Abstract
Background
This study aims to identify self-management strategies used by patients with diabetes in hot weather, examine knowledge of safe temperatures and exposure times, and evaluate comprehension of weather data.
Methods
Patients attending an endocrinology clinic in southwestern United States were surveyed.
Results
One hundred fifty-two surveys completed from November 30 to December 31, 2009 werMean patient age was 64 years; diabetes duration e analyzed 15 years; 51% were women 83% had type 2 diabetes, 58% were non Hispanic white, and 77% were on insulin injections. Mean hemoglobin A1c was 7.9%; 38% had hemoglobin A1c values of 8.0% or higher. Patients used an array of personal protective measures during hot weather, and 71% limited heat exposure to less than one hour. Respondents typically took steps to protect their diabetes medication and supplies, but 37% chose to leave medications and supplies at home. Although 73% of respondents had received information regarding the effect of heat on insulin, only 39% had received information about the effect of heat on oral medications, 41% on glucose meters, and 38% on glucose test strips. The temperature at which patients took protective measures varied. Only 55% knew the definition of the heat index.
Conclusion
Most survey participants took measures to protect themselves from the heat, although gaps in knowledge were evident. Many patients had suboptimal glycemic control, placing them potentially at risk for dehydration during the hottest months. Increased public awareness of this topic is needed, and diabetes education programs should include information about the heat where appropriate.
Keywords: desert climate, diabetes, heat
Introduction
Heat remains the number one weather-related killer in the general population.1 As core body temperature rises, the primary physiologic measure to cool the body is sweating, with subsequent heat removal through evaporation.2 Some patients with diabetes may have increased susceptibility to the heat because of impairment of this thermoregulatory mechanism and also from alterations in cutaneous vasodilation; impaired orthostatic responses at elevated temperatures have also been documented.2–7 Whether these physiologic impairments are associated with increased heat related illness is not known, however, patients with diabetes do have higher numbers of emergency department visits, hospitalizations, and mortality documented during heat waves.8–10 Changes in insulin kinetics and stability are possible.3 The effect of heat on equipment performance (e.g., glucose meters, insulin pumps) is another concern.3
Millions of individuals with diabetes live in zones characterized by hot weather. The Middle East, sub-Saharan Africa, and India have high prevalence rates of diabetes, and will witness some of the largest increases in the number of affected persons in the next two decades.11,12 Diabetes prevalence has been increasing in the southwestern United States.13 Temperatures that would be viewed as extreme across much of the United States are common across the Sonoran Desert, which covers parts of Arizona and California. Metropolitan Phoenix has up to 133 days with temperatures higher than 95 °F (35 °C) and as many as 61 days with temperatures higher than 104 °F (40 °C). Thus, the southwestern United States, and metropolitan Phoenix specifically, could serve as suitable geographic models to examine the relationship between heat and diabetes care.
Public awareness campaigns, educational materials, and programs advising patients how to cope when “the heat is on” are important. Such efforts should parallel initiatives undertaken to advise patients with diabetes on how to prepare for natural disasters.14–21 From a public health standpoint, cities are not well prepared to deal with the health consequences of hot weather.22 Moreover, there are no data on level of “heat awareness” of patients. We conducted a survey of patients with diabetes that gauged the types of self-management strategies utilized during hot weather, examined knowledge of safe temperatures and exposure times, assessed comprehension of weather data, and determined sources of weather information.
Methods
Questionnaire Development
The study was approved by the Mayo Clinic Institutional Review Board. A questionnaire (see Appendix) was constructed to gain insight into the following areas: (1) identify what diabetes self-management strategies patients use during hot weather; (2) learn the temperature thresholds at which patients consider taking protective measures; (3) ascertain if patients previously received information about the heat and their diabetes; (4) assess knowledge of hot weather data; and (5) determine sources of weather information. The questionnaire was developed by a team of endocrinologists, family practitioners, diabetes educators, and members of the U.S. National Weather Service.
