Abstract
Aims: A family history of Huntington disease (HD) or receiving results of HD predictive genetic testing can influence individual well-being, family relationships, and social interactions in positive and negative ways. The aim of this study was to examine benefits reported by people with an HD family history or those who have undergone predictive HD testing, as well as the personal variables associated with perceived benefits. Methods: Seventy-four of 433 people completing the International Response of a Sample Population to HD risk (I-RESPOND-HD) survey reported benefits. Knowledge and understanding was perceived as the most common benefit from participants in both groups. The next most frequent perceived benefits from a family history were connecting with others and achieving life meaning and insights. The next most common perceived benefits from genetic testing were life planning and social support. The least common perceived benefit for both groups was renewed hope and optimism. Older age and spirituality were significantly associated with benefits in both groups. Conclusions: Perceptions of benefit may not be as likely until later years in people with prodromal HD. A developed sense of spirituality is identified as a personal resource associated with the perception of benefit from genetic testing for HD. Associations among spirituality, perceived benefits, and other indicators of personal and family well-being may be useful in genetic counseling and health care of people with prodromal HD.
Introduction
Huntington disease (HD) is an autosomal dominant neurodegenerative condition. A clinical diagnosis is typically made when motor symptoms appear. However, subtle changes in cognition, behavior, and motor control are detectable years before the clinical diagnosis (Paulsen, 2010). Discrepancies in self-ratings with companion ratings of frontal lobe behaviors in persons with an expansion in the gene for HD, but who have not received a clinical diagnosis (prodromal HD), suggest that self-awareness may be decreased in those closest to HD diagnosis (Duff et al., 2010). However, people with prodromal HD report perceiving negative experiences and may make decisions about their day-to-day lives based in part on these perceptions. After the gene mutation for HD was identified and predictive testing was available to at-risk persons, reports described a range of both negative and positive consequences of knowing one's family history or one's gene mutation status at a time when the person was not experiencing symptoms of HD. Little is known regarding factors associated with perceptions of positive consequences, or benefit.
Negative consequences
Much attention has focused on potential negative consequences of genetic testing that include risk for genetic discrimination. Although perceptions of discrimination regarding insurance and social relationship (Penziner et al., 2008; Erwin et al., 2010) are shared across recent reports, other arenas in which discrimination is perceived to occur include health insurance (Oster et al., 2008), family (Bombard et al., 2009), and life insurance access (Barlow-Stewart et al., 2009). Other negative consequences may include depression, difficulties with transitions such as starting new relationships, planning a family, or coping with favorable test results (DudokdeWit et al., 1998; Tibben, 2007; Gargiulo et al., 2009). Those with specific personal characteristics, unspecified test motivation, or limited social networks may be at higher risk for long-term distress (Decruyenaere et al., 2003; Tibben, 2007; Licklederer et al., 2008; Taylor, 2005). The potential for suicide ideation or behavior has been closely monitored. Although HD may be considered as a risk factor for suicide, this risk may not be elevated in research study samples of people with or at risk for HD (Fiedorowicz et al., 2010).
Those with a family history of HD who were raised by a parent with HD may be at increased risk for difficulty in establishing close emotional bonds in parent–child relationships (Van der Meer et al., 2006), and some people rate having a parent with HD as being difficult or as splitting the family apart (Vamos et al., 2007).
Positive consequences
Benefits of an HD family history or predictive test have also been reported, with 22.4% of persons in the International Response of a Sample Population to HD risk (I-RESPOND-HD) study reporting one or more benefits from knowing their family history or their positive test results (Erwin et al., 2010). People who decide to have predictive testing may be less likely to question their abilities to cope if problems arise (Codori et al., 1994; Meiser and Dunn, 2000). Benefits of genetic testing include knowing one's genetic status, having an increased appreciation for the present, having information for reproductive decisions, and acquiring significant life knowledge (Bloch et al., 1992; Decruyenaere et al., 2004, 2007; Taylor, 2004). After completing genetic testing, some people with positive or negative results report starting new relationships, and some who are in a partner relationship report increased communication and support from partners (Decruyenaere et al., 2004). Some adults who grew up with a parent affected with HD report that HD brought the family closer together, and they feel good about their families (Vamos et al., 2007). One report of Australian youth who completed predictive testing for HD noted that benefits included not only knowledge and relief from uncertainty, but also positive effects on family and friend relationships, feeling empowerment, and a sense of clarity about what was important to the participants in their lives (Duncan et al., 2008).
Personal factors and consequences
Multiple personal factors influence psychological outcomes of genetic testing. Individuals who avoid HD-related situations and thoughts may find avoidance to be a useful strategy that does not interfere with making health-related decisions such as reproductive choices (Decruyenaere et al., 2003). However, a passive avoidant coping strategy is one of several factors associated with poorer adjustment (Pakenham et al., 2004). Contextual factors, including expectations for ability to cope with results and prior experiences within the HD family, likely influence perceptions of negative and positive experiences after receiving testing results (Taylor, 2004). Although research is not as extensive regarding benefits, both personal factors and life experiences are believed to influence perceptions of benefits from having a family history of HD or having a genetic test in people who are at risk but are not found to have HD.
