Abstract
The regenerative capability of enamel, the hardest tissue in the vertebrate body, is fundamentally limited due to cell apoptosis following maturation of the tissue. Synthetic strategies to promote enamel formation have the potential to repair damage, increase the longevity of teeth and improve the understanding of the events leading to tissue formation. Using a self-assembling bioactive matrix, we demonstrate the ability to induce ectopic formation of enamel at chosen sites adjacent to a mouse incisor cultured in vivo under the kidney capsule. The resulting material reveals the highly organized, hierarchical structure of hydroxyapatite crystallites similar to native enamel. This artificially triggered formation of organized mineral demonstrates a pathway for developing cell fabricated materials for treatment of dental caries, the most ubiquitous disease in man. Additionally, the artificial matrix provides a unique tool to probe cellular mechanisms involved in tissue formation further enabling the development of tooth organ replacements.
Keywords: RGDS peptide, self-assembly, peptide amphiphile, extracellular matrix, epithelial cell, cell activation, cell adhesion, biomineralization
1. Introduction
The leading cause of enamel loss is dental caries, the most prevalent and infectious disease of mankind [1]; in addition, the loss of enamel can also occur with congenital malformation, trauma and mastication. Carious destruction occurs due to a maternally derived biofilm, which produces an acidic environment leading to preferential dissolution of the mineral [2, 3]. Replacing the lost enamel currently relies on synthetic restorative materials such as polymers, metals or ceramics, which often fail due to poor adhesion or cracking. As a result, alternative materials and approaches for treating dental caries are currently under investigation [4-10].
Teeth are well known for their durability, a property attributable to the organ’s unique structure and hierarchical organization [11, 12]. The outermost covering of teeth is enamel, the hardest and most highly mineralized tissue in the vertebrate body. Enamel differs from other mineralized tissues by its origin in the ectoderm germ layer rather than the mesenchyme, its lack of collagen, and the use of a transient protein precursor to produce the highly organized mineral [13]. Mature enamel contains multiple levels of hierarchy to optimize the overall mechanical properties of the tissue [13-19]. It is comprised of nanoscale carbonated hydroxyapatite (HA) crystallites arranged anisotropically in tightly packed bundles called rods (or prisms). The rod is the fundamental structural unit of enamel and each rod contains tens of thousands of mineral crystallites with their c-axis aligned along the long axis of the rod. They are organized in distinct patterns to optimize wear resistance [15, 20]. Only trace amounts of protein are present in the mature tissue due to proteolytic processing during later stages of development, increasing overall hardness of the tissue.
Highly orchestrated extracellular processes involving proteins, supersaturated mineral ions and proteases direct the arrangement, nucleation and growth of HA crystals. The initial mineral crystals in enamel were first observed to be associated with mineralized collagen from dentin [21], however this theory was later refuted and mineral was instead found to be nucleated independently from the underlying dentin-associated collagen [22]. The enamel crystals originated in the microenvironment provided by supramolecular assemblies of enamel matrix proteins [16, 23, 24]. This matrix-mediated mineralization occurs in a delineated, extracellular space adjacent to ameloblast cells. Each cell is responsible for the synthesis of a single enamel rod [11, 25] and organization of these rods is achieved through highly controlled cell-cell interactions [15, 20]. Ameloblasts secrete a cylinder of matrix proteins principally comprised of amelogenin. Amelogenin self-assembles into nanospheres [23] to regulate the mineral phase by promoting growth of the hydroxyapatite c-axis while retarding growth along the a- and b- faces [26]. Ameloblastin, the second most abundant enamel matrix protein is associated with demarcating rod boundaries and promoting cell to matrix interactions during formation [27-29]. With proteolytic processing of proteins and removal of water, the crystallites replace the organic species and grow to approximately 60 nm in width and up to millimeters in length [17, 30].
Enamel formation originates from interactions between ectoderm-derived oral epithelium and neural crest-derived ectomesenchyme [31-33]. During the early stages of enamel formation, the dental epithelium is in contact with the basement membrane, a proteinaceous matrix responsible for providing critical signals to direct cellular proliferation and differentiation mediated in part through cell-based integrin receptors [34, 35]. Fibronectin is one of several extracellular matrix (ECM) proteins present in the basement membrane that contains an integrin-based Arg-Gly-Asp-Ser (RGDS, also referred to as RGD) domain [36-38]. Exclusively produced by cells of mesenchyme origin [39], fibronectin has also been shown to induce differentiation of ameloblasts, in vitro [40]. The recent identification of a fibronectin-binding domain in a major enamel matrix protein, ameloblastin [41], further supports the central role of integrins in development of enamel tissue. As tissue maturation continues, fibronectin and integrin expression are reduced and enamel organ epithelial (EOE) cells differentiate into secretory ameloblasts that synthesize, secrete and interact with the enamel matrix proteins that control the mineral habit. Defects in enamel matrix protein production or in cell-matrix interactions disturb enamel formation and function. For example, loss of basement membrane proteins or their receptors in the odontogenic epithelia results in deleterious impacts on enamel formation and suggests the requirement for continuous cell to matrix interactions [36, 42-47].
We chose to develop an artificial matrix and cell-based strategy for regeneration of enamel by using bioactive nanostructures to trigger biological events involved in enamel formation. The artificial matrix we used is based upon self-assembling molecules known as peptide amphiphiles (PAs). Peptide amphiphiles are small molecules comprised of a hydrophobic alkyl segment covalently conjugated to a hydrophilic peptide head group. Under physiological conditions, salts screen electrostatic repulsion between PA molecules and induce self-assembly, promoting formation of high-aspect-ratio nanofibers nanometers in diameter and up to microns in length [48-50]. The assembled nanoscale fibers mimic the ECM and display biological moieties on their surfaces in three dimensions to instruct surrounding cells to proliferate and/or differentiate [51-54]. Peptide amphiphiles exhibit biocompatibility [55] and have been designed for multiple biological applications including promoting biomineralization [56-59] and controlling the differentiation pathway of neural [52] and vascular precursors [51, 60]. Additionally, PAs displaying an integrin-specific RGD moiety have been shown to promote cell adhesion, proliferation, and differentiation [53, 54]. The density of RGDS epitopes presented on the PA surface can be controlled by using branched, linear, and even cyclic PA architectures [53, 61]. In the context of enamel regeneration, we chose to use a branched RGDS-bearing PA to provide a synthetic extracellular environment similar to that at the time of ameloblast differentiation. Additionally, the branched architecture of PAs has demonstrated increased signaling capacity relative to their linear counterparts [53, 61, 62]. Using transplantation of mouse incisors under the kidney capsule, we report here on the use of self-assembling peptide amphiphiles (PAs) displaying a branched RGDS motif to trigger the formation of enamel when injected among dental epithelial cells.
