Abstract
Because blood pressure (BP) is an ever changing hemodynamic phenomenon, a BP value, once measured at a physician's office (Office BP), is often unrepresentative of an individual's true BP status. Both ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) provide more accurate and reproducible estimate of BP, and produce stronger predictive ability for cardiovascular outcome than conventional office BP. Two BP measuring techniques, ABPM and HBPM have been widely in clinical use for the detection and management of hypertension. However, they have different advantages and limitations in practice. At present, it has become crucial to understand the characteristics and clinical implications of these BP measuring techniques for those responsible for the care of hypertensive patients.
Keywords: Hypertension, Blood pressure monitoring
Introduction
Arterial blood pressure (BP) is a continuously changing hemodynamic phenomenon that can be influenced by many factors, including an individual's physical and emotional status, and environmental circumstances. It is also controlled by the autonomic nervous system, renin-angiotensin-aldosterone system and other numerous neurohumoral factors. Therefore, once a BP value is measured at a physician's office (office BP), it may not truthfully represent the individual's BP status.1)
Both ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) are alternative methods of measuring BP. They may overcome the problems associated with office BP measurements.
In the past 30 years, these two main BP measuring techniques have been widely used in clinical practice. Since then the awareness of the limitations of office BP measurement has been raised, and wider availability of simple and accurate ABPM and HBPM devices have been made available.1),2) Initially, ABPM was considered as an investigational tool and its used was confined to specialized hypertension centers due to its relatively high cost and inconvenience in the clinical application,3-5) but over the years its availability has gradually increased. On the other hand, physicians have been reluctant in using HBPM in the routine management of hypertensive patients. Rather, it has spread through the non-medical electronic device market in some countries. The official validation of these equipments must be determined before clinical use. At present, up-to-date lists of validated monitors are available through the Internet.2),6)
It is widely accepted that both ABPM and HBPM provide more reliable BP measurements, and give better prediction of organ damage and the risks of cardiovascular (CV) complications than office BP. However, there are some differences in the clinical usefulness and limitations between ABPM and HBPM.7),8)
Ambulatory Blood Pressure Monitoring
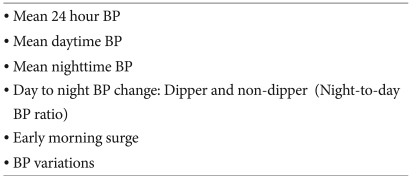
ABPM provides automated measurements of arterial BP for 24 hours or longer, while patients go about their usual daily activities. Most modern ABPM monitors use the oscillometric technique. They weigh only less than 1 kg, and can be simply worn on a belt, and are connected to a sphygmomanometer cuff on the upper arm by a rubber tube. The monitors are programmed to take readings at desired intervals, usually every 15 to 30 minutes, throughout the day and night.1) At the end of the recording, the readings are downloaded onto a computer which is programmed to process the data using various parameters (Table 1).
Table 1.
Parameters for usual analysis of data in ambulatory blood pressure monitoring in clinical practice
BP: blood pressure
There is accumulated evidence that demonstrate the prognostic value of ABPM.9-23) The Ohasama study was conducted on a general population in a Japanese rural area.11) They reported more distinctive association between ambulatory BP and CV mortality than that between office BP and CV mortality. After adjustment for age, gender, smoking status, baseline office BP, and the use of antihypertensive drugs, the risk of CV mortality during a follow-up period of 5.1 years was increased in the highest quintile of the distribution of average 24-hour systolic BP, whereas there was no significant association between office BP and the CV mortality. It was the first study to address the prognostic value of ABPM in the general population.
In a subgroup setting of the Systolic Hypertension in Europe (Syst-Eur) study, the association of ambulatory blood pressure (ABP) with the CV risk was evaluated.14) The Syst-Eur study was a randomized double-blind clinical trial which validated the efficacy of active treatment with a calcium channel blocker-based regimen in older patients with isolated systolic hypertension.24) At the time of randomization, ABPM was performed in 808 patients of whom 98 patients developed major CV events during a median follow-up period of 4.4 years. After adjusting for sex, age, previous CV complications, smoking, and residency in Western Europe, higher 24-hour BP was associated with total, cardiac, and cerebrovascular events in untreated hypertensive patients. For every 10-mmHg increase in mean 24-hour BP, hazard rate for total and CV mortality was 1.23 {95% confidence interval (CI), 1.00-1.50} and 1.34 (95% CI, 1.03-1.75) respectively. In the untreated patients group, the night-time systolic BP predicted end points more accurately than did daytime BP.