The data in this study are from the I-RESPOND-HD study in which participants were asked to identify benefits as well as negative experiences in questions throughout the survey. Research questions were (1) what benefits are reported by people with an HD family history or by people who have completed HD predictive DNA testing and (2) what personal characteristics are associated with reported benefits from an HD family history or predictive DNA testing.
Materials and Methods
The complete description of the I-RESPOND-HD study is reported elsewhere (Erwin et al., 2010; Williams et al., 2010). In brief, the aim of I-RESPOND-HD was to examine elements of genetic stigma and discrimination among an at risk, clinically undiagnosed HD population. The study included the development of a paper-and-pencil survey geared specifically for assessing perceptions of discrimination, stigma, and benefits reported by respondents.
Sample
The I-RESPOND-HD sample included a portion of respondents who had previously undergone predictive DNA testing to identify a CAG repeat expansion in HTT, the gene that encodes huntingtin (OMIM, 2009), and did not have a clinical diagnosis of HD; such participants were recruited through prior enrollment in the PREDICT-HD study (Paulsen et al., 2006). A second portion of the sample was individuals who were at risk for HD but had not undergone predictive testing; such participants were recruited through prior enrollment in the PHAROS study (Huntington Study Group PHAROS Investigators, 2006). The remaining respondents were people attending an annual meeting of the Huntington Disease Society of America and who met the inclusion criteria for either the PREDICT-HD or PHAROS studies.
Design
The study used a cross-sectional, descriptive, mixed-method survey design with closed- and open-ended response formats addressing multiple topics in context to HD, including perceptions of genetic discrimination based on family history, perceptions of genetic discrimination based on genetic test results, employment, insurance, and legal issues. Additionally, there included a section for collecting demographic information.
Instruments
Among the multiple sections of the I-RESPOND-HD survey, two items specifically addressed benefits. These items were completed by respondents who first reported discrimination experiences based on their family history of HD or their genetic test results. The first question (C7) asked, “Were there any incidents where you felt you benefited from your family history of HD?” and the second (D10) asked, “Were there any incidents where you felt you benefited because of your genetic test results?” Each question offered a yes/no response as well as a follow-up request for a narrative description of the incident.
Additionally, seven standardized measures of personal factors were given to all participants, either along with the survey or during the parent study visit: the Medical Outcomes Study Short Form Version 2 (SF-36v2) (SF-36 vsHealth Survey, 2000), the Rydell-Rosen Ambiguity Tolerance Scale (AT-20) (Rydell and Rosen, 1966), the Spiritual Well-Being Scale (SWBS) (Bufford et al., 1991; Ellison, 1983), the Miller Behavioral Style Scale (MBSS) (Miller, 1987), the Life Orientation Test-Revised (LOT-R) (Scheier et al., 1994), the Impact of Events Scale-Revised (IES-R) (Horowitz et al., 1979), and the Beck Depression Inventory II (BDI-II) (Beck et al., 1996). These measures were selected to characterize the at-risk cohort who had undergone genetic testing, to enhance understanding of their behaviors, perceptions, and experiences, and to allow comparison with the cohort of at-risk HD participants who had chosen not to undergo genetic testing.
The SF-36v2 contains scales on physical functioning, role limitation, bodily pain, vitality, social functioning, mental health, and general health (Ware and Sherbourne, 1992; McHorney et al., 1993). The AT-20 is a measure of level of comfort with ambiguous situations (MacDonald, 1970). The SWBS is intended to assess a person's self-reported overall SWB (Paloutzian and Park, 2005) and contains a subscale on religious well-being along the vertical dimension of spirituality, as well as a subscale on existential well-being, addressing factors such as life purpose, satisfaction, and meaningful relationships with others (Vollman et al., 2009). The MBSS is intended to identify coping styles by summing the monitoring and blunting responses to four hypothetical threatening situations; monitoring refers to sensory vigilance and active information seeking, while blunting refers to psychologically absenting oneself from an unpleasant or dangerous situation (Bijttebier et al., 2001). The LOT-R is a measure of generalized optimism that measures expectancies for positive versus negative outcomes and yields an overall optimism score (Scheier et al., 1994). The IES-R documents participants' perceived stress responses after the significant event of genetic testing or learning of their family history of HD and permits comparison of the impact of different kinds of life events and individual differences in response to these events (Horowitz et al., 1993; Sundin and Horowitz, 2002). The BDI-II is a 21-item rating scale that provides a quantitative assessment of the intensity of depression (Beck et al., 1996).
Ethical considerations
The study was approved by The University of Iowa IRB and at the IRB (or equivalent overseeing body) at each participating institution. Participants provided consent at either parent study visits or via post.
Research procedure
People aged 18 or older who had enrolled in PREDICT-HD or PHAROS, or who had attended the 2007 annual HDSA meeting and fit the inclusion criteria were asked to participate in the study. Those with evidence of unstable medical or psychiatric illness, with a history of severe learning disability, mental retardation, or other CNS condition, or taking antipsychotic medications did not meet inclusion criteria. The survey was administered at a scheduled site visit or at the HDSA annual conference and returned to the investigators upon completion of the survey packet or by return mail.