2.0 Materials and Methods
2.1 Peptide amphiphile synthesis and purification
The branched RGDS peptide amphiphiles (bRGDS PA) and its control scrambled (Scr) bRGDS PA shown in Fig. 1A and 1B, respectively were synthesized using standard 9-fluorenyl methoxy carbonyl (Fmoc) solid phase peptide synthesis [61]. Palmitic acid was attached by first removing a 4-methyltrityl (Mtt) protecting group from the ε-amine of a lysine residue and coupling the palmitic acid to the resulting free amine. The branched architecture was achieved by a similar method where the bioactive peptide sequence was coupled to the ε-amine of a lysine side chain [61]. Fmoc deprotection was performed using 30% piperidine in dimethylformamide (DMF) twice for 10 minutes each. Amino acid and palmitic acid coupling reactions were performed with a mixture of 4 molar equivalents of protected amino acid or palmitic acid, 3.95 equivalents of 2-(1H-benzotriazol-1-yl)-1,1,2,2-tetramethyluronium hexafluorophosphate (HBTU) and 6 equivalents of diisopropylethylamine (DIEA) in a solvent mixture of 50% DMF, 25% dichloromethane (DCM) and 25% N-methyl pyrrolidine (NMP) for a minimum of 1 hour. Kaiser tests were performed following amino acid and palmitic acid coupling to confirm a negative result for the presence of free amines. If necessary, the coupling was repeated until the test read a negative result. Molecules were cleaved from the resin and protecting groups removed using a mixture of 92.5% trifluoroacetic acid (TFA), 2.5% triisopropylsilane (TIS), 2.5% 1-2 ethanedithiol (EDT) and 2.5% water for 3 hours. Excess TFA and scavengers were removed by rotary evaporation and the remaining solution was triturated with cold diethyl ether to form a white precipitate. MBHA Rink amide resin, Fmoc protected amino acids, Boc-Lys (Boc)-OH, Fmoc-Lys(Mtt)-OH and HBTU were purchased from EMD Chemicals, Inc. All other reagents were purchased from VWR.
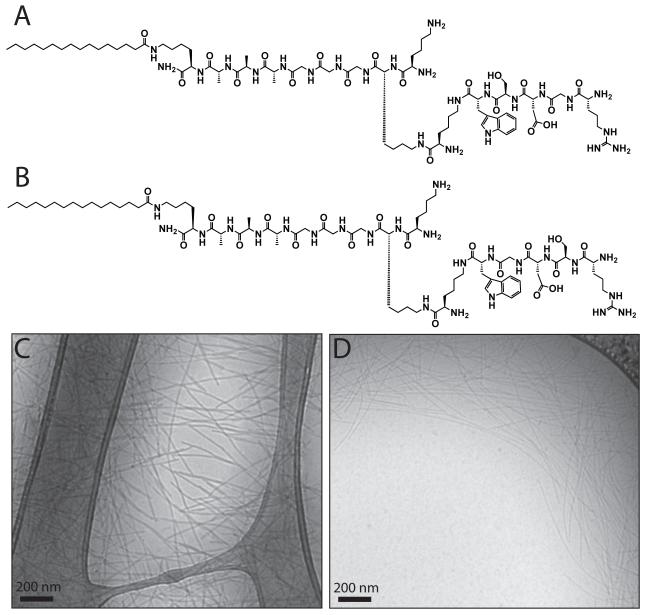
Figure 1. Characterization of peptide amphiphile assembly.
Chemical structures of (A) the branched RGDS-bearing peptide amphiphile (bRGDS PA) and (B) a scrambled control molecule (Scr bRGDS PA) that has a charge matched, but altered amino acid sequence to disrupt bioactivity. Cryogenic TEM images of the (C) bRGDS PA and the (D) Scr bRGDS PA demonstrate the formation of cylindrical micelles at 1% (w/v) in phosphate buffered saline.
All molecules were purified using reverse phase high performance liquid chromatography (HPLC) on a Varian Prostar Model 210 preparative scale HPLC system equipped with a Phenomenex Gemini NX column (C18 stationary phase, 5 μm, 100Å, 30 × 150 mm). A mobile gradient of water and acetonitrile with 0.1% TFA was used at a flow rate of 25 mL/min. The elution of the molecules was monitored by UV absorbance at 220 nm and 280 nm. Purified fractions were characterized by electrospray ionization mass spectrometry (ESI-MS) using an Agilent 6510 quadrupole time-of-flight (Q-Tof) instrument. Pure fractions were collected and combined and excess organic solvent was removed using rotary evaporation. The molecules were lyophilized and stored at −20°C until use.
For visualization, a rhodamine tagged PA was prepared using 5-rhodamine carboxylic acid (Anaspec) activated with neat thionyl chloride (Sigma-Aldrich). The fluorescent dye was coupled to the ε-amine of the terminal lysine following Mtt deprotection in place of the bioactive peptide sequence.
2.2 Cryogenic transmission electron microscopy
Cryogenic transmission electron microscopy (cryo-TEM) was performed on a JEOL 1230 microscope with an accelerating voltage of 100 kV. A Vitrobot Mark IV equipped with controlled humidity and temperature was used for plunge freezing samples. A small volume (5-10 μL) of the peptide amphiphile at 1% (w/v) in phosphate buffered saline (Hyclone Inc.) was deposited on a copper TEM grid with holey carbon support film (Electron Microscopy Sciences) and held in place with tweezers mounted to the Vitrobot. The specimen was blotted in environment with 90-100% humidity and plunged into a liquid ethane reservoir that was cooled by liquid nitrogen. The vitrified samples were transferred in a nitrogen environment into liquid nitrogen and transferred to a Gatan 626 cryo-holder using a cryo-transfer stage. Samples were imaged using a Hamatsu CCD camera.
2.3 Injection and long term culture of mouse incisors
Animal experiments were performed under a protocol approved by the Institutional Animal Care and Use Committee. Timed pregnant Swiss Webster mice were euthanized (vaginal plug = day 0) and tooth organs were harvested as described previously [63]. Briefly, following overnight culture at the air-media interface, in an atmosphere of 5% CO2 and 95% air at 37°C, the incisor primordia were injected with approximately 5-10 nanoliters cell culture medium (sham treatment) or selected peptide amphiphiles at a concentration of 1% (w/v) through a heat-drawn borosilicate glass capillary. For some organs, multiple injections were performed along the rostral-caudal gradient of epithelial differentiation exhibited by the incisor tooth organ [63, 64].
For long-term culture of 8 to 10 weeks, incisors were transplanted under the kidney capsules of host mice. Under general anesthesia, the left kidney of a host mouse (Swiss-Webster or GFP-transgenic mouse) was exteriorized. The PA-injected embryonic dental organs were inserted through a small incision in the renal capsule and were allowed to develop beneath the capsules for variable periods of time. The grafts were harvested and processed after selected periods of time.
2.4.1 Microcomputed tomography
The injected tooth organs were recovered from the host’s kidney capsule and subjected to microcomputed tomography (microCT) analysis using a Siemens microCAT II operating at 80 kV and 250 μA with 10μm voxel resolution. Reconstruction of the virtual slices and three-dimensional rendering was performed using Siemens proprietary software. Sites of mineral density were assigned based on a minimal threshold set by the density of the authentic enamel. Increased values of attenuation were used to identify putative sites of enamel nodule formation.
