Abstract
Objective
To report contemporary estimates of the prevalence of hip-related osteoarthritis (OA) outcomes in African-Americans and Caucasians aged ≥ 45 years.
Methods
Weighted prevalence estimates and their corresponding 95% confidence intervals for hip symptoms, radiographic hip OA, symptomatic hip OA, and severe radiographic hip OA were calculated using SUDAAN® for age, race, and sex subgroups among 3,068 participants (33% African-Americans, 38% men) in the baseline examination (1991–1997) of The Johnston County Osteoarthritis Project, a population-based study of OA in North Carolina. Radiographic hip OA was defined as Kellgren-Lawrence radiographic grade ≥ 2, moderate/severe radiographic hip OA as grades 3 and 4, and symptomatic hip OA as hip symptoms in a hip with radiographic OA.
Results
Hip symptoms were present in 36%; 28% had radiographic hip OA; nearly 10% had symptomatic hip OA; and 2.5% had moderate/severe radiographic hip OA. Prevalence of all 4 outcomes was higher in older individuals; most outcomes were higher for women and African-Americans.
Conclusion
These hip-related outcomes were common in this population, and African-Americans did not have a lower prevalence as previous studies have suggested. Increasing public and health system awareness of the relatively high prevalence of these outcomes, which can be disabling, may help to decrease their impact and ultimately prevent them.
Keywords: osteoarthritis, hip pain, racial disparities
INTRODUCTION
Arthritis and other rheumatic conditions are a large, growing, and newly recognized public health problem in the United States (1). Arthritis affected 46 million adults in 2003–2005 (2), was the most common cause of disability in 1999 in the United States (3), severely affected health related quality of life (4), and has been associated with significant costs (5–7). Direct and indirect costs attributable to arthritis and other rheumatic conditions in 2003 totaled an estimated $128 billion, accounting for ~1% of gross domestic product (6–7). These burdens and impacts are likely to increase as the population ages over the coming decades.
Few epidemiological data are available for specific types of arthritis, making it difficult to identify high risk groups and target interventions. Osteoarthritis (OA) is the most common specific condition, affecting 27 million people in the United States in 2005 (8). Knee and hip OA are generally considered to have the greatest impact due to effects on ambulation; OA of these joints accounted for most of the 478,000 total knee replacements and 234,000 total hip replacements for arthritis in 2004 (9).
Despite this impact, the prevalence of hip OA overall and among demographic subgroups is not well characterized (10), with the only population-based estimate in the United States available from the 1971–1974 NHANES-I survey (11). A few small cross-studies comparisons have suggested a much lower prevalence of hip OA among African black populations than Caucasians (12–13), but no large recent studies have been performed to compare possible racial differences directly. Further, definitions of hip OA and the most appropriate means to measure it in epidemiologic studies are in flux. While early studies used radiographic measures only, such as the Kellgren and Lawrence scale (K-L) (14), as the field’s standard of measurement for OA (15), some persons with radiographic OA may have no symptoms, and some of those with even severe symptoms may have normal radiographs. Given that symptoms drive care-seeking and the need for interventions, definitions of clinical or symptomatic OA may be most relevant for clinical and public heath practice (15).
Accurate prevalence estimates of OA are critical for understanding the spectrum of disease, identifying high risk groups, and guiding intervention efforts efficiently to limit the progression of disease (16–18). We recently analyzed data from the Johnston County Osteoarthritis Project to update and expand older and more narrowly focused prevalence estimates for knee OA (19). The purpose of the current study is to improve characterization of hip OA in a similar fashion by reporting prevalence estimates from this same study for 4 hip OA-related measures in African-American and Caucasian men and women—joint symptoms, radiographic OA, symptomatic OA, and moderate/severe radiographic OA—for the population overall and by age, sex, and race.
MATERIALS AND METHODS
At the time this study was designed in 1990, Johnston County, North Carolina, had a population of about 81,000 and a rural area of about 800 square miles. It had and continues to have a high prevalence of socio-demographic subgroups at high risk for poor health outcomes. Specifically, a majority of residents (66%) lived in completely rural areas, with the remainder in small towns (20). African-American residents and persons 60 years of age or older constituted 20% and 17% of the population, respectively. Households with limited education and lower income were also common, with 35% of individuals over 25 years of age having less than a high school diploma and approximately 30% of jobs in the county in manufacturing, service, or farming (20–21).