Data analysis
Narrative comments for questions asking the participant to describe any incidents where the person benefited from their family history or genetic test results were coded according to procedures for descriptive qualitative analysis (Knafl and Webster, 1988; Sandelowski, 2000). All data were entered into the NVivo (2008) software program for data management. The data were quantified to reduce them in a manner to optimize descriptive, interpretive, and internal validity (Maxwell, 1992; Sandelowski et al., 2009), and they focused on the range of experiences of reported benefits. Three members of the research team sorted statements that were similar into distinct categories. The process continued until there was 100% agreement. The remainder of the research team validated the analysis. The purpose of the qualitative data analysis was to produce a comprehensive summary of benefits statements in everyday language (Sandelowski, 2000).
For categorical variables, chi-square tests were used to examine proportional differences between the group reporting benefit from a family history of HD or predictive genetic testing and the group reporting no benefit to the same. Mean differences between groups were compared using independent t-tests. A multivariate logistic regression model was used to evaluate the association between report of benefit and selected covariates.
Results
Sample description
Of the 74 people who gave responses to either question C7, “Were there any incidents where you felt you benefited from your family history of HD?” or D10, “Were there any incidents where you felt you benefited because of your genetic test results?” there were 43 “yes” responses to the question regarding benefit from family history, and 51 “yes” responses to the question regarding benefit from genetic testing (Table 1). There were no statistically significant differences on demographic characteristics in the group who did and the group who did not provide an answer to either question.
Table 1.
Demographics for Individuals Reporting Benefit
| Gender | |
| Male | 20 (27%) |
| Female | 54 (73%) |
| Children | |
| 0–2 | 30 (55%) |
| >2 | 25 (45%) |
| Age | 46.90 (SD = 10.41) |
| Marital | |
| Married | 50 (70%) |
| Never married | 11 (15%) |
| Not married now | 10 (14%) |
| Work | |
| Not working | 16 (23%) |
| Retired | 7 (10%) |
| Working | 48 (68%) |
| Country | |
| Australia | 23 (31%) |
| Canada | 5 (7%) |
| United States | 46 (62%) |
| Number of missing observations | |
| Marital | 3 |
| Children | 19 |
| Work | 3 |
| Age | 1 |
Perceived benefits
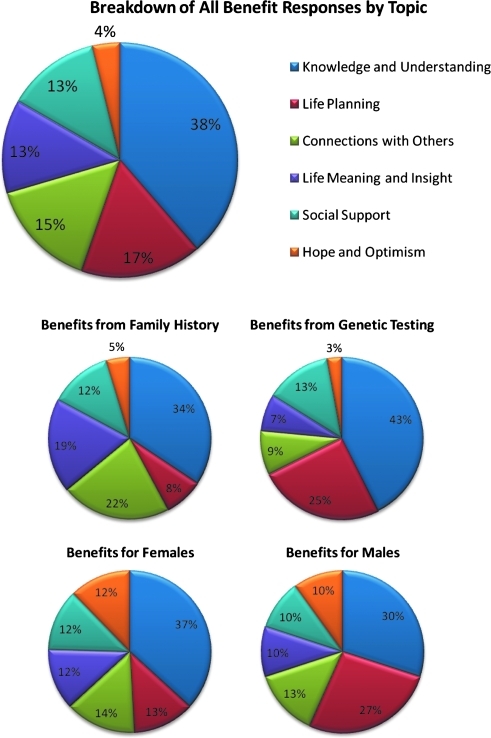
Participants who had a positive family history and had completed genetic testing could provide answers to both questions, and participants could provide multiple responses. Sixty-four benefits were reported by people with a positive family history, and 68 benefits were reported by people who had completed genetic testing with either a positive or a negative test result. Through procedures of content analyses, perceived benefits from all responses were grouped into six major categories (Fig. 1). Statements by individuals illustrating each category are identified according to family history (FH) or genetic testing (GT), and according to female (F) or male (M) gender.
FIG. 1.
Breakdown of all benefit responses by topic.
Knowledge and understanding
The most common benefit by all participants was knowledge and understanding. This category reflects statements of perceived benefits of information for the person as well as for others. This category includes knowledge and life knowledge (Bloch et al., 1992; Decruyenaere et al., 2004; Taylor, 2004), as well as relief from uncertainty identified in multiple studies as a motivation for seeking predictive testing (Tibben, 2007). In this sample, statements were not specific to relief from uncertainty, but may have reflected this emotion. Respondents identified that participation in research was a benefit. To our knowledge, this has not been reported as a perceived benefit when having an HD family history or completing genetic testing. One participant stated, “I am hopeful of a cure and I always signed up for all study groups I qualified for as my way of fighting HD” (1FH,F). The second component of this category was being able to advocate or educate oneself or others. One respondent stated:
“Yes, in everyday interaction, I can pass on something tangible to others about my situation. For me to know that they understand that I've seen health professionals and been through a predictive program is useful because it gives me some confirmation that they have understood, or are in a position to understand that this illness and the situation in general are serious enough to warrant such attention.” (2GT,M)
A third component of this category was having an explanation for symptoms in their relatives or themselves. For example, “I now understand that my mother's life was difficult because of her illness and her aggression towards family members (especially toward myself ) was not an expression of her true self, but the illness overtaking her personality (mood disorder)” (3FH,F). In the fourth component of this category, respondents described relief. One participant stated, “Peace of mind for me and my wife” (4GT,M).