2.4.2 Focused ion beam milling and SEM imaging
For preparation of transmission electron microscopy (TEM) specimens of authentic enamel and ectopic enamel pearls, a Helios Nanolab SEM/FIB (FEI) equipped with an in situ nanomanipulator (AutoProbe™ 200, Omniprobe Inc.) was used following standard procedures for in situ lift out and thinning described previously [65]. Prior to the lift-out process, the sample was dehydrated in a graded ethyl alcohol series, dried at the critical point of CO2 using a Tousimis Samdri-795 critical point dryer and mounted on a scanning electron microscopy (SEM) stub with carbon adhesive (Electron Microscopy Sciences). The sample was coated with approximately 50 nm of platinum using a Denton Desk III magnetron sputter coater. Using the SEM/FIB, the sample was imaged using the electron beam and milled using a gallium focused ion beam (FIB). A strap of FIB-deposited platinum (FIB-Pt) was deposited over the region of interest and large trenches were subsequently milled on both sides of the deposited metal at 30 kV. The sample was cut free with the FIB and mounted to a nanomanipulator using FIB-Pt. The sample was transferred and welded with FIB-Pt to a copper half TEM grid (Omniprobe, Inc.) and the nanomanipulator was milled free. The sample was successively thinned edge-on with the ion beam at 90 degree incidence and as a final step the sample was cleaned with low energy 5 kV ions.
2.6 Transmission electron microscopy and elemental spectroscopy
Bright-field scanning transmission electron microscopy (STEM) imaging of focused ion beam FIB milled samples was performed on a Hitachi HD2300A STEM with an accelerating voltage of 200 kV. Selected area electron diffraction of transmission electron microscopy (TEM) samples of enamel pearls and authentic enamel was performed on a Hitachi H-8100 TEM operating at 200 kV. Energy dispersive X-ray spectroscopy (EDS) was carried out using a silicon drift EDS detector (Oxford Instruments) in a JEOL 2100F TEM operating at 200 kV. Several areas were selected and Ca/P ratios were averaged over multiple areas. Elemental quantitative analysis was obtained using the Oxford Instruments INCA microanalysis suite.
2.7 Immunohistochemistry
Immunostaining was performed as described previously [63]. Briefly, the PA-injected tooth organs were fixed overnight in freshly prepared 4% paraformaldehyde in PBS, pH 7.4, at 4 °C. In selected cases, the injected organs were partly demineralized using isotonic 100 mM ethylene diamine tetra acetic acid (EDTA) to chelate the mineral phase to permit serial sectioning of paraffin embedded samples. Tissue sections of 6 μm in thickness were prepared and blocked for nonspecific absorption. After incubation with the selected primary antibody, the localization of the antibody-antigen was visualized with a suitable chromogen-tagged secondary antibody. In the case of the anti-mouse amelogenin polyclonal antibody (1:1000) raised in chicken and recovered from the egg yolk as IgY, an anti-chicken horseradish peroxidase (HRP)-conjugated secondary antibody (1:1500, Zymed) and a peroxidase substrate (AEC, Invitrogen) was used for detection by local precipitation of the visible chromogen.
2.8 Fluorescent microscopy
Imaging of 15 μm thick paraffin embedded tissue sections with regenerated enamel pearls were performed using a Nikon TE300 Quantum upright confocal microscope. Excitation of hematoxylin and eosin (H&E) stained sections was achieved using Ar and HeNe lasers. The emission peak of 545 nm was used for eosin-Y, the main fluorescent component in eosin.
2.9 Statistical analysis
Each experiment was repeated at least three times. Statistical analysis was performed using the student’s t-test and statistical significance is defined as p < 0.05.
3.0 Results and discussion
3.1.1 Injection of bRGDS PA into the developing murine incisor
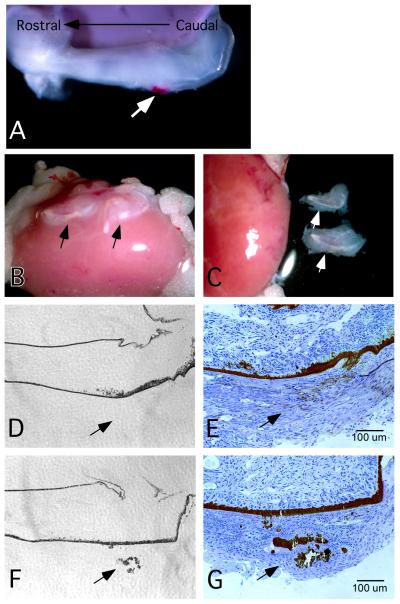
Branched RGDS-containing peptide amphiphiles (bRGDS PA, Fig. 1A) and a control non-bioactive molecule containing a “scrambled” form of the signal and the same formal charge (RSDG sequence) (Scr bRGDS PA, Fig. 1B) both formed high aspect ratio cylindrical nanofibers in a physiological salt solution as evidenced by cryoTEM (Figs. 1C and 1D). These self-assembled nanostructures display a high density of the RGDS bioactive epitope on the nanofiber surface. When injected along the rostral-caudal developmental gradient of the mouse incisor (Fig 2A), the PA undergoes self-assembly and remains localized at the site of injection. The injection site was chosen such that the PA was administered exclusively in the enamel organ epithelia, avoiding the underlying dentin-forming mesenchyme of the developing tooth [63]. Long-term culture of the 1-day postnatal PA injected incisors was achieved by transplanting the organs under the renal capsule of a recipient mouse (Fig. 2B). The organs were recovered at designated time points for further analysis (Fig. 2C). Previously, we have shown that the artificial PA matrix induced both cell proliferation and differentiation in the odontogenic epithelia that came into contact with the material [63]. To illustrate the capability of the bRGDS PA to promote biomineralization, Figs. 2D-G show tissue sections of a bRGDS PA injected incisor stained with von Kossa dye to visualize calcium. Mineral deposits were observed in the recovered bRGDS PA injected incisors after only 3-days of transplantation under the renal capsule (Figs. 2F-G). In contrast, identical incisors injected with the Scr RGDS PA consistently failed to induce mineral deposits (Figs. 2D-E). This rapid onset of biomineralization indicates that the RGDS epitopes on the surface of the bRGDS PA are capable of signaling surrounding cells to begin production of a matrix competent for mineral accumulation.
Figure 2. Animal model for injection of peptide amphiphiles into mouse incisors.
Peptide amphiphiles are injected adjacent to the ameloblasts of 1-day postnatal dental incisors, explanted to the renal capsule for selected times and recovered for analysis. (A) 1-day postnatal dental incisor injected with bRGDS PA mixed with a rhodamine containing PA to fluorescently label the site of injection. The injection site (arrow) can be varied along the rostral-caudal gradient of incisor development. The number of injections within a single incisor can also be varied from one to multiple sites. Following injection of the incisors, they are (B) surgically placed under the kidney capsule for selected periods of time. (C) Incisors are explanted and dissected free of the capsule for further analysis. (D-G) show incisors recovered from the renal capsule after three days’ culture. (D, F) Phase contrast images of the incisor injected with the control scrambled peptide amphiphile and the bioactive bRGDS PA, respectively. (E, G) Calcium salts were identified using von Kossa staining with Kohler illumination of incisors injected with the control scrambled peptide amphiphile and the bioactive bRGDS PA, respectively. Mineral deposits only formed in the bRGDS PA injected incisors.