The sampling and methods of the Johnston County Osteoarthritis Project have been described previously (19). In brief, it is a population-based prospective longitudinal cohort study of knee and hip OA designed to be representative of the civilian, non-institutionalized, African-American or Caucasian population, aged 45 years and older, who were residents of 1 of 6 townships in Johnston County for at least 1 year, and who were physically and mentally capable of completing the study’s protocol. The protocol involved an initial home interview, 1 visit to a local clinic, and a subsequent second home interview approximately 2 weeks after the clinic visit. The study was approved by the Institutional Review Boards of the University of North Carolina Schools of Medicine and Public Health and the Centers for Disease Control and Prevention. All participants gave written informed consent at the time of recruitment. The baseline evaluation that forms the basis for this report was conducted between 1991 and 1997.
Racial group was self-reported. Hip symptoms were assessed separately for right and left sides of the body by the following question: “On most days, do you have pain, aching, or stiffness in your (right, left) hip?” Hip symptoms were defined for analysis as an affirmative response to this question in at least 1 hip. All men, and women 50 years of age and older, had a supine anterior posterior pelvic film with feet in 15° rotation. Hip radiographs were read without knowledge of participant clinical status, by a single bone and joint radiologist (JBR) using the K-L radiographic atlas for overall hip radiographic grades (14). This scale defines radiographic OA in 5 categories: K-L grade 0 (normal) had no radiographic features of OA; K-L grade 1 (questionable) had a minute radiographic osteophyte of doubtful pathologic significance; K-L grade 2 (mild) had an osteophyte but no joint space narrowing; K-L grade 3 (moderate) had a moderate diminution of joint space; and K-L grade 4 (severe) had severe joint space narrowing with subchondral bone sclerosis (14). Inter-rater reliability assessed with another trained radiologist and intra-rater reliability for the radiologist were high (weighted kappa for inter-rater reliability was 0.86; kappa for intra-rater reliability was 0.89), as described previously (22). Radiographic hip OA was defined for analysis as K-L grade of at least 2 in at least 1 hip. Moderate/severe radiographic hip OA was defined as K-L grade 3 or 4 in at least 1 hip. Symptomatic hip OA was defined as the presence of hip symptoms in at least 1 hip with corresponding radiographic hip OA in that joint.
All analyses were performed with SAS® version 9.1 and SUDAAN® version 9.0 (23–24). SUDAAN is a software package designed for the analysis of complex survey data (24). Weighted prevalence estimates for the 4 hip outcomes and their corresponding 95% confidence intervals were derived for the total study population and for African-American and Caucasian men and women in 4 age categories: 45–54 years, 55–64 years, 65–74 years, and 75 years and older (25). Since women younger than 50 did not get hip radiographs (because of risk of pregnancy), the age range for the youngest category of women was 50–54 years for radiographic, symptomatic, and moderate/severe radiographic hip OA outcomes. Women younger than 50 years were included in the estimates of hip symptoms.
RESULTS
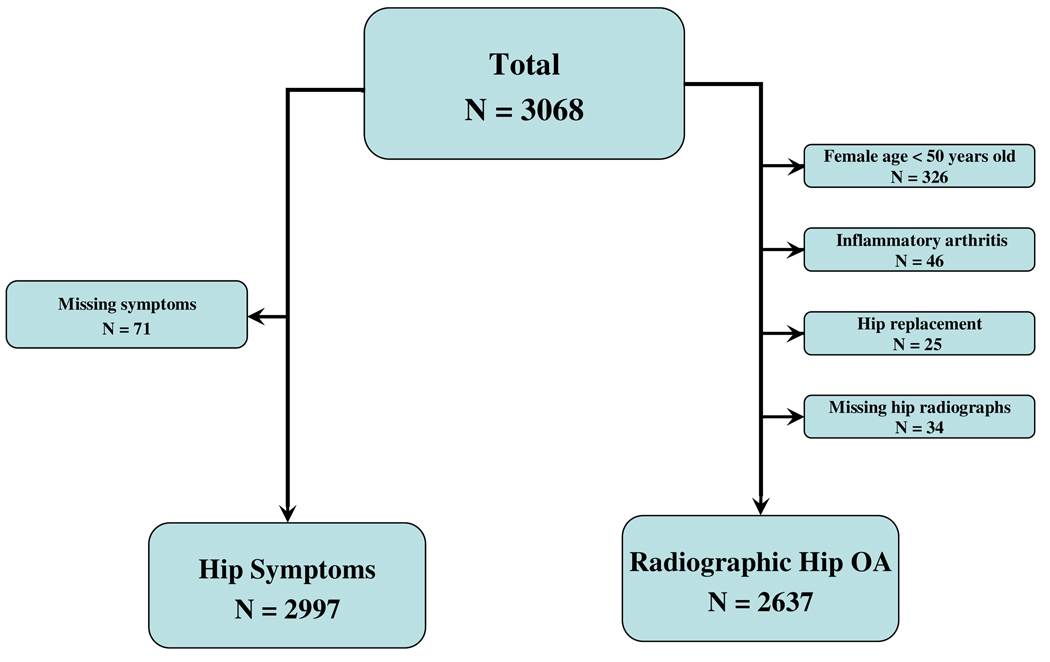
The target population of residents age 45 and older in the 6 townships of the Johnston County Osteoarthritis Project consisted of 57.4% women and 18.5% African-Americans (Table 1). A total of 3068 participants completed both the 1st home interview and clinic exam at baseline. For analysis of hip symptoms, we excluded 71 persons with missing data, leaving 2,997 for analysis (Figure 1); there were no significant differences by age, race, gender, or BMI between those with missing hip symptoms data or complete hip symptoms data. For analysis of the three radiographic hip outcomes, we excluded 326 women below the age of 50 years (10.6%) who by protocol did not have hip radiography performed, 46 participants (1.5%) with radiographic evidence of inflammatory arthritis in the knee (n = 17) and/or hip (n = 35), 25 participants who had total hip replacements, and 34 participants with missing hip radiographic data, leaving 2,637 for analysis (Figure 1). The 34 individuals with missing hip x-ray data were similar in age, gender, race, and BMI to those with complete hip x-ray data.