The survey included questions on patient demographics, diabetes type and duration, and method of disease treatment (Appendix). The most recent hemoglobin A1c (HbA1c) value was recorded. In addition, patients were asked whether they spent their summers in the metropolitan Phoenix area. Our clinic provides care for many patients who do not summer in the Southwest. Hence, this latter question was intended to distinguish these patients from individuals who were full-time residents of the region and who would represent those at greatest risk of exposure to hot weather. For patients not residing in metropolitan Phoenix, we examined medical records to determine if they lived in other regions of the Southwest characterized by high summer temperatures.
The next group of questions gauged the type of protective measures patients utilized during hot weather and evaluated temperature ranges and exposure times at which they instituted these measures. Similar questions were also included pertaining to diabetes medications and supplies. Participants were asked if they read the product information for their medications and supplies, and if they had received information about the effect of heat on these products (Appendix).
The final questions evaluated patient knowledge of heat index and humidity, primary sources of weather information, time of day and frequency of monitoring weather reports, and if this weather information affected how participants cared for their diabetes. The type of information patients sought to obtain from weather reports was also determined (Appendix). The survey tool underwent repeated cycles of review and revision, was piloted twice, then finalized. Patients presenting for their diabetes evaluation from November 30 to December 31, 2009, were asked to complete the survey.
Assessment of Seasonal HbA1c Values
Although little epidemiological information is available, the combination of poor glycemic control and heat exposure may make a diabetes patient more susceptible to dehydration. We reviewed our electronic medical records for January 1 to December 31, 2009, to determine the result of all available HbA1c values; results were averaged by quarter (quarter 1, January–March; quarter 2, April–June; quarter 3, July–September; quarter 4, October–December). If a patient had more than one HbA1c determination per quarter, results were averaged for that quarter. This cross- sectional analysis was undertaken to provide an estimate of the population at risk for dehydration from the combined effects of poor glycemic control and hot weather.
Data Analysis
Analysis consisted of descriptive statistics for continuous variables, and frequencies for categorical variables. Results are expressed as mean [standard deviation (SD)] or percentage of total responses where applicable. In addition to determining mean quarterly HbA1c values, the percentage of patients with HbA1c values of 8.0% or higher was also determined for each quarter.
Results
Patient Characteristics
Overall, 178 patients were approached, 174 consented, and 169 completed the survey. Of these, 17 individuals did not reside in the Southwest during the summer, resulting in 152 questionnaires analyzed. Mean age of these 152 participants was 64 (14) years (1) with a high mean body mass index. About half were women, and the majority were of white, non-Hispanic ethnicity. Nearly all had higher education (1). The majority had type 2 diabetes, with a mean diabetes duration of 15 (12) years. Most patients [117 (77%)] were on insulin therapy, either as monotherapy, in combination with other agents, or via an insulin pump. HbA1c values were typically obtained within one month of the clinic visit. The mean HbA1c value was 7.9% (1.4%), with nearly 40% having a value of 8.0% or higher (1).
Table 1.
Characteristics of 152 Patients with Diabetes Participating in Survey
| Characteristic | Valuea |
|---|---|
| Age, year | 64 (14) |
| Body mass index, kg/m2 | 31 (6) |
| Women | 77 (51) |
| Race/ethnicity | |
| White, non-Hispanic | 88 (58) |
| White, Hispanic | 42 (28) |
| Other | 22 (14) |
| Education levelb | |
| Grade 8 | 2 (1) |
| High school | 22 (15) |
| Some college | 41 (28) |
| Associate degree | 14 (10) |
| Bachelor's degree | 39 (27) |
| Master's degree | 21 (14) |
| Doctorate | 7 (5) |
| Type 2 diabetes | 126 (83) |
| Diabetes duration, year | 15 (12) |
| Method of treatment | |
| Lifestyle only | 2 (1) |
| Oral agents only | 29 (19) |
| Insulin injections only | 71 (47) |
| Oral agents and insulin | 33 (22) |
| Insulin pump | 11 (7) |
| Otherc | 6 (4) |
| HbA1c, % | 7.9 (1.4) |
| Patients with HbA1c ≥8.0% | 58 (38) |
Values are mean (SD) or number (percentage).