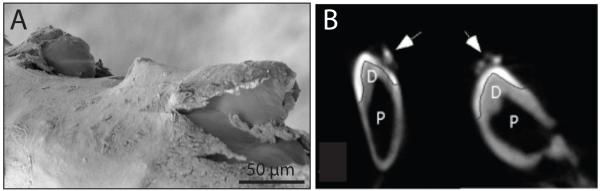
To further investigate the effect of culturing the incisors for longer time periods, the bRGDS PA was administered and the incisors were maintained for 8-10 weeks beneath the kidney capsule of a host mouse. Following culture, the incisors were excised and SEM consistently revealed the presence of elliptically shaped mineralized structures at the PA injection site (Fig. 3A). We have termed these structures as enamel pearls. These enamel pearls formed in 100% of the bRGDS PA injected incisors (n=16) as shown in Table 1, whereas in the Scr bRGDS PA (n=12) and sham injected (n=10) groups, mineralized nodules did not form. Additionally, multiple injections of the bRGDS PA resulted in a one to one concordance in ectopic enamel pearl formation regardless of the location of the injection site along the rostral-caudal gradient of differentiation in the mouse incisor. These pearls were also visualized by microcomputed tomography (microCT). A representative microCT cross sectional image of an injected incisor reveals singular or multiple radiographic densities adjacent to the authentic enamel at the site of single or multiple bRGDS PA injections (Fig. 3B, arrows).
Figure 3. Regenerated enamel pearls form at the site of peptide amphiphile injection.
(A) SEM reveals the presence of pearls along the anterior enamel surface at sites of injected bRGDS PA. (B) Microcomputed tomography reveals the presence of enamel pearls (arrows) adjacent to authentic enamel in a sagittal view of the PA-injected incisors. Multiple bRGDS PA injection sites result in multiple sites of ectopic enamel formation. A line is introduced to demarcate the enamel (E) from the underlying dentin (D) and the soft-tissue containing pulp chamber (P).
Table 1.
Enamel pearl formation for bioactive or control treatments
| Sham Treatment | Scr bRGDS PA | bRGDS PA | |
|---|---|---|---|
| Total samples (n) | 10 | 12 | 16 |
| Number of enamel “pearls” formed |
0 | 0 | 16 |
| Total Yield (%) | 0 | 0 | 100 |
3.1.2 Characterization of enamel pearl ultrastructure
To characterize the structure of the enamel pearls on the nanoscale, we employed an in situ lift-out technique using a FIB to prepare a sample for TEM (Supplemental Fig. 1). FIB milling techniques have been widely used for preparing TEM specimens for a large range of materials [65] including semiconductors, metals, ceramics, polymers and more recently, biological tissues including bone-like ivory dentin [66] and human dentin [67]. This technique is extremely useful because it allows the possibility of creating a highly site specific preparation in either cross section or plane view.
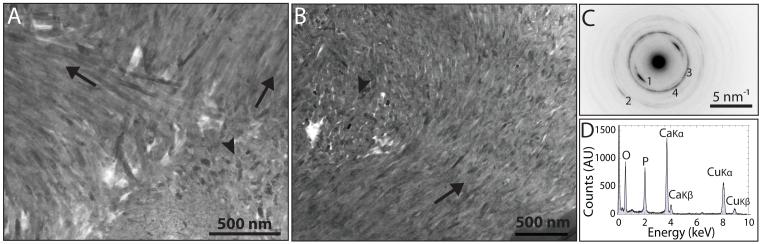
We performed FIB in situ TEM lift-outs of both canonical enamel (Supplemental Fig. 2) and enamel pearls (Figs. 4A-B) to compare the structural organization and crystallinity of the mineral phase. Both authentic enamel and enamel pearls exhibited aligned crystallites arranged in bundles identical to rods, the structural unit of enamel tissue. Additionally, pearls obtained from different locations along the rostral-caudal developmental gradient exhibited crystallite organization consistent with mature enamel (Figs. 4A-B). Selected area electron diffraction of enamel pearl samples indicated the presence of a polycrystalline hydroxyapatite with preferential orientation of the c-axis in the direction of the rod, as evidenced by a clear texture of the (002) arcs in the diffraction pattern (Fig. 4C). This texture is well documented and has been observed previously in the most mature region of canonical enamel [68]. Energy dispersive X-ray spectroscopy (EDS) revealed the mineral components to be composed primarily of calcium and phosphorus (Fig. 4D). The Ca/P ratios were similar for both the authentic enamel (1.57 ± 0.13) and enamel pearl (1.53 ± 0.10) when prepared using FIB milling techniques. With comparable crystal habit and crystallite orientation, the PA-triggered enamel pearls are nearly identical in composition and architecture to mature authentic enamel.
Figure 4. The ultrastructure of the enamel pearl reveals aligned rod-like structures consisting of aligned hydroxyapatite crystals.
Bright field STEM images of FIB milled samples revealed rod structures sectioned longitudinally (arrows) and in cross section (arrowheads). Images of enamel pearl lift-outs located in a rostral (A) segment of development and a caudal (B) section of the developing incisor. (C) Selected area for electron diffraction of the pearls indicate that they are made of hydroxyapatite with texture along the c-axis in the direction of the rod imaged in (B), identical to authentic enamel. 1: (002), 2: (004), 3: (211), 4: (310) (D) A representative EDS spectrum showing that the pearl is composed of calcium and phosphorus, as expected. The copper X-ray emission lines are due to the copper grid on which the sample was mounted.
Both microCT (Fig. 3) and hematoxylin and eosin (H&E) (Fig. 5A-C) staining of tissue sections taken from the PA injected incisors revealed the presence of the enamel pearls separate from the developed enamel organ. Histological sections identified the pearl to be a uniformly eosinophilic structure separated from the enamel organ (Fig. 5A). Since the enamel pearl is being nucleated in the absence of an underlying mesenchyme, this phenomenon directly proves that neither collagen from dentin nor a mineral substrate for epitaxial growth is required to form the complex, mineralized enamel tissue. The presence of a nanofiber gel alone with a scrambled RGDS epitope was incapable of nucleating mineral, indicating that the nanofiber structure alone was not sufficient to induce mineralization (Table 1). Thus, we believe that the bRGDS PA is acting through a variety of cell-matrix interactions to provide a niche in which cells are capable of differentiating and secreting enamel matrix proteins that subsequently nucleate hydroxyapatite.
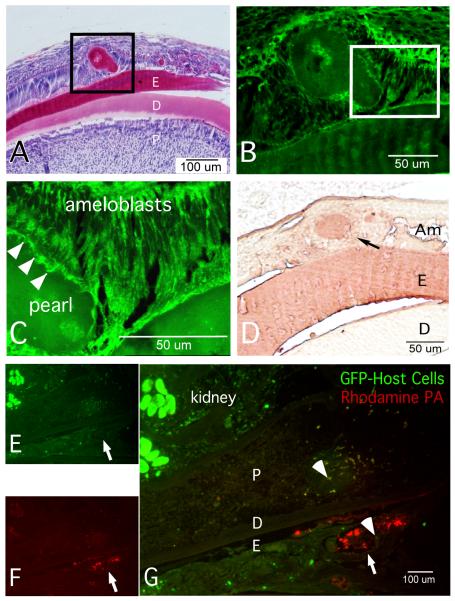
Figure 5. Incisors injected with bRGDS PA forms regenerated enamel nodules in the shape of a pearl, complete with ameloblasts after 56 days in the kidney capsule.