Definition of normality for ambulatory blood pressure monitoring
There has been much debate on the definition of diagnostic thresholds for ABP. According to recent guidelines for the BP measurement, an average daytime ABP of less than 135 mmHg systolic, and 85 mmHg diastolic is generally considered normal. This cut-off has been thought to be reasonable because it corresponds approximately to an office BP of 140/90 mmHg. The threshold value for the average night-time ABP is 120 mmHg systolic, and 70 mmHg diastolic.1),25)
However, more recently, a collaborative population based CV outcome-driven study proposed lower diagnostic thresholds for ABPM. The International Database on Ambulatory BP monitoring in relation to Cardiovascular Outcome (IDACO) study26) was designed as a population based longitudinal follow-up CV outcome study. Twenty-four hour ABPM was performed on 5,682 participants enrolled in the prospective population studies in Denmark (Copenhagen), Belgium (Noorderkempen), Japan (Ohasama), and Sweden (Uppsala). In multivariate analyses, the ABP thresholds were determined, which yielded 10-year CV risks similar to that associated with optimal (120/80 mmHg), normal (130/85 mmHg), and high (140/90 mmHg) BP on office measurement. Over 9.7 years of follow-up, 814 CV end point events were recorded. The rounded optimal, normal and high ABP are as follows: systolic/diastolic thresholds for optimal ABP were 115/75 mmHg for 24 hour, 120/80 mmHg for the daytime, and 100/65 mmHg for the nighttime. Corresponding rounded threshold for normal ABP were 125/75, 130/85, and 110/70 mmHg, respectively. That for ambulatory hypertension were 130/80, 140/85, and 120/70 mmHg, respectively. Eventually, these values came out lower than that currently proposed by hypertension guidelines (Table 2).27) However, one should remember that the ABP value is a continuous variable, and the relationship between CV outcomes and BP is also continuous. Therefore, a critical level can not be pinpointed, above which the risk suddenly rises.28)
Table 2.
Threshold blood pressure values proposed by the IDACO study compared with ESH guidelines (average systolic BP/diastolic BP mmHg)
IDACO: the International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes, ESH: the European Society of Hypertension, BP: blood pressure
Day-night blood pressure changes
In subjects with normotension or hypertension, a pronounced diurnal rhythm of BP is present. BP usually falls during the first few hours of sleep, and there is a marked rise in the morning coincidently with the transition from sleep to wakefulness. The average difference between waking and sleeping systolic and diastolic BP is 10-20%. In some subjects, the normal nocturnal fall of BP is diminished (<10%), and they are referred to as "non-dippers", in contrast to normal "dippers".29) In extreme cases, BP rises during the night (reverse dippers). The non-dipping pattern has multiple causes, such as highly active adrenergic activity during the night, poor quality of sleep, presence of renal disease, and use of corticosteroids.6) The classification of 'non-dipper' or 'dipper' is based on the hypothesis that target organ damage and prognosis are worse when BP load is persistent throughout a 24 hour period, than when it is limited to the daytime hours. Because BP is a continuous variable, an arbitrary dichotomization, such as the dipper/non-dipper classification has been criticized. Therefore, an analysis of the diurnal change of BP as a continuous variable could be more reasonable. The day-night BP changes or the day-night BP ratio will be more useful than a dichotomous classification, such as dipper and non-dipper, in this point of the view.30)
In subjects with diminished or abolished fall in BP from day to night, not only left ventricular hypertrophy,31-34) but also silent cerebrovascular disease,35) microalbuminuria,36) and progression of renal damage30) were greater than in those with normal day-night BP difference.
A blunted day-night changes of BP has a greater prognostic significance. It appears that regardless of one's BP status, a non-dipper has poorer CV outcome. In the Ohasama study, Ohkubo et al.37) found an increased CV mortality in non-dippers (relative risk 2.56, p=0.02), and inverted dippers (relative risk 3.69, p=0.004) compared with dippers.
As mentioned earlier, in the analysis of Syst-Euro study,14) the night/day ratio of ambulatory systolic BP was an independent predictor of CV events in the patient group randomized to placebo. It suggests that the mean night-time BP has a better predictive value than the mean daytime BP, although some reports have shown no difference in the predictive power for CV risk between night-time and daytime BP.38) In the previously mentioned IDACO study analysis, this long term follow-up prospective cohort study showed that when adjusted for the daytime BP, night-time BP more accurately predicted total and CV mortality than daytime BP.39) This is the reason why recording ABPM throughout the day is necessary. ABPM is the unique technique capable of recording a series of night-time BP non-invasively in modern clinical practice.
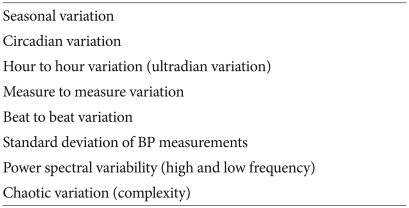
Blood pressure variability
BP variability is measurable in many different ways, ranging from beat-to-beat changes, to changes over periods of weeks or months (Table 3). It may also show seasonal variation or daily changes (circadian variation). The day-night BP change is a typical example of circadian variation. Because the readings are taken intermittently during ABPM, we can only obtain a crude estimation of the true variations, as hour-to-hour (ultradian) or measure-to-measure variations. The calculated standard deviations (SD) of the readings of 24-hour, daytime, and nighttime BP are also crude estimations of an ultradian variation. In studies on ABPM, the frequency and severity of target organ damage were greater in subjects with high SD of BP readings than in those with low SD.40),41) In the Progetto Ipertensione Umbra Monitoraggio Ambulatoriale study,42) the rate of major CV morbid events was higher in subjects with SD of the daytime or the night-time systolic BP above the group mean, compared to those with SD below the group mean. However, this difference vanished in the Cox multivariate analysis after adjustment for age, diabetes, previous CV events, and ABP.
Table 3.
Theoretical classification of blood pressure (BP) variation
The mechanisms and contributing factors to BP variability are still not completely understood. The seasonal, day-to-night changes or measure-to-measure variations may have different mechanisms from each other, and they can also be influenced by different contributing factors. This needs to be clarified, and the association between CV risk and BP variability also remains to be determined.