Of 146 participants who chose to answer the question.
Other includes one on exenatide, one on exenatide and insulin, three on oral agents and exenatide, and one on oral agents, exenatide, and insulin.
Temperature Thresholds When Patients Take Protective Measures
Participants were asked, “At what temperature would you start taking measures to protect yourself from the heat?” Some patients indicated fairly high temperatures before they would start protecting themselves (Figure 1A). For instance, one-fifth of the respondents said they would not take protective measures until temperatures reached as high as 101 to 105 °F, but some reported even higher temperature ranges; no one indicated a temperature higher than 116 °F (Appendix). Patients seemed familiar with the concept of limiting the amount of time spent in the heat. In response to the question “How much time would you spend in the heat before you started protecting yourself?”, 71% indicated they limited exposure to less than one hour.
Figure 1.
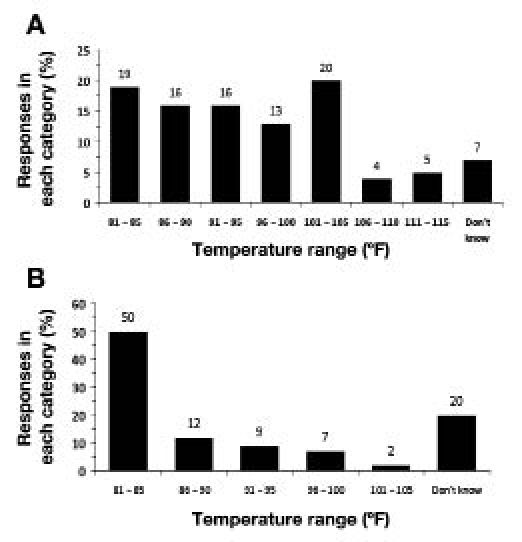
(A) Temperature ranges at which patients with diabetes reported taking personal protective measures in the heat; no one indicated a temperature higher than 116 °F. (B) Temperature ranges at which respondents reported protecting their diabetes equipment, medications, and supplies; no patients reported waiting until temperatures reached ranges of 106 °F or higher.
Less variability was seen in response to the question, “At what temperature would you protect your diabetes equipment, medications and supplies?” Half the respondents reported they would take steps to protect their diabetes medications and supplies at the lowest temperature range presented in the question of 81 to 85 °F (Figure 1B); however, many patients did report higher temperature ranges and even 20% did not know. No patients indicated they would wait until temperatures exceeded 106 °F (Appendix).
Types of Protective Measures
Patients used multiple methods to protect themselves from the heat (Figure 2A). The most common response was to “stay in and avoid the heat,” followed by “take additional fluids and drink on a schedule,” “apply sunscreen” or “wear a hat, long sleeves, or other protective clothing,” then “drink only when thirsty” and “other”; only a few indicated they “don't know, never received any information about how to protect myself from the heat.”
Figure 2.
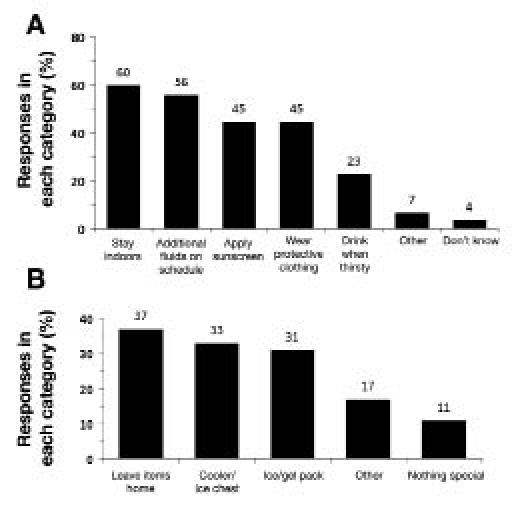
Types of protective measures patients with diabetes reported using in the heat for themselves (A) and for their equipment, medications, and supplies (B).
