Abstract
Objectives: The aim of this study was to evaluate the effectiveness of two types of lasers, the Nd:YAG laser and the 685-nm diode laser, as dentin desensitizers as well as both the immediate and late therapeutic effects on teeth with gingival recession. Materials and Methods: The study was conducted on 56 teeth in 14 patients with Miller's class 1 and 2 gingival recession with clinically elicitable dentin hypersensitivity (DH). The patients were divided into two groups: a Nd:YAG-laser-treated group and a 685-nm diode laser-treated group. DH was assessed by means of an air stimulus, and a visual analog scale (VAS) was used to measure DH. The selected teeth in the two groups received laser therapy for three sessions. Teeth subjected to Nd:YAG-laser treatment were irradiated at 1 W and 10 Hz for 60 sec at 1064 nm, and those receiving 685-nm diode laser treatment were irradiated at 25 mW and 9 Hz for 100 sec. Results: Significant reductions in DH occurred at all time points measured during the three treatment sessions in both treatment groups. Comparing the means of the responses in the three treatment sessions for the two groups revealed that the Nd:YAG laser group had a higher degree of desensitization compared to the other group (p < 0.01). The immediate and late therapeutic effects of the Nd:YAG laser were more evident than those of the 685-nm diode laser. Conclusions: Both of these lasers can be used to reduce DH without adverse effects. Desensitization of teeth with gingival recession with the Nd:YAG laser was more effective than with the diode laser. The Nd:YAG laser appears to be a promising new tool for successfully reducing DH.
Introduction
Dentin hypersensitivity (DH) is one of the most painful and poorly treated chronic problems in clinical dentistry. This problem is characterized by short, sharp, severe pain arising from exposed dentin in response to thermal, evaporative, tactile, osmotic, or chemical stimuli, and ceases after removal of the inciting factor.1–6 The prevalance of this disorder has been reported in different studies to vary from 4–73%.1,4,5 DH may affect patients of any age, and it affects women more often than men.1 The condition may affect any tooth, but it most often affects canines and premolars.7 DH occurs when dentin is exposed and dentinal tubules are opened. The exposure of dentin and its sensitivity may occur via one or both of two processes: removal of enamel, or denudation of the root surface due to loss of the overlying cementum and periodontal tissues. To date, little is known about the precise etiology of DH and its effective treatment. DH is becoming a widespread problem and increasing numbers are reported of teeth with gingival recession due to poor toothbrushing habits, abrasion due to overbrushing, erosion from dietary factors, teeth abnormally positioned in the arch, chronic periodontal disease, periodontal surgery, root planing, occlusal wear, and aging.1,2 This condition makes activities of daily living such as eating, drinking, brushing, and even breathing, more difficult for those afflicted.
Various agents have been recommended to reduce DH, including sodium fluoride, potassium ion, oxalates, resin bonding agents, and abrasive dentifrices.1,2 However, most treatments are either ineffective or are effective only for short periods.
The use of dental lasers has been cited as a possible new treatment option for DH, and has become a subject of intensive research in recent decades. The use of lasers for the treatment of sensitive teeth may be divided into two groups: lasers with moderate power outputs, one of which is the Nd:YAG laser, and low-level lasers, one of which is the 685-nm diode laser. Both the Nd:YAG laser8–14 and the 685-nm diode laser15–17 have been tested for the treatment of DH by many investigators. Many of them, in spite of the wide variety of methods and types of lasers used, have proven to be successful.
The mechanism by which the Nd:YAG laser affects DH is thought to be laser-induced occlusion or narrowing of dentinal tubules as a form of nerve analgesia. Dentin may be fused by brief exposure to the Nd:YAG laser, and the fused dentin solidifies into a glazed, non-porous surface.8 After the application of Nd:YAG laser energy, the morphological dentin changes seen are characterized by a melted and re-solidified surface, and by the presence of craters, cracks, and globules.18–21
Previous results of treatment of DH with the diode laser have revealed that the laser's interaction with the dental pulp induces a photobiomodulating effect that increases cellular metabolic activity of odontoblasts, obliterates the dentinal tubules, and intensifies tertiary dentin production.15,17
Because of the great variety of methods and types of lasers used, it is impossible to propose a definitive means of laser treatment of DH. Although lasers have often been suggested for this indication, prior to this study there have been no published data available comparing the clinical effectiveness of the Nd:YAG and the 685-nm diode laser for the treatment of DH. The purpose of this study was to evaluate and compare the two types of lasers as dentin desensitizers, and to assess both the immediate and late therapeutic effects on teeth with gingival recession.