TABLE 1.
Unweighted and weighted distributions of baseline demographic and clinical variables of study participants, n = 3,068. Johnston County Osteoarthritis Project, 1991–199718
| Variable | Categories | Unweighted | Weighted | ||
|---|---|---|---|---|---|
| Count | % | %* | 95% CI | ||
| Age group, (years) |
45–54 | 1,008 | 32.9 | 33.8 | 31.9, 35.6 |
| 55–64 | 885 | 28.8 | 27.1 | 25.8, 28.4 | |
| 65–74 | 794 | 25.9 | 26.5 | 25.1, 28.0 | |
| 75+ | 381 | 12.4 | 12.6 | 11.4, 13.8 | |
| Sex | Men | 1,162 | 37.9 | 42.6 | 41.2, 44.0 |
| Women | 1,906 | 62.1 | 57.4 | 56.0, 58.8 | |
| Race/Racial/ ethnicity |
Caucasian | 2,069 | 67.4 | 81.5 | 79.4, 83.5 |
| African-American | 999 | 32.6 | 18.5 | 16.5, 20.6 | |
| Body mass index, (kg/m2)+ |
<18.5 (underweight) | 35 | 1.2 | 1.1 | 0.8, 1.3 |
| 18.5–24.9 (normal) | 749 | 24.5 | 25.1 | 23.9, 26.4 | |
| 25.0–29.9 (overweight) | 1,160 | 38.0 | 39.5 | 38.1, 40.9 | |
| >= 30 (obese) | 1,112 | 36.4 | 34.3 | 32.9, 35.8 | |
Weighted to the 1990 target population.
World Health Organization categories (34); values for 12 participants are missing.
Figure 1.
Sample size for hip symptoms and radiographic hip OA analyses: The Johnston County Osteoarthritis Project
Overall, 36% reported hip symptoms, 27.6% had radiographic hip OA, 9.7% had symptomatic hip OA, and 2.5% had moderate/severe radiographic hip OA (Table 2). The prevalence of these 4 outcomes was consistently and often significantly higher for older age groups. Three outcomes (hip symptoms, radiographic hip OA, and symptomatic hip OA) were significantly higher among women compared to men, and 2 outcomes (radiographic hip OA, symptomatic hip OA) were significantly higher among African-Americans than Caucasians (Table 2).
TABLE 2.
Weighted prevalence for 4 hip outcomes, all participants and by selected demographic subgroups, Johnston County Osteoarthritis Project, 1991–1997*.