The most common technique patients used to protect their diabetes medications and supplies from the heat was simply to “leave items home,” followed by “carry items in a cooler/ice chest,” and “carry items in a commercially produced case with ice/gel packs” (Figure 2B). Some individuals used other methods (e.g., “carry in purse” or “store in refrigerator in automobile”); a few indicated they did “nothing special” to safeguard their medications and supplies from the heat.
When queried if they read the product information on their diabetes medications, 86% said “yes,” and 68% read their glucose meter product information. Although the numbers of these patients were small, 82% of insulin pump users indicated they read their product information. In terms of patient education related to heat effects, 73% of respondents receiving insulin and 91% on insulin pumps indicated they had received information regarding the effects of heat on their insulin. Only 39% of individuals taking oral medications acknowledged having received information about the effect of heat on those agents. Just 41% of all respondents stated they had received information regarding the effects of heat on glucose meters and just 38% on glucose test strips.
Understanding of Weather Data and Sources of Weather Information
Only 55% of patients knew the correct definition of the heat index as “a measure of how hot it really feels when humidity is added to actual temperature,” and 29% indicated they did not know the meaning. Humidity was better understood, with 83% marking the correct answer (i.e., “a measure of dampness in the air”). The most common source for weather information was television (89%); 35% listened to the radio, 34% used the Internet, and 26% read the newspaper. No patient received information via text messaging, and 6% reported using other means of obtaining weather information (e.g., “we have our own weather station,” or “usually walk outside and see and feel”).
When asked about the time of day they checked the weather forecast, the majority (64%) of respondents checked in the morning, and 66% indicated they listened for it every day. Only 38% of participants indicated that the temperature forecast affected how they took care of their diabetes medications and supplies, 47% said it did not, and 15% stated only sometimes. The information participants most commonly sought to obtain from the weather reports was temperature, cited by 91% of patients.
Quarterly HbA1c Values
Mean HbA1c was 7.8% (1.2%) for quarter 1 (n=67), 7.2% (1.1%) for quarter 2 (n=77), 8.0% (1.7%) for quarter 3 (n=90), and 7.9% (1.3%) for quarter 4 (n=126)(Figure 3A). The proportion of patients with HbA1c values of 8.0% or higher was lowest in quarter 2, but was 40% or higher for the other quarters, with the most in quarter 3 (Figure 3B).
Figure 3.
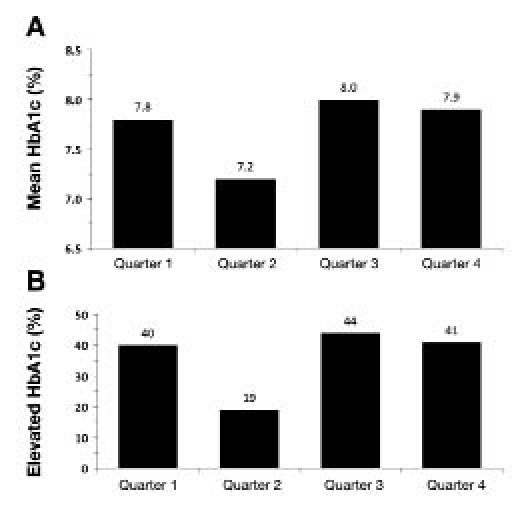
Mean hemoglobin A1c (HbA1c) values (A) and percentage of HbA1c values of 8.0% or higher (B) by quarter.
Discussion
Municipalities appear to be largely unprepared to address heat emergencies.22 For now, it will likely fall to clinical programs to provide necessary information to patients with diabetes. A few patient education materials are available on the topic of diabetes and the heat,23–27 but there are no data from the patient's perspective and this area remains vastly understudied. We therefore surveyed patients receiving care in an endocrinology clinic in metropolitan Phoenix to gain insight into current diabetes self-management practices and knowledge about the heat.
