Abstract
A 34-year-old man, who had been treated with an endoscopic injection of a mixture of n-butyl-2-cyanoacrylate (Histoacryl) and Lipiodol for control of variceal bleeding 6 months previously, presented with an intracardiac mass in the right atrium (RA). Two-dimensional echocardiography revealed an intracardiac mass in the RA that appeared to extend from the inferior vena cava. The origin of the sclerosant was traced by computed tomography (CT). This is a very rare case in which the sclerosant migration route was demonstrated by CT scan. The findings of this case suggest that the systemic migration of sclerosant into an intracardiac chamber should be considered in patients with an intracardiac mass, especially with a history of previous sclerotherapy for variceal bleeding.
Keywords: N-butyl-2-cyanoacrylate, Esophageal varix, Sclerotherapy, Embolism, Right atrium
Introduction
The systemic migration of sclerosant is a rare complication of endoscopic injection sclerotherapy. Serious complications, such as embolization to the brain,1) lungs,2) and portal veins3) have been occasionally reported. However, it is not well known how systemic sclerosant migration occurs.
We report a rare case of sclerosant migration presenting as an intracardiac mass after endoscopic sclerotherapy for variceal bleeding, and demonstrate the entire migration route.
Case
A 34-year-old man with hepatits B virus-related liver cirrhosis (Child-Pugh Score B), was referred to our clinic for an intracardiac mass detected incidentally by transthoracic echocardiography. Six months previously, he had been treated with an endoscopic injection of a mixture of n-butyl-2-cyanoacrylate (Histoacryl) and Lipiodol for control of variceal bleeding. At presentation, the patient had no cardiac symptoms. On physical examination, his vital signs were stable and he had normal respiratory and cardiovascular findings. His sclerae were icteric and his abdomen was distended with ascites. A chest X-ray was unremarkable.
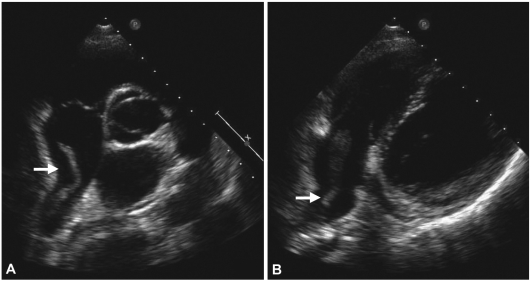
Two-dimensional echocardiography revealed an intracardiac mass in the right atrium (RA) that appeared to extend from the inferior vena cava. It was a 5 cm elongated, hypermobile structure (Fig. 1). The echogenic mass, suggestive of a thrombus, resembled a blood vessel.
Fig. 1.
Transthoracic echocardiography shows an elongated intracardiac mass in the right atrium (arrow), which appears to extend from the inferior vena cava. A: parasternal short axis view, aortic valve level. B: off-axis modified four-chamber view.
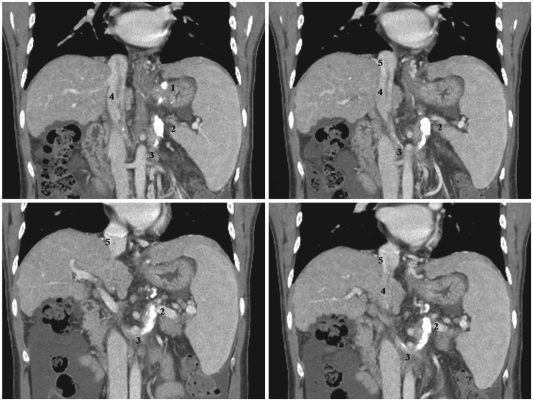
Even though it appeared to extend from the inferior vena cava, the exact origin was not clearly demonstrated by echocardiography. Portal-phase abdominal computed tomography (CT) with coronal reconstruction identified the origin of the elongated intracardiac mass (Fig. 2). After originating from varices at the gastroesophageal junction, a partially radio-opaque and radiolucent intraluminal material, consistent with a mixture of sclerosant and thrombus, traversed a gastrorenal shunt, extended through the inferior vena cava, and stopped in the RA.
Fig. 2.
Portal-phase abdominal computed tomography scans with coronal reconstruction demonstrate a partial radio-opaque and radiolucent intraluminal material consistent with a mixture of sclerosant and thrombus, which originates from the gastroesophageal junction (1) and forms an intraluminal and intracardiac mass traversing a gastrorenal shunt (2), the left renal vein (3), the inferior vena cava (4) and right atrium (5).
Close clinical observation was undertaken for 2 weeks. Follow-up echocardiography showed no significant interval change compared with the initial study, and no cardiac symptoms developed. The patient did not manifest any signs or symptoms of systemic embolization by sclerosant. