC and total mortality
A total of 12 articles regarding TC and all-cause mortality were included. This corresponded to 13,622 participants: 3,789 aged 80 and above in eight studies [10–17] and 9,833 aged 71–103 (mean age 78 years) in four studies (the exact number of 80+-year-olds was not given) [18–21] (Table 1).
Table 1.
Observational studies
| Authors, year | Number of 80+ years old | Number of years in follow-up | Mortality/outcome | Findings | Comments |
|---|---|---|---|---|---|
| Casiglia et al, 1993 [10] | 318 | 7 years | CVD and all-cause mortality | TC negative associated with CVD and total mortality | Survival bias, selection |
| Clarke et al., 2007 [22] | 187 | 7 years | IHD mortality | TC not associated, but TC/HDL positively associated with IHD mortality | Only men included |
| Corti et al., 1995 [24] | 1,239 | 4.4 years | CHD mortality | HDL and CHD mortality negatively associated | U-shaped association between TC and CHD mortality |
| Corti et al., 1997 [23] | 4,066 (≥71 years) | 5 years | CHD mortality | TC and CHD mortality positively associated | After adjustment, negative association disappeared |
| Dontas et al., 1996 [11] | 287 | 5 years | All-cause mortality | TC and all-cause mortality negatively associated | Participants all entering a residential home |
| Foody et al., 2003 [12] | 599 | 6 years | All-cause mortality | No association between elevated TC and all-cause mortality | Elderly survivors of AMI included |
| Jonsson et al., 1997 [13] | 105 | 14 years | All-cause mortality | An inverted U-shaped association between TC and total mortality | Random sample of 80+-year old in Reykjavik |
| Koropatnick et al., 2008 [27] | 3,562 (71–93-year old), mean 78 years | 8 years | All-cause and CVD mortality | HDL and CVD mortality negative associated, but no association with all-cause mortality | No measure of TC |
| Kronmal et al., 1993 [14] | 622 | years | CHD, non-CHD and all-cause mortality | TC and total mortality and CHD mortality was negatively associated | From the Framingham population |
| Krumholz et al., 1994 [18] | 997 (71–104-year old), mean 78/79 | 4 years | CHD and all-cause mortality | No association between TC and all-cause mortality | No association between TC and CHD mortality |
| Landi et al., 2008 | 359 | 2 years | All-cause mortality | HDL and all-cause mortality negatively associated | Selective survival? |
| Nikkila and Heikkinen, 1990 [15] | 535 | 5 years | All-cause mortality | J-shaped relation between TC and all-cause mortality | Negative association between HDL and all-cause mortality |
| Raiha et al., 1997 [25] | 66 | 11 years | Vascular and non-vascular mortality | TC and non-vascular mortality negatively associated | No association between TC and vascular mortality |
| Schatz et al., 2001 [19] | 3,572 (71–93-year old), mean 78 | 3–5 years | All-cause mortality | TC and all-cause mortality negatively associated | Long-term low TC increased the risk of death |
| Schupf et al., 2005 [20] | 1,136 ≥75 years | 3 years | All-cause mortality | TC and all-cause mortality negative associated | Low TC a surrogate for frailty? |
| Volpato et al., 2001 [21] | 4.128 (70–103-year old), mean 78.7 | 4.9 years | All-cause mortality | TC and all-cause mortality negatively associated | Adjustment for HDL and albumin eliminated this association |
| Weverling-Rijnsburger et al.,1997 [16] | 724 | 10 years | All-cause and CVD mortality | TC and all-cause mortality negatively associated , no association with CVD mortality | 1 mmol/l increase in TC reflect a 15% mortality decrease |
| Weverling-Rijnsburger et al., 2003 [17] | 599 | 4 years | All-cause and CVD mortality | TC and all-cause mortality negatively associated | Low HDL a risk factor for CVD mortality |
| Zimetbaum et al., 1992 [26] | 350 (75–85-year old), mean 79 years | 10 years | CVD mortality | HDL and CVD mortality negatively associated in men | No association in women |
HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol; IHD, ischaemic heart disease; AMI, acute myocardial infarction.