Kario et al.43) reported that a higher morning BP surge was associated with stroke risk, independent of ABP, nocturnal BP fall, and the presence of silent cerebral infarction in elderly hypertensives. They define morning surge as the difference between morning systolic BP (average of four readings after awaking) and the lowest systolic BP during sleep (average of three BP readings centered on the lowest nighttime reading). They found that a 10 mmHg increase in this surge was associated with 22% (95% CI, 5-40%) increased risk in stroke events.
On the contrary, the Syst-Eur study24) showed that a large morning surge was associated with significantly lower risk of total CV events in untreated elderly hypertensive patients. These results indicated a lower risk of the morning surge in BP, and are consistent with the strong predictive value of nighttime BP that was also identified in this study. In the Ohasama study,44) they found that a higher magnitude of morning surge tended to be associated with an increased risk of cerebral hemorrhage, but not with the risk of cerebral infarction during a mean follow period of 10.4 years in 1,430 individuals in a general population.
Such discrepancy between these prospective studies is due to different study populations, relatively small number of events, and differences in definitions and target outcomes. To elucidate the prognostic significance of the morning surge in BP more precisely, larger prospective studies with longer follow-up periods, including a variety of outcomes, are required.45)
White coat hypertension and white coat effect
White coat hypertension (WCH), also referred to as "isolated office hypertension", is generally defined as persistently high office BP, with a normal BP outside the office.1),30) The alerting reaction to a visit into the physician's office may cause transient elevation in BP. The diagnosis of WCH is important, because it is generally accepted that patients with WCH have relatively low CV risk and are unlikely to benefit from antihypertensive pharmacologic therapy.6) The Ohasama study46) also showed that CV morbidity was lower in WCH than in ambulatory hypertension, and was not dissimilar between WCH and clinical normotension in a mixed population of treated and untreated subjects. However, the prognosis is not always benign. Some studies identified that more frequent target organ damage was present in WCH than clinical normotension.47) In long-term follow up studies, CV risk was increase in patients with WCH. According to an analysis of the pooled data of four different cohort studies, sustained hypertension may develop in some patients with WCH, and the risk of stroke may increase after a mean follow-up period of six years.48) It could reflect a higher inherent risk in subjects with WCH of developing sustained hypertension in the long run.49) Therefore, in patients with WCH, long-term follow up with repeated ABPM or HBPM is necessary.6)
WCH must to be distinguished from the "white coat effect" or "white coat phenomenon", which is the term used to describe transient increase in BP that occurs in a medical environment regardless of the ABP status of patients. Measuring BP in the physician's office may trigger an alerting reaction, which causes a rise in BP. The white coat effect is found in many hypertensive patients, whereby the office BP is usually greater than the average daytime ABP.1) Patients diagnosed with severe hypertension by office BP may have only mild hypertension on ABPM, due to marked white coat effect.
It could elicit misinterpretation of the patient's BP status from the physician responsible for the hypertension management. Physicians are likely to identify patients with poorly controlled BP, when in fact they have normal ABP. For correct diagnosis of white coat effect, ABPM and HBPM are very useful in clinical practice.1),2),6)
Masked hypertension
"Masked hypertension (MH)" or "Reverse white coat hypertension" is defined as having a normal office BP and a high ambulatory or home BP.50) MH was associated with poor CV outcome in a population based study of untreated elderly patients.18) After adjustment for CV risk factors, MH was an independent predictor of CV morbidity when compared to normotensive subjects. The Ohasama study with 24-hour ABPM confirmed an excessive risk of events in subjects with MH, compared to subjects with normal office and ABP.46) When people already have MH, it follows that they should be regarded as being genuinely hypertensive.1) Identifying MH is substantially important in treated patients. The mechanisms responsible for this phenomenon may be different between treated and untreated patients. Drug treatment may elicit a different drop in office BP and ABP attributable to time of administration with respect to the visit and duration of action of drugs. In treated patients, high prevalence of MH may be partly explained by the fact that the office BP is often taken at the time of peak drug effect, whereas ABP or home BP may be taken at its trough, which is particularly evident when short-acting drugs are taken.2)
A study showed that the prevalence of MH was present in one third of treated hypertensive patients in a hypertension clinic. Over five-years of follow-up, their relative risk for CV events was 2.28, as compared to patients whose office and ABP were adequately controlled.51)
The challenge for clinical practice is how to identify and manage these patients, because the prevalence of MH is estimated to be more than 10 percent of the general population. MH may be suspected in individuals who have had an increased office BP at some time, in young persons with a normal or high-normal office BP who had early target organ damage, in individuals with a family history of hypertension in both parents, patients with multiple risks for CV disease, and probably diabetic patients.1)
Home Blood Pressure Monitoring
Over the decades HBPM has been used mostly by patients regardless of physician concern. It was spread via the health care equipment markets in some countries. However, it has recently become increasingly popular and is now gaining more acceptance by patients and physicians, because not only the importance of out-of-office BP measurement has been widely accepted but also more reliable automatic devices have been made available in the market.2),52)
A modern HBPM monitor is very simple and weighs under 1 kg, with a sphygmomanometer cuff connected to a rubber tube which in turns connect to the body of the device. BP is very easily measured using automated oscillometric technique, as by ABPM.
Methodological aspects
Because not all HBPM devices on the market have fulfilled the validation criteria, it is essential to choose a validated device for clinical use. The European Society of Hypertension (ESH) and the British Hypertension Society (BHS) have supported the establishment of websites to provide updated lists of validated BP-measuring devices (www.dableducational.org and www.bhsoc.org respectively).
