Abstract
Objectives: Determine symptoms, correlates, or predictors of depression and anxiety in paid caregivers of elderly persons with dementia.
Participants: The 28 participants were paid caregivers of patients attending an adult day-care program for patients with Alzheimer disease. Each participant had a total score of 16+ or a score of 3+ on at least one item of the Problems and Complaints Inventory.
Measurements: Participants completed the Hamilton Depression (HAM-D) and Anxiety (HAM-A) scales and the Zarit Burden Interview. The total daily and weekly time that caregivers worked with their patients was recorded.
Results: Severity of depression (HAM-D scores) was significantly related to Zarit Burden Interview scores (p<0.001). In addition, HAM-D scores tended to be related to the number of hours per week provided by a caregiver (p=0.09). Severity of anxiety (HAM-A scores) tended to be related to Zarit Burden Interview scores (p=0.08).
Conclusion: These findings indicate the need to devise strategies for alleviating work-related symptoms in paid caregivers.
Keywords: Dementia, caregivers, depression, anxiety
Introduction
The impact of caregiving has been extensively studied in caregivers of adults with a wide variety of physical and emotional illnesses. Most of these studies assessed the psychological and economic impact of caregiving on families of patients with dementia.1,2 Few studies have focused on the psychological symptoms in paid caregivers of dementia patients.
About five million persons are afflicted with Alzheimer disease in the United States.3 As the aging population increases, the number of noninstitutionalized patients with dementia will also increase, indicating a growing need for both family and paid caregivers. Depressive symptoms are reported in 24 to 48 percent of family caregivers of dementia patients4–7 and anxiety symptoms in 10 to 32 percent.5,8 Other problems reported in family caregivers include anger, fatigue, sleepiness, guilt, worry, family conflicts, loss of friends and hobbies, difficulty assuming new roles and responsibilities, and violence.9
In our clinical experience interviewing paid nonrelated caregivers of dementia patients, we have frequently found symptoms of depression, anxiety, helplessness, hopelessness, anger, stress, burden, and guilt. Hence we decided to conduct a pilot study to examine this issue.
Methods
The participants were paid caregivers of patients attending an adult day-care program for patients with Alzheimer disease. All patients lived in their own homes and received varying hours of home care. None of the patients had any family members living with them. All patients had been previously evaluated regarding diagnosis and treatment by Author #1 as part of regular psychiatric care in the day program. The diagnosis of Alzheimer disease was established by evaluation of documentation in the medical record. No additional cognitive scales were used. The study was approved by the Institutional Review Board of St. John's Episcopal Hospital. Caregivers were informed about the study and an invitation for voluntary participation was mailed out to the caregivers. Those caregivers who agreed to participate by responding to the invitation were included in the study.
The participants completed a 53-item problem and complaint questionnaire. Each item is rated from 1 (no symptom) to 5 (extremely severe). Participants who scored 3+ on one item or who had a total score of 16+ (excluding 1 and 2) entered into the study and were evaluated with the Hamilton Depression10 (HAM-D–17 item version) and Anxiety11 (HAM-A) scales and the Zarit Burden Interview (ZBI)12 and received a clinical diagnostic interview to assess other psychopathology as per DSM-IV criteria. The Zarit Burden Interview is one of the most widely used burden measures. The psychometric properties of the full and abridged versions of this scale have been examined in detail.13–15 Pratt, et al., have provided evidence of construct validity in that burden was negatively related to morale and positively related to hours spent giving care.16 Possible scores on the HAM-D range from 0 to 52, HAM-A scores from 0 to 56, and the ZBI scores from 0 to 88. The number of hours worked per week by each participant was also recorded
Statistical Analysis
The association of HAM-D and HAM-A scores with variables indicating a caregiver's time spent with a patient was examined by means of a generalized linear model analysis. HAM-D and HAM-A scores separately served as the dependent variable in the analysis. Caregivers' effort and time were used as independent variables. A separate analysis was conducted for each of the independent variables of interest (total score on the ZBI and number of working hours per day or week). The association was tested by the likelihood-ratio χ2 test.
The relationship between psychopathology and a caregiver's involvement (Burden Interview scores and number of hours per week) was investigated by means of a canonical correlation analysis. For each participant, caregiver time and effort was indicated by the ZBI scores and the number of hours per day or week provided by the caregiver.