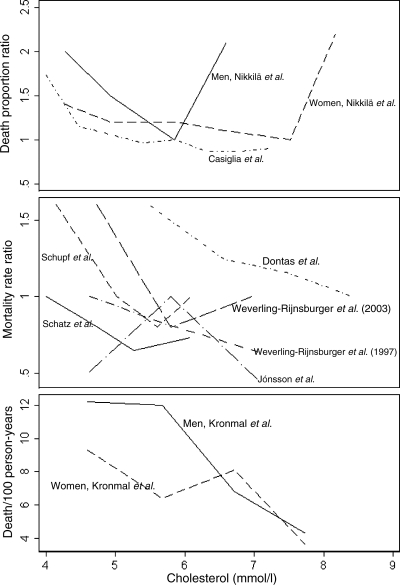
Figure 2, showing the relation between TC and total mortality, was drawn on the basis of nine studies. The three studies not included did not report specific calculations of the total mortality risk in relation to the TC in the 80+-year-old participants in their studies [12, 18, 21]. The association between TC and total mortality was not simple and was further complicated by different effect measures used in the studies: death proportion ratio, mortality rate ratio or death/100 person-years, respectively [10, 11, 13–17, 19, 20]. The association could prevailingly be described as ‘a reverse J-shaped’ association, where low TC was associated with the highest total mortality in the population of 80+-year olds. Most of the observational studies found this trend of association, whereas a few found a U-shaped association, where high TC was associated with increasing mortality as well [15, 17, 20]. As seen in Figure 2, five studies found either a less steep falling gradient at the highest level of TC or an almost flat curve, with an almost constant level of mortality from around the intermediate level of TC [10, 11, 14, 16, 19]. Regarding all-cause mortality in the 80+-year olds, low TC did not seem beneficial in any study, whereas the association with high TC seemed less consistent in the studies, and this association could in the majority of cases be described as ‘a reverse J-shaped’ configuration, as illustrated in Figure 2. Although a general tendency was that the lower level of TC (<5.5 mmol/l) was associated with higher mortality, most of the studies describing this shape of association found the lowest mortality around TC at 6 mmol/l [10, 15, 17, 19].
Figure 2.
All-cause mortality and cholesterol in the elderly. At the x-axis, the cholesterol was plotted as an exact measure of TC (mmol/l), even though most studies had each point responding to an interval of cholesterol, where we chose the middle of this interval as the point to plot. In the top panel, one study has two U-shaped plots corresponding to women and men, respectively [15], and one study a reverse J-shaped configuration [9]. The middle panel showed six studies: three describing ‘a reverse J-shaped configuration’ [10, 16, 19], two describing an almost declining curve [10, 15] and one study an inverted U-shaped configuration [12]. The lower panel was one study showing a fluctuating mortality in women and a decreasing mortality when TC increased in men [14]. The three studies not included did not report specific calculations on the total mortality risk in relation to the TC in the 80+-year-old participants [12, 18, 21]. Among those two studies described, no association between TC and all-cause mortality was found, whereas one study found the higher total mortality related to low TC disappearing when adjusted for low HDL and albumin among people aged 70 and above [12, 18, 21].
One of the studies illustrated in Figure 2, in the middle panel, found an association, where each 1 mmol/l increase in TC corresponded to a 15% decrease in total mortality [16]. A single study found an inverted U-shaped association as seen in the middle panel of Figure 2 [13]. Among the studies not included in Figure 2, two studies found no association between TC and all-cause mortality, while one study found the higher total mortality related to low TC disappearing when adjusted for low HDL and albumin among people aged 70 and above [12, 18, 21]. The findings might be explained by heterogeneity, i.e. some elderly have a low TC due to chronic or terminal illness and some due to a healthy cardiovascular health profile [13, 16, 21].