| Demographic subgroup |
Hip symptoms | Radiographic Hip OA |
Symptomatic Hip OA |
Severe Radiographic Hip OA |
||||
|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| All participants | 36.2 | 34.7,37.8 | 27.6 | 26.3,28.9 | 9.7 | 8.9,10.6 | 2.5 | 2.2, 3.0 |
| Age group | ||||||||
| 45–54+ | 30.7 | 28.5,33.0 | 21.2 | 19.0,23.6 | 5.9 | 4.7, 7.3 | 1.4 | 0.8, 2.4 |
| 55–64 | 35.9 | 33.6,38.3 | 23.0 | 21.1,25.1 | 8.9 | 7.5,10.5 | 1.1 | 0.8, 1.6 |
| 65–74 | 40.7 | 38.1,43.4 | 31.1 | 28.9,33.4 | 10.8 | 9.4,12.5 | 3.6 | 2.8, 4.6 |
| 75+ | 42.3 | 38.3,46.3 | 42.9 | 39.2,46.7 | 17.0 | 14.6,19.6 | 5.7 | 4.3, 7.5 |
| Sex | ||||||||
| Men | 31.8 | 29.8,33.8 | 25.4 | 23.6,27.3 | 8.3 | 7.2, 9.5 | 2.6 | 2.0, 3.2 |
| Women | 39.5 | 37.7,41.5 | 29.5 | 27.8,31.3 | 11.1 | 9.9,12.3 | 2.5 | 2.1, 3.1 |
| Race/ethnicity | ||||||||
| Caucasians | 36.0 | 34.3,37.8 | 26.6 | 25.1,28.1 | 9.2 | 8.3,10.2 | 2.4 | 2.0, 3.0 |
| African-Americans | 37.1 | 34.9,39.4 | 32.1 | 29.9,34.4 | 12.0 | 10.3,13.9 | 3.1 | 2.5, 4.0 |
Weighted to the 1990 target population.
Radiographic data were available only for age 50 and older in women.
Results of age, sex, and racial group stratified analyses are presented in Table 3. Prevalence of hip symptoms was generally similar by age for both sexes and racial groups; for 3 outcomes (radiographic hip OA, symptomatic hip OA, and moderate/severe radiographic hip OA), prevalence was generally higher in those 75+ and occasionally for those 65–74, compared to younger ages in both sex and racial groups, but these differences were not large. One notable exception was the category of African-American men aged 75 years or older, in whom the prevalence of hip symptoms and symptomatic hip OA was lower than in the younger age categories.
TABLE 3.
Weighted prevalence for 4 hip outcomes, by race/ethnicity, sex, and age group, Johnston County Osteoarthritis Project 1991–1997*.
| Racial/ethnic group Sex |
Hip symptoms | Radiographic Hip OA | Symptomatic Hip OA | Severe Radiographic Hip OA | |||||
|---|---|---|---|---|---|---|---|---|---|
| Age group | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Caucasian | |||||||||
| Men | All | 31.7 | 29.6,34.0 | 23.8 | 21.9,25.9 | 7.6 | 6.4, 8.9 | 2.5 | 1.9, 3.3 |
| 45–54 | 30.3 | 26.5,34.3 | 20.9 | 17.8,24.5 | 6.6 | 4.8, 9.0 | 1.7 | 0.9, 3.5 | |
| 55–64 | 29.7 | 25.7,34.0 | 18.5 | 15.8,21.7 | 5.7 | 4.2, 7.8 | 0.9 | 0.5, 1.8 | |
| 65–74 | 33.5 | 29.9,37.4 | 32.0 | 27.9,36.3 | 8.3 | 6.2,10.9 | 5.8 | 4.3, 7.9 | |
| 75+ | 40.1 | 32.7,47.9 | 30.9 | 24.6,38.0 | 16.2 | 11.3,22.7 | 1.6 | 0.8, 3.3 | |
| Women | All | 39.4 | 37.1,41.6 | 29.1 | 27.1,31.2 | 10.8 | 9.5,12.2 | 2.3 | 1.8, 3.0 |
| 45–54 | 30.6 | 27.6,33.7 | |||||||
| 50–54+ | 18.5 | 15.5,21.9 | 4.1 | 2.6, 6.2 | 1.1 | 0.4, 3.1 | |||
| 55–64 | 39.7 | 36.3,43.2 | 25.1 | 22.1,28.3 | 10.1 | 8.1,12.5 | 1.1 | 0.7, 1.8 | |
| 65–74 | 45.1 | 41.2,49.1 | 28.7 | 25.5,32.1 | 11.3 | 9.2,13.9 | 1.5 | 0.8, 2.8 | |
| 75+ | 45.2 | 39.7,50.9 | 47.4 | 41.8,53.2 | 17.6 | 14.5,21.2 | 7.1 | 5.0,10.1 | |
| African American | |||||||||
| Men | All | 32.0 | 28.5,35.8 | 33.2 | 29.6,37.0 | 11.7 | 9.1,14.9 | 2.7 | 1.7, 4.2 |
| 45–54 | 26.1 | 21.0,32.0 | 29.3 | 23.7,35.6 | 5.7 | 3.2,10.0 | 0.9 | 0.4, 2.2 | |
| 55–64 | 35.3 | 28.4,42.8 | 34.2 | 26.7,42.6 | 14.7 | 8.9,23.4 | 1.5 | 0.6, 3.6 | |
| 65–74 | 41.7 | 35.7,48.0 | 34.1 | 28.2,40.6 | 16.9 | 12.8,22.0 | 5.3 | 3.4, 8.1 | |
| 75+ | 21.1 | 12.9,32.5 | 43.0 | 33.3,53.2 | 12.9 | 6.0,25.5 | 5.8 | 1.3,21.9 | |
| Women | All | 40.3 | 37.7,43.0 | 31.2 | 28.2,34.4 | 12.2 | 10.3,14.5 | 3.5 | 2.7, 4.6 |
| 45–54 | 36.3 | 32.1,40.7 | |||||||
| 50–54+ | 21.3 | 16.0,27.7 | 7.8 | 4.4,13.4 | 0.9 | 0.3, 2.3 | |||