(A) shows a representative tissue section of a bRGDS PA injected incisor stained with hematoxylin and eosin in Kohler illumination. (B, C) show laser excited fluorescence images of the hematoxylin and eosin (H & E) section shown in (A) captured by confocal microscopy of the nodule at lower (B) and higher (C) magnification. The cells contacting the nodule are polarized and resemble authentic ameloblasts with the specialized secretory-end of the ameloblast know as Tomes’ processes (arrowheads). (D) Amelogenin immunostaining of a representative section containing an enamel pearl detected enamel matrix protein production and accumulation. To identify host cells that could contribute to pearl formation, a transgenic mouse strain constitutively expressing a green fluorescent protein (E) was used as a host for a wild type incisor primordia injected with a combination of rhodamine conjugated PA and bioactive bRGDS PA (F). The merged image (G) shows several GFP-marked cells (arrowheads) surrounding the bRGDS PA injection site and within the pulp (P). None of the ameloblast cells contributing to the formation of the pearl are GFP-labeled suggesting that they originate from the incisor tooth and not from the host. Abbreviations: P, pulp; D, dentin; E, enamel.
3.3 Cellular organization surrounding enamel pearls
To characterize the cellular organization and morphology during enamel pearl formation, tissue sections were taken from the PA injected incisors. After demineralization and staining with H&E (Fig 5A), there was no indication of residual PA matrix; instead, a material that stained uniformly by eosin was present. The periphery of this structure contained ameloblast cells that exhibited a highly polarized cytology (Figs. 5B-C). At higher magnification, the apical pole of the cells surrounding the regenerated tissue were observed to form a secretory end piece in contact with the eosinophilic matrix similar to the Tomes’ process of an ameloblast cell (Fig. 5C, arrowheads). Each of these cells appeared to organize the extracellular matrix identical to the manner in which ameloblasts engaged in formation of authentic enamel tissue. Using immunohistochemical detection, we found that these polarized cells expressed the enamel matrix protein, amelogenin (Fig. 5D), the most abundant protein found within forming mammalian enamel [69]. We conclude that the pearl is a nodule of regenerated enamel, organized by polarized ameloblast cells that surround the PA injection site. These cells are sufficiently differentiated to secrete enamel matrix proteins from their apical pole into the extracellular matrix space forming regenerated ectopic enamel pearl.
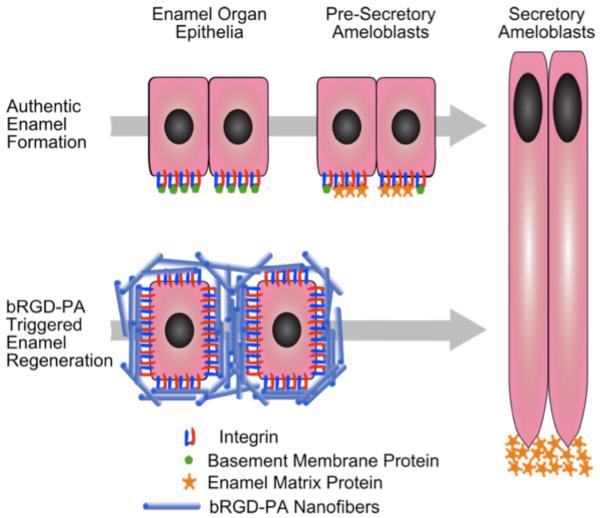
In previous studies, we have shown that the artificial matrix served to initiate cell proliferation, increase integrin expression and organize the surrounding cells [63]. After longer intervals, we demonstrate further cell differentiation as evidenced by cell polarity with the nucleus moving away from the artificial matrix and the secretion of enamel matrix proteins into the extracellular space formed between the PA and the secretory end of the differentiated ameloblasts. These proteins include amelogenin (Fig. 5D). When PA injected organs are transferred to the kidney capsule to support long-term development, the artificial matrix admixes with enamel matrix proteins and is converted into mature mineralized enamel over the eight-week transplantation period. We propose that the bRGDS PA serves as an acellular equivalent to the dental ectomesenchyme that is associated with authentic enamel formation. It is well appreciated that the odontogenic epithelium is patterned by a variety of growth factors and matrix ligands that guide cell fate and instruct their differentiation to ameloblasts while regulating the amount of enamel produced at a specific site [70-73]. These data suggest that the bRGDS PA triggers naive cells to behave as if they were taking part in authentic enamel production, resulting in the formation of a regenerated nodule of enamel (Fig. 6).
Figure 6. The artificial matrix displaying a high density of RGDS epitopes serves as a signal to induce changes in gene expression in the odontogenic epithelia that it contacts.
The artificial matrix provides cell-matrix interactions similar to that of the dental mesenchyme during authentic enamel formation. The responding cells differentiate along an ameloblast lineage and enamel matrix proteins accumulate to produce an extracellular matrix capable of guiding the habit and orientation of hydroxyapatite crystals yielding a pearl of enamel analogous to authentic enamel.
Furthermore, we show that cells contributing to the formation of the pearls most likely arise from cells of the enamel organ and not from the host animal. Anticipating the potential for host stem cells to contribute to the pearl, we examined multiple incisors grafted to the kidney capsule in which all host cells were marked with green fluorescent protein (GFP) (Figs. 5 E-G). While we identified GFP-labeled host cells adjacent to the regenerated epithelial tissue (Fig. 5G, arrows), GFP-labeled stem cells in the vicinity of ameloblasts engaged in forming the regenerated ectopic enamel pearl were not observed. Interestingly, GFP-labeled stem cells were also observed in the mesenchyme of the pulp tissue (Fig. 5G, arrowhead). The signals responsible for recruiting these cells into the pulp tissue underlying the site of the PA injection suggests a diffusible signal, however investigating these signals further is beyond the scope of this paper. It is possible that sampling limits our ability to identify the rare event of a stem cell differentiating into a functional ameloblast, as reported previously [74].
3.4 Paradigm shifts for regenerated enamel
Among the phenomena relevant to tooth development demonstrated in these experiments, we focus on the issues of epithelial plasticity, cell polarity, cell-to-cell interactions, mineral nucleation and control over the mineral habit. With regard to epithelial plasticity, we show that the artificial matrix created by the self-assembling peptide amphiphile is competent to provide both permissive and inductive signals to the enamel organ epithelium (EOE) with which it makes contact. The nanofibers display RGDS signals that are denser than what one would expect from native matrix molecules [53]. The EOE cells respond to this dense array of epitopes by up-regulating the integrin signaling cascade and re-entering a proliferative state prior to differentiating into ameloblasts [63]. Noteworthy is the fact that during authentic tooth development, the EOE cells contacts the mesenchyme and basement membrane with only one surface. In contrast, with the self-assembling PA matrix, the EOE cells are initially circumscribed by this matrix and receive signals simultaneously in three dimensions. This creates a physically unique matrix milieu that does not exist during authentic development. The artificial matrix also provides permissive signals to the proliferating EOE cells resulting in re-establishment of a basement membrane microenvironment. We hypothesize that the artificial matrix combined with the basement membrane components that are synthesized serve as an ectomesenchyme equivalent. The RGDS PA injection site and the resulting regenerated enamel pearl contain only ectoderm-derived cells that cannot make contact with the ectomesenchyme cells that are physically isolated some distance away. The cells differentiate as enamel matrix producing ameloblasts and re-establish cell polarity with respect to the artificial matrix. With the expression of enamel matrix proteins, the RGDS PA appears to be converted into a biomineralized pearl of enamel. The ameloblasts in contact with the regenerated nodule of enamel control the biomineralization of the matrix similarly to authentic enamel, forming rod-to-rod boundaries that reflect the ameloblast to ameloblast boundaries comprising the pearl. The rod organization is reflected by the protein secretion patterns of ameloblasts, which are responsible for guiding the final mineral habit and orientation. The matrix also initiates mineral deposition as demonstrated in the short-term culture experiments in which calcium salts are deposited in the bioactive matrix but not in the control matrix.
