The preliminary results of infectious complications in orthotopic liver transplantation (OLT) using FK 506 as a primary immunosuppressive agent were encouraging.1 This early experience, however, was limited to only 20 patients who were followed for a short period of time. We have now extended our observations to 110 consecutive adult liver transplant recipients of first livers enrolled in the first human clinical trial of OLT under FK 506. A longer follow-up period (5 to 12 months) has allowed us to compare FK 506 with previous studies of infections in the cyclosporine (Cy A) era2 and to assess whether this new agent alters the infectious profile and overall rate of infection. The influence of FK 506 on well established risk factors for infection were specifically addressed, and include preoperative patient status, requirement for additional immunosuppression, reoperation, and retransplantation.
METHODS
The patient population included 110 consecutive adults who underwent OLT between August 18, 1989 and February 18, 1990. All patients were followed prospectively from the time of surgery to discharge or death. Out-patient follow-up continued until July 1, 1990. General characteristics and indications for OLT are summarized in Table 1. The mean age was 46 ± 12 years, with 17 patients older than 60 years of age. There were 58 males and 52 females. Mean follow-up was 214 ± 50 days with a range of 134 to 315 days. Eight-five patients were seriously ill (status 3, 4, or UNOstat), as defined by the current United Network for Organ Sharing (UNOS) stratification: status 1, at home, functioning Without domiciliary nursing care; status 2, at home, not working and requiring professional nursing care; status 3, hospital bound; status 4, intensive care unit bound. UNOstat-ICU bound requiring life support. The most frequent indication for OLT was nonalcoholic cirrhosis followed by alcoholic and cholestatic liver disease.
Table 1.
Patient Population and Indications for OLTx
| Demographics | |
| No. of patients | 110 |
| No. of transplants | 124 |
| Age (y) | 46 + 12 (18 to 69) |
| Sex (M/F) | 58/52 |
| Mean follow-up (d) | 214 + 50 |
| Indications | |
| Nonalcoholic cirrhosis | 45 (41.0%) |
| Alcoholic cirrhosis | 28 (25.5%) |
| Cholestatic disease | 28 (25.5%) |
| Fulminant failure | 3 (2.7%) |
| Tumor | 2 (1.8%) |
| Miscellaneous | 4 (3.5%) |
Immunosuppression
Immunosuppression protocol included FK 506 and steroids in all patients. The first 57 patients received FK 506 as an IV loading dose of 0.15 mg/kg followed by an IV maintenance dose of 0.075 mg/kg twice a day. Conversion from IV to oral doses was usually overlapped for 1 day with oral maintenance doses of 0.15 mg/kg given every 12 hours. Initial steroid therapy included a 1 g IV bolus of methylprednisolone intraoperatively. A 200 mg dose on the first postoperative day was then reduced by 40 mg increments to a maintenance dose of 20 mg by day 6. The subsequent 53 patients received IV maintenance doses of FK 506 and methylprednisolone from the outset, omitting the loading dose of FK 506 and both the steroid bolus and taper. Subsequent adjustments were dictated by the quality of the graft, the presence of rejection, toxicity symptoms, and the FK 506 plasma levels.
Infection Prophylaxis
The patients received perioperatlve IV cefotaxime and ampicillin 3 g/d which was continued for the first 3 days after transplant. Oral mycostatin 2 million U/d was given for the first 6 months. High dose oral acyclovir ranging from 400 mg to 3200 mg/d was given with dose adjustment according to renal function. One tablet of Bactrim SS daily (80 mg of trimethoprim plus 400 mg of sulfamethoxazole) was given for almost 1 year.