| 55–64 | 42.1 | 37.4,46.9 | 23.6 | 19.9,27.8 | 11.6 | 8.6,15.5 | 1.4 | 0.5, 3.9 | |
| 65–74 | 42.0 | 37.4,46.9 | 37.1 | 30.8,44.0 | 12.3 | 8.7,17.2 | 5.3 | 3.7, 7.5 | |
| 75+ | 42.1 | 34.2,50.5 | 45.7 | 39.5,52.0 | 17.7 | 14.0,22.0 | 7.3 | 4.8,10.9 | |
Weighted to the 1990 target population.
Radiographic data were available only for age 50 and older in women.
Women had higher prevalence of hip symptoms than men for both racial groups overall and for several of the age groups within racial groups (Table 3). The prevalence of radiographic hip OA and symptomatic hip OA was higher among Caucasian women than Caucasian men overall and for several of the age groups examined, but there was little difference between African-American women and men overall or within age groups for these outcomes. No differences in prevalence by sex was seen for moderate/severe radiographic hip OA overall or by racial or age groups.
African-Americans had a higher prevalence of radiographic hip OA and symptomatic hip OA than Caucasians overall, among men, and for several of the age groups among men, but racial comparisons in women showed no differences (Table 3); no racial differences in the prevalence of hip symptoms or moderate/severe radiographic hip OA were seen overall or by sex or age groups.
DISCUSSION
In residents aged 45 years and older in the sampled 6 townships of Johnston County, these hip OA-related measures occurred at surprisingly high but different frequencies, with hip symptoms occurring most commonly, followed by radiographic hip OA, symptomatic hip OA, and moderate/severe radiographic hip OA. This is the first U.S. study to provide prevalence estimates for these 4 outcomes by age, sex, and race. Contrary to previous indirect comparisons, African-Americans did not have lower prevalence of radiographic hip OA or moderate/severe radiographic hip OA and were at least as likely, if not more likely, as Caucasians to have these 4 hip outcomes.
For hip symptoms, the only previous population-based prevalence estimates of hip-related OA outcomes in men and women in the United States came from the 1971–1975 NHANES-I and the 1988–1994 NHANES-III. NHANES-I focused on the civilian, non-institutionalized population age 25–74 (for hip outcomes, men ages 25–74 years and women 50–74 years) in the contiguous United.States. Defining hip pain as “ever having significant pain in your hips on most days for at least 1 month”, this study reported an overall prevalence of 6.6%, and found generally increasing rates by age and roughly similar rates by sex and white/black race (11). The more recent NHANES-III defined hip pain as “significant hip pain on most days over the preceding 6 weeks” and in analyses confined to those 60 years of age and older, found hip pain reported by 14.3% overall with higher estimates in women than men, a higher estimate among non-Hispanic black men (14.8%) than non-Hispanic white men (12.4%), and the opposite race effect among women (26). The higher prevalence of hip pain in NHANES-III compared with NHANES-I was speculated to be related to possible non-articular source of pain in older individuals, or potentially an increase in incidence of hip OA(26). Our Johnston County prevalence estimates for hip symptoms were about 4–5 times higher for comparable age ranges than NHANES-I and 2–3 times higher than NHANES-III; higher among women; and similar by race. Our prevalence estimates are probably higher in part than these other studies as a result of applying a broader case definition (aching or stiffness as well as pain) without requiring a specific duration criterion (“at least 1 month” or “over the preceding 6 weeks”) or “significant” pain.