4 Conclusions
We have created an artificial matrix composed of self-assembling nanofibers displaying a high density of the epitope RGDS. With this matrix, we have demonstrated the ability to induce the proliferation and differentiation of ameloblasts that are competent to synthesize, organize and biomineralize an enamel nodule physically separated from the authentic enamel. The capability to trigger, at will, the formation of enamel nodules containing structures analogous to authentic enamel affords unique potential to provide authentic enamel to replace that lost to disease, trauma and congenital defects.
Supplementary Material
Acknowledgements
The authors are grateful for funding from the National Institute for Dental and Craniofacial Research (NIDCR) 5R01DE015920-05.
Confocal fluorescent images were acquired at the USC Keck Center for Liver Diseases Confocal Microscopy Core, supported by NIH, USPHS grant P50AA11999. Microtomography images were acquired at the USC Molecular Imaging Center. The SEM/FIB and analytical TEM work was performed in the EPIC facility of NUANCE Center at Northwestern University. The NUANCE Center is supported by NSF-NSEC, NSF-MRSEC, Keck Foundation, the State of Illinois and Northwestern University. The cryo-TEM was performed at the Northwestern University Biological Imaging Facility generously supported by the NU Office for Research.
The authors would like to thank the following colleagues for their invaluable assistance with the following techniques: Mr. Ben Myers for FIB milling and TEM sample preparation techniques; Ms. Archana Tank and Mr. Ryan Park for microtomography and image processing; Ms. Michelle MacVeigh-Aloni for confocal imaging and processing; Dr. Byungmin Ahn for SEM imaging and FIB milling.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Taubman MA, Nash DA. The scientific and public-health imperative for a vaccine against dental caries. Nat Rev Immunol. 2006;6:555–63. doi: 10.1038/nri1857. [DOI] [PubMed] [Google Scholar]
- [2].Robinson C, Shore RC, Brookes SJ, Strafford S, Wood SR, Kirkham J. The chemistry of enamel caries. Crit Rev Oral Biol Med. 2000;11:481–95. doi: 10.1177/10454411000110040601. [DOI] [PubMed] [Google Scholar]
- [3].Caufield PW, Li Y, Dasanayake A. Dental caries: an infectious and transmissible disease. Compend Contin Educ Dent. 2005;26:10–6. [PubMed] [Google Scholar]
- [4].Hu B, Nadiri A, Kuchler-Bopp S, Perrin-Schmitt F, Peters H, Lesot H. Tissue Engineering of Tooth Crown, Root, and Periodontium. Tissue Eng. 2006;12:2069–75. doi: 10.1089/ten.2006.12.2069. [DOI] [PubMed] [Google Scholar]
- [5].Mitsiadis TA, Graf D. Cell fate determination during tooth development and regeneration. Birth Defects Res C Embryo Today. 2009;87:199–211. doi: 10.1002/bdrc.20160. [DOI] [PubMed] [Google Scholar]
- [6].Duailibi SE, Duailibi MT, Vacanti JP, Yelick PC. Prospects for tooth regeneration. Periodontol 2000. 2006;41:177–87. doi: 10.1111/j.1600-0757.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- [7].Chai Y, Slavkin HC. Prospects for tooth regeneration in the 21st century: a perspective. Microsc Res Tech. 2003;60:469–79. doi: 10.1002/jemt.10287. [DOI] [PubMed] [Google Scholar]
- [8].Thesleff I, Wang XP, Suomalainen M. Regulation of epithelial stem cells in tooth regeneration. C R Biol. 2007;330:561–4. doi: 10.1016/j.crvi.2007.03.005. [DOI] [PubMed] [Google Scholar]
- [9].Snead ML. Whole-tooth regeneration: it takes a village of scientists, clinicians, and patients. J Dent Educ. 2008;72:903–11. [PMC free article] [PubMed] [Google Scholar]
- [10].Sharpe PT, Young CS. Test-tube teeth. Sci Am. 2005;293:34–41. doi: 10.1038/scientificamerican0805-34. [DOI] [PubMed] [Google Scholar]
- [11].Boyde A. Microstructure of enamel. Ciba Found Symp. 1997;205:18–27. doi: 10.1002/9780470515303.ch3. discussion-31. [DOI] [PubMed] [Google Scholar]
- [12].Zaslansky P, Friesem AA, Weiner S. Structure and mechanical properties of the soft zone separating bulk dentin and enamel in crowns of human teeth: insight into tooth function. J Struct Biol. 2006;153:188–99. doi: 10.1016/j.jsb.2005.10.010. [DOI] [PubMed] [Google Scholar]
- [13].Paine ML, White SN, Luo W, Fong H, Sarikaya M, Snead ML. Regulated gene expression dictates enamel structure and tooth function. Matrix Biol. 2001;20:273–92. doi: 10.1016/s0945-053x(01)00153-6. [DOI] [PubMed] [Google Scholar]
- [14].Weiner S, Addadi L. Biomineralization. At the cutting edge. Science. 2002;298:375–6. doi: 10.1126/science.1078093. [DOI] [PubMed] [Google Scholar]
- [15].White SN, Luo W, Paine ML, Fong H, Sarikaya M, Snead ML. Biological organization of hydroxyapatite crystallites into a fibrous continuum toughens and controls anisotropy in human enamel. J Dent Res. 2001;80:321–6. doi: 10.1177/00220345010800010501. [DOI] [PubMed] [Google Scholar]
- [16].Robinson C, Brookes SJ, Shore RC, Kirkham J. The developing enamel matrix: nature and function. Eur J Oral Sci. 1998;106(Suppl 1):282–91. doi: 10.1111/j.1600-0722.1998.tb02188.x. [DOI] [PubMed] [Google Scholar]
- [17].Smith CE. Cellular and chemical events during enamel maturation. Crit Rev Oral Biol Med. 1998;9:128–61. doi: 10.1177/10454411980090020101. [DOI] [PubMed] [Google Scholar]
- [18].Simmer JP, Fincham AG. Molecular mechanisms of dental enamel formation. Crit Rev Oral Biol Med. 1995;6:84–108. doi: 10.1177/10454411950060020701. [DOI] [PubMed] [Google Scholar]
- [19].Fong H, White SN, Paine ML, Luo W, Snead ML, Sarikaya M. Enamel structure properties controlled by engineered proteins in transgenic mice. J Bone Miner Res. 2003;18:2052–9. doi: 10.1359/jbmr.2003.18.11.2052. [DOI] [PubMed] [Google Scholar]
- [20].Bechtle S, Habelitz S, Klocke A, Fett T, Schneider GA. The fracture behaviour of dental enamel. Biomaterials. 2009;31:375–84. doi: 10.1016/j.biomaterials.2009.09.050. [DOI] [PubMed] [Google Scholar]
- [21].Arsenault AL, Robinson BW. The dentino-enamel junction: a structural and microanalytical study of early mineralization. Calcif Tissue Int. 1989;45:111–21. doi: 10.1007/BF02561410. [DOI] [PubMed] [Google Scholar]