Participants with a family history or who had completed genetic testing provided statements in the remaining five categories. However, the relative frequency of responses for these categories was not in the same order for each group. For respondents with a Family History, the next most common category was Connections with others.
Connections with others
This category refers to those statements that included perceptions of benefits that involved family, community, or other relationships. This category may be similar to reports of bringing the family closer together (Vamos et al., 2007), and increased satisfaction with relationships (Decruyenaere et al., 2004). The first component of this category was connections within the family. For example, “I feel lucky to have so much support in my family (spouse, sister, husband family, in-laws, my kids). They are all out there helping me through the good and bad days” (5FH,F). The second component was connections with community. One person reported: “All of the people through this process to me have been very supportive. I have been in contact with many folks who understand Huntington and that gives me comfort” (6GT,F). Perceived benefits were reported with regard to the connections with others in the workplace. For example, “My present employer has given me a lot of extra time to get work-related issues under control. My staff has also made it clear what situation to ask for help on and which situations I can do by myself” (7FH,M).
Life meaning and insight
The third most common category of benefits reported by those with a family history of HD was life meaning and insight. This category contains a review of the meaning of one's life. A benefit reported in one study of youth who had undergone genetic testing reported a sense of clarity about what was important (Duncan et al., 2008), which may be related to the benefits expressed by participants in this category. The first component of this category is life meaning. One participant reported, “I feel I live my life more deliberately and with a greater sense of purpose that I might otherwise have” (8FH,F). The second component was development of one's inner life. This may be similar to the report of having an increased appreciation for the present (Bloch et al., 1992). An example of these statements is, “I feel that having a history of HD has made me stronger, more compassionate, understanding, and tolerant of different people and circumstances” (9FH,F).
Two other major categories were shared with those who had completed genetic testing. These categories were the second and third most commonly endorsed categories by those who had completed genetic testing.
Life planning
This category pertains to planning that was important to the person and his/her family, and included reproduction, work or retirement, finances for family after the person has died, and planning on behalf of their children. This category may overlap with benefits previously reported that include reproductive decisions (Decruyenaere et al., 2007) as well as more general comments in the literature related to significant life knowledge. One example in this category was regarding reproduction: “My husband and I decided not to have children” (10GT,F). Another participant described plans for retirement by stating, “I was allowed to retire earlier than I usually would have” (11FH.M). Some statements were not specific to any life event. For example, “I obtained long-term care, disability, health, life insurance years before I might have ordinarily” (12FH,F).
Receiving social support
The third most frequent comments were in the category of receiving social support. To our knowledge, this category has not been addressed in prior reports. The items in this category are statements of perceived benefits when something the person desired could be attained by those without a family history or genetic test for HD, and was also obtained by the individual. An example is, “Once I got my results, I informed my insurance provider and then they removed the loading on my premium, which was a major benefit” (13GT,M). Another person reported: “When I graduated from high school, I received a scholarship for college. I think, I was picked due to the fact that my mother had Huntington disease” (14FH,F).
Renewed hope and optimism
The sixth major category contains statements of perceived benefits from both those with a family history and those who have completed genetic testing. This category contained the fewest comments. Statements in this category reflect personal views about one's life. One participant reported:
“Knowing the family history, to me, was always a source of great liberation and insight, as opposed to trepidation and fear. Although there are no solitary incidents, the overall psychological effects of knowing the family history of HD have been positive. I have benefited courtesy of liberation from fear.” (15FH,M)
To summarize the categories of benefit, participants who had a family history or had also undergone genetic testing provided descriptions of perceived benefits in all six major categories. Among those who had completed genetic testing, some identified the outcome of the test, and benefits were cited by those who indicated a positive or a negative test result. Some benefits mirrored previously reported benefits, while the perceived benefit of participating in research and in receiving social support, to our knowledge, have not been reported previously.
Personal factors associated with benefits
The second research question examined if personal characteristics were associated with reported benefits from an HD family history or predictive DNA testing. Demographic information for the individuals who noted a benefit from either family history or genetic test appears in Table 1. Individuals who reported a benefit tended to be female (74%), had between 0 and 2 children (55%), and were married (70%). Further, most of the individuals who reported a benefit were working individuals (68%) in the United States (62%) with an average age of ∼47 years (and a standard deviation of about 10 years).
The results from the statistical analyses are provided in Table 2, presenting results of t-tests for the continuous variables. The only variables on which the benefit group and the nonbenefit group significantly differed on were older age (both family history and genetic test), increased SWB (both family history and genetic test), increased SWB religious (both family history and genetic test), and increased SWB existential (genetic test). For all other variables, there was not sufficient evidence to claim that the benefit group and the nonbenefit group differed in the population.
Table 2.
Comparison of Perceived Benefits from Huntington Disease Family History and from Huntington Disease Genetic Testing and Demographic Characteristics for Continuous Variables
| |
Family history |
Gene test |
||
|---|---|---|---|---|
| t-Value | p-Value | t-Value | p-Value | |
| Age | −2.08 | 0.039 | −2.8800 | 0.005 |
| SWB | −2.29 | 0.024 | −2.7600 | 0.007 |
| SWB religious | −1.99 | 0.049 | −2.1200 | 0.036 |
| SWB existential | −1.73 | 0.087 | −2.3500 | 0.021 |
SWB, spiritual well-being.