For radiographic hip OA outcomes, the only previous population-based prevalence estimates came from NHANES-I, which defined radiographic hip OA based on the overall K-L grade of non-weight-bearing hip radiographs subjectively synthesized by the non-radiologist readers (11), using the 1963 Atlas of Standard Radiographs (14). Prevalence of radiographic hip OA among those 45–54, 55–64, and 65–74 years were about 0.7%, 2.7%, and 3.6%, respectively and was higher in men than women ages 65–74 years (4.6% in men, 2.7% in women) (11). Comparable overall age-specific prevalence figures from our study were 8–30 times higher than those from NHANES-I (at 21%, 23%, and 31%, respectively) and were similar for men and women ages 65–74 years. There may be several reasons for the difference. First, NHANES-I radiographs may have been under-read, resulting in an underestimate of the true prevalence (27). Second, men in rural or non-metropolitan areas such as Johnston County may have a higher prevalence of radiographic hip OA than those in urban or metropolitan areas (28). Third, geographic variation in risk factors for hip OA may exist between NHANES-I and our study (the contiguous United States and the South, respectively). Finally, differences in radiographic techniques and secular trends in underlying risk factors in the 20 year interval may preclude direct comparisons of estimates between the 2 studies.
A special contribution of this study is the finding that African-Americans were at least as likely, if not more likely, to have radiographic and symptomatic hip OA than Caucasians. Prior studies had suggested a much lower prevalence of hip OA among native black Africans (12–13), as did studies comparing African and Caribbean blacks to European Caucasians (29). In addition, it has been unclear if the lower rate of total hip replacement surgery among blacks in the United States (30) was related to a lower prevalence of hip OA in this demographic group, or to patient preferences, health care system, cultural, or other reasons for lower utilization of this treatment modality, as seen in racial disparities of utilization of total knee replacement for knee OA(31). Our data, as well as the report by Tepper and Hochberg showing no significant racial difference in radiographic hip OA in the NHANES-I (11), together suggest that African-Americans are not spared radiographic and symptomatic hip OA, and that alternate explanations for racial disparities in the use of joint replacement for hip OA should be investigated. These data also suggest the possibility of unmet need in this group and the need for education of health care providers about this issue.
This study has several limitations. First, as is typical for most population-based studies utilizing radiographs for diagnosis, it occurred in a limited geographic region that may not be representative of the United States as a whole in terms of geography, rurality, and important factors such as obesity. However, about 70% of our sample was overweight or obese, similar to current figures for the rest of the country (32) suggesting that the high prevalence of obesity may not be such a limitation. Second, this study focused only on those 45 and older, although these are the ages when OA begins to be detected more commonly. Finally, symptoms were not defined using groin pain, a more specific hip symptom than what people perceive to be hip symptoms, which can mistakenly include sciatica and lumbar pain (33).
On the other hand, this study has several significant strengths. It occurred relatively recently in a well-defined population with a large sample size and a sizable proportion of African-Americans and men. The 2 racial groups were recruited from the same geographic location, decreasing the systematic bias that inevitably occurs by comparing racial groups recruited from different geographic regions. Both racial groups underwent identical examination using the same techniques, with very high reproducibility of the radiographic reading procedure. Additionally, participants were well-characterized for OA using radiographs and symptoms, allowing 4 outcomes to be examined. Specifically, our estimates of radiographic outcomes excluded people with findings consistent with inflammatory arthritis, thereby sharpening the distinction between those with and those without radiographic hip OA, in contrast to other studies that did not make this clarification (11). Our estimates may be conservative because we excluded those with hip replacements, most of whom probably had OA (9). Finally, our exclusions of those with missing symptom or radiographic data were unlikely to bias our results because those with missing data were similar to those with complete data.
Our results have demonstrated that these 4 outcomes represent a common occurrence for many persons aged 45 years and older, for both sexes, and for African-Americans as well as Caucasians. Although these estimates can strictly apply only to the target population in which the study was conducted, it appears likely that the frequencies of these outcomes have substantially increased over the last 20 to 30 years. In the future as our population ages, and the obesity epidemic goes unchecked (32), the prevalence of these hip related OA outcomes and accompanying disability can be expected to increase for all ages, both sexes, and these racial groups. Reducing this impact will require educating the public and health care community about modifiable risk factors for hip OA occurrence and progression, finding new modifiable risk factors, and developing effective interventions to treat, slow progression, and ultimately prevent OA.
ACKNOWLEDGMENTS
The authors thank the staff of the Johnston County Osteoarthritis Project for their long-standing and dedicated work, as well as the Project participants, without whose continuing cooperation none of this work would be possible.