- [22].Diekwisch TG, Berman BJ, Gentner S, Slavkin HC. Initial enamel crystals are not spatially associated with mineralized dentine. Cell Tissue Res. 1995;279:149–67. doi: 10.1007/BF00300701. [DOI] [PubMed] [Google Scholar]
- [23].Fincham AG, Moradian-Oldak J, Diekwisch TG, Lyaruu DM, Wright JT, Bringas P, Jr., et al. Evidence for amelogenin “nanospheres” as functional components of secretory-stage enamel matrix. J Struct Biol. 1995;115:50–9. doi: 10.1006/jsbi.1995.1029. [DOI] [PubMed] [Google Scholar]
- [24].Tarasevich BJ, Howard CJ, Larson JL, Snead ML, Simmer JP, Paine M, et al. The nucleation and growth of calcium phosphate by amelogenin. J Cryst Growth. 2007;304:407–15. doi: 10.1016/j.jcrysgro.2007.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Warshawsky H, Smith CE. A three-dimensional reconstruction of the rods in rat maxillary incisor enamel. Anat Rec. 1971;169:585–91. doi: 10.1002/ar.1091690308. [DOI] [PubMed] [Google Scholar]
- [26].Du C, Falini G, Fermani S, Abbott C, Moradian-Oldak J. Supramolecular assembly of amelogenin nanospheres into birefringent microribbons. Science. 2005;307:1450–4. doi: 10.1126/science.1105675. [DOI] [PubMed] [Google Scholar]
- [27].Hu CC, Fukae M, Uchida T, Qian Q, Zhang CH, Ryu OH, et al. Sheathlin: cloning, cDNA/polypeptide sequences, and immunolocalization of porcine enamel sheath proteins. J Dent Res. 1997;76:648–57. doi: 10.1177/00220345970760020501. [DOI] [PubMed] [Google Scholar]
- [28].Fukumoto S, Kiba T, Hall B, Iehara N, Nakamura T, Longenecker G, et al. Ameloblastin is a cell adhesion molecule required for maintaining the differentiation state of ameloblasts. J Cell Biol. 2004;167:973–83. doi: 10.1083/jcb.200409077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zhu D, Paine ML, Luo W, Bringas P, Jr., Snead ML. Altering biomineralization by protein design. J Biol Chem. 2006;281:21173–82. doi: 10.1074/jbc.M510757200. [DOI] [PubMed] [Google Scholar]
- [30].Simmer JP, Hu JC. Expression, structure, and function of enamel proteinases. Connect Tissue Res. 2002;43:441–9. doi: 10.1080/03008200290001159. [DOI] [PubMed] [Google Scholar]
- [31].Slavkin HC. Molecular determinants of tooth development: a review. Crit Rev Oral Biol Med. 1990;1:1–16. doi: 10.1177/10454411900010010201. [DOI] [PubMed] [Google Scholar]
- [32].Jowett AK, Vainio S, Ferguson MW, Sharpe PT, Thesleff I. Epithelial-mesenchymal interactions are required for msx 1 and msx 2 gene expression in the developing murine molar tooth. Development. 1993;117:461–70. doi: 10.1242/dev.117.2.461. [DOI] [PubMed] [Google Scholar]
- [33].Chen Y, Bei M, Woo I, Satokata I, Maas R. Msx1 controls inductive signaling in mammalian tooth morphogenesis. Development. 1996;122:3035–44. doi: 10.1242/dev.122.10.3035. [DOI] [PubMed] [Google Scholar]
- [34].Thesleff I, Vaahtokari A, Partanen AM. Regulation of organogenesis. Common molecular mechanisms regulating the development of teeth and other organs. Int J Dev Biol. 1995;39:35–50. [PubMed] [Google Scholar]
- [35].Salmivirta K, Gullberg D, Hirsch E, Altruda F, Ekblom P. Integrin subunit expression associated with epithelial-mesenchymal interactions during murine tooth development. Dev Dyn. 1996;205:104–13. doi: 10.1002/(SICI)1097-0177(199602)205:2<104::AID-AJA2>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- [36].Fukumoto S, Yamada Y. Review: extracellular matrix regulates tooth morphogenesis. Connect Tissue Res. 2005;46:220–6. doi: 10.1080/03008200500344017. [DOI] [PubMed] [Google Scholar]
- [37].Thesleff I, Stenman S, Vaheri A, Timpl R. Changes in the matrix proteins, fibronectin and collagen, during differentiation of mouse tooth germ. Dev Biol. 1979;70:116–26. doi: 10.1016/0012-1606(79)90011-3. [DOI] [PubMed] [Google Scholar]
- [38].Gollard RP, Slavkin HC, Snead ML. Polyoma virus-induced murine odontogenic tumors. Oral Surg Oral Med Oral Pathol. 1992;74:761–7. doi: 10.1016/0030-4220(92)90405-f. [DOI] [PubMed] [Google Scholar]
- [39].Hurmerinta K, Kuusela P, Thesleff I. The cellular origin of fibronectin in the basement membrane zone of developing tooth. J Embryol Exp Morphol. 1986;95:73–80. [PubMed] [Google Scholar]
- [40].Tabata MJ, Matsumura T, Fujii T, Abe M, Kurisu K. Fibronectin accelerates the growth and differentiation of ameloblast lineage cells in vitro. J Histochem Cytochem. 2003;51:1673–9. doi: 10.1177/002215540305101211. [DOI] [PubMed] [Google Scholar]
- [41].Beyeler M, Schild C, Lutz R, Chiquet M, Trueb B. Identification of a fibronectin interaction site in the extracellular matrix protein ameloblastin. Exp Cell Res. 2010;316:1202–12. doi: 10.1016/j.yexcr.2009.12.019. [DOI] [PubMed] [Google Scholar]
- [42].Asaka T, Akiyama M, Domon T, Nishie W, Natsuga K, Fujita Y, et al. Type XVII collagen is a key player in tooth enamel formation. Am J Pathol. 2009;174:91–100. doi: 10.2353/ajpath.2009.080573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Wright JT, Hall KI, Deaton TG, Fine JD. Structural and compositional alteration of tooth enamel in hereditary epidermolysis bullosa. Connect Tissue Res. 1996;34:271–9. doi: 10.3109/03008209609005271. [DOI] [PubMed] [Google Scholar]
- [44].Fukumoto S, Miner JH, Ida H, Fukumoto E, Yuasa K, Miyazaki H, et al. Laminin alpha5 is required for dental epithelium growth and polarity and the development of tooth bud and shape. J Biol Chem. 2006;281:5008–16. doi: 10.1074/jbc.M509295200. [DOI] [PubMed] [Google Scholar]
- [45].Bei M, Stowell S, Maas R. Msx2 controls ameloblast terminal differentiation. Dev Dyn. 2004;231:758–65. doi: 10.1002/dvdy.20182. [DOI] [PubMed] [Google Scholar]
- [46].Ryan MC, Lee K, Miyashita Y, Carter WG. Targeted disruption of the LAMA3 gene in mice reveals abnormalities in survival and late stage differentiation of epithelial cells. J Cell Biol. 1999;145:1309–23. doi: 10.1083/jcb.145.6.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hormia M, Sahlberg C, Thesleff I, Airenne T. The epithelium-tooth interface--a basal lamina rich in laminin-5 and lacking other known laminin isoforms. J Dent Res. 1998;77:1479–85. doi: 10.1177/00220345980770070201. [DOI] [PubMed] [Google Scholar]
- [48].Stupp SI, LeBonheur VV, Walker K, Li LS, Huggins KE, Keser M, et al. Supramolecular Materials: Self-Organized Nanostructures. Science. 1997;276:384–9. doi: 10.1126/science.276.5311.384. [DOI] [PubMed] [Google Scholar]