Results
Of the 66 caregivers who were screened, 28 met the selection criteria. The 28 participants did not differ from the 38 excluded in terms of caregiver's time and effort spent on a patient. The participants' mean (±SD) age was 51.3±11.3; 19 were African Americans, three were Hispanic, three were Caucasian, and three were of other ethnic backgrounds. Their mean HAM-D and HAM-A scores were 8.7±5.3 and 13.5±7.1, respectively, and the ZBI score was 14.6±8.4. They worked a mean of 63.9±38.4 hours per week as caregivers. None met DSM-IV diagnostic criteria for a psychiatric disorder. See Table 1 for demographic information of participants.
Table 1.
Background characteristics of the 28 participants
| African American | 67.8% |
| Hispanic | 10.7% |
| White | 10.7% |
| Other races | 10.7% |
| Age in years | 51.3±11.3 |
| HAM-D total score (mean±SD) | 8.7±5.3 |
| HAM-A total score (mean±SD) | 13.5±7.1 |
| ZBI score (mean±SD) | 14.6±8.4 |
| Hours worked per week (mean±SD) | 63.9±38.4 |
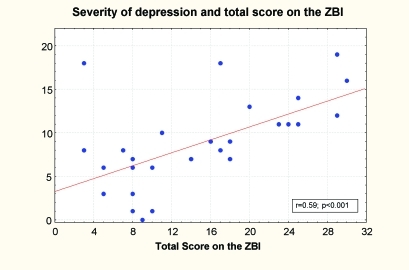
Level of depression (HAM-D scores) was significantly related to the ZBI scores (χ2=16.8; p<0.001) (Figure 1). In addition, HAM-D scores tended to be related to the number of hours per week provided by a caregiver (χ2=2.9; p=0.09). Level of anxiety (HAM-A scores) tended to be related to the ZBI scores (χ2=3.1; p=0.08). The relationship between anxiety level and caregivers' time (number of hours per day or week) failed to reach statistical significance.
Figure 1.
Severity of depression and total score on the ZBI.
Nine of the 28 caregivers reported significant symptoms of anxiety (a score of 20 or more on the HAM-A scale), and seven reported significant symptoms of depression (a score of 12 or more on the HAM-D scale).
Discussion
The limitations of this study include the uncontrolled design and the small number of participants. The inclusion of all participants screened would possibly have yielded more useful data for analysis. However, this was a pilot study and a future large scale study could address these issues. We did not assess the functional staging of dementia or the degree of behavioral and psychological symptoms of the demented patients cared for by these subjects, which could affect the caregivers—paid or unpaid. The use of clinical diagnostic interview as opposed to standardized interview might have contributed to the absence of DSM IV diagnosis in the caregivers. Other issues that deserve consideration for a future study include analysis of past psychiatric history, alcohol and substance abuse history, and psychosocial stressors, if any, of the caregivers.
Takahashi, et al., conducted a study of depression and associated factors of informal caregivers versus professional caregivers of demented patients.17 The professional caregivers in this study were working in the dementia unit of a psychiatric hospital. Measurements included severity of dementia as rated by Clinical Dementia Rating Scale (CDRS)18 and Mini Mental State Examination (MMSE),19 levels of caregiver depression as rated by Beck Depression Inventory (BDI),20 care burden as rated by ZBI and quality of life as rated by World Health Organization-Quality of Life-26(WHO-QOL26).21 Informed caregivers had the highest BDI score and ZBI, and the lowest WHO-QOL among the three groups, which included a control group. There was a strong positive correlation between BDI and ZBI scores, and the scores were significantly high when patients exhibited behavioral problems. The four WHO-QOL categories of physical domain, psychological domain, social relationships, and environment had a strong negative correlation with BDI. The BDI score of the professional caregivers had a strong negative correlation with BDI. The BDI score of the professional caregivers had a strong negative correlation with the physical and psychological domains and environment categories of WHO-QOL. The significant association of the BDI score with the psychological domain and environment was also observed in the regression analysis. Since our dementia patients were higher functioning (living at home and followed in a day program) compared to the hospitalized dementia patients with serious behavior problems, as in the Takahashi, et al., study, comparison of findings may not be appropriate.