This work was supported by the Centers for Disease Control and Prevention/Association of Schools of Public Health S043 and S3486 (JMJ, JBR, GL, ADD, JW, FF, LFC, WDK); 5-P60-AR30701, 5-P60-AR49465 from the National Institute of Arthritis, Musculoskeletal and Skin Diseases (JMJ, JBR, GL, ADD, JW, FF, TAS, LMA, LFC) and T-32 Arthritis and Immunology Training Grant (AEN). The John A. Hartford Foundation Center of Geriatric Excellence also supported this work (AEN). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
This is a pre-copy-editing, author-produced PDF of an article accepted for publication in The Journal of Rheumatology following peer review. The definitive publisher-authenticated version: Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, Fang F, Schwartz TA, Nelson AE, Abbate LM, Callahan LF, Kalsbeek WD, Hochberg MC. Prevalence of Hip Symptoms and Radiographic and Symptomatic Hip Osteoarthritis in African Americans and Caucasians: The Johnston County Osteoarthritis Project. J Rheumatol 2009; 36(4):809-15 is available online at: http://jrheum.org/content/36/4/809.full
Public access to the manuscript must be delayed until 12 months after first online publication in The Journal of Rheumatology.
Contributor Information
Joanne M. Jordan, Departments of Medicine, Orthopaedics, and Adjunct Professor of Epidemiology, University of North Carolina at Chapel Hill.
Charles G. Helmick, Centers for Disease Control and Prevention. Atlanta GA.
Jordan B. Renner, Departments of Radiology and Allied Health Sciences, University of North Carolina at Chapel Hill.
Gheorghe Luta, Department of Biostatistics, Bioinformatics, and Biomathematics, Georgetown University.
Anca D. Dragomir, Department of Epidemiology at UNC, currently National Institute of Child Health and Human Development, National Institutes of Health, Bethesda MD.
Janice Woodard, University of North Carolina at Chapel Hill.
Fang Fang, University of North Carolina at Chapel Hill.
Todd A. Schwartz, Department of Biostatistics, University of North Carolina at Chapel Hill.
Amanda E. Nelson, Department of Medicine, University of North Carolina at Chapel Hill.
Lauren M. Abbate, Departments of Medicine and Epidemiology, University of North Carolina at Chapel Hill.
Leigh F. Callahan, Departments of Medicine, Orthopaedics, Social Medicine, and Epidemiology, University of North Carolina at Chapel Hill.
William D. Kalsbeek, Department of Biostatistics, University of North Carolina at Chapel Hill.
Marc C. Hochberg, Department of Medicine, University of Maryland.
References
- 1.Meenan RF, Callahan LF, Helmick CG. The National Arthritis Action Plan: a public health strategy for a looming epidemic. Arthritis Care Res. 1999;12(2):79–81. [PubMed] [Google Scholar]
- 2.Lethbridge-Cejku M, Schiller JS, Bernadel L. Summary health statistics for U.S. adults: National Health Interview Survey, 2002. Vital Health Stat. 2004;10(222):1–151. [PubMed] [Google Scholar]
- 3.Prevalence of disabilities and associated health conditions among adults--United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50(7):120–125. [PubMed] [Google Scholar]
- 4.Mili F, Helmick CG, Moriarty DG. Health related quality of life among adults reporting arthritis: analysis of data from the Behavioral Risk Factor Surveillance System, US, 1996-99. J Rheumatol. 2003;30(1):160–166. [PubMed] [Google Scholar]
- 5.Lethbridge-Cejku M, Helmick CG, Popovic JR. Hospitalizations for arthritis and other rheumatic conditions: data from the 1997 National Hospital Discharge Survey. Med Care. 2003;41(12):1367–1373. doi: 10.1097/01.MLR.0000100582.52451.AC. [DOI] [PubMed] [Google Scholar]
- 6.Update: direct and indirect costs of arthritis and other rheumatic conditions--United States, 1997. MMWR Morb Mortal Wkly Rep. 2004;53(18):388–389. [PubMed] [Google Scholar]
- 7.Yelin E, Cisternas MG, Pasta DJ, Trupin L, Murphy L, Helmick CG. Medical care expenditures and earnings losses of persons with arthritis and other rheumatic conditions in the United States in 1997: total and incremental estimates. Arthritis Rheum. 2004;50(7):2317–2326. doi: 10.1002/art.20298. [DOI] [PubMed] [Google Scholar]
- 8.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeFrances CJ, Podgornik MN. 2004 National Hospital Discharge Survey. Adv Data. 2006;(371):1–19. [PubMed] [Google Scholar]
- 10.Jordan JM. Epidemiology of osteoarthritis. In: Hochberg MC, editor. Rheumatology. 4th edition. Philadelphia: Elsevier; 2008. pp. 1689–1700. [Google Scholar]