Detailed description of the technical aspects of device selection and BP measurement is beyond the scope of this article. More precise information can be found in the BP measurement guidelines published by the international academic and professional societies.1),2)
Selection of the optimal schedule for HBPM should include consideration for its ability to provide reliable and reproducible assessment of the usual home BP for each individual. According to outcome studies and clinical pharmacologic trials using HBPM, to achieve the optimal prognostic power, a 7-day schedule with duplicate morning and evening home BP measurements was suggested as appropriate.53) The ESH Working Group on BP monitoring recommended that for the evaluation of hypertensive patients, home BP should be monitored for seven days, with at least two morning and two evening measurements. To enable clinical decision-making, the average of all values should be used, with the exception of the first day values, which should de discarded. Because home BP values on the initial monitoring day were shown to be higher and more unstable, discarding them improves the reproducibility of home BP measurement.1),2)
Because the association between BP and CV risk is continuous, it is difficult to determine a cut-off diagnostic hypertension threshold for HBPM. According to longitudinal population and patients cohort studies, the suggested thresholds differ slightly between them.21),54-56) However, a practical agreement has been made on the diagnostic threshold by international professional societies, which was 135 mmHg for systolic and 85 mmHg for diastolic home BP.1),2) It is very close to the diagnostic threshold of the mean daytime BP for ABPM.
The target home BP for therapy should logically be below the threshold used to diagnose hypertension. That is, it should be lower than 135 mmHg systolic and lower than 85 mmHg for diastolic home BP. Much lower home BP targets are advised in high risk patients, such as those with diabetes mellitus, a history of stroke, coronary heart disease or renal disease.2)
Advantages of home blood pressure monitoring
By using HBPM, it is possible to take BP measurement repeatedly over long periods of time, which allows more reliable estimates of BP. Therefore HBPM predicts clinical outcomes of hypertension better than office BP measurements (Table 4).
Table 4.
Advantages and limitations of home blood pressure monitoring
BP: blood pressure, CV: cardiovascular, HT: hypertension
For diagnosis and management of WCH and MH, HBPM is also as useful as ABPM. The prevalence of these two conditions in the general population is relatively high in the literature (15-20% for WCH and 10-15% for MH).2),46) Even though such results have been obtained using ABPM, HBPM also provided similar estimates, although the results obtained with the two techniques do not overlap completely.2),57)
In treated hypertensive patients, improved long-term control of hypertension is expected by HBPM use. It has the ability to provide information about BP control outside the office, thereby facilitating the identification of treated hypertensive patients with WCH or MH.
WCH is also highly prevalent in treated hypertensive patients, which means that many patients who appear to be refractory to treatment in the doctor's office may have adequately controlled BP at home. In those patients, HBPM can be helpful both in confirming or in rejecting the diagnosis of resistant hypertension.2),58)
The identification of treated patients with MH may be even more important, because this condition appears to be common and is associated with similar CV risk to sustained uncontrolled hypertension.59) Because identifying patients with WCH and MH is difficult in clinics, ideally HBPM should be performed in all treated hypertensive patients, even if they have controlled office BP. It is more strongly recommended to perform HBPM in patients likely to have MH, especially patients with high normal BP, who have high risk of CV diseases, and those with evidence of target organ damage, or those diagnosed with CV disease.2)
Uncontrolled hypertension is usually caused by poor patient adherence to therapy. HBPM is the BP measurement method that requires particular cooperation from the patient, therefore it may affect favorably on patients' perception of their disease, and encourage them to be more compliant with lifestyle modifications and antihypertensive drug therapy.60)
Most validated modern HBPM devices are easy to measure BP using the oscillometric technique. New devices with special functions useful in particular clinical situations are subsequently developed. Digitized data can be stored in some devices, and can be analyzed with built-in software. Other features which may be useful in some patients are developed including external computer connectivity, possibility of printout, automated nighttime measurements, possibility of selecting specific time periods for statistical analysis, and telemonitoring.2)
Limitations of home blood pressure monitoring
Generally, HBPM devices are thought to be very easy to use, and frequently patients monitor BP on their own initiative, using purchased devices without medical advice. However, for accurate measurement and precise interpretation of BP, patients need be trained properly. Patient education must include selection of appropriate devices, with proper cuff size and measurement methodology (Table 4).2),61)
In fact, usually HBPM is unable to measure night-time sleeping BP. On the contrary, ABPM is able to provide a series of frequent and automated BP measurements throughout the 24-hour period. It may be a major disadvantage of HBPM, compared to ABPM. Therefore, with the use of HBPM, it is not possible to analyze BP changes over relative short periods of time, including day-night BP difference, BP variability and excessive morning BP surge, which may have clinical implications on the evidence supporting the adverse prognostic relevance of specific patterns of BP variability over a 24-hour period.8)
Measured home BP values are often reported by patients in handwritten log books. Interestingly, it has been shown that they are frequently inaccurate and illegible, and do not provide immediate insight into the overall time course and control of BP.62) A HBPM device with automated digitized data recording capability will help to resolve the problem.
It should also be considered that HBPM may induce anxiety, resulting in excessive and compulsive BP measurements in some patients. Moreover, the finding of transient high or low BP readings may lead patients to inappropriate self-modification of drug dosage or unnecessary clinic visit.2) Mostly, it can be overcome by adequate patient education.