Conclusion
The important clinical finding of our preliminary study is that paid caregivers of dementia patients show symptoms of depression and anxiety that are related to the degree of their involvement with dementia patients. Depressive symptoms (HAM-D scores) were significantly associated with a measure of emotional involvement (the ZBI scores).
These findings need to be taken into consideration while devising strategies for alleviating these symptoms. Whether respite care would be an answer to this problem needs to be investigated. In the case of family caregivers, relief services, such as home health aides and brief hospitalization, can increase the family's ability to care for the cognitively impaired at home, lessen the difficulties they face, and help keep down the increasing costs of nursing home care.9
References
- 1.Thompson C, Briggs M. Support for carers of people with Alzheimer’s type dementia. Cochrane Database Syst Rev. 2000;(2):CD000454. doi: 10.1002/14651858.CD000454. [DOI] [PubMed] [Google Scholar]
- 2.Rabins PV. The caregiver’s role in Alzheimer’s disease. Dement Geriatr Cogn Disord. 1998;9(Suppl3):25–8. doi: 10.1159/000051200. [DOI] [PubMed] [Google Scholar]
- 3.Cummings JL, Cole G. Alzheimer disease. JAMA. 2002;287:2335–8. doi: 10.1001/jama.287.18.2335. [DOI] [PubMed] [Google Scholar]
- 4.Rivera PA, Rose JM, Futterman A, et al. Dimensions of perceived social support in clinically depressed and non-depressed female caregivers. Psychol Aging. 1991;6:232–7. doi: 10.1037//0882-7974.6.2.232. [DOI] [PubMed] [Google Scholar]
- 5.Marsh NV, Kersel DA, Havill JH, Sleigh JW. Caregiver burden at one year following severe traumatic brain injury. Brain Injury. 1998;12:1045–59. doi: 10.1080/026990598121954. [DOI] [PubMed] [Google Scholar]
- 6.Kiecolt-Glaser JK, Dura JR, Speicher CE, et al. Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosom Med. 1991;53:345–62. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Dura JR, Stukenberg KW, Kiecolt-Glaser JK. Anxiety and depressive disorders in adult children caring for demented parents. Psychol Aging. 1991;6:467–73. doi: 10.1037//0882-7974.6.3.467. [DOI] [PubMed] [Google Scholar]
- 8.Kinney JM, Stephens MA. Caregiving Hassles Scale: Answering the daily hassles of caregiving for a family member with dementia. Gerontologist. 1989;29:328–32. doi: 10.1093/geront/29.3.328. [DOI] [PubMed] [Google Scholar]
- 9.Rabins PV, Mace NL, Lucas MJ. The impact of dementia on the family. JAMA. 1982;2483:333–5. [PubMed] [Google Scholar]
- 10.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–96. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton M. Diagnosis and rating of anxiety. Br J Psychiatry. 1969;(suppl):76–9. [Google Scholar]
- 12.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly. Correlates of feelings of burden. Gerontologist. 1980;20:649–55. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 13.Vitaliano PP, Young HM, Russo J. Burden: A review of measures used among caregivers of individuals with dementia. Gerontologist. 1991;31(1):67–75. doi: 10.1093/geront/31.1.67. [DOI] [PubMed] [Google Scholar]
- 14.O’Rourke N, Tuokko HA. Psychometric properties of an abridged version of the Zarit Burden Interview within a representative Canadian caregiver sample. Gerontologist. 2003;43:121–7. doi: 10.1093/geront/43.1.121. [DOI] [PubMed] [Google Scholar]
- 15.Gallagher D, Rappaport M, Benedict A, et al. Reliability of selected interview and self-report measures with family caregivers. Paper presented of the Annual Scientific Meeting of the Gerontological Society of America, New Orleans 1985.
- 16.Pratt C, Schmall V, Wright S. Family caregivers and dementia Social casework: J Contemp Social Work. 1986:119–24. [Google Scholar]
- 17.Takahashi M, Katsutoshi T, Miyaoda H. Depression and associated factors of informal caregivers of demented patients. Psychiatry Clin Neurosc. 2005;59(4):473–80. doi: 10.1111/j.1440-1819.2005.01401.x. [DOI] [PubMed] [Google Scholar]
- 18.Hughes CP, Berg L, Danziger WL, et al. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 21.Group TWHOQOL. The World Health Organization quality of life assessment (WHOQOL): Development and general psychometric properties. Soc Sci Med. 1998;46:1569–85. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]