Materials and Methods
The research protocol was initially submitted to the Ethics Committee and the Institutional Internal Review and Ethics Board at the Gülhane Military Medical Academy (GMMA), Sciences of Dentistry, and Attatürk University, Faculty of Dentistry and they approved the study. The study population consisted of 14 patients with 56 hypersensitive teeth with Miller's class 1 and class 2 gingival recession (8 women and 6 men; age 19–51 y, mean age 34.2 ± 9.3 y) who visited the periodontology clinics of GMMA in Ankara, and Attatürk University in Erzurum, Turkey (Table 1).
Table 1.
Age, Gender, Gingival Recession Type, and Tooth Type, in Patient Population
| Variable | n | Nd:YAG-treated group n | 685-nm diode-treated group n |
|---|---|---|---|
| Age (years) | |||
| 19–25 | 4 | 2 | 2 |
| 26–35 | 5 | 2 | 3 |
| 36–51 | 5 | 3 | 2 |
| Gender | |||
| Female | 8 | 4 | 4 |
| Male | 6 | 3 | 3 |
| Gingival recession type | |||
| Miller Class I | 28 | 14 | 14 |
| Miller Class II | 28 | 14 | 14 |
| Tooth type | |||
| Anterior | 23 | 11 | 12 |
| Premolar | 17 | 9 | 8 |
| Molar | 16 | 8 | 8 |
Written informed consent was obtained from each study subject after all procedures had been fully explained.
Selection of subjects and test teeth
Inclusion criteria
The criteria used in selecting patients were: they were all in good overall health, they had clinically elicitable DH, and they were able to understand verbal and written instructions. All experimental teeth had Miller's class 1 or class 2 gingival recession.22
Exclusion criteria
Exclusion criteria included: those with chronic or debilitating diseases and daily pain episodes; those who were on any analgesic, anticonvulsive, antihistaminic, sedative, tranquilizing, or anti-inflammatory medications in the 72 h preceding treatment; those who had used any desensitizing paste or mouthwash in the last 3 mo; and those who had periodontal surgery in the last 6 months. Teeth with cracks, carious lesions, and restorations, and those with active periodontal disease were also excluded.
Pain and DH assessment
A visual analog scale (VAS) was used to measure DH. The VAS was administered in a standard manner, with the initial explanation was given by the same clinician to all participants. All patients were asked to define their level of DH on a VAS with a scale from 0 to 10 (a 10-cm line). On this scale, 0 and 10 represented “no pain/discomfort” and “the worst pain/discomfort imaginable,” respectively. All pain assessments were performed in the morning in the same clinic, in an area free of noise, music, or conversation. The patients were asked to rate their pain when a jet of air was directed to the root surface both before and after treatment. After and before each session, we gave each patient a new copy of the scale so they would not be influenced by the previous results. The reproducibility of the VAS was tested on two separate occasions by five patients, and there was a strong correlation between the two sets of responses (Spearman's rho >0.93, p < 0.001).
First the patient rated their pain before air jet application. Then the jet of air (60 psi at 22°C) was delivered by a dental syringe for 1 sec, with the syringe held perpendicularly 2 to 3 mm from the root surface. After stimulation, the patient again scored their pain on the VAS. The air pressure, temperature, and distance between the tooth surface and the tip of the air syringe was kept constant for all cases. All stimuli were applied by a single investigator in the same dental chair with the same equipment.
Treatment
After the baseline pain assessment, the teeth were randomly assigned to group 1 (Nd:YAG-laser treatment) or group 2 (685-nm diode-laser treatment).
Prior to laser therapy, all of the teeth received scaling, root planing, and polishing. The region being treated was isolated with the aid of a cotton roll, and the buccal surface was dried with gauze before each treatment session. The vitality of the teeth was tested with a pulp tester after each treatment session. The patients were blinded as to what type of laser therapy each tooth was receiving.