In patients with cardiac arrhythmias, the use of HBPM raises special concerns. In atrial fibrillation or frequent extrasystoles, large variation of BP from beat to beat often makes accurate BP measurement impossible. Particularly, BP measurement is virtually difficult with oscillometric devices, the software of which is unable to calculate systolic and diastolic BP accurately. In such circumstance, the auscultatory method still remains a useful option for HBPM in patients with arrhythmias.2)
Special applications of home blood pressure monitoring
When applying HBPM, particular consideration is needed in the following clinical situations: in elderly or obese individuals, pregnant women, those with chronic kidney disease, and diabetic patients who have combined hypertension.
In elderly hypertensive patients, there are several specific features, including high WCH prevalence,63) a more pronounced BP variability including excessive morning BP surge,43) and more frequent symptomatic hypotension during treatment than in younger patients. Although ABPM appears to be most suitable for the diagnosis of these problems, HBPM may also be useful in identifying these features and in achieving optimal 24-hour BP control in these patients.
In very elderly patients, it may be difficult to use HBPM due to physical and intellectual limitations. With the assistance of family members, integrated HBPM devices specially designed for the elderly individuals are preferred.2)
In obese individuals, discrepancies between office and home BP are more common, and the severity of obesity appears to be associated with a higher prevalence of both WCH and MH.64) An important difficulty in BP measurement for obese individuals is related to inappropriate cuff size, which may affect the measurement accuracy. The use of a regular cuff may lead to BP overestimation in obese individuals. For accurate BP measurement, it is essential to use an appropriate cuff.
A conical shaped arm, common in obese individuals, makes it difficult to fit the cuff to the arm. The use of wrist devices may help to avoid these problems and represents a potential alternative for HBPM in obese individuals.1),2)
In pregnant women, early detection and optimal treatment of hypertension can reduce potential risks for both the mother and the baby. HBPM can be especially helpful to optimize management of hypertension in hypertensive pregnant women. In addition, because identification of elevated BP is a reliable way to diagnose pre-eclampsia, and regular antenatal care and HBPM can improve the chances of detection.65) Particularly, HBPM is also very helpful in women with previous pre-eclampsia history, who are likely to have a recurrence.
HBPM devices using the oscillometric technique tend to underestimate BP, because of altered hemodynamics often observed in pre-eclampsia. Nonetheless, the degree of error found in most officially approved devices does not necessarily preclude their use in clinical practice. However, some machines have a large unacceptable error, and recommendation remains that each device intended for use in the pregnant population should be specially evaluated.2)
Patients with chronic kidney disease are likely to have coexisting hypertension and have more frequent states of "non-dipper" and "reverse dipper".66) This is also a common finding in patients undergoing hemodialysis or peritoneal dialysis. It has been demonstrated that in these patients, adequate BP control reduces the rate of renal function deterioration, CV morbidity and mortality. The superior prognostic value of HBPM, as compared to office BP, has also been demonstrated, in terms of prediction of composite CV events, end-stage renal disease and death.67)
Because patients with diabetes are very likely to have high CV risk, it is crucial to manage BP optimally for diabetic patients who have combined hypertension. The usefulness of HBPM in this population is particularly related to its ability to detect MH. Indeed, diabetic patients have a very high prevalence of MH detected with HBPM, and are at high risk of developing stroke and kidney damage.68) Therefore, out-of office monitoring of BP should be performed in diabetic patients, even in patients with normal office BP particularly in treated patients, because of the possibility of detecting high trough BP levels.2) Home BP was proven to be a strong and independent predictor of renal function deterioration in diabetic patients, and that such deterioration was present even at relatively low home BP levels. Based on these observations, it was suggested that the therapeutic target for these patients should be lower than that of office BP.69)
Research application of home blood pressure monitoring
Using officially validated and fully automated oscillometric devices, HBPM becomes a valuable tool to evaluate the BP-lowering effect of antihypertensive drugs not only in clinical practice, but in pharmacologic research. HBPM has several advantages in this indication.2)
Most importantly, HBPM provides a more accurate and reproducible estimate of BP compared to office BP, which increases the statistical power of HBPM. HBPM makes it possible to minimize the number of patients to be included in clinical trials. As in clinical practice, both placebo and white coat effect is frequently observed in conventional office BP measurements in the research field. It may also be minimized by the use of HBPM.70),71)
And HBPM can be used as a guide to initiate and titrate antihypertensive therapy in the research setting.70) It also contributes to assess the duration of the action of antihypertensive drugs. This can be achieved by measuring BP before the morning dose, as a trough BP, and again when the full effect of drug is expected, for instance, at midday or in the evening. It is also possible to calculate the morning : evening (M/E) ratio, which may provide similar information to the trough : peak (T : P) ratio, an index often calculated in ABPM and is widely used to estimate the duration of action of antihypertensive drugs.70)
HBPM can be carried out for long periods, in weeks or months, providing valuable information on BP changes occurring throughout the trial. Finally, implementing HBPM in clinical trials may be motivating for patients, thereby contributes to improved compliance and BP control.72)
The reliability of HBPM increased with the use of a proper BP measurement schedule. In the research setting, it is also advised to use a previously described standardized schedule, a 7-day schedule with at least two morning and two evening measurements discarding the first day readings, unless there are specific reasons to modify it. In clinical trials, only validated HBPM monitors should be used, with preference for those with memory storage for BP readings, or for devices with a printout or data download to an external computer, in order to prevent reporting bias.2)
Conclusion
An accurate estimate of BP can be produced by both ABPM and HBPM. And both techniques of BP measurement have stronger prognostic values, compared to conventional office BP. Although a larger amount of outcome data from clinical research has been accumulated for ABPM, HBPM is proven to have a potent predictive value for CV outcomes.
ABPM provides a series of frequent automated BP measurements by programmed intervals throughout a 24 hour period, with which BP changes in relatively short periods can be analyzed. However, repeated performance of ABPM needs special consideration because it is relatively expensive and inconvenient to apply. On the contrary, HBPM produces repeated measurements of BP in long periods of time. It may be extended even into a period of one's life-time. In fact ABPM and HBPM are complementary tools in the evaluation and management of hypertensive patients. While a preferential role of HBPM could lie on the long term management of hypertension, ABPM is a useful tool for the initial assessment of hypertension, and for the evaluation of relatively high risk patients, especially in those who have target organ damage or diagnosed CV diseases.
There is yet to be large clinical outcome data using BP monitoring in Korea. Therefore the Korean Ambulatory Blood Pressure (Kor-ABP) Registration study, which is a web-based long-term registration project (www.korabp.org), had been constructed in 2009.73) At present, about 24 hospitals and institutions throughout the nation have actively participated in this study, and they are increasing in number. Long-term follow-up nation-wide CV outcome data of ABPM is expected.
References
- 1.O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505–1526. doi: 10.1097/HJH.0b013e328308da66. [DOI] [PubMed] [Google Scholar]
- 3.Yoo WS, Park HJ, Lee EY, Choi SK. A representative value for 24-h ambulatory blood pressure monitoring. Korean Circ J. 1985;15:209–214. [Google Scholar]
- 4.Park IS, Rho TH, Park JW, et al. Prevalence of urinary microalbuminuria in normal and hypertensive Koreans and its correlation with blood pressure measured by 24 hours ambulatory blood pressure monitoring. Korean Circ J. 1994;24:834–840. [Google Scholar]
- 5.Jeon HC, Kim YK, Kim KY, et al. Determination of left ventricular mass in healthy adults: a study using echocardiography and 24 hour ambulatory blood pressure monitoring. Korean Circ J. 1995;25:811–819. [Google Scholar]
- 6.Pickering TG, Shimbo D, Hass D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 7.Verdecchia P, Angeli F, Mazzotta G, Gentile G, Reboldi G. Home blood pressure measurement will not replace 24-hour ambulatory blood pressure measurement. Hypertension. 2009 doi: 10.1161/HYPERTENSIONAHA.108.122861. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Parati G, Omboni S, Bilo G. Why is out-of-office blood pressure measurement needed?: home blood pressure measurements will increasingly replace ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Hypertension. 2009 doi: 10.1161/HYPERTENSIONAHA.108.122853. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressure. JAMA. 1983;249:2792–2798. [PubMed] [Google Scholar]
- 10.Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801. doi: 10.1161/01.hyp.24.6.793. [DOI] [PubMed] [Google Scholar]
- 11.Ohkubo T, Imai Y, Tsuji I, et al. Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in Ohasama. J Hypertens. 1997;15:357–364. doi: 10.1097/00004872-199715040-00006. [DOI] [PubMed] [Google Scholar]
- 12.Redon J, Campos C, Narciso ML, Rodicio JL, Pascual JM, Ruilope LM. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension. 1998;31:712–718. doi: 10.1161/01.hyp.31.2.712. [DOI] [PubMed] [Google Scholar]
- 13.Khattar RS, Senior R, Lahiri A. Cardiovascular outcome in white-coat versus sustained mild hypertension: a 10 year follow-up study. Circulation. 1998;98:1892–1897. doi: 10.1161/01.cir.98.18.1892. [DOI] [PubMed] [Google Scholar]
- 14.Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. JAMA. 1999;282:539–546. doi: 10.1001/jama.282.6.539. [DOI] [PubMed] [Google Scholar]
- 15.Kario K, Shimata K, Schwartz JE, Matsuo T, Hoshide S, Pickering TG. Silent and clinically overt stroke in older Japanese subjects with white-coat and sustained hypertension. J Am Coll Cardiol. 2001;38:238–245. doi: 10.1016/s0735-1097(01)01325-0. [DOI] [PubMed] [Google Scholar]
- 16.Gustavsen PH, Hoegholm A, Bang LE, Kristensen KS. White coat hypertension is a cardiovascular risk facter: a 10-year follow-up study. J Hum Hypertens. 2003;17:811–817. doi: 10.1038/sj.jhh.1001643. [DOI] [PubMed] [Google Scholar]
- 17.Clement DL, Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–2415. doi: 10.1056/NEJMoa022273. [DOI] [PubMed] [Google Scholar]
- 18.Bjorklund K, Lind L, Zethelius B, Andren B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297–1302. doi: 10.1161/01.cir.0000054622.45012.12. [DOI] [PubMed] [Google Scholar]
- 19.Pierdomenico SD, Lapenna D, Bucci A, et al. Cardiovascular and renal events in uncomplicated mild hypertensive patients with sustained and white coat hypertension. Am J Hypertens. 2004;17:876–881. doi: 10.1016/j.amjhyper.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Fagard RH, Van den Broeke C, De Cort P. Prognostic significance of blood pressure measured in office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–807. doi: 10.1038/sj.jhh.1001903. [DOI] [PubMed] [Google Scholar]
- 21.Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from Pressioni Arteriose Monitorate e Loro Associozioni (PAMELA) Study. Circulation. 2005;111:1777–1783. doi: 10.1161/01.CIR.0000160923.04524.5B. [DOI] [PubMed] [Google Scholar]