The logistic regression analyses indicate that both older age and higher spirituality serve as statistically significant predictors of benefit status (defined as benefiting either from family history or from genetic test) (Table 3). Both these variables are significant predictors in a one-variable regression model (i.e., only that particular variable is used to predict benefit status), as noted under the “Univariate” column. Further, both these variables yield statistically significant prediction power when they are added last in a hierarchical regression model (i.e., both age and spirituality contribute significant prediction power after the other variable is already used as a predictor), as noted under the “Multivariate” column. The gender variable did not yield statistically significant prediction power, however, either in the one-variable regression model or in the hierarchical regression model.
Table 3.
Logistic Regression Analysis
| |
Family history |
Gene test |
||||||
|---|---|---|---|---|---|---|---|---|
| |
Univariate |
Multivariate |
Univariate |
Multivariate |
||||
| Odds ratio | p-Value | Odds ratio | p-Value | Odds ratio | p-Value | Odds ratio | p-Value | |
| Age | 1.036 | 0.042 | 1.050 | 0.026 | 1.052 | 0.007 | 1.062 | 0.008 |
| Gender | 1.718 | 0.190 | 1.563 | 0.366 | 0.848 | 0.685 | 0.802 | 0.656 |
| Spiritual | 1.024 | 0.026 | 1.024 | 0.035 | 1.030 | 0.009 | 1.034 | 0.006 |
Discussion
This article reports benefits as identified by people who participated in an international survey on perceptions of genetic discrimination. This study added new findings of benefits, beyond family closeness (Vamos et al., 2007), from those who had not undergone testing at the time of enrollment in the parent study, but who had a family history of HD. Those who had completed genetic testing endorsed benefits previously reported, including relief from uncertainty of one's gene status, appreciation for the present, acquiring significant life knowledge, making future plans, and reproductive decisions (Bloch et al., 1992; Decruyenaere et al., 2004, 2007; Taylor, 2004; Duncan et al., 2008). The benefits included topics that are similar to those reported from qualitative descriptive studies. This study identified two new themes, participation in research and support from others, that the authors believe have not been reported previously. Personal characteristics of older age and increased spirituality were associated with a greater likelihood of reporting having derived some benefits from having a family history of HD or having completed predictive genetic testing.
The categories for what benefits were perceived were not predetermined, but rather were identified from topics provided by the participants. Although this does not yet allow for generalization to the larger HD population, data from informants, rather than forced choice predetermined categories, add insights into the points of view of persons in this population (Willgerodt, 2003). Findings from this study contribute a wider range of benefits perceived by people at risk for HD or who have received a positive HD test result than have previously been reported. These new categories may be useful in future development of paper-and-pencil measures of benefits of HD family history, or knowledge of risk for HD.
The report of perceived benefit from participating in research, and the receipt of social support are novel to this study. The examples of social support covered a wide range of social interactions, some related to receiving disability benefits or qualifying for assisted living. Others described involvement with the courts or insurance providers. All had a consistent theme of receiving services or opportunities due to illness in family members with HD or their own at-risk status, with a positive outcome. Increased understanding about HD by those who are at risk, such as using information on HD organization Web sites, as well as social services providers may have contributed to these perceived beneficial experiences.
The benefit of participation in research has not been reported previously in this population. Applied to individuals involved in HD research, this suggests that individuals facing this devastating disorder can find optimism and a renewed sense of contribution through these activities and connections. The novel finding that participation in research in an observational study is perceived as good in itself has important implications for the inclusion of individuals in long-term research.
The finding that increased age was associated with a perception of benefits suggests several explanations. The spiritual benefits of an increased sense of connection to others, life meaning and insight, are more perceived by individuals of greater age and by those who self-reported a stronger sense of SWB. More attention to this potential for existential benefit may enhance our understanding of the reasons why individuals continue participation in long-term research studies. The life-span theory of control (Heckhausen and Schulz, 1995) addresses life stages and coping with life events for which people have no control, such as health risks where one cannot change the circumstances to fit the needs of the person. This theory posits that when faced with uncontrollable events, people may alter their response to these circumstances. One of the ways in which people in the present study reported deriving benefit was from deriving meaning in their lives, an activity that is sometimes associated with older age (Heckhausen and Schulz, 1995). Aging and spirituality may interact as people assess the importance of their inner life, and that spirituality may be a capacity that continues to develop regardless of other effects of aging (Atchley, 1999).
Narratives of spirituality often reflect the underlying growth of understanding and compassion for other persons in the world. The development of spirituality requires that one not turn away from unpleasant truths. In the context of health and illness, spirituality may be thought of as that which pertains to those things that give transcendent meaning and purpose to one's life and has clinical relevance (Post et al., 2000). Spirituality, however it is defined, is an important aspect of the care of the whole person and can give shape and dimension to individual experiences in the clinic and beyond.
