Abstract
Background
To effectively and efficiently respond to the growing health needs of older people, it is critical to have an indepth understanding about their health status, quality of life (QoL) and related factors. This paper, taking advantage of the INDEPTH WHO-SAGE study on global ageing and adult health, aims to describe the pattern of health status and QoL among older adults in a rural community of Viet Nam, and examine their associations with some socio-economic factors.
Methods
The study was carried out in the Bavi District, a rural community located 60 km west of Hanoi, the capital, within the Epidemiological Field Laboratory of Bavi (FilaBavi). Face-to-face household interviews were conducted with people aged 50 years and over who lived in the FilaBavi area. The interviews were performed by trained surveyors from FilaBavi using a standard summary version SAGE questionnaire. Both descriptive and analytical statistics were used to examine the patterns of health status and QoL, and associations with socio-economic factors.
Results
Higher proportions of women reported both poor health status and poor QoL compared to men. Age was shown to be a factor significantly associated with poor health status and poor QoL. Higher educational level was a significant positive predictor of both health status and QoL among the study subjects. Higher economic status was also associated with both health status and QoL. The respondents whose families included more older people were significantly less likely to have poor QoL.
Conclusion
The findings reveal problems of inequality in health status and QoL among older adults in the study setting by sex, age, education and socio-economic status. Given the findings, actions targeted towards improving the health of disadvantaged people (women, older people and lower education and economic status) are needed in this setting.
Keywords: older people, health status, quality of life, rural, Viet Nam, INDEPTH WHO-SAGE
During the past few decades, under the forces of a demographic transition characterised by declining fertility rates and increasing life expectancy, the proportion of people in the world population who reach middle age and beyond is increasing sharply (1–3). Developing countries are currently ageing much faster than industrialised countries (3, 4). In 2002, almost 400 million people aged 60 and over lived in the developing world. By 2025, it may rise to 840 million representing 70% of all older people worldwide (2, 3).
Population ageing in low- and middle-income countries has special implications for many public services, especially for health care, in these countries. The health care systems of many developing countries are still focused on childhood and infectious diseases as well as reproductive health services. But the ageing population leads to increasing demands for care that addresses chronic health conditions (2). Nowadays, in all countries, and in low- and middle-income countries in particular, measures to help older people remain healthy and active are urgently needed (2, 4). To effectively and efficiently respond to the growing health needs of older populations, it is critical to have an indepth understanding about their health conditions, quality of life (QoL) and related socio-economic factors.
Viet Nam, a developing country in South-East Asia, is undergoing demographic transition and experiencing rapid population ageing. The proportion of people aged 50 years and over rose from 12.6% in 2000 to 14.1% in 2005 and will account for 18.9% of the total population in 2015 (3). In Viet Nam, the number of older people living in rural areas is about 3.5 times higher than those living in urban areas (5). About 44% of older Vietnamese are working, but mostly in agricultural activities which provide low and unstable incomes. Other sources of income, including pension and social assistance benefits, are significant factors to reduce risks for older people. However, the coverage of the current social protection system in Viet Nam is not adequate (6).
Life expectancy in Viet Nam reached 72.2 years in 2005, a relatively high level compared to the nation's economic conditions. However, the average healthy life expectancy was for lower, at 58.2 years and ranked 116 among 174 countries in the world (7). Health care for the older people in Viet Nam has been improved, but the accessibility for vulnerable and low-income older people is still low, and the poorer shoulder greater burdens of health care costs in terms of percentage of household expenditure (8)
As in other developing countries, little empirical research has been conducted in Viet Nam on the health status, QoL and related socio-economic status among older people. This article, therefore, taking advantage of the INDEPTH WHO-SAGE study on global ageing and adult health (9), aims to describe the patterns of health status and QoL among older adults in a rural community of Viet Nam, and examine their associations with some socio-economic factors.
Methods
Study design and setting
This was a population-based cross-sectional study, carried out in Bavi District, a rural community located 60 km west of Hanoi, the capital, within the Epidemiological Field Laboratory of Bavi (FilaBavi). The FilaBavi Health and Demographic Surveillance System (HDSS), supported by Sida/SAREC, was established in 1999 with a sample of around 50,000 individuals from the Bavi District. People aged 50 and over accounted for about 17% of the total population under surveillance. The surveyed population includes three distinct groups: those in mountainous areas, highlands, and riverside or island dwellers (10). The FilaBavi HDSS is a member of the INDEPTH network (11).
