From May 1990 to August 1993, 59 patients received intestinal transplantation under FK 506 immunosuppression at the University of Pittsburgh. Preliminary data from our series have been reported before.1–4
CASE MATERIAL
Of the 59 recipients, 32 were children with a mean age of 3.8 ± 3.7 years, and 27 were adults with a mean age of 33.4 ± 9.8 years. There were 3 types of intestinal transplantation. An isolated graft was given to 22 patients who had irreversible intestinal failure but normal liver function. Combined intestine and liver grafts were transplanted to 26 patients who had failure of both organs. Eleven patients who had thrombosis in the 2 central arteries or in the mesenteric venous system, or abnormality of the entire gastrointestinal tract, received multivisceral grafts. There were an additional 2 adult patients who died on the table from massive bleeding during dissection of the native organs for multivisceral transplantation.
The operative procedures for organ procurement and transplantation, as well as postoperative management, were described previously1–6 and in this issue.7–9
RESULTS
Forty-two patients are currently alive with a minimum follow-up of 2 months. The patient survival was 84.6% at 3 months, 80.6% at 6 months, 77.6% at 12 months, and 71.4% at 24 months. Causes of the 17 mortalities were sepsis from graft rejection (n = 9), technical failure (n = 3), posttransplant lymphoproliferative disease (n = 2), and other (n = 3). Two patients had evidence of graft-versus-host disease at autopsy.
Twelve grafts were removed at various postoperative periods due to acute rejection (n = 7), chronic rejection (n = 2), or other reasons (n = 3), of which four underwent retransplantation. Graft survival was 73.9% at 3 months, 72.0% at 6 months, 67.1% at 12 months, and 53.1% at 24 months. There were no differences in patient and graft survival between adult and pediatric recipients.
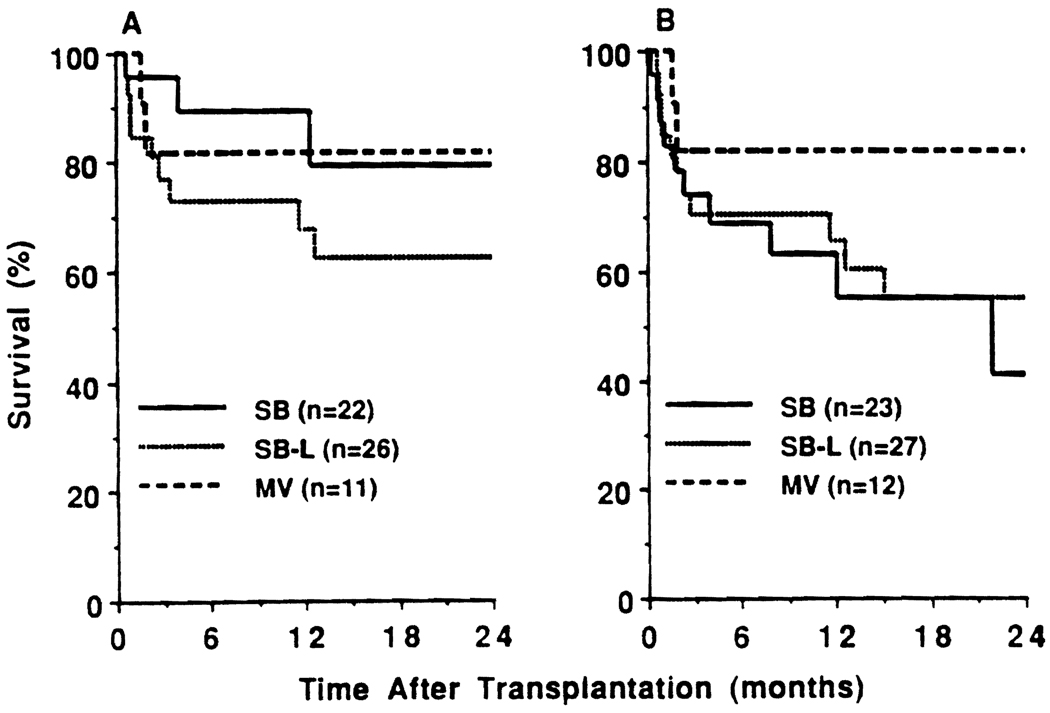
Of the 22 isolated intestinal recipients, 5 died and 8 required graft removal. Patient and graft survival rates were 95.5% and 73.9% at 3 months, 89.1% and 68.6% at 6 months, 89.1% and 62.9% at 12 months, and 79.2% and 41.3% at 24 months, respectively (Fig 1). Of the 26 combined intestine and liver recipients, 10 died and 3 required graft removal. Patient and graft survival rates for this group were 76.9% and 70.4% at 3 months, 73.1% and 70.4% at 6 months, 67.9% and 65.3% at 12 months, and 62.6% and 54.8% at 24 months, respectively. Of the 11 multivisceral patients, 2 died and 1 required removal of the pancreatic graft for hemorrhagic pancreatitis. The patient and graft survival rate was 81.8% for these patients.
Fig 1.
Patient and graft survival after intestinal transplantation. (A) Patient survival. (B) Graft survival.
Of the 42 recipients who are currently alive, 34 are completely free from total parenteral nutrition (TPN) on an unrestricted oral diet, 4 require partial TPN support, and 4 resumed TPN after graft removal.
SUMMARY
Our experience with clinical intestinal transplantation under FK 506 immunosuppression showed that 50% of the recipients were able to be independent from TPN after transplantation, but 10% require partial TPN with functioning grafts, 10% needed total TPN after graft removal, and 30% of the recipients died postoperatively, mostly from sepsis due to severe graft rejection. For further improvement in patient survival and in the quality of life for patients after intestinal transplantation, it is mandatory to establish a new strategy for treatment and prevention of graft rejection and systemic infection.
REFERENCES
- 1.Todo S, Tzakis AG, Abu-Elmagd K, et al. Transplantation. 1992;53:369. doi: 10.1097/00007890-199202010-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzakis AG, Todo S, Abu-Elmagd K, et al. Transplant Proc. 1992;24:1238. [PMC free article] [PubMed] [Google Scholar]
- 3.Todo S, Tzakis AG, Abu-Elmagd K, et al. Ann Surg. 1992;216:223. doi: 10.1097/00000658-199209000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Todo S, Tzakis AG, Abu-Elmagd K, et al. Transplant Proc. 1993;25:2195. [PubMed] [Google Scholar]
- 5.Starzl TE, Todo S, Tzakis AG, et al. Surg Gynecol Obstet. 1991;172:335. [PMC free article] [PubMed] [Google Scholar]
- 6.Casavilla A, Selby R, Abu-Elmagd K, et al. Ann Surg. 1992;216:605. doi: 10.1097/00000658-199211000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abu-Elmagd K, Bonet H, Manez R, et al. Transplant Proc. (this issue) [Google Scholar]
- 8.Reyes J, Bonet H, Green M, et al. Transplant Proc. (this issue) [Google Scholar]
- 9.Furukawa H, Casavilla A, Kadry Z, et al. Transplant Proc. (this issue) [Google Scholar]