- 11.Tepper S, Hochberg MC. Factors associated with hip osteoarthritis: data from the First National Health and Nutrition Examination Survey (NHANES-I) Am J Epidemiol. 1993;137(10):1081–1088. doi: 10.1093/oxfordjournals.aje.a116611. [DOI] [PubMed] [Google Scholar]
- 12.Solomon L, Beighton P, Lawrence JS. Rheumatic disorders in the South African Negro. Part II. Osteo-arthrosis. S Afr Med J. 1975;49(42):1737–1740. [PubMed] [Google Scholar]
- 13.Ali-Gombe A, Croft PR, Silman AJ. Osteoarthritis of the hip and acetabular dysplasia in Nigerian men. J Rheumatol. 1996;23(3):512–515. [PubMed] [Google Scholar]
- 14.Kellgren JH, Lawrence JS, editors. The epidemiology of chronic rheumatism, atlas of standard radiographs. Oxford: Blackwell Scientific; 1963. [Google Scholar]
- 15.Spector TD, Hochberg MC. Methodological problems in the epidemiological study of osteoarthritis. Ann Rheum Dis. 1994;53(2):143–146. doi: 10.1136/ard.53.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hochberg MC. Osteoarthritis. In: Silman AJ, Hochberg MC, editors. Epidemiology of the Rheumatic Diseases Second Edition. Second ed. New York, NY: Oxford University Press; 2001. pp. 205–229. [Google Scholar]
- 17.Hochberg MC. Development and progression of osteoarthritis. J Rheumatol. 1996;23(9):1497–1499. [PubMed] [Google Scholar]
- 18.Meenan R, Sharpe P, Boutaugh M, Brady T. Work Group Recommendations: 2002 Exercise and Physical Activity Conference, St. Louis, Missouri - Session VI: Population Approaches to Health Promotion and Disability Prevention Through Physical Activity; Arth Care Res; 2003. p. 477. [DOI] [PubMed] [Google Scholar]
- 19.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians:The Johnston County Osteoarthrtis Project. J Rheumatol. 2007;34(1):172–180. [PubMed] [Google Scholar]
- 20.US Department of Commerce - Bureau of the Census. Washington: US GPO: Census of Population and Housing; 1990. 1990. [Google Scholar]
- 21.Johnston County Health Department. Johnston County Health Department community diagnosis and comprehensive plan, fiscal year 1989–1991. Johnston County: Johnston county health department. 1989 [Google Scholar]
- 22.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8(4):242–250. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 23.SAS Institute 2000 SAS®, version 9.1. Cary, NC: SAS Institute; 2000. [Google Scholar]
- 24.SUDAAN® Language Manual. NC: Research Triangle Park; 2004. [Google Scholar]
- 25.Kalton G, Flores-Cervantes I. Weighting Methods. Journal of Official Statistics. 2003;19(2):81–97. [Google Scholar]
- 26.Christmas C, Crespo CJ, Franckowiak SC, Bathon JM, Bartlett SJ, Andersen RE. How common is hip pain among older adults? Results from the Third National Health and Nutrition Examination Survey. Journal of Family Practice. 2002;51(4):345–348. [PubMed] [Google Scholar]
- 27.Helmick CG, Pollard RA, Jordan JM, Renner JB, Fryer JG. Evidence for underreading of radiographic osteoarthritis of the hips and knees in the first National Health and Nutrition Examination Survey (NHANES I) Arthritis and Rheumatism. 1994;37(9):S301. [Google Scholar]
- 28.Grubber JM, Callahan LF, Helmick CG, Zack MM, Pollard RA. Prevalence of radiographic hip and knee osteoarthritis by place of residence. J Rheumatol. 1998;25(5):959–963. [PubMed] [Google Scholar]
- 29.Lawrence JS, Sebo M. The geography of osteoarthritis. In: Nuki G, editor. The aetiopathogenesis of osteoarthritis. Baltimore: University Park Press; 1980. pp. 155–183. [Google Scholar]
- 30.Hoaglund FT, Oishi CS, Gialamas GG. Extreme variations in racial rates of total hip arthroplasty for primary coxarthrosis: a population-based study in San Francisco. Ann Rheum Dis. 1995;54(2):107–110. doi: 10.1136/ard.54.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: a comparison between African American and white patients. Arth Care & Res. 2001;45(4):340–345. doi: 10.1002/1529-0131(200108)45:4<340::AID-ART346>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 32.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 33.Birrell F, Croft P, Cooper C, Hosie G, Macfarlane G, Silman A The PCR Hip Study Group. Health impact of pain in the hip region with and without radiographic evidence of osteoarthritis: a study of new attenders to primary care. Ann Rheum Dis. 2000;59(11):857–863. doi: 10.1136/ard.59.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]