Analysis revealed aspects of diabetes management strategies in hot weather about which the respondents seemed to be well informed and others where knowledge deficits and education could be improved. For instance, respondents reported a wide range of thresholds when asked, “At what temperature would you start taking measures to protect yourself from the heat?” Nearly one-third of patients indicated they would not start taking protective measures until temperatures were higher than 101 °F. When the heat index is considered (for which only about half the respondents knew the correct meaning and more than one-quarter did not know), heat-related symptoms can begin occurring with lower temperatures in the range of 80 to 90 °F.28 Thus, the thresholds reported by many patients surveyed are probably higher than the temperatures at which steps should be taken to avoid heat-related illnesses, and this represents an opportunity for educational intervention. Most patients were familiar with the need to keep exposure time in the heat short. Additionally, patients were taking appropriate protective measures during hot weather. One observation that raises concern (and presents another opportunity for education) is that about a quarter of patients stated they would drink only when thirsty, while fluid intake in the heat should be prophylactic to prevent dehydration from occurring.29
When asked, “At what temperature would you protect your diabetes equipment, medications and supplies?”, the majority of respondents marked the lowest temperature threshold of 81 to 85 °F. Thus, patients in general seemed aware of the sensitivity of their medications and supplies to the heat; moreover, most participants indicated they read their product information and were presumably familiar with appropriate storage instructions. It should be noted, however, that 20% of patients stated they did not know at what temperature they should take measures to protect these vital components of diabetes management.
The most common method used by nearly 40% of patients to protect their diabetes medications and supplies was simply to “leave items home.” This practice could be of concern, given that patients would then not have the means to check their blood glucose (before driving, for example), give extra insulin when dining out, or know when to seek medical care in the event of a glycemic emergency. These patients could be at risk for motor vehicle accidents from undetected hypoglycemia30 or occupational injuries if they work in labor-intensive environments and do not have the means to check glucose levels. The need to have their medications and supplies with them at all times represents another educational opportunity, and diabetes patients can be given tips on how to protect these items from the heat, including information on vendors who sell specially designed carrying cases.
Diabetes medications are susceptible to heat damage.3 Moreover, equipment used by patients for self-management such as glucometers can fail at high temperatures,31 and the oxidized mediator on glucose monitoring strips can be denatured if exposed to heat, causing inaccurate readings.32,33 We also set out to determine if patients had received information about the effect of heat on their diabetes medications and supplies. We did not inquire about the nature, source, or types of heat-related information received (a detail we can include on future revisions of the questionnaire). Suggestions for how to transport items in the heat, safe exposure times, and how to recognize heat-damaged materials are all relevant and may not be encountered in standard product information. Most of the surveyed patients were on insulin—a medication particularly susceptible to heat degradation. While a large percentage stated they had received informa-tion on the effect of heat on insulin, only a minority of respondents reported receiving information about heat and oral medications, glucose meters, and glucose test strips.
If public awareness campaigns are to be developed and alerts relating to heat are to be disseminated to patients with diabetes, then it will be important to establish how patients acquire their weather information. Survey participants obtained weather information from multiple media sources, with television used most commonly. While these may be suitable methods for public outreach, quicker, real-time methods such as text messages via cell phones may be employed to communicate heat advisories as part of heat wave preparedness campaigns. Our local weather office does offer this service, but individuals must register to receive the notifications, and it is unclear how well known the service is among patients with chronic illnesses. The majority of individuals in this study listened to the weather forecast principally in the morning, with temperature being the most sought-after piece of information. Of concern is that almost half of respondents stated that temperature information did not affect how they cared for their diabetes medications and supplies, suggesting a possible disconnect between interest in predicted temperatures and translating that information to the daily management of their diabetes.