- [49].Hartgerink JD, Beniash E, Stupp SI. Peptide-amphiphile nanofibers: a versatile scaffold for the preparation of self-assembling materials. Proc Natl Acad Sci U S A. 2002;99:5133–8. doi: 10.1073/pnas.072699999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Cui H, Webber MJ, Stupp SI. Self-assembly of peptide amphiphiles: from molecules to nanostructures to biomaterials. Biopolymers. 2010;94:1–18. doi: 10.1002/bip.21328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Rajangam K, Behanna HA, Hui MJ, Han X, Hulvat JF, Lomasney JW, et al. Heparin binding nanostructures to promote growth of blood vessels. Nano Lett. 2006;6:2086–90. doi: 10.1021/nl0613555. [DOI] [PubMed] [Google Scholar]
- [52].Silva GA, Czeisler C, Niece KL, Beniash E, Harrington DA, Kessler JA, et al. Selective differentiation of neural progenitor cells by high-epitope density nanofibers. Science. 2004;303:1352–5. doi: 10.1126/science.1093783. [DOI] [PubMed] [Google Scholar]
- [53].Storrie H, Guler MO, Abu-Amara SN, Volberg T, Rao M, Geiger B, et al. Supramolecular crafting of cell adhesion. Biomaterials. 2007;28:4608–18. doi: 10.1016/j.biomaterials.2007.06.026. [DOI] [PubMed] [Google Scholar]
- [54].Webber MJ, Tongers J, Renault MA, Roncalli JG, Losordo DW, Stupp SI. Development of bioactive peptide amphiphiles for therapeutic cell delivery. Acta Biomater. 2010;6:3–11. doi: 10.1016/j.actbio.2009.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Ghanaati S, Webber MJ, Unger RE, Orth C, Hulvat JF, Kiehna SE, et al. Dynamic in vivo biocompatibility of angiogenic peptide amphiphile nanofibers. Biomaterials. 2009;30:6202–12. doi: 10.1016/j.biomaterials.2009.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Hartgerink JD, Beniash E, Stupp SI. Self-assembly and mineralization of peptide-amphiphile nanofibers. Science. 2001;294:1684–8. doi: 10.1126/science.1063187. [DOI] [PubMed] [Google Scholar]
- [57].Spoerke ED, Anthony SG, Stupp SI. Enzyme Directed Templating of Artificial Bone Mineral. Advanced Materials. 2009;21:425–30. doi: 10.1002/adma.200802242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Palmer LC, Newcomb CJ, Kaltz SR, Spoerke ED, Stupp SI. Biomimetic systems for hydroxyapatite mineralization inspired by bone and enamel. Chem Rev. 2008;108:4754–83. doi: 10.1021/cr8004422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Mata A, Geng Y, Henrikson KJ, Aparicio C, Stock SR, Satcher RL, et al. Bone regeneration mediated by biomimetic mineralization of a nanofiber matrix. Biomaterials. 2010;31:6004–12. doi: 10.1016/j.biomaterials.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Rajangam K, Arnold MS, Rocco MA, Stupp SI. Peptide amphiphile nanostructure-heparin interactions and their relationship to bioactivity. Biomaterials. 2008;29:3298–305. doi: 10.1016/j.biomaterials.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Guler MO, Hsu L, Soukasene S, Harrington DA, Hulvat JF, Stupp SI. Presentation of RGDS epitopes on self-assembled nanofibers of branched peptide amphiphiles. Biomacromolecules. 2006;7:1855–63. doi: 10.1021/bm060161g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Guler MO, Soukasene S, Hulvat JF, Stupp SI. Presentation and recognition of biotin on nanofibers formed by branched peptide amphiphiles. Nano Lett. 2005;5:249–52. doi: 10.1021/nl048238z. [DOI] [PubMed] [Google Scholar]
- [63].Huang Z, Sargeant TD, Hulvat JF, Mata A, Bringas P, Jr., Koh CY, et al. Bioactive nanofibers instruct cells to proliferate and differentiate during enamel regeneration. J Bone Miner Res. 2008;23:1995–2006. doi: 10.1359/JBMR.080705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Kallenbach E. Electron microscopy of the differentiating rat incisor ameloblast. J Ultrastruct Res. 1971;35:508–31. doi: 10.1016/s0022-5320(71)80008-4. [DOI] [PubMed] [Google Scholar]
- [65].Giannuzzi LA, Stevie FA. A review of focused ion beam milling techniques for TEM specimen preparation. Micron. 1999;30:197–204. [Google Scholar]
- [66].Jantou V, Turmaine M, West GD, Horton MA, McComb DW. Focused ion beam milling and ultramicrotomy of mineralised ivory dentine for analytical transmission electron microscopy. Micron. 2009;40:495–501. doi: 10.1016/j.micron.2008.12.002. [DOI] [PubMed] [Google Scholar]
- [67].Nalla RK, Porter AE, Daraio C, Minor AM, Radmilovic V, Stach EA, et al. Ultrastructural examination of dentin using focused ion-beam cross-sectioning and transmission electron microscopy. Micron. 2005;36:672–80. doi: 10.1016/j.micron.2005.05.011. [DOI] [PubMed] [Google Scholar]
- [68].Jodaikin A, Weiner S, Traub W. Enamel rod relations in the developing rat incisor. J Ultrastruct Res. 1984;89:324–32. doi: 10.1016/s0022-5320(84)80048-9. [DOI] [PubMed] [Google Scholar]
- [69].Paine ML, Snead ML. Protein interactions during assembly of the enamel organic extracellular matrix. J Bone Miner Res. 1997;12:221–7. doi: 10.1359/jbmr.1997.12.2.221. [DOI] [PubMed] [Google Scholar]
- [70].Amar S, Luo W, Snead ML, Ruch JV. Amelogenin gene expression in mouse incisor heterotopic recombinations. Differentiation. 1989;41:56–61. doi: 10.1111/j.1432-0436.1989.tb00732.x. [DOI] [PubMed] [Google Scholar]
- [71].Couwenhoven RI, Snead ML. Early determination and permissive expression of amelogenin transcription during mouse mandibular first molar development. Dev Biol. 1994;164:290–9. doi: 10.1006/dbio.1994.1199. [DOI] [PubMed] [Google Scholar]
- [72].Xu Y, Zhou YL, Luo W, Zhu QS, Levy D, MacDougald OA, et al. NF-Y and CCAAT/enhancer-binding protein alpha synergistically activate the mouse amelogenin gene. J Biol Chem. 2006;281:16090–8. doi: 10.1074/jbc.M510514200. [DOI] [PubMed] [Google Scholar]
- [73].Tummers M, Thesleff I. The importance of signal pathway modulation in all aspects of tooth development. J Exp Zool B Mol Dev Evol. 2009;312B:309–19. doi: 10.1002/jez.b.21280. [DOI] [PubMed] [Google Scholar]
- [74].Hu B, Unda F, Bopp-Kuchler S, Jimenez L, Wang XJ, Haikel Y, et al. Bone marrow cells can give rise to ameloblast-like cells. J Dent Res. 2006;85:416–21. doi: 10.1177/154405910608500504. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.