Definition of Infections
We followed the definitions of infections described by Kusne et al2 from our institution with classification done according to the time of diagnosis, maior pathogen, and site of occurrence. An infection was considered to be associated with death if it was found at the autopsy or if the patient was still under treatment for the infection at the time of death. An infection was defined as severe if it involved solid organs or cavities and required treatment with specific antibiotics and/or surgical intervention. Examples of severe infections in this study included peritonitis, pneumonia, cholangitis, abdominal or liver abscess, pericarditis, symptomatic CMV and Epstein-Barr virus (EBV) infections, invasive candidiasis, and aspergillosis. Examples of nonsevere infections included line infection, superficial wound infection, colitis, sinusitis, otitis, mucocutaneous herpes simplex, and candida colonization.
Statistics
The number of infections per patient was compared between patient groups nonparametrically using the Wilcoxon two-sample test for location. Although follow-up time varied from patient to patient, follow-up time was not related to the number of infections.
RESULTS
From July 1, 1990 (when data compilation closed) to August 16, 1990, 102 (92.7%) of the patients are alive. Ten patients underwent retransplantation, with six requiring one graft and four, two grafts. Six of these patients are alive. Five of eight deaths were due to infection (62.5%) and three to other causes such as heart failure, stroke, and multiorgan failure. Of the infection related deaths, two occurred following retransplantation. The majority of bacterial and fungal infections were seen within the first 60 days with viral infections persisting through the first 6 months. The severity and frequency of infections are shown in Table 2. Overall, 50% of patients developed infection of which 38% suffered severe ones. Bacterial infections predominated with some patients infected with multiple organisms. Sixty-four episodes of bacterial infection, which ranged in severity, were noted. A combination of viral, bacterial, or fungal infection was noted in 16% of the patients while a single type of infection occurred in 34%. No protozoal infections were seen. Eight of the III (7.2%) episodes resulted in death and were predominantly bacterial and fungal (7).
Table 2.
Percentage of Patients Infected and the Episodes of Infection Per Patient
| % Patients Infected | Episodes of Inf × Pt | |||
|---|---|---|---|---|
| All | Several | All | Several | |
| Bacterial | 36 | 19 | 0.58 | 0.24 |
| Viral | 24 | 23 | 0.31 | 0.28 |
| Fungal | 9 | 6 | 0.12 | 0.06 |
| Total | 50 | 38 | 1.01 | 0.58 |
Note: Distinction has been made between severe and overall infections. Sixteen percent of patients suffered overlapping infections (9% bacterial + viral. 3% bacterial + fungal. 4% bacterial + viral + fungal) while 34% developed only one type (20% bacterial, 11% viral, 2% fungal).
In the bacterial group (Table 3) the most frequent severe infections were pneumonia (8), peritonitis (8), and cholangitis (6). The majority of the microorganisms isolated were aerobic gram positive (38) and gram negative aerobes (23). Anaerobes were unusual with Clostridium difficile accounting for seven of eight cases.
Table 3.
Number of Episodes of Infection That Occurred in 55 of 110 Patients
| Bacterial (64)* | |
| Soft tissue | (12) |
| Line sepsis | (11) |
| Pneumonia | (8) |
| Peritonitis | (8) |
| Colitis | (7) |
| Cholangitis | (6) |
| Urinary tract | (5) |
| Sinusitis | (2) |
| Intrabdominal abscess | (1) |
| Liver abscess | (1) |
| Pericarditis | (1) |
| Cervical TB | (1) |
| Otitis media | (1) |
| Viral (34) | |
| CMV | (27) |
| Herpes Simplex | (4) |
| EBV | (3) |
| Fungal (13) | |
| Candidiasiasis | (5) |
| Colonized candida | (6) |
| Aspergillosis | (2) |
Note. Severe infections are italicized.
19 episodes of bacteremia are included, all of known origin.
Cervical lymphadenitis caused by Mycobacterium tuberculosis was seen in one patient and required prolonged treatment with conventional triple therapy (isoniazid, ethambutol, and rifampin). However, 3 months later isoniazid hepatotoxicity necessitated discontinuation of this drug.