Superimposed on the risk to patients from possible abnormal thermoregulatory and cardiovascular responses to heat is the potential for dehydration when high temperatures are combined with poor glycemic control. We found that nearly 40% of patients had HbA1c values of 8.0% or higher at the time of the survey. Moreover, cross-sectional analysis undertaken to estimate the number of patients that could be at risk revealed that a substantial number of individuals had HbA1c values of 8.0% or higher, three out of four quarters, with the highest percentage occurring during the hottest and most humid months of Arizona (quarter 3, July–September). Thus, many patients may be at risk for adverse health consequences (i.e., more emergency department visits) due to the combined effects of poor glycemic control and heat. Better glycemic control during quarter 2 may have reflected more intense exercise by participants in the prior, cooler quarter. Our analysis was not a prospective study designed to test the hypothesis that seasonal changes in glycemic control occur or to identify the variables that may account for such differences, but such a future study would be of interest.
This study has some limitations. The respondents represented a convenience sample of patients and were predominately higher-educated, white, non-Hispanic individuals. This sampling may therefore be biased in terms of patient perceptions and cultural norms in management of their diabetes. Diabetes self-care practices during hot weather and knowledge about what to do during times of excessive high temperatures may vary in different populations. Patients with diabetes from underserved populations, for example, may not have ready access to electronic media to gain weather information, or access to air conditioning.
The survey did not ask about participant occupation. It would have been interesting to see if responses varied among outdoor laborers and those who primarily worked in covered or cooled environments. Diabetes self-care practices may be different in outdoor laborers, and these individuals may have developed novel ways to protect their diabetes care products. Examining heat adaptation strategies among athletic patients with diabetes who exercise outdoors would be of future interest as well. Adapting the survey to include adolescents and recruit-ment of younger adults with diabetes to understand their self-care practices during hot weather would be another important area of investigation. Out of convenience, we conducted the survey during one of the coolest months in the region. Responses may have been different if the study had been performed during the heat of the summer.
Finally, large-scale analysis of statewide, electronic, hospital discharge data to examine seasonal trends in emergency department visits and hospitalizations among patients with diabetes will be important for future studies to confirm if such events increase during times of hot weather or heat waves. Examination of these trends in relationship to glycemic control could be undertaken. Additionally, it would be useful to modify our current survey tool to include a question about recent emergency department visits or hospitalizations and the reasons for seeking medical attention.
Conclusion
To our knowledge, this is the first study gauging self-care practices and knowledge of patients with diabetes who live in a hot climate. Most respondents took measures to protect themselves from the heat, although gaps in knowledge were evident. Continued efforts to teach basic principles of weather knowledge such as definitions of temperature, humidity, and heat index are important for patients to understand the weather-related information they encounter. Many patients had suboptimal glycemic control, potentially placing them at risk for dehydration during the hottest months. Further study is needed to gauge patient awareness of their diabetes in relation to the environment in which they live and the impact the latter may have on control of their disease. Increased public awareness of this topic is needed, and diabetes education programs should include information on managing or combating the effects of hot weather.