- 22.Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 23.Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinical blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–161. doi: 10.1161/01.HYP.0000170138.56903.7a. [DOI] [PubMed] [Google Scholar]
- 24.Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350:757–764. doi: 10.1016/s0140-6736(97)05381-6. [DOI] [PubMed] [Google Scholar]
- 25.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part I. blood pressure measurement in humans. A statement for professionals from the sub-committee of professional and public education of the American Heart Association council on high blood pressure research. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 26.Kikuya M, Hansen TW, Thijs L, et al. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Circulation. 2007;115:2145–2152. doi: 10.1161/CIRCULATIONAHA.106.662254. [DOI] [PubMed] [Google Scholar]
- 27.Hansen TW, Kikuya M, Thijs L, et al. Diagnostic thresholds for ambulatory blood pressure moving lower: a review based on a meta-analysis-clinical implications. J Clin Hypertens (Greenwich) 2008;10:377–381. doi: 10.1111/j.1751-7176.2008.07681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kikuya M, Hansen TW, Thijs L, et al. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Blood Press Monit. 2007;12:393–395. doi: 10.1097/MBP.0b013e3282f2b53d. [DOI] [PubMed] [Google Scholar]
- 29.O'Brien E, Sheridan J, O'Malley K. Dipper and non-dippers. Lancet. 1988;2:397. doi: 10.1016/s0140-6736(88)92867-x. [DOI] [PubMed] [Google Scholar]
- 30.Verdecchia P. Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension. 2000;35:844–851. doi: 10.1161/01.hyp.35.3.844. [DOI] [PubMed] [Google Scholar]
- 31.Verdecchia P, Schillaci G, Guerrieri M, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–536. doi: 10.1161/01.cir.81.2.528. [DOI] [PubMed] [Google Scholar]
- 32.Kim SJ, Kang HS, Hwang SJ, et al. The relation of circadian blood pressure variation to left ventricular mass, diastolic function and dynamic QT dispersion. Korean Circ J. 2005;35:382–388. [Google Scholar]
- 33.Lee JU, Kim KS, Kim SK, et al. Left ventricular geometric patterns of dippers and non-dippers in essential hypertension. Korean Circ J. 1996;26:44–51. [Google Scholar]
- 34.Lee CK, Her GM, Park GE, et al. Interrelationship between left ventricular mass and diurnal variations of blood pressure in patients with essential hypertension. Korean Circ J. 1997;27:13–19. [Google Scholar]
- 35.Shimada K, Kawamoto A, Matsubayashi K, et al. Diurnal blood pressure variations and silent cerebrovascular damage in elderly patients with hypertension. J Hypertens. 1992;10:875–878. [PubMed] [Google Scholar]
- 36.Redon J, Liano Y, Lozano JV, Miralles A, Pascual JM, Cooper RS. Ambulatory blood pressure and microalbuminuria in essential hypertension: role of circadian variability. J Hypertens. 1994;12:947–953. [PubMed] [Google Scholar]
- 37.Ohkubo T, Imai Y, Tsuji I, et al. Relation between nocturnal decline in blood pressure and mortality: the Ohasama study. Am J Hypertens. 1997;10:1201–1207. doi: 10.1016/s0895-7061(97)00274-4. [DOI] [PubMed] [Google Scholar]
- 38.Bjorklund K, Lind L, Zethelius B, Berglund L, Lithell H. Prognostic significance of 24-h ambulatory blood pressure characteristics for cardiovascular morbidity in a population of elderly men. J Hypertens. 2004;22:1691–1697. doi: 10.1097/00004872-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Boggia J, Li Y, Thijs L, et al. Prognositic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–1229. doi: 10.1016/S0140-6736(07)61538-4. [DOI] [PubMed] [Google Scholar]
- 40.Kikuya M, Hozowa A, Ohkubo T, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension. 2000;36:901–906. doi: 10.1161/01.hyp.36.5.901. [DOI] [PubMed] [Google Scholar]
- 41.Rim SJ. Blood pressure variation and cardiovascular risks. Korean Circ J. 2008;38:131–134. [Google Scholar]
- 42.Verdecchia P, Borgioni C, Ciucci A, et al. Prognostic significance of blood pressure variability in essential hypertension. Blood Press Monit. 1996;1:3–11. [PubMed] [Google Scholar]
- 43.Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–1406. doi: 10.1161/01.cir.0000056521.67546.aa. [DOI] [PubMed] [Google Scholar]
- 44.Metoki H, Ohkubo T, Kikuya M, et al. Prognostic significance for stroke of a morning pressure surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149–154. doi: 10.1161/01.HYP.0000198541.12640.0f. [DOI] [PubMed] [Google Scholar]
- 45.Ohkubo T, Metoki H, Imai Y. Prognostic significance of morning surge in blood pressure: which definition, which outcome? Blood Press Monit. 2008;13:161–162. doi: 10.1097/MBP.0b013e3282fd16a9. [DOI] [PubMed] [Google Scholar]
- 46.Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of "masked" hypertension and "white-coat" hytertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–515. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 47.Kim HY, Kwack NJ, Park NK, et al. Influences of white-coat hypertension and white-coat effect on the left ventricular mass and diastolic function. Korean Circ J. 1995;25:987–997. [Google Scholar]
- 48.Verdecchia P, Reboldi GP, Angeli F, et al. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension. 2005;45:203–208. doi: 10.1161/01.HYP.0000151623.49780.89. [DOI] [PubMed] [Google Scholar]