In the majority of the observational studies, a predominantly negative association between TC and all-cause mortality was seen. Low TC was associated with the highest total mortality in all the studies, and high TC varied with either a less steep gradient, flat or an increment in total mortality, as seen in the figure [10, 11, 14–17, 19, 20].
TC and CVD mortality
The association between TC and CVD mortality was reported in 10 studies, as seen in Table 1. Two studies found a positive association, where a high TC was associated with high CVD/ischaemic heart disease mortality in at least some of the participants [22, 23], whereas six studies found no association between TC and CVD mortality [16–18, 24–26]. Two studies found a negative association where a low TC was associated with high CVD mortality [10, 14]. One study described a similar U-shaped association between TC and CVD mortality in 80+-year-old people [24].
With regard to CVD-specific mortality among 80+-year-old participants, the study results varied from finding TC associated both positively and negatively or not associated at all.
Fractioning the cholesterol into HDL and LDL in the elderly
The association between HDL cholesterol and total mortality was also different among the observational studies, two found no association [18, 27], whereas another two found a significant negative association, where increasing HDL cholesterol was associated with decreasing total mortality [15, 28]. A single study found a negative association between both HDL and LDL cholesterol and total mortality in old people [14].
Regarding the cause-specific mortality, one study found low HDL cholesterol associated with increased CHD mortality in people older then 70 years, whereas Krumholz et al. did not find any association between HDL cholesterol and CVD mortality in a smaller part of the same cohort as included in the previous study [18, 24]. A negative association between HDL cholesterol and CVD mortality, but no association with non-CVD mortality, was found in an American study on Japanese-American men [27]. One study found the ratio TC:HDL cholesterol to be a strong predictor of ischaemic heart disease mortality in 80+-year olds [22].
Conclusion
Low TC (<5.5 mmol/l) is associated with increased mortality among 80+-year olds. There was no clear optimal level of cholesterol in 80+-year-old people. Some studies found the intermediate level of the cholesterol (around 6 mmol/l) to be associated with the lowest mortality, but this was not consistent (Figure 2). Few data on TC and mortality are available on 80+-year olds.
Should we initiate and continue lipid-lowering treatment among 80+-year olds?
To answer this question, we included treatment studies, both randomised controlled trials and observational studies based on the search strategy described in Figure 1. For 80+-year olds, data were not available that allowed considering the different effect of statin therapy in the primary and secondary prevention.
None of the randomised clinical trials (RCTs) completely fulfilled the inclusion criteria, regarding separating 80+-year olds from the younger participants, as seen in Table 2. The four trials included 13,674 persons 70–82 years old, and the observational treatment studies included 12,231 participants aged 80 or above. The randomised trials and the observational treatment studies included risk or high-risk populations regarding CVD, either known CVD, systolic heart failure or diabetes [29–32]. No RCT included participants without any risk factors regarding CVD and all the trials had younger participants included (Table 2).
Table 2.
Randomised clinical trials and observational treatment studies
| Authors, year, design | Number of 80+ years old | Number of years in follow-up | Mortality/outcome | Findings | Comments |
|---|---|---|---|---|---|
| Foody et al., 2006 [33], observational study | 8,452 | 3 years | All-cause mortality | No association between statin discharge and all-cause mortality | Mortality after discharge diagnosis AMI |
| Heart Protection Study Collaborative Group, 2005 [30], RCTa | 5,806 (70–80-year olds) | 5 years | Total, vascular and non-vascular mortality | Statin allocation reduced vascular, all-cause but not non-vascular mortality significant | Participants had diabetes or vascular disease |
| Kjekshus, 2007 [31], RCT | 2,064 (≥75-year olds) | 3 years | Total and CVD mortality | No difference in total and CVD mortality in the statin and placebo groups | Participants had known systolic heart failure |
| MRC/BHF, 2002 [29], RCTa | 5,806 (70–80-year olds), 1,263 (75–80-year olds) | 5 years | Total and CVD mortality | Statin allocation reduced CVD and all-cause mortality among 70+-year old significant | Participants had diabetes or vascular disease |
| Shah et al., 2008 [34], observational study | 3,779 | 3 years | All-cause mortality | Positive association between statin discharge and all-cause mortality | Mortality after discharge diagnosis HF |
| Shepherd et al., 2002 [32], RCT | 5,804 (70–82-year olds), mean 75 years | 3.2 years | Total and CHD mortality | Statin allocation not associated with all-cause mortality but positively with CHD mortality | High-risk participants |
RCT, randomised clinical trial; AMI, acute myocardial infarction; HF, heart failure.
aSame study population.
Two trials found no association between statin allocation and all-cause mortality [31, 32], whereas two different trials of the same study population found a reduction in all-cause mortality when allocated to statin treatment compared with placebo [29, 30]. Two trials found a significant reduction in the number of CVD events (approximately 25%) when participants were allocated to statins, but Shepherd et al. found no difference in all-cause mortality among 70–82-year olds treated with pravastatin compared with placebo [29, 32]. One study could not exclude that the use of statins in the elderly in the primary prevention of CVD could be harmful and, at best, could result in a change in the type of mortality from CVD to cancer, even though total mortality was unchanged [32]. Kjekshus et al. [31] found no difference in the all-cause mortality or CVD outcome between patients with known systolic heart failure treated with either rosuvastatin or placebo. Two observational treatment studies found statin treatment associated with a reduction in all-cause mortality in heart failure patients aged 85 or above, but no changes in all-cause mortality in post-AMI patients 80+ years old, respectively [33, 34].
Conclusion
No RCT had demonstrated an effect of cholesterol-lowering treatment on total mortality for 80+-year-old people. There was no trial evidence that statins decrease all-cause mortality in elderly people without known vascular disease, on the contrary, it was even possible that statins increased all-cause mortality in this group as described by Goldstein et al. [35] The participants in the trials included were 70+-year-olds, all had some kind of CVD risk and probably few were 80+ years old. Currently, it is not clear if or when initiation and continuation of lipid-lowering treatment in the 80+-year-old people should be done. Two trials found it beneficial to the CVD mortality to be allocated to statins among 70–80-year olds, whereas two trials found no difference in all-cause mortality in the statin and placebo allocated, respectively. Similar results were found in the secondary analysis of the JUPITER study, where treatment with the potent rosuvastatin did not have any effect on total mortality in people 70 years or older [36]. In the PROSPER study, only elderly who were carriers of the KIF6 719Arg variant and with prior vascular disease had significant benefit from pravastatin therapy [37]. The existing data were not sufficient to recommend anything regarding lipid-lowering treatment for the population aged 80+.
Optimal level of cholesterol and recommendation for lipid-lowering treatment at the highest ages
A large proportion of elderly patients are treated with lipid-lowering drugs, many of those will enter their ninth decade using lipid-lowering drugs, which raises a number of questions. First, it is important that the medication is both safe and beneficial to the patient (evidence-based medicine). Second, we shall be aware of the potential compliance problems where the old patients choose to stop taking medication due to ‘polypharmacy’. Third, there is an economic aspect, with regard to both society and the old patient. Still, it is unclear whether elderly patients should be treated for the rest of their lives when started lipid-lowering therapy or whether the treatment has different limits at old ages.
Other still open questions are whether it is reasonable to generalise from younger cohorts in their 60s or 70s to the 80+-year olds and whether the new cohorts of 80+-year olds are biologically different (younger) than previous cohorts of 80+-year olds [38]. Based on the available literature, the optimal cholesterol level for people aged 80 or above is not known, neither is it known whether lipid-lowering drugs should be used in this age group. Low TC (<5.5 mmol/l) is associated with the highest mortality rate in observational studies of 80+-year olds. No clear optimal level of TC was identified. There is not sufficient observational or RCT data to recommend anything regarding initiation or continuation of lipid-lowering treatment for the population aged 80+.
Key points.
One-third of the 75–84-year-old Swedes are treated with statins.
The lowest cholesterol levels are associated with higher all-cause mortality among 80+-year olds.
No evidence of an effect of lipid-lowering treatment on all-cause mortality among 80+-year olds was found.
The data were not sufficient to make any recommendation regarding 80+-year olds and lipid-lowering treatment.
Conflicts of interest
All the authors declare to have no conflict of interest.
Funding
The Danish Aging Research Center is supported by the VELUX foundation. The research was supported by the US National Institute on Aging, research grant NIA-P01-AG08761, and by a Danish grant from Savværksejer Jeppe Juhl og Hustru Ovita Juhls Mindelegat.
References
- 1.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–208. doi: 10.1016/S0140-6736(09)61460-4. doi:10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98. doi: 10.1056/NEJMoa0801369. doi:10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 3.Hjemdahl P, Allhammar A, Heaton C, et al. SBU should investigate what is an evidence-based and cost-effective use of statins. Lakartidningen. 2009;106:1992–4. [PubMed] [Google Scholar]
- 4.Aronow WS. Managing hyperlipidaemia in the elderly: special considerations for a population at high risk. Drugs Aging. 2006;23:181–9. doi: 10.2165/00002512-200623030-00001. doi:10.2165/00002512-200623030-00001. [DOI] [PubMed] [Google Scholar]
- 5.Aronow WS. Treatment of high-risk older persons with lipid-lowering drug therapy. Am J Ther. 2008;15:102–7. doi: 10.1097/MJT.0b013e31802b5aa4. doi:10.1097/MJT.0b013e31802b5aa4. [DOI] [PubMed] [Google Scholar]
- 6.Eimer MJ, Stone NJ. Evidence-based treatment of lipids in the elderly. Curr Atheroscler Rep. 2004;6:388–97. doi: 10.1007/s11883-004-0051-4. doi:10.1007/s11883-004-0051-4. [DOI] [PubMed] [Google Scholar]
- 7.Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. doi:10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 8.Lewington S, Whitlock G, Clarke R, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370:1829–39. doi: 10.1016/S0140-6736(07)61778-4. doi:10.1016/S0140-6736(07)61778-4. [DOI] [PubMed] [Google Scholar]
- 9.Anum EA, Adera T. Hypercholesterolemia and coronary heart disease in the elderly: a meta-analysis. Ann Epidemiol. 2004;14:705–21. doi: 10.1016/j.annepidem.2003.10.009. doi:10.1016/j.annepidem.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Casiglia E, Spolaore P, Ginocchio G, et al. Predictors of mortality in very old subjects aged 80 years or over. Eur J Epidemiol. 1993;9:577–86. doi: 10.1007/BF00211430. [DOI] [PubMed] [Google Scholar]
- 11.Dontas AS, Toupadaki N, Tzonou A, Kasiviki-Charvati P. Survival in the oldest old: death risk factors in old and very old subjects. J Aging Health. 1996;8:220–37. doi: 10.1177/089826439600800204. doi:10.1177/089826439600800204. [DOI] [PubMed] [Google Scholar]
- 12.Foody JM, Wang Y, Kiefe CI, et al. Long-term prognostic importance of total cholesterol in elderly survivors of an acute myocardial infarction: the Cooperative Cardiovascular Pilot Project. J Am Geriatr Soc. 2003;51:930–6. doi: 10.1046/j.1365-2389.2003.51305.x. doi:10.1046/j.1365-2389.2003.51305.x. [DOI] [PubMed] [Google Scholar]
- 13.Jonsson A, Sigvaldason H, Sigfusson N. Total cholesterol and mortality after age 80 years. Lancet. 1997;350:1778–9. doi: 10.1016/S0140-6736(05)63609-4. doi:10.1016/S0140-6736(05)63609-4. [DOI] [PubMed] [Google Scholar]
- 14.Kronmal RA, Cain KC, Ye Z, Omenn GS. Total serum cholesterol levels and mortality risk as a function of age. A report based on the Framingham data. Arch Intern Med. 1993;153:1065–73. doi:10.1001/archinte.153.9.1065. [PubMed] [Google Scholar]
- 15.Nikkila M, Heikkinen J. Serum cholesterol, high-density lipoprotein cholesterol and five-year survival in elderly people. Age Ageing. 1990;19:403–8. doi: 10.1093/ageing/19.6.403. doi:10.1093/ageing/19.6.403. [DOI] [PubMed] [Google Scholar]
- 16.Weverling-Rijnsburger AW, Blauw GJ, Lagaay AM, Knook DL, Meinders AE, Westendorp RG. Total cholesterol and risk of mortality in the oldest old. Lancet. 1997;350:1119–23. doi: 10.1016/s0140-6736(97)04430-9. doi:10.1016/S0140-6736(97)04430-9. [DOI] [PubMed] [Google Scholar]
- 17.Weverling-Rijnsburger AW, Jonkers IJ, van EE, Gussekloo J, Westendorp RG. High-density vs low-density lipoprotein cholesterol as the risk factor for coronary artery disease and stroke in old age. Arch Intern Med. 2003;163:1549–54. doi: 10.1001/archinte.163.13.1549. doi:10.1001/archinte.163.13.1549. [DOI] [PubMed] [Google Scholar]
- 18.Krumholz HM, Seeman TE, Merrill SS, et al. Lack of association between cholesterol and coronary heart disease mortality and morbidity and all-cause mortality in persons older than 70 years. JAMA. 1994;272:1335–40. doi:10.1001/jama.272.17.1335. [PubMed] [Google Scholar]
- 19.Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet. 2001;358:351–5. doi: 10.1016/S0140-6736(01)05553-2. doi:10.1016/S0140-6736(01)05553-2. [DOI] [PubMed] [Google Scholar]
- 20.Schupf N, Costa R, Luchsinger J, Tang MX, Lee JH, Mayeux R. Relationship between plasma lipids and all-cause mortality in nondemented elderly. J Am Geriatr Soc. 2005;53:219–26. doi: 10.1111/j.1532-5415.2005.53106.x. doi:10.1111/j.1532-5415.2005.53106.x. [DOI] [PubMed] [Google Scholar]
- 21.Volpato S, Leveille SG, Corti MC, Harris TB, Guralnik JM. The value of serum albumin and high-density lipoprotein cholesterol in defining mortality risk in older persons with low serum cholesterol. J Am Geriatr Soc. 2001;49:1142–7. doi: 10.1046/j.1532-5415.2001.49229.x. doi:10.1046/j.1532-5415.2001.49229.x. [DOI] [PubMed] [Google Scholar]
- 22.Clarke R, Emberson JR, Parish S, et al. Cholesterol fractions and apolipoproteins as risk factors for heart disease mortality in older men. Arch Intern Med. 2007;167:1373–8. doi: 10.1001/archinte.167.13.1373. doi:10.1001/archinte.167.13.1373. [DOI] [PubMed] [Google Scholar]
- 23.Corti MC, Guralnik JM, Salive ME, et al. Clarifying the direct relation between total cholesterol levels and death from coronary heart disease in older persons. Ann Intern Med. 1997;126:753–60. doi: 10.7326/0003-4819-126-10-199705150-00001. [DOI] [PubMed] [Google Scholar]
- 24.Corti MC, Guralnik JM, Salive ME, et al. HDL cholesterol predicts coronary heart disease mortality in older persons. JAMA. 1995;274:539–44. doi:10.1001/jama.274.7.539. [PubMed] [Google Scholar]
- 25.Raiha I, Marniemi J, Puukka P, Toikka T, Ehnholm C, Sourander L. Effect of serum lipids, lipoproteins, and apolipoproteins on vascular and nonvascular mortality in the elderly. Arterioscler Thromb Vasc Biol. 1997;17:1224–32. doi: 10.1161/01.atv.17.7.1224. [DOI] [PubMed] [Google Scholar]
- 26.Zimetbaum P, Frishman WH, Ooi WL, et al. Plasma lipids and lipoproteins and the incidence of cardiovascular disease in the very elderly. The Bronx Aging Study. Arterioscler Thromb. 1992;12:416–23. doi: 10.1161/01.atv.12.4.416. [DOI] [PubMed] [Google Scholar]
- 27.Koropatnick TA, Kimbell J, Chen R, et al. A prospective study of high-density lipoprotein cholesterol, cholesteryl ester transfer protein gene variants, and healthy aging in very old Japanese-american men. J Gerontol A Biol Sci Med Sci. 2008;63:1235–40. doi: 10.1093/gerona/63.11.1235. [DOI] [PubMed] [Google Scholar]
- 28.Landi F, Russo A, Pahor M, et al. Serum high-density lipoprotein cholesterol levels and mortality in frail, community-living elderly. Gerontology. 2008;54:71–8. doi: 10.1159/000111381. doi:10.1159/000111381. [DOI] [PubMed] [Google Scholar]
- 29.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. doi:10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 30.Heart Protection Study Collaborative Group. The effects of cholesterol lowering with simvastatin on cause-specific mortality and on cancer incidence in 20,536 high-risk people: a randomised placebo-controlled trial [ISRCTN48489393] BMC Med. 2005;3:6. doi: 10.1186/1741-7015-3-6. doi:10.1186/1741-7015-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kjekshus J, Apetrei E, Barrios V, et al. Rosuvastatin in older patients with systolic heart failure. N Engl J Med. 2007;357:2248–61. doi: 10.1056/NEJMoa0706201. doi:10.1056/NEJMoa0706201. [DOI] [PubMed] [Google Scholar]
- 32.Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30. doi: 10.1016/s0140-6736(02)11600-x. doi:10.1016/S0140-6736(02)11600-X. [DOI] [PubMed] [Google Scholar]
- 33.Foody JM, Rathore SS, Galusha D, et al. Hydroxymethylglutaryl-CoA reductase inhibitors in older persons with acute myocardial infarction: evidence for an age-statin interaction. J Am Geriatr Soc. 2006;54:421–30. doi: 10.1111/j.1532-5415.2005.00635.x. doi:10.1111/j.1532-5415.2005.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shah R, Wang Y, Foody JM. Effect of statins, angiotensin-converting enzyme inhibitors, and beta blockers on survival in patients >or=65 years of age with heart failure and preserved left ventricular systolic function. Am J Cardiol. 2008;101:217–22. doi: 10.1016/j.amjcard.2007.08.050. doi:10.1016/j.amjcard.2007.08.050. [DOI] [PubMed] [Google Scholar]
- 35.Goldstein MR, Mascitelli L, Pezzetta F. Statin therapy in the elderly: misconceptions. J Am Geriatr Soc. 2008;56:1365. doi: 10.1111/j.1532-5415.2008.01716.x. doi:10.1111/j.1532-5415.2008.01716.x. [DOI] [PubMed] [Google Scholar]
- 36.Glynn RJ, Koenig W, Nordestgaard BG, Shepherd J, Ridker PM. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med. 2010;152:488–96. doi: 10.1059/0003-4819-152-8-201004200-00005. W174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iakoubova OA, Robertson M, Tong CH, et al. KIF6 Trp719Arg polymorphism and the effect of statin therapy in elderly patients: results from the PROSPER study. Eur J Cardiovasc Prev Rehabil. 2010;17:455–61. doi: 10.1097/HJR.0b013e328336a0dd. [DOI] [PubMed] [Google Scholar]
- 38.Engberg H, Christensen K, Andersen-Ranberg K, Vaupel JW, Jeune B. Improving activities of daily living in Danish centenarians—but only in women: a comparative study of two birth cohorts born in 1895 and 1905. J Gerontol A Biol Sci Med Sci. 2008;63:1186–92. doi: 10.1093/gerona/63.11.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]