Abbreviations
- HbA1c
hemoglobin A1c
- SD
standard deviation
References
- 1.National Oceanic and Atmospheric Administration. Heat wave: a major summer killer [monograph on the Internet]. Washington: United States Department of Commerce; [cited 2010 Feb 8]. Available from: http://www.noaawatch.gov/themes/heat.php. [Google Scholar]
- 2.Petrofsky JS, Lee S, Patterson C, Cole M, Stewart B. Sweat production during global heating and during isometric exercise in people with diabetes. Med Sci Monit. 2005 Nov;11(11):CR515–521. [PubMed] [Google Scholar]
- 3.Westphal SA, Childs RD, Seifert KM, Boyle ME, Fowke M, Iñiguez P, Cook CB. Managing diabetes in the heat: potential issues and concerns. Endocr Pract. 2010 May–Jun;16(3):506–511. doi: 10.4158/EP09344.RA. [DOI] [PubMed] [Google Scholar]
- 4.Petrofsky JS, McLellan K, Bains GS, Prowse M, Ethiraju G, Lee S, Gunda S, Lohman E, Schwab E. Skin heat dissipation: the influence of diabetes, skin thickness, and subcutaneous fat thickness. Diabetes Technol Ther. 2008 Dec;10(6):487–493. doi: 10.1089/dia.2008.0009. [DOI] [PubMed] [Google Scholar]
- 5.Fealey RD, Low PA, Thomas JE. Thermoregulatory sweating abnormalities in diabetes mellitus. Mayo Clin Proc. 1989 Jun;64(6):617–628. doi: 10.1016/s0025-6196(12)65338-5. [DOI] [PubMed] [Google Scholar]
- 6.Wick DE, Roberts SK, Basu A, Sandroni P, Fealey RD, Sletten D, Charkoudian N. Delayed threshold for active cutaneous vaso-dilation in patients with type 2 diabetes mellitus. J Appl Physiol. 2006 Feb;100(2):637–641. doi: 10.1152/japplphysiol.00943.2005. Epub 2005 Oct 6. [DOI] [PubMed] [Google Scholar]
- 7.Petrofsky JS, Besonis C, Rivera D, Schwab E, Lee S. Impairment in orthostatic tolerance during heat exposure in individuals with type 1 and type 2 diabetes. Med Sci Monit. 2005;11(4):CR153–159. [PubMed] [Google Scholar]
- 8.Schuman SH. Patterns of urban heat-wave deaths and implications for prevention: data from New York and St. Louis during July, 1966. Environ Res. 1972 Mar;5(1):59–75. doi: 10.1016/0013-9351(72)90020-5. [DOI] [PubMed] [Google Scholar]
- 9.Semenza JC, McCullough JE, Flanders WD, McGeehin MA, Lumpkin JR. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999 May;16(4):269–277. doi: 10.1016/s0749-3797(99)00025-2. [DOI] [PubMed] [Google Scholar]
- 10.Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, Trent R, English P. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009 Jan;117(1):61–67. doi: 10.1289/ehp.11594. Epub 2008 Aug 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diabetes Unit, Department of Chronic Diseases and Health Promotion (CHP). Prevalence of diabetes – world map [monograph on the Internet]. Geneva: World Health Organization; 2004 [cited 2010 Feb 11] Available from: http://www.who.int/diabetes/actionnow/en/mapdiabprev.pdf.
- 12.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 13.Department of Health and Human Services. Diabetes data & trends [monograph on the Internet]. Atlanta: Centers for Disease Control and Prevention [cited 2010 Feb 11]. Available from: http://apps.nccd.cdc.gov/DDTSTRS/default.aspx. [Google Scholar]
- 14.Chitwood M, Lewis C, Harle C. Preparing for natural disasters: a survival plan for persons with diabetes. Diabetes Educ. 1992;18(3):246–247. doi: 10.1177/014572179201800314. May-Jun. 250. [DOI] [PubMed] [Google Scholar]
- 15.D'Arrigo T. Disaster strikes: are you ready? Diabetes Forecast. 2006;59(2):46–48. Feb. 50, 52. [PubMed] [Google Scholar]
- 16.Stallwood LG. Assessing emergency preparedness of families caring for young children with diabetes and other chronic illnesses. J Spec Pediatr Nurs. 2006 Oct;11(4):227–233. doi: 10.1111/j.1744-6155.2006.00074.x. [DOI] [PubMed] [Google Scholar]
- 17.Cefalu WT, Smith SR, Blonde L, Fonseca V. The Hurricane Katrina aftermath and its impact on diabetes care: observations from “ground zero”: lessons in disaster preparedness of people with diabetes. Diabetes Care. 2006 Jan;29(1):158–160. doi: 10.2337/diacare.29.1.158. [DOI] [PubMed] [Google Scholar]
- 18.Fonseca VA, Smith H, Kuhadiya N, Leger SM, Yau CL, Reynolds K, Shi L, McDuffie RH, Thethi T, John-Kalarickal J. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009 Sep;32(9):1632–1638. doi: 10.2337/dc09-0670. Epub 2009 Jun 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Division of Diabetes Translation. Diabetes care during natural disasters, emergencies, and hazards [monograph on the Internet]. Atlanta: National Center for Chronic Disease Prevention and Health Promotion [reviewed 2009 Sept 23; updated 2009 Sept 23; cited 2009 August 11]. Available from: http://www.cdc.gov/diabetes/news/docs/disasters.htm.
- 20.Renukuntla VS, Hassan K, Wheat S, Heptulla RA. Disaster preparedness in pediatric type 1 diabetes mellitus. Pediatrics. 2009 Nov;124(5):e973–977. doi: 10.1542/peds.2008-3648. Epub 2009 Oct 12. [DOI] [PubMed] [Google Scholar]
- 21.Katzki D, Katzki L. Disaster preparedness: it's never too early to plan ahead! Diabetes Self Manag. 2009 Sep–Oct;26(5):27–31. [PubMed] [Google Scholar]
- 22.Bernard SM, McGeehin MA. Municipal heat wave response plans. Am J Public Health. 2004 Sep;94(9):1520–1522. doi: 10.2105/ajph.94.9.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weil RM. Sports & fitness: planning an active summer. Diabetes Self Manag. 2002 May–Jun;19(3):89–94. 97, 101. [PubMed] [Google Scholar]
- 24.Swank A. The heat is on [monograph on the Internet]. Novato (CA): Diabetes Health; 2005 Jul 1 [cited 2010 Feb 9]. Available from: http://www.diabeteshealth.com/read/2005/07/01/4307/the-heat-is-on/
- 25.Medical News Today. Tips for handling summer heat for people with diabetes [monograph on the Internet]. East Sussex (United Kingdom): MediLexicon International Ltd.; 2006 Aug 13 [cited 2010 Feb 9]. Available from: http://www.medicalnewstoday.com/articles/49504.php.
- 26.Craig J. What's to drink? Staying hydrated in the heat. Diabetes Self Manag. 2006 Jul–Aug;23(4):6–8. 11-2, 14. [PubMed] [Google Scholar]
- 27.D'Arrigo T. Fun in the sun: get the most out of the season with these tips from the experts. Diabetes Forecast. 2007 Aug;60(9):54–55. [PubMed] [Google Scholar]
- 28.Weather Forecast Office. Heat index chart [monograph on the Internet]. Peachtree City (GA): National Weather Service [updated 2009 Jul 30; cited 2010 Feb 8]. Available from: http://www.srh.noaa.gov/ffc/?n=hichart.
- 29.Weather Forecast Office Excessive heat [monograph on the Internet] Peachtree City (GA): National Weather Service Weather Forecast Office [updated 2009 Aug 14;. cited 2010 Feb 8]. Available from: http://www.srh.noaa.gov/ffc/?n=heat2.
- 30.Cox DJ, Ford D, Gonder-Frederick L, Clarke W, Mazze R, Weinger K, Ritterband L. Driving mishaps among individuals with type 1 diabetes: a prospective study. Diabetes Care. 2009 Dec;32(12):2177–2180. doi: 10.2337/dc08-1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tonyushkina K, Nichols JH. Glucose meters: a review of technical challenges to obtaining accurate results. J Diabetes Sci Technol. 2009 Jul 1;3(4):971–980. doi: 10.1177/193229680900300446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ginsberg BH. Factors affecting blood glucose monitoring: sources of errors in measurement. J Diabetes Sci Technol. 2009 Jul 1;3(4):903–913. doi: 10.1177/193229680900300438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bamberg R, Schulman K, MacKenzie M, Moore J, Olchesky S. Effect of adverse storage conditions on performance of glucometer test strips. Clin Lab Sci. 2005 Fall;18(4):203–209. [PubMed] [Google Scholar]