The relationship of spirituality to health and well-being has begun to be explored in HD and other clinical situations. Personal factors associated with spirituality include optimism, female gender, and personality traits that may be protective regarding health such as conscientiousness, agreeableness, and extraversion (Labbé and Forbes, 2010). Spirituality was found to mediate the relationship between religiosity and the development of depression in people who have developed prostate cancer (Nelson et al., 2009). Daily spiritual experiences, but not religious attendance, were found to be related to greater performance of constructive health behaviors, that is, medication adherence and after dietary, alcohol usage, and exercise advice in younger adult cancer survivors (Park et al., 2009). The role of spiritual involvement, beliefs, and coping has been examined with regard to family caregivers of people with HD in the late stages in which spiritual involvement and beliefs were found to be positively correlated with life satisfaction and self-related health, and negatively associated with depressive symptoms in a sample of U.S. caregivers (Roscoe et al., 2009).
Little research has been done on the interplay of spirituality and the loss of cognitive ability or dementia that may occur in the later stages of HD. On the basis of interviews with residents of a locked dementia ward, Atchley (2009) makes the argument that if spirituality is a type of beingness, “as long as there is the possibility of spirituality, and as long as there is spirituality, there is a right to be considered a person. In fact, the experience of beingness may be the last experience to be lost to dementia.” This may have significance for the HD community because those who report a significant spiritual life may be more likely not only to experience benefit in daily living after a genetic test, but they may also be more likely to retain a sense of beingness, or spirituality into later stages of dementia. This observation may require additional study of individuals with severe cognitive decline.
The findings from this study have several limitations. Data were obtained from written comments and there was no opportunity to request clarification or elaboration of statements. A second limitation is that the sample is comprised of those who participated in the PREDICT or PHAROS research studies, and may represent a bias of people who enroll in research. There is also the potential for diminished self-awareness in persons who are closer to the time of HD diagnosis. The nearness to diagnosis was not calculated in this sample, and thus various levels of capacity for self-awareness are unknown in the cohort reporting perceived benefits.
Conclusions
Those who have undergone genetic testing or have a family history of HD do not present a special case of the human search for meaning in illness, but their experience provides a window into the benefits that can be ascribed to the process of clarifying those things that are important and give meaning to life. From the narrative comments provided by these respondents, it appears that the relationship between self-reported benefits and SWB may represent an overlap or merging of the common themes of seeking clarification of meaning in one's life and the importance of relationships.
The individuals who found benefits in their life, in spite of the perception of genetic discrimination, teach others who will come after them that those who find meaning in the midst of the burden of a certain degenerative condition can turn suffering into a personal triumph if they choose an attitude that seeks to understand what gives meaning to their lives. Those who related benefits seemed to have sensed that they have something to offer the world, whether participation in research and the advancement of knowledge, or in teaching others.
Recommendations
The benefits reported by these participants reveal a way toward living positively with the risk of HD. Patients and clinicians can benefit from these reports by making them more widely known. Clinicians who work with people at risk for HD may find these reports of benefit useful in understanding the suffering and despair felt by some individuals and the hope and optimism felt by others. Examples of people in this study who reframed a past experience or focused on what a person can contribute to others may provide useful illustrations in counseling situations. The reported beneficial consequences of these individual approaches suggest that more attention can be paid to the existential benefits of participation in research. Although there is no direct medical benefit reported here, individuals derived psychological benefit from participation in research. Some reported a sense of efficacy in making a difference in the world, connections to others similarly situated, or simply a deepened sense of understanding. These benefits are little understood and merit further investigation regarding how these benefits may offer an important sense of meaning to individuals faced with the risk of HD.
Acknowledgments
The study was supported by the National Human Genome Institute (R01 HG003330), the National Institute of Neurological Disorders and Stroke (NS40068), and CHDI Foundation, Inc. The authors thank the PREDICT-HD sites, the study participants, and the National Research Roster for Huntington Disease Patients and Families.
Disclosure Statement
No competing financial interests exist for all authors.