- 49.Ugajin T, Hozawa A, Ohkubo T, et al. White-coat hypertension as a risk factor for the development of home hypertension: the Ohasama study. Arch Intern Med. 2005;165:1541–1546. doi: 10.1001/archinte.165.13.1541. [DOI] [PubMed] [Google Scholar]
- 50.Pickering T, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40:795–796. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 51.Pierdomenico SD, Lapenna D, Bucci A, et al. Cardiovascular outcome in treated hypertensive patients with responder, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18:1422–1428. doi: 10.1016/j.amjhyper.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 52.Verberk WJ, Kroon AA, Kessels AG, de Leeuw PW. Home blood pressure measurement: a systemic review. J Am Coll Cardiol. 2005;46:743–751. doi: 10.1016/j.jacc.2005.05.058. [DOI] [PubMed] [Google Scholar]
- 53.Mengden T, Chamontin B, Phong CN, LuisPalma GJ, Chanudet X. User procedure for self-measurement of blood pressure. First International Consensus Conference on Self Blood Pressure Measurement. Blood Press Monit. 2000;5:111–129. [PubMed] [Google Scholar]
- 54.Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension. 2006;47:846–853. doi: 10.1161/01.HYP.0000215363.69793.bb. [DOI] [PubMed] [Google Scholar]
- 55.Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–975. doi: 10.1097/00004872-199816070-00010. [DOI] [PubMed] [Google Scholar]
- 56.Ohkubo T, Asayama K, Kikuya M, et al. Prediction of ischaemic and heamorrhagic stroke by self-measured blood pressure at home: the Ohasama study. Blood Press Monit. 2004;9:315–320. doi: 10.1097/00126097-200412000-00009. [DOI] [PubMed] [Google Scholar]
- 57.Stergiou GS, Zourbaki AS, Skeba II, Mountokalakis TD. White coat effect detecting using self-monitoring of blood pressure at home: comparison with ambulatory blood pressure. Am J Hypertens. 1998;11:820–827. doi: 10.1016/s0895-7061(98)00038-7. [DOI] [PubMed] [Google Scholar]
- 58.Denolle T, Waeber B, Kjeldsen S, Parati G, Wilson M, Asmar R. Self-measurement of blood pressure in clinical trials and therapeutic applications. Blood Press Monit. 2000;5:145–149. [PubMed] [Google Scholar]
- 59.Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of 'masked hypertension' detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–1349. doi: 10.1001/jama.291.11.1342. [DOI] [PubMed] [Google Scholar]
- 60.Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich) 2006;8:174–180. doi: 10.1111/j.1524-6175.2006.04872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Logan AG, Dunai A, McIssac WJ, Irvine MJ, Tisler A. Attitudes of primary care physicians and their patients about home blood pressure monitoring in Ontario. J Hypertens. 2008;26:446–452. doi: 10.1097/HJH.0b013e3282f2fdd4. [DOI] [PubMed] [Google Scholar]
- 62.Mengden T, Hemandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H. Reliability of reporting self-measured blood pressure values by hypertensive patients. Am J Hypertens. 1998;11:1413–1417. doi: 10.1016/s0895-7061(98)00241-6. [DOI] [PubMed] [Google Scholar]
- 63.Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet. 2000;355:865–872. doi: 10.1016/s0140-6736(99)07330-4. [DOI] [PubMed] [Google Scholar]
- 64.Lurbe E, Invitti C, Torro I, et al. The impact of the degree of obesity on the discrepancies between office and ambulatory blood pressure values in youth. J Hypertens. 2006;24:1557–1564. doi: 10.1097/01.hjh.0000239291.32883.e3. [DOI] [PubMed] [Google Scholar]
- 65.Milne F, Redman C, Walker J, et al. The preeclampsia community guideline (PRECOG): how to screen for and detect onset of preeclampsia in the community. BMJ. 2005;330:576–580. doi: 10.1136/bmj.330.7491.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Redon J, Oliver V, Zaragoza MD, Galindo MJ. Ambulatory blood pressure during diseases of the kidney. Blood Press Monit. 1999;4:267–274. [PubMed] [Google Scholar]
- 67.Agarwal R, Andersen MJ. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am J Nephrol. 2006;26:503–510. doi: 10.1159/000097366. [DOI] [PubMed] [Google Scholar]
- 68.Eguchi K, Ishikawa J, Hoshide S, Pickering TG, Shimada K, Kario K. Masked hypertension in diabetes mellitus: a potential risk. J Clin Hypertens (Greenwich) 2007;9:601–607. doi: 10.1111/j.1524-6175.2007.06610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rave K, Bender R, Heise T, Sawicki PT. Value of blood pressure self-monitoring as a predictor of progression of diabetic nephropathy. J Hypertens. 1999;17:597–601. doi: 10.1097/00004872-199917050-00002. [DOI] [PubMed] [Google Scholar]
- 70.Vaur L, Duborca I, Dutrey-Dupagne C, et al. Superiority of home blood pressure measurements over office measurements for testing antihypertensive drugs. Blood Press Monit. 1998;3:107–114. [PubMed] [Google Scholar]
- 71.Staessen JA, Den HE, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004;291:955–964. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]
- 72.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomized trials. BMJ. 2004;329:145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kim JH, Park JC. Variables and end-points in Korean Ambulatory Blood Pressure (Kor-ABP) registry. J Korean Soc Hypertens. 2009;15(Suppl I):I74–I80. [Google Scholar]