The Nd:YAG laser used in this study was a Smarty A10 laser (DEKA, Italy) in Attatürk University. The 685-nm diode laser used was a BTL-2000 laser (Dravotnicka Techika, Prague, Czech Republic in GMMA). Teeth subjected to Nd:YAG laser treatment were irradiated (1064 nm) with 1 W at 10 Hz for 60 sec, with a sweeping motion and no cooling. The distance between the end of the optical fiber and tooth surface was maintained at 2 mm. Teeth subjected to the 685-nm diode laser treatment were irradiated (685 nm) with 25 mW at 9 Hz for 100 sec (2 J/cm2) in continuous mode, with application to the buccal surface and the region of exposed dentinal neck. While the lasers were in use, protective eyewear was worn by both the investigator and the patient.
All the patients used a standardized toothbrush and toothpaste with no anti-hypersensitivity agent (including fluoride) during the 3-month trial period. All participants completed the study and reported 100% compliance.
The laser therapy was performed by a single investigator and the pain assessments were carried out by another investigator.
Study Design
The treatments were carried out in three sessions, with 14 d between sessions, for a period of 30 consecutive days. The measurements were performed before each treatment session and 30 min after laser application to verify the capacity, extent, and the duration of desensitization after irradiation. This result was called the immediate effect. Additional measurements were also performed at 15, 30, and 60 d after the conclusion of treatment to assess the extent of desensitization obtained with the two types of lasers. This result was called the late effect.
Statistical analysis
The data thus collected were assessed using SPSS 11.0 statistical software (SPSS, Inc., Chicago, IL, USA). The Mann-Whitney U test was used to compare groups 1 and 2, and the differences in the mean VAS scores were calculated.
The differences in mean VAS scores between pretreatment and 30 min post-treatment were evaluated using Wilcoxon's signed ranks test. The Friedman test was used to assess the differences in mean VAS values for the late effects of treatment (at 15, 30, and 60 d). Associations between age, gender, gingival recession type, tooth type, and VAS scores for all sessions were determined with Spearman's rank correlation coefficient.
Results
The mean VAS values before and after treatment of DH with the Nd:YAG laser and the 685-nm diode laser at different time points are shown in table (Table 2).
Table 2.
Comparison of the Mean VAS Scores in the Two Groups at Different Time Points
| Nd:YAG-laser-treated group | Diode-laser-treated group | p Value | |
|---|---|---|---|
| Immediate effect | |||
| Session 1 | |||
| Pretreatment | 7.76 ± 0.75 | 7.71 ± 0.55 | >0.05 |
| 30 min | 5.00 ± 0.62a | 7.14 ± 0.89 | <0.001 |
| Session 2 | |||
| Pretreatment | 4.86 ± 0.77 | 6.90 ± 0.87 | <0.001 |
| 30 min | 4.00 ± 0.76b | 5.90 ± 1.48a | <0.001 |
| Session 3 | |||
| Pretreatment | 3.90 ± 0.75 | 4.76 ± 1.31 | <0.05 |
| 30 min | 1.24 ± 0.75a | 3.95 ± 1.31b | <0.001 |
| Late effect | |||
| 15 days | 1.14 ± 0.64 | 3.52 ± 1.01 | <0.001 |
| 30 days | 1.14 ± 0.64 | 3.43 ± 1.00 | <0.001 |
| 60 days | 1.05 ± 0.65 | 3.00 ± 0.69 | <0.001 |
Significant differences between pretreatment and 30 min: ap < 0.05; bp < 0.01.
The mean VAS score at pretreatment before session 1 for the Nd:YAG-treated group was 7.76 ± 0.75. The corresponding value for the 685-nm diode-treated group was 7.71 ± 0.55. These values were not statistically significantly different (p >0.05). A significant decrease in mean VAS score 30 min after session 1 was seen in the Nd:YAG-treated group (5.00 ± 0.62; p < 0.01), whereas the same value at 30 min after session 1 for the 685-nm diode-treated group was 7.14 ± 0.89, which was not statistically significantly different (p > 0.05).