Data collection
Face-to-face household interviews were planned for all people aged 50 years and over who lived in the FilaBavi area between the end of 2006 and the beginning of 2007. The interviews were done by trained surveyors from FilaBavi using a summary version of the SAGE questionnaire (available as a Supplementary File to this paper). Further details of the study methodology are available separately (9). The questionnaire was translated into the local language and pre-tested before official use. Spot-checks and re-checks on sample data were conducted by supervisors for quality control.
Measurements
Outcome variable
Self-reported health status and QoL among the study subjects were outcome variables. Health status scores were calculated based on self-reported health levels in eight health domains covering: affect, cognition, interpersonal activities and relationships, mobility, pain, self-care, sleep/energy, and vision. Each domain included at least two questions. Asking more than one question about difficulties in a given domain provides more robust assessments of individual health levels and reduces measurement error for any single self-reported item. Health status scores were computed by using Item Response Theory (IRT) parameter estimates in Winsteps®, a Rasch measurement software package (http://www.winsteps.com). Higher health status scores within a 0–100 scale imply better health status. Respondents who had health status scores below the median were categorised as having poor health status. QoL was assessed by using the eight-item version of the World Health Organization Quality of Life instrument (WHOQoL). Results from the eight items were summed to get an overall WHOQoL score which was then transformed into a 0–100 scale. The higher the WHOQoL score, the better the QoL. Respondents who had WHOQoL scores less than the median were considered as having poor QoL. More details on how scores for this study were derived are given elsewhere (9).
Explanatory variables
Explanatory variables included sex (male, female), age (grouped as 50–59, 60–69, 70–79, 80+ years), educational level (no formal education, up to 6 years of formal education, more than 6 years of education), marital status (in current partnership, never married, separated, divorced and widowed), wealth index (quintiles), whether respondent stays alone (yes or no) and proportion of people aged 50 years and over in the same household (<25%, 25–49%, 50–74%, >75% +). The wealth quintiles were constructed by using principal component analysis techniques (12). Variables used included household income, the area of land owned, type of house, materials of roof and floor, toilet facilities, electricity and water supplies, and ownership of a range of durable assets for each household.
Data analysis
Both descriptive and analytical statistics were performed. The data analysis began with calculation of frequencies and percentages of the variables of interest. Multivariable logistic regressions were then carried out to examine the association between health status and QoL with the selected explanatory variables.
Ethical considerations
The protocol of this study was approved by the Scientific Board of FilaBavi. All subjects in the study were asked for their written informed consent before collecting data, and they had complete right to withdraw from the study at any time without disadvantage.
Results
Characteristics of the study populations
Of the total 8,874 people aged 50 and over living in the study setting at the time of the survey, there were 8,535 who participated in the study (amounting to 96%). Four percent of subjects were unable to participate as they were away (2.3%) or were not healthy enough to take part in the survey (1.7%). The background characteristics of potential study subjects (respondents and non-respondents) are described in Table 1. There were no significant differences in socio-economic characteristics between the respondents and the non-respondents.
Table 1.