Symptomatic CMV was the most frequent viral infection and occurred in 23 patients. The liver and gastrointestinal tract were the predominant sites of infection (eight episodes each) followed by the lungs (five examples). Three patients developed multiple and recurrent episodes of CMV at different sites and all were fund to have concomitant retinitis as a late manifestation. The first patient was a 19-year-old man, retransplanted after 40 days for rejection. He was seronegative for CMV and received his second liver from a seropositive donor. He had a positive cytotoxic crossmatch with both donors and heavy immunosuppression was required throughout his early course for persistent rejection. Multiple episodes of symptomatic CMV subsequently developed and included pneumonia, hepatitis, and retinitis at 3, 4, and 6 months respectively. Two patients had a similar course with initial episodes of CMV infection occurring during the third month posttransplant (hepatitis-I, pneumonia-I) with readmission required at 5 months for concomitant CMV gastritis and retinitis. In all cases treatment with DHPG was successful and none of the patients had residual sequelae from the retinitis.
EBV infection associated with polyclonal lymphoproliferative disease was confirmed histologically in three patients. A 19-year-old man developed an infectious mononucleosis syndrome with enlargement of the tonsils and was successfully treated with tracheostomy, tonsillectomy, acyclovir, and reduction of the FK dose. The other two patients developed polyclonal lymphoma arising in the allograft. One highly sensitized patient (positive cross-match with all donors) died of overwhelming pseudomonas and candida sepsis 9 days after undergoing a third transplant for rejection, while the other patient whose lymphoma was confined to the graft recovered following left hepatic segmentectomy.
Of the five cases of invasive candidiasis, two were associated with death. A fatal aspergillosis was seen in a 31-year-old woman. Twenty-one days after transplant, she was noted to have several pulmonary nodules, which contained aspergillus on biopsy. She received a full course of amphotericin B therapy (3 g total dose), with partial regression of these nodules. She then required retransplantation for hepatic artery thrombosis at 3.5 months and succumbed to bacterial sepsis and recurrent aspergillus in her thoracic spine at 5 months (vertebral osteomyelitis).
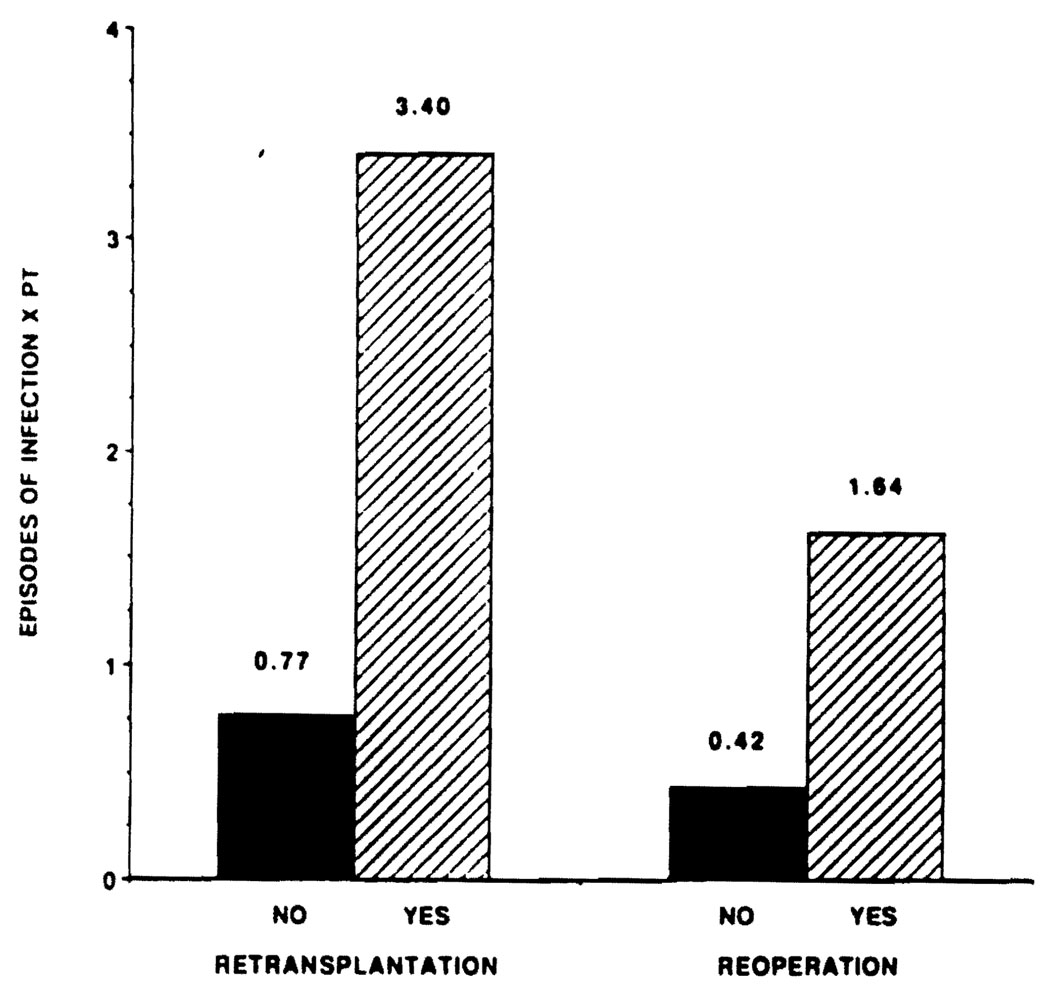
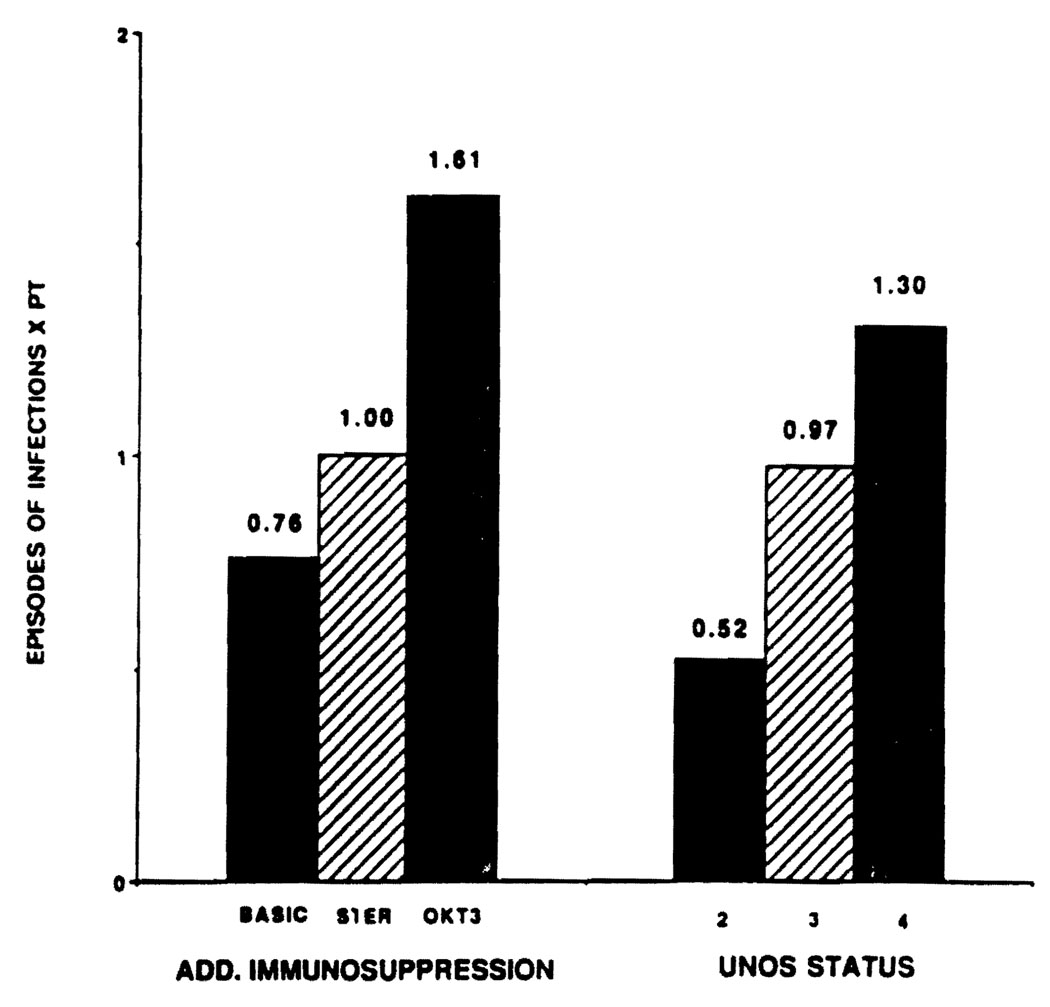
Significant higher rates of infection were seen in the sickest pretransplant patients and in those receiving additional intense immunosuppression (steroid boluses, recycles, or OKT3) (Fig 1). The need for retransplantation or additional surgery was associated with especially high rates of infection (Fig 2).