The mean VAS score pretreatment before session 2 for the Nd:YAG-treated group was 4.86 ± 0.77, and at 30 min post-treatment the mean VAS score was 4.00 ± 0.76 (p < 0.01). The corresponding values at pre- and post-treatment for session 3 were 3.90 ± 0.75 and 1.24 ± 0.75, respectively (p < 0.05). In the 685-nm diode-treated group, the corresponding values were 6.90 ± 0.87 and 5.90 ± 1.48, respectively, for session 2 (p < 0.05), and 4.76 ± 1.31 and 3.95 ± 1.31, respectively, for session 3 (p < 0.01).
Table 2 also shows the mean VAS scores for the late effects seen at the follow-up time points of 15, 30, and 60 d after the conclusion of treatment with the Nd:YAG laser and the 685-nm diode laser groups.
On the day 15, the Nd:YAG-treated group has a mean VAS score of 1.14, compared to that of the 685-nm diode-treated group, which was 3.52, which was statistically significantly different (p < 0.01). Both groups also showed significant decreases in mean VAS scores at day 60 post-treatment (p < 0.05 for the Nd:YAG-treated group, and p < 0.01 for the 685-nm diode-treated group).
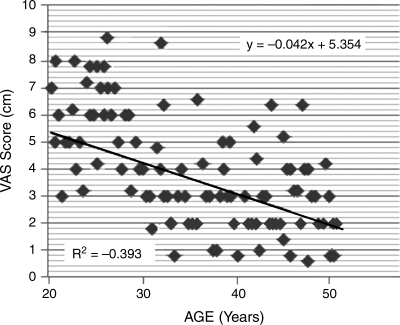
Spearman's rank correlation coefficients were calculated for age, gender, gingival recession type, tooth type, and VAS scores. No correlations were found between gender, gingival recession type, tooth type, or VAS scores. However, a significant negative correlation between age and VAS scores was observed. The VAS scores decreased with increasing age for both laser-treated groups (Spearman rho –0.592; p < 0.013) (y = −0.042 × +5.354; R2 = −0.393) (Fig. 1).
FIG. 1.
Association between age and visual analog scale (VAS) scores. Black line = Spearman rho.
Discussion
The problem of DH is an enigma that has interested many clinicians. It can be a major problem for periodontal patients who frequently have gingival recession and exposed root surfaces. The present study provides information about the clinical effectiveness of the Nd:YAG and 685-nm diode lasers in the treatment of DH.
DH is a painful condition that is difficult to quantify. In the present study, a visual analog scale (VAS) was used to assess DH. In previous clinical studies, several investigators have also used the VAS, because it is easily understood by patients, it is sensitive in discriminating among the effects of various types of treatments, and it thus is suitable for evaluating the pain response seen in studies of DH.8,9,15
The results of the present clinical trial demonstrate that both the Nd:YAG and 685-nm diode lasers were effective in desensitizing hypersensitive teeth. The results particularly illustrate their effectiveness following cold air jet stimulation. The laser-induced reductions in discomfort were still seen at 60 d post-treatment.
The laser parameters affecting the amount of energy applied to a given surface include power level (W), exposure time (seconds), pulsed versus continuous wave energy, energy density (J/cm2), distance from the surface, and the angle between the target tissue and the fiber tip. As a laser beam strikes a target tissue surface, the light energy can be affected in four ways: it can be reflected, transmitted, absorbed, or scattered, and the changes seen in target tissues are largely due to the absorbed energy.2 Therefore, the most important issue in laser therapy is to determine the correct parameters to use to achieve optimal results, without inducing detrimental thermal effects in the pulp, or causing fracturing or carbonization.
In the Nd:YAG laser-treated group, the mean VAS scores showed decreases from pretreatment to post-treatment at all time points assessed, and these changes were statistically significant. These findings are similar those obtained by Birang et al.,8 who also used a Nd:YAG laser and achieved similar reductions in DH pain; similar observations were made by several other sets of investigators.9–12 Kumar and Mehta9 saw a decrease of 44–62% in mean VAS scores in their Nd:YAG laser-treated group. Ciaramicoli et al.10 also saw reductions in hypersensitivity in their groups that received Nd:YAG laser treatment. However, there are differences between the results seen in the present study and those of other studies, that found no improvements after Nd:YAG laser treatment.13,14 Perhaps this was due to their use of water cooling during Nd:YAG laser therapy, which may have limited the photothermal effects induced in the dental tissues.