Background characteristics of study subjects (respondents and non-respondents)
| Respondents (n = 8,535) | Non-respondents (n = 339) | |
|---|---|---|
| Gender | ||
| Male (%) | 3,469 (40.6) | 140 (42.6) |
| Female (%) | 5,066 (59.4) | 189 (57.4) |
| Age (years) | ||
| 50–59 (%) | 3,221 (37.7) | 148 (45) |
| 60–69 (%) | 2,258 (26.5) | 87 (26.3) |
| 70–79 (%) | 2,086 (24.4) | 45 (13.8) |
| 80 years and over | 970 (11.4) | 49 (14.9) |
| Mean age (SD) | 65.3 (10.7) | 63.7 (19.2) |
| Education | ||
| No formal education (%) | 878 (10.3) | 85 (25.9) |
| Primary or <6 years (%) | 4,190 (49.1) | 112 (33.9) |
| More than 6 years (%) | 3,467 (40.6) | 132 (40.2) |
| Marital status | ||
| In current partnership (%) | 5,895 (69.1) | 215 (65.5) |
| Now single (%) | 2,640 (30.9) | 114 (34.5) |
| Economic status of household | ||
| Poorest quintile | 1,209 (14.2) | 41 (12.4) |
| Second quintile | 1,548 (18.2) | 52 (15.7) |
| Third quintile | 1,787 (21) | 65 (19.9) |
| Fourth quintile | 1,996 (23.4) | 81 (24.6) |
| Least poor quintile | 1,976 (23.2) | 90 (27.4) |
| Mean number of household members (SD) | 4.2 (2) | 4.3 (1.9) |
| Proportion of household members aged 50 and over (SD) | 50.7 (28.9) | 49.5(28.8) |
Distribution of health status and WHOQoL scores
Table 2 presents the distribution of health status scores of the study population by age and sex. The overall mean health status score was 66.2 and median 65.0. In both sexes, the average health status scores decreased with age. Men had higher health status scores than women of the same age group. Overall, the proportion of respondents with below-median health status among men and women was 39.1 and 58.3%, respectively.
Table 2.
Distribution of health status scores by age and sex among 8,535 adults aged 50 years and over in northern rural Viet Nam
| Variables | Men (n = 3,469) | Women (n = 5,066) |
|---|---|---|
| Mean health status score (SD) | ||
| 50–59 years | 72.5 (11.5) | 68.8 (9.4) |
| 60–69 years | 68.8 (9.9) | 64.8 (7.9) |
| 70–79 years | 65.3 (9.2) | 61.7 (8.2) |
| 80 years and over | 60.1 (8.8) | 57.6 (8.2) |
| All ages | 60.1 (8.8) | 57.6 (8.2) |
| Proportion of respondents with health status score below the median | 68.9 (11.0) | 64.4 (8.4) |
| 50–59 years (%) | 24.4 | 35.4 |
| 60–69 years (%) | 33.1 | 51.7 |
| 70–79 years (%) | 50.1 | 67.1 |
| 80 years and over (%) | 70.0 | 81.5 |
| All ages (%) | 35.9 | 54.2 |
A similar pattern was observed for QoL. The overall mean WHOQoL score was 61.2, median 62.5. In both sexes, the average WHOQoL score decreased with age. Women had lower WHOQoL scores than men of the same age group. Overall, the proportion of respondents with poor QoL among men and women was 38.4 and 52.4%, respectively (Table 3).
Table 3.
Distribution of WHOQoL scores by age and sex among 8,535 adults aged 50 years and over in northern rural Viet Nam
| Variables | Men (n = 3,469) | Women (n = 5,066) |
|---|---|---|
| Mean QoL score (SD) | ||
| 50–59 years | 65.7 (12.7) | 62.2 (12.3) |
| 60–69 years | 64.1 (13.2) | 60.9 (12.6) |
| 70–79 years | 61.9 (14.1) | 57.7 (13.2) |
| 80 years and over | 56.6 (14.1) | 53.8 (14.0) |
| All ages | 63.7 (13.5) | 59.5 (13.2) |
| Proportion of respondents with WHOQoL score below median | ||
| 50–59 years (%) | 32.0 | 45.1 |
| 60–69 years (%) | 37.3 | 48.6 |
| 70–79 years (%) | 44.5 | 58.3 |
| 80 years and over (%) | 60.9 | 66.2 |
| All ages (%) | 38.4 | 52.4 |
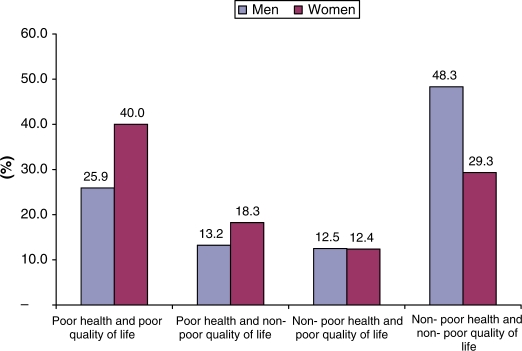
Fig. 1 shows the distribution of the study subjects by health status and QoL. Women were shown to have poorer health status than men. About 25.9% of men and 40% of women reported having both poor health status and poor QoL.