Fig. 1.
Effect of additional Immunosuppression (boluses or recycles of steroids and OKT3) and UNOS status on the incidence of infections.
Fig. 2.
Effect of retransplantation and additional immunosuppression on incidence of infections. The differences are statistically significant (P < .05).
DISCUSSION
Advances in preservation, combined with technical improvements, and the routine use of veno-veno bypass have contributed to lowering morbidity of OLT. However, the intense immunosuppression required under conventional therapy continues to play a key role in contributing to infectious outcome.3,4
This large series of OLT patients receiving FK 506 has confirmed our early enthusiasm for this agent. As reported by Todo et al.5 rejection, early graft dysfunction, and the need for retransplantation have been reduced in FK 506 treated patients. The potent immunosuppressive properties of this drug have allowed for significant reductions in steroid use without increasing the risk of rejection. In fact, fewer infections were seen.
The patterns and timing of the infections that did occur were similar to those developing under conventional therapy, with bacterial and fungal infections predominating early in the course. However, 50% of patients receiving FK 506 were entirely free of infections compared with only 17% in the historical controls from Kusne’s earlier report from our institution.2 Although infection continues to cause or be associated with the majority of deaths, the death rate has been reduced.
Symptomatic CMV remains the most common infection. However, all herpes infections have been significantly less, an improvement that may be related to recent changes in prophylaxis with the use of acyclovir. The notable absence of protozoal infections can be explained, at least in part, in the same way.
High risk factors continue to be retransplantation, reoperation, intense additional immunosuppression in the management of rejection, and grave deterioration from end-stage liver disease going into transplantation. However, the poor prognostic portent of these risk factors has seemed less grim in the FK 506 treated patients than in the past. A generally good quality of liver graft function, which has been achievable with low (and often no) dose steroids appears to be the explanation for the improved outlook.
Acknowledgments
Supported by research grants from the Veterans Administration and project grant no. DK 29961 from the National Institutes of Health, Bethesda, Maryland.
REFERENCES
- 1.Alessiani M, Kusne S, Martin FM, et al. Transplant Proc. 1990;22:44. [PMC free article] [PubMed] [Google Scholar]
- 2.Kusne S, Dummer JS, Singh N, et al. Medicine. 1988;67:132. doi: 10.1097/00005792-198803000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ascher NL, Stock PG, Bumgardner GL, et al. Surg Gynecol Obstet. 1988;167:474. [PubMed] [Google Scholar]
- 4.Paya CV, Hermans PE, Washington JA, II, et al. Mayo Clin Proc. 1989;64:555. doi: 10.1016/s0025-6196(12)65561-x. [DOI] [PubMed] [Google Scholar]
- 5.Todo S, Fung JJ, Slarzl TE, et al. Ann Surg. (in press) [Google Scholar]