Several studies have been performed to analyze the mechanism of action of Nd:YAG laser irradiation in decreasing pain due to DH. According to these studies, when the laser power level is less than 1.5 W, the irradiation causes alterations such as melting of dentin and closure of exposed dentinal tubules, as well as cracking and fissuring of the root surface; but when the power level is more than 1.5 W, cracking and fissuring of the dentin and changes in the dentin's protein structure may occur, with resulting injury to the pulp.21,23,24
The results obtained here indicate that successful desensitization of teeth with gingival recession can be attained with the Nd:YAG laser. Also, the Nd:YAG laser was more effective than the 685-nm diode laser in inducing these effects. This is likely due to the dentinal fusion seen during Nd:YAG laser irradiation, and this is probably an effect of the occlusion or narrowing of dentinal tubules, thereby blocking fluid flow through the dentin. The 685-nm diode laser blocks depolarization of C-fiber afferents,25 and its effects are due to laser-induced changes in neural transmission within the pulp, rather than alterations in the exposed dentin surface, such as those seen with other types of treatment. Moreover, besides the immediate analgesic effects, 685-nm diode laser therapy may stimulate normal physiological cellular functions.16–17 In the 685-nm diode laser-treated group, the mean VAS scores showed decreases from pretreatment to post-treatment at all time points, and these were statistically significant changes. Our findings confirm the findings of earlier studies of this phenomenon.15–17
The vitality testing done before and after laser treatment had similar results, indicating that the laser therapy did not adversely affect the pulp.
One of the purposes of the present study was to evaluate to what extent patient pain responses were related to age, gender, gingival recession type, and tooth type. We found that there was no difference in patient pain responses with regard to gender for both groups. This finding disagrees with other reports, that indicated that females have greater dentin sensitivity and lower tolerance for pain than males.26 However, Strahan and Glenwright found no statistically significant differences in pain between genders after periodontal surgery.27 Similar results were also obtained in response to periodontal therapy.28,29 The reasons for the lack of any difference between genders seen in our study are unclear, but no significant differences existed for the Turkish patient population we studied.
The results demonstrated that VAS scores decreased with increasing age for both laser-treated groups. A general clinical impression is that elderly people are frequently more tolerant of pain than are the young. Age has been widely discussed as an important factor in how pain is experienced.28 In elderly subjects, their higher pain threshold may due to tissue changes such as reduced vascularity, fatty degeneration of bony tissue,30 and secondary dentin formation.31 Alterations in the morphology of the pulp-dentin complex also result from the physiological process of aging.15 Thus our findings are in accord with those of previous reports.
Laser treatment appears to be beneficial as an alternative treatment for DH. However, lasers are not yet in wide use due to their high cost. We are hopeful that the laser may soon find more widespread use in dental clinics as a means of relieving orofacial pain, treating periodontal disease, and repairing bone.
Conclusions
Both of the lasers tested here can be used to reduce DH with no adverse effects on tooth vitality. The desensitization of teeth with gingival recession seen with the Nd:YAG laser was more apparent than that of the diode laser, and thus we can confidently say that Nd:YAG laser irradiation is more effective than 685-nm diode laser irradiation for the treatment of DH. The Nd:YAG laser will become a useful tool for successfully reducing the pain of DH, and our 60-day results are particularly promising. Further studies are needed to evaluate the long-term effects of this type of therapy.
Acknowledgments
The investigation was supported by grant (PN-2005/243) from Atatürk University, Erzurum, Turkey. We would like to thank Dr. Erkan Oktay for statistical assistance.
Disclosure Statement
No conflicting financial interests exist.