Fig. 1.
Distribution (%) of study subjects by health status and quality of life, among 8,535 adults aged 50 years and over in northern rural Viet Nam.
Factors associated with poor health status and poor quality of life (QoL)
Multivariate logistic regression analyses of the association between poor health status and poor QoL, and socio-economic status are shown in Table 4. Men were shown to be significantly less likely to have poor health status compared to women. Older respondents had poorer health status than those younger. People with lower educational levels had a significantly higher probability of having poor health status than those with higher educational levels. Study subjects in the lowest wealth quintile were more likely to have poor health status than those belonging to the highest wealth quintile. There was no significant association between poor health status and marital status or the proportion of older people living in a household.
Table 4.
Factors associated with poor health status and poor quality of life among 8,535 adults aged 50 years and over in northern rural Viet Nam
| OR with 95% CI | |||
|---|---|---|---|
| Variables | Poor health | Poor QoL | Poor health and poor QoL |
| Gender | |||
| Men | 0.7 (0.6–0.8)a | 0.8 (0.7–0.9)a | 0.8 (0.7–0.9)a |
| Women | 1 | 1 | 1 |
| Age group | |||
| 50–59 years | 1 | 1 | 1 |
| 60–69 years | 1.5 (1.3–1.7)a | 1.0 (0.9–1.1) | 1.3 (1.1–1.5)a |
| 70–79 years | 2.4 (2.1–2.8)a | 1.2 (1.1–1.4)a | 1.9 (1.6–2.2)a |
| 80 years and over | 4.6 (3.7–5.7)a | 1.8 (1.5–2.1)a | 3.0 (2.4–3.6)a |
| Educational level | |||
| No formal education | 2.7 (2.2–3.3)a | 2.1 (1.7–2.5)a | 2.3 (1.9–2.9)a |
| Less than or equal to 6 years | 1.6 (1.4–1.7)a | 1.5 (1.4–1.7)a | 1.6 (1.4–1.8)a |
| More than 6 years | 1 | 1 | 1 |
| Marital status | |||
| Now single | 1 | 1 | 1 |
| In current partnership | 0.9 (0.8–1.0) | 0.9 (0.8–1.0) | 0.8 (0.7–0.9)a |
| Proportion of people aged 50 years and over in the same household | |||
| <25% | 1.2 (1.0–1.4) | 1.6 (1.4–1.9)a | 1.4 (1.2–1.6)a |
| 25–49% | 1.1 (1.0–1.3) | 1.6 (1.4–1.9)a | 1.4 (1.2–1.6)a |
| 50–74% | 1.2 (1.0–1.4) | 1.5 (1.3–1.7)a | 1.4 (1.2–1.6)a |
| ≥75% | 1 | 1 | 1 |
| Socio-economic quintile | |||
| Poorest quintile | 1.7 (1.4–2.0)a | 3.2 (2.7–3.8)a | 2.5 (2.1–3.0)a |
| Second quintile | 1.2 (1.0–1.4) | 2.0 (1.8–2.4)a | 1.6 (1.4–1.9)a |
| Third quintile | 1.2 (1.0–1.4) | 1.7 (1.5–2.0)a | 1.5 (1.3–1.8)a |
| Fourth quintile | 1.1 (1.0–1.3) | 1.6 (1.4–1.9)a | 1.5 (1.3–1.7)a |
| Least poor quintile | 1 | 1 | 1 |
aSignificant results (95% CI does not include 1).
Similar to the pattern of health status, poor QoL was shown to be significantly associated with women, older ages, lower educational levels and lower economic status. Table 4 shows that the respondents whose families had more elderly people (≥75% people aged over 50 years and over in the same household) were significantly less likely to have poor QoL. Women, older people, those with lower educational level, without any marital partnership, with fewer older people in the family and with lower economic status were more likely to have both poor health status and poor QoL.
Discussion
This article describes the pattern of health status and QoL among older adults in a rural community of Viet Nam. It reveals socio-economic inequalities in health status and QoL among older adults in the study setting. We found that a higher proportion of women reported both poor health status and poor QoL compared to men. The findings are in line with recent studies on health status from other Asian countries such as Pakistan (13), Bangladesh (14) and Singapore (15). Gender inequality in health has been well documented in the international literature (16). The findings are also consistent with results from previous studies on QoL that reported female disadvantages in both emotional and subjective well-being (17–20). One likely explanation could be that women are more likely to suffer from conditions that are debilitating but not fatal. The paradox is that women report poorer health but live longer, and this is true in almost every country in the world (21).
Age was shown to be a factor significantly associated with poor health status and poor QoL. This has been consistently shown in previous studies (13–15). In our setting, chronic diseases were shown to be more prevalent among women and older people (22).
We found that higher educational levels were significant positive predictors of both health status and QoL among the study subjects. Education is well known as an important factor for health, both among men and women, particularly in rural areas. The findings are consistent with previous studies (13–15). Education is assumed to have a positive effect on health status since persons with more education are assumed to be better informed about health matters, diet and disease prevention measures leading to better health conditions, consequently leading to higher QoL.
Similarly, improvements in economic status are also likely to raise both health status and QoL. In addition to providing means for purchasing health care, higher economic status can provide better nutrition, housing and recreational opportunities. The findings are consistent with previous studies in Asia (13–15), in Europe (23) and the Americas (24).
This study also revealed a positive effect of having more older people living in the same family. This positive effect may be the result of mutually practised health beliefs and behaviours, shared physical environments and interpersonal relations between the older people in the same family.
We need to note some limitations of this study. Firstly, the cross-sectional nature of the data limited our ability to understand causal mechanisms that resulted in particular heath status and QoL outcomes among the study population. Secondly, low educational level and the presence of impaired cognition in older people might have led to inaccuracies in the self-reported data. Our careful training and field supervision would have overcome this problem to some extent.
In summary, this study provides cross-sectional evidence on patterns of health status and QoL among older adults in rural Viet Nam. The findings reveal problems of inequality in health status and QoL among older adults in the study setting by sex, age, education and economic status. Given these findings, actions to enhance the health of disadvantaged people (women, the elderly, less educated and lower economic status) are needed in this setting.
Supplementary Material
Access the supplementary material to this article: INDEPTH WHO-SAGE questionnaire (including variants of vignettes), a data dictionary and a password-protected dataset (see Supplementary files under Reading Tools online). To obtain a password for the dataset, please send a request with “SAGE data” as its subject, detailing how you propose to use the data, to global.health@epiph.umu.se
Acknowledgements
This research was supported by FAS, the Swedish Council for Social and Work Life Research, Grant No. 2003-0075. We would like to thank INDEPTH WHO-SAGE for support and contribution of the SAGE instrument.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.Omran AR. The epidemiological transition theory revisited thirty year later. World Health Statistic Quart. 1998;51:99–119. [Google Scholar]
- 2.World Health Organization. Active aging: a policy framework. Geneva: World Health Organization; 2002. [Google Scholar]
- 3.United Nations. World population prospects: the 2006 revision and world urbanization prospects. 2006. Available from: http://esaunorg/unpp [cited 10 December 2009]