References
- Atchley RC. The Johns Hopkins University Press; Baltimore: 1999. Continuity and Adaptation in Aging: Creating Positive Experiences. [Google Scholar]
- Atchley RC. Spirituality and Aging. The Johns Hopkins University Press; Baltimore: 2009. [Google Scholar]
- Barlow-Stewart K. Taylor SD. Treloar SA, et al. Verification of consumers' experiences and perceptions of genetic discrimination and its impact on utilization of genetic testing. Genet Med. 2009;11:193–201. doi: 10.1097/GIM.0b013e318194ee75. [DOI] [PubMed] [Google Scholar]
- Beck AT. Steer RA. Brown GK. Beck Depression Inventory-II: Manual. The Psychological Corporation; San Antionio: 1996. [Google Scholar]
- Bijttebier P. Vertommen H. Vander Steen G. Assessment of cognitive coping styles: a closer look at situation-response inventories. Clin Psychol Rev. 2001;21:85–104. doi: 10.1016/s0272-7358(99)00041-0. [DOI] [PubMed] [Google Scholar]
- Bloch M. Adam S. Wiggins S, et al. Predictive testing for Huntington disease in Canada: the experience of those receiving an increased risk. Am J Med Genet. 1992;42:499–507. doi: 10.1002/ajmg.1320420416. [DOI] [PubMed] [Google Scholar]
- Bombard Y. Veenstra G. Friedman JM, et al. Perceptions of genetic discrimination among people at risk for Huntington's disease: a cross sectional survey. BMJ. 2009;338:b2175. doi: 10.1136/bmj.b2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufford RK. Paloutzian RF. Ellison CW. Norms for the spiritual well-being scale. J Psychol Theol. 1991;19:56–70. [Google Scholar]
- Codori AM. Hanson R. Brandt J. Self-selection in predictive testing for Huntington's disease. Am J Med Genet. 1994;54:167–173. doi: 10.1002/ajmg.1320540303. [DOI] [PubMed] [Google Scholar]
- Decruyenaere M. Ever-Kiebooms G. Boogaerts A, et al. The complexity of reproductive decision-making in asymptomatic carriers of the Huntington mutation. Eur J Hum Genet. 2007;15:453–462. doi: 10.1038/sj.ejhg.5201774. [DOI] [PubMed] [Google Scholar]
- Decruyenaere M. Evers-Kiebooms G. Closstermans T, et al. Psychological distress in the 5-year period after predictive testing for Huntington's disease. Eur J Hum Genet. 2003;11:30–38. doi: 10.1038/sj.ejhg.5200913. [DOI] [PubMed] [Google Scholar]
- Decruyenaere M. Evers-Kiebooms G. Cloostermans T, et al. Predictive testing for Huntington's disease: relationship with partners after testing. Clin Genet. 2004;65:24–31. doi: 10.1111/j..2004.00168.x. [DOI] [PubMed] [Google Scholar]
- DudokdeWit AC. Tibben A. Duivenvooden HJ, et al. Predicting adaptation to presymptomatic DNA testing for late onset disorders: who will experience distress? J Med Genet. 1998;35:745–754. doi: 10.1136/jmg.35.9.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff K. Paulsen JS. Beglinger L, et al. “Frontal” behaviors before the diagnosis Huntington's disease and its relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22:196–207. doi: 10.1176/appi.neuropsych.22.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan RE. Gillam L. Savulescu J, et al. “You're one of us now”: young people describe their experiences of predictive genetic testing for Huntington disease (HD) and familial adenomatous polyposis (FAP) Am J Med Genet C Semin Med Genet. 2008;148C:47–55. doi: 10.1002/ajmg.c.30158. [DOI] [PubMed] [Google Scholar]
- Ellison CW. Spiritual well-being: conceptualization and measurement. J Psychol Theol. 1983;11:330–338. [Google Scholar]
- Erwin C. Williams JK. Juhl A, et al. Perception, experience and response to genetic discrimination in Huntington disease: the International RESPOND-HD study. Am J Med Genet B. 2010;153B:1081–1093. doi: 10.1002/ajmg.b.31079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiedorowicz JG. Ruggle A. Paulsen JS. Suicide Risk Associated with Medical Disorders (Tentative Title) In: Berman L, editor; Pompili M, editor. Suicide and Huntington disease. American Association of Suicidology; Washington, DC: 2010. (In press). [Google Scholar]
- Gargiulo M. Lejeune S. Tanguy ML, et al. Long-term outcome of presymptomatic testing in Huntington disease. Eur J Hum Genet. 2009;17:165–171. doi: 10.1038/ejhg.2008.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckhausen J. Schulz R. A life-span theory of control. Psychol Rev. 1995;102:284–304. doi: 10.1037/0033-295x.102.2.284. [DOI] [PubMed] [Google Scholar]
- Horowitz M. Wilner N. Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med. 1979;41:209–217. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ. Field NP. Classen CC. Stress response syndromes and their treatment. In: Goldberger L, editor; Breznitz S, editor. Handbook of Stress: Theoretical and Clinical Aspects. The Free Press; New York: 1993. pp. 757–774. [Google Scholar]
- Huntington Study Group PHAROS Investigators. At risk for Huntington disease: the PHAROS (Prospective Huntington At Risk Observational Study) cohort enrolled. Arch Neurol. 2006;63:991–996. doi: 10.1001/archneur.63.7.991. [DOI] [PubMed] [Google Scholar]
- Knafl KA. Webster DC. Managing and analyzing qualitative data: a description of tasks, techniques, and materials. West J Nurs Res. 1988;10:195–218. doi: 10.1177/019394598801000207. [DOI] [PubMed] [Google Scholar]
- Labbé EE. Fobes A. Evaluating the interplay between spirituality, personality and stress. Appl Psychopahysiol Biofeedback. 2010;35:141–146. doi: 10.1007/s10484-009-9119-9. [DOI] [PubMed] [Google Scholar]
- Licklederer C. Wolff G. Barth J. Mental health and quality of life after genetic testing for Huntington disease: a long-term effect study in Germany. Am J Med Genet A. 2008;146A:2078–2085. doi: 10.1002/ajmg.a.32423. [DOI] [PubMed] [Google Scholar]
- MacDonald AP. Revised scale for ambiguity tolerance: reliability and validity. Psychol Rep. 1970;26:791–798. [Google Scholar]
- Maxwell JA. Understanding and validity in qualitative research. Harv Educ Rev. 1992;62:279–300. [Google Scholar]
- McHorney CA. Ware JE., Jr. Raczek AE. The MOS 36-item short-form health survey (SF-36): II Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Meiser B. Dunn S. Psychological impact of genetic testing for Huntington's disease: an update of the literature. J Neurol Neurosurg Psychiatry. 2000;69:574–578. doi: 10.1136/jnnp.69.5.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller SM. Monitoring and blunting: validation of a questionnaire to assess styles of information seeking under threat. J Pers Soc Psychol. 1987;52:345–353. doi: 10.1037//0022-3514.52.2.345. [DOI] [PubMed] [Google Scholar]
- Nelson C. Jacobson CM. Weinberger MI, et al. The role of spirituality in the relationship between religiosity and depression in prostate cancer patients. Ann Behav Med. 2009;38:105–114. doi: 10.1007/s12160-009-9139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OMIM. Huntington disease. 2009. www.ncbi.nlm.nih.gov/omim/ [Sep 2;2009 ]. www.ncbi.nlm.nih.gov/omim/
- Oster E. Dorsey ER. Bausch J, et al. Fear of health insurance loss among individuals at risk for Huntington disease. Am J Med Genet A. 2008;146A:2070–2077. doi: 10.1002/ajmg.a.32422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakenham KI. Goodwin VA. MacMillan JC. Adaptation to being at-risk for Huntington's disease and the availability of genetic testing: application of a stress and coping model. Psychol Health Med. 2004;9:380–397. [Google Scholar]
- Paloutzian RF. Park CL. Guilford Press; New York: 2005. Handbook of the Psychology of Religion and Spirituality. [Google Scholar]
- Park CL. Edmondson D. Hale-Smith A. Blank TO. Religiousness/spirituality and health behaviors in younger adult cancer survivors: does faith promote a healthier lifestyle? J Behav Med. 2009;32:582–591. doi: 10.1007/s10865-009-9223-6. [DOI] [PubMed] [Google Scholar]
- Paulsen JS. Early detection of Huntington's disease. Future Neurol. 2010;5:85–104. doi: 10.2217/fnl.09.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulsen JS. Hayden M. Stout JC, et al. Preparing for preventive clinical trials: the Predict-HD study. Arch Neurol. 2006;63:883–890. doi: 10.1001/archneur.63.6.883. [DOI] [PubMed] [Google Scholar]
- Penziner E. Williams JK. Erwin C, et al. Perceptions of discrimination among persons who have undergone predictive testing for Huntington's disease. Am J Med Genet. 2008;147B:320–325. doi: 10.1002/ajmg.b.30600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post SG. Puchalski CM. Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med. 2000;132:578–583. doi: 10.7326/0003-4819-132-7-200004040-00010. [DOI] [PubMed] [Google Scholar]
- Roscoe LA. Corsentino E. Watkins S, et al. Well-being of family caregivers of persons with late-stage Huntington's disease: lessons in stress and coping. Health Commun. 2009;24:239–248. doi: 10.1080/10410230902804133. [DOI] [PubMed] [Google Scholar]
- Rydell ST. Rosen E. Measurement and some correlates of need-cognition. Psychol Rep. 1966;19:139–165. doi: 10.2466/pr0.1966.19.1.139. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Voils CI. Knafl G. On Quantitizing. J Mix Methods Res. 2009;3:208–222. doi: 10.1177/1558689809334210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier MF. Carver CS. Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Sundin EC. Horowitz MJ. Impact of event scale: psychometric properties. Br J Psychiatry. 2002;180:205–209. doi: 10.1192/bjp.180.3.205. [DOI] [PubMed] [Google Scholar]
- Taylor SD. Gender differences in attitudes among those at risk for Huntington's disease. Genet Test. 2005;9:152–157. doi: 10.1089/gte.2005.9.152. [DOI] [PubMed] [Google Scholar]
- Taylor SD. Predictive genetic test decisions for Huntington's disease: context, appraisal and new moral imperatives. Soc Sci Med. 2004;58:137–149. doi: 10.1016/s0277-9536(03)00155-2. [DOI] [PubMed] [Google Scholar]
- Tibben A. Predictive testing for Huntington's disease. Brain Res Bull. 2007;72:165–171. doi: 10.1016/j.brainresbull.2006.10.023. [DOI] [PubMed] [Google Scholar]
- Vamos M. Hambridge J. Edwards M, et al. The impact of Huntington's disease on family life. Psychosomatics. 2007;48:400–404. doi: 10.1176/appi.psy.48.5.400. [DOI] [PubMed] [Google Scholar]
- Van der Meer L. Timman R. Trijsburg W, et al. Attachment in families with Huntington's disease: a paradigm in clinical genetics. Patient Educ Couns. 2006;63:246–254. doi: 10.1016/j.pec.2005.11.019. [DOI] [PubMed] [Google Scholar]
- Vollman MW. LaMontagne LL. Wallston KA. Existential well-being predicts perceived control in adults with heart failure. Appl Nurs Res. 2009;22:198–203. doi: 10.1016/j.apnr.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Ware JE., Jr. Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Williams JK. Erwin C. Juhl A, et al. In their own words: reports of stigma and genetic discrimination by people at-risk for Huntington disease in the International RESPOND-HD study. Am J Med Genet B. 2010 doi: 10.1002/ajmg.b.31080. Apr 5 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willgerodt MA. Using focus groups to develop culturally relevant instruments. West J Nurs Res. 2003;25:798–814. doi: 10.1177/0193945903256708. [DOI] [PubMed] [Google Scholar]