References
- 1.Orchardson R. Gillam D.G. Managing dentin hypersensitivity. J. Am. Dent. Assoc. 2006;137:990–998. doi: 10.14219/jada.archive.2006.0321. [DOI] [PubMed] [Google Scholar]
- 2.Kimura Y. Wilder-Smith P. Yonaga K. Matsumoto K. Treatment of dentine hypersensitivity by lasers: a review. J. Clin. Periodontol. 2000;27:715–721. doi: 10.1034/j.1600-051x.2000.027010715.x. [DOI] [PubMed] [Google Scholar]
- 3.Addy M. Etiology and clinical implications of dentine hypersensitivity. Dent. Clin. North Am. 1990;34:503–514. [PubMed] [Google Scholar]
- 4.Rees J.S. Addy M. A cross-sectional study of dentine hypersensitivity. J. Clin. Periodontol. 2002;29:997–1003. doi: 10.1034/j.1600-051x.2002.291104.x. [DOI] [PubMed] [Google Scholar]
- 5.Canakci C.F. Canakci V. Pain experienced by patients undergoing different periodontal therapies. J. Am. Dent. Assoc. 2007;138:1563–1573. doi: 10.14219/jada.archive.2007.0105. [DOI] [PubMed] [Google Scholar]
- 6.Canakci V. Canakci C.F. Pain levels in patients during periodontal probing and mechanical non-surgical therapy. Clin. Oral Invest. 2007;11:377–383. doi: 10.1007/s00784-007-0126-z. [DOI] [PubMed] [Google Scholar]
- 7.Addy M. Mostafa P. Newcombe R.G. Dentine hypersensitivity: the distribution of recession, sensitivity and plaque. J. Dent. 1987;15:242–248. doi: 10.1016/0300-5712(87)90045-5. [DOI] [PubMed] [Google Scholar]
- 8.Birang R. Poursamimi J. Gutknecht N. Lampert F. Mir M. Comparative evaluation of the effects of Nd:YAG and Er:YAG laser in dentin hypersensitivity treatment. Lasers Med. Sci. 2007;22:21–24. doi: 10.1007/s10103-006-0412-z. [DOI] [PubMed] [Google Scholar]
- 9.Kumar N.G. Mehta D.S. Short-term assessment of the Nd:YAG laser with and without sodium fluoride varnish in the treatment of dentin hypersensitivity—a clinical and scanning electron microscopy study. J. Periodontol. 2005;76:1140–1147. doi: 10.1902/jop.2005.76.7.1140. [DOI] [PubMed] [Google Scholar]
- 10.Ciaramicoli M.T. Carvalho R.C. Eduardo C.P. Treatment of cervical dentin hypersensitivity using neodymium:yttrium-aluminum-garnet laser. Clinical evaluation. Lasers Surg. Med. 2003;33:358–362. doi: 10.1002/lsm.10232. [DOI] [PubMed] [Google Scholar]
- 11.Renton-Harper P. Midda M. NdYAG laser treatment of dentinal hypersensitivity. Br. Dent. J. 1992;172:13–16. doi: 10.1038/sj.bdj.4807731. [DOI] [PubMed] [Google Scholar]
- 12.Lan W.H. Liu H.C. Treatment of dentin hypersensitivity by Nd:YAG laser. J. Clin. Laser Med. Surg. 1996;14:89–92. doi: 10.1089/clm.1996.14.89. [DOI] [PubMed] [Google Scholar]
- 13.Lier B.B. Rosing C.K. Aass A.M. Gjermo P. Treatment of dentin hypersensitivity by Nd:YAG laser. J. Clin. Periodontol. 2002;29:501–506. doi: 10.1034/j.1600-051x.2002.290605.x. [DOI] [PubMed] [Google Scholar]
- 14.Gutknecht N. Moritz A. Dercks H.W. Lampert F. Treatment of hypersensitive teeth using neodymium:yttrium-aluminum-garnet lasers: a comparison of the use of various settings in an in vivo study. J. Clin. Laser Med. Surg. 1997;15:171–174. doi: 10.1089/clm.1997.15.171. [DOI] [PubMed] [Google Scholar]
- 15.Ladalardo T.C. Pinheiro A. Campos R.A., et al. Laser therapy in the treatment of dentine hypersensitivity. Braz. Dent. J. 2004;15:144–150. doi: 10.1590/s0103-64402004000200011. [DOI] [PubMed] [Google Scholar]
- 16.Corona S.A. Nascimento T.N. Catirse A.B. Lizarelli R.F. Dinelli W. Palma-Dibb R.G. Clinical evaluation of low-level laser therapy and fluoride varnish for treating cervical dentinal hypersensitivity. J. Oral Rehabil. 2003;30:1183–1189. doi: 10.1111/j.1365-2842.2003.01185.x. [DOI] [PubMed] [Google Scholar]
- 17.Gerschman J.A. Ruben J. Gebart-Eaglemont J. Low level laser therapy for dentinal tooth hypersensitivity. Aust. Dent. J. 1994;39:353–357. doi: 10.1111/j.1834-7819.1994.tb03105.x. [DOI] [PubMed] [Google Scholar]
- 18.Zapletalova Z. Perina J., Jr. Novotny R. Chmelickova H. Suitable conditions for sealing of open dentinal tubules using a pulsed Nd:YAG laser. Photomed. Laser Surg. 2007;25:495–499. doi: 10.1089/pho.2007.2085. [DOI] [PubMed] [Google Scholar]
- 19.Naylor F. Aranha A.C. Eduardo Cde. P. Arana-Chavez V.E. Sobral M.A. Micromorphological analysis of dentinal structure after irradiation with Nd:YAG laser and immersion in acidic beverages. Photomed. Laser Surg. 2006;24:745–752. doi: 10.1089/pho.2006.24.745. [DOI] [PubMed] [Google Scholar]
- 20.Aranha A.C. Domingues F.B. Franco V.O. Gutknecht N. Eduardo Cde. P. Effects of Er:YAG and Nd:YAG lasers on dentin permeability in root surfaces: a preliminary in vitro study. Photomed. Laser Surg. 2005;23:504–508. doi: 10.1089/pho.2005.23.504. [DOI] [PubMed] [Google Scholar]
- 21.Lan W.H. Liu H.C. Lin C.P. The combined occluding effect of sodium fluoride varnish and Nd:YAG laser irradiation on human dentinal tubules. J. Endod. 1999;25:424–426. doi: 10.1016/S0099-2399(99)80271-4. [DOI] [PubMed] [Google Scholar]
- 22.Miller P.D., Jr. A classification of marginal tissue recession. Int. J. Periodontics Restorative Dent. 1985;5:8–13. [PubMed] [Google Scholar]
- 23.Lan W.H. Lee B.S. Liu H.C. Lin C.P. Morphologic study of Nd:YAG laser usage in treatment of dentinal hypersensitivity. J. Endod. 2004;30:131–134. doi: 10.1097/00004770-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Yonaga K. Kimura Y. Matsumoto K. Treatment of cervical dentin hypersensitivity by various methods using pulsed Nd:YAG laser. J. Clin. Laser Med. Surg. 1999;17:205–210. doi: 10.1089/clm.1999.17.205. [DOI] [PubMed] [Google Scholar]
- 25.Wakabayashi H. Hamba M. Matsumoto K. Tachibana H. Effect of irradiation by semiconductor laser on responses evoked in trigeminal caudal neurons by tooth pulp stimulation. Lasers Surg. Med. 1993;13:605–610. doi: 10.1002/lsm.1900130603. [DOI] [PubMed] [Google Scholar]
- 26.McGrath P.A. Psychological aspects of pain perception. Arch. Oral Biol. 1994;39:55s–62s. doi: 10.1016/0003-9969(94)90189-9. [DOI] [PubMed] [Google Scholar]
- 27.Strahan J.D. Glenwright H.D. Pain experience in periodontal surgery. J. Periodontal Res. 1967;1:163–166. doi: 10.1111/j.1600-0765.1967.tb01884.x. [DOI] [PubMed] [Google Scholar]
- 28.Fardal O. Johannessen A.C. Linden G.J. Patient perceptions of periodontal therapy completed in a periodontal practice. J. Periodontol. 2002;73:1060–1066. doi: 10.1902/jop.2002.73.9.1060. [DOI] [PubMed] [Google Scholar]
- 29.Karadottir H. Lenoir L. Barbierato B., et al. Pain experienced by patients during periodontal maintenance treatment. J. Periodontol. 2002;73:536–542. doi: 10.1902/jop.2002.73.5.536. [DOI] [PubMed] [Google Scholar]
- 30.Masaro R. Physiology of aging, in: Geriatric Dentistry. In: Pedersen P.H., editor; Löe H., editor. A Textbook of Oral Gerontology. Copenhagen; Munksgaard: 1986. pp. 34–69. [Google Scholar]
- 31.Mjor I. Age changes in the teeth, in: Geriatric Dentistry. In: Pedersen P.H., editor; Löe H., editor. A Textbook of Oral Gerontology. Copenhagen; Munksgaard: 1986. pp. 94–101. [Google Scholar]