- 4.Shrestha LB. Population aging in developing countries. Health Aff (Millwood) 2000;19:204–12. doi: 10.1377/hlthaff.19.3.204. [DOI] [PubMed] [Google Scholar]
- 5.UNFPA Viet Nam. How can Vietnam respond to population ageing? Hanoi: UNFPA; 2009. [Google Scholar]
- 6.Giang TL, Dfau WD. Demographic changes and the long-term pension finances in Vietnam: a stochastic actuarial assessment. J Popul Ageing. 2009;1:125–51. [Google Scholar]
- 7.Ministry of Health of Vietnam. Hanoi: Ministry of Health of Vietnam; 2008. Joint annual health review 2008: health financing in Vietnam. [Google Scholar]
- 8.Giang TL. Health status and accessibility to health facilities of the elderly in Viet Nam. Soc Insur Rev. 2008;7:37–43. [Google Scholar]
- 9.Kowal P, Kahn K, Ng N, Naidoo N, Abdullah S, Bawah A, et al. Ageing and adult health status in eight low-income countries: the INDEPTH WHO-SAGE collaboration. Global Health Action Supplement 2. 2010 doi: 10.3402/gha.v3i0.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chuc NTK, Diwan VK. FilaBavi, a demographic surveillance site, an epidemiological field laboratory in Vietnam. Scand J Public Health. 2003;31:3–7. doi: 10.1080/14034950310015031. [DOI] [PubMed] [Google Scholar]
- 11.INDEPTH Network. Volume 1: population, health, and survival. Ottawa: INDEPTH Network, IDRC; 2002. Population and health in developing countries. [Google Scholar]
- 12.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad K, Jafar T, Chaturvedi N. Self-rated health in Pakistan: results of a national health survey. BMC Public Health. 2005;5:51. doi: 10.1186/1471-2458-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rahman MO, Barsky AJ. Self-reported health among older Bangladeshis: how good a health indicator is it? Gerontologist. 2003;43:856–63. doi: 10.1093/geront/43.6.856. [DOI] [PubMed] [Google Scholar]
- 15.Lim W-Y, Ma S, Heng D, Bhalla V, Chew S. Gender, ethnicity, health behaviour & self-rated health in Singapore. BMC Public Health. 2007;7:184. doi: 10.1186/1471-2458-7-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vlassoff C. Gender inequalities in health in the third world: uncharted ground. Soc Sci Med. 1994;39:1249–59. doi: 10.1016/0277-9536(94)90357-3. [DOI] [PubMed] [Google Scholar]
- 17.Netuveli G, Blane D. Quality of life in older ages. 2008; ldn003. Br Med Bull. 2008;85:113–26. doi: 10.1093/bmb/ldn003. [DOI] [PubMed] [Google Scholar]
- 18.Smith A, Sim J, Scharf T, Phillipson C. Determinants of quality of life amongst older people in deprived neighbourhoods. Ageing Soc. 2004;24:793–814. [Google Scholar]
- 19.Kabir ZN, Tishelman C, Agüero-Torres H, Chowdhury AMR, Winblad B, Höjer B. Gender and rural–urban differences in reported health status by older people in Bangladesh. Arch Gerontol Geriatrics. 2003;37:77–91. doi: 10.1016/s0167-4943(03)00019-0. [DOI] [PubMed] [Google Scholar]
- 20.Srapyan Z, Armenian HK, Petrosyan V. Health-related quality of life and depression among older people in Yerevan, Armenia: a comparative survey of retirement home and household residents aged 65 years old and over. Age Ageing. 2006;35:190–3. doi: 10.1093/ageing/afj039. [DOI] [PubMed] [Google Scholar]
- 21.Mascitelli L, Pezzetta F, Sullivan JL. Why women live longer than men: sex differences in longevity. Gend Med. 2006;3:341. doi: 10.1016/s1550-8579(06)80221-4. [DOI] [PubMed] [Google Scholar]
- 22.Hoang Van M, Dao Lan H, Kim Bao G. Self-reported chronic diseases and associated sociodemographic status and lifestyle risk factors among rural Vietnamese adults. Scand J Public Health. 2008;36:629–34. doi: 10.1177/1403494807086977. [DOI] [PubMed] [Google Scholar]
- 23.Aberg-Yngwe M, Diderichsen F, Whitehead M, Holland P, Burstrom B. The role of income differences in explaining social inequalities in self-rated health in Sweden and Britain. J Epidemiol Community Health. 2001;55:556–61. doi: 10.1136/jech.55.8.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith KV, Goldman N. Socioeconomic differences in health among older adults in Mexico. Soc Sci Med. 2007;65:1372–85. doi: 10.1016/j.socscimed.2007.05.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Access the supplementary material to this article: INDEPTH WHO-SAGE questionnaire (including variants of vignettes), a data dictionary and a password-protected dataset (see Supplementary files under Reading Tools online). To obtain a password for the dataset, please send a request with “SAGE data” as its subject, detailing how you propose to use the data, to global.health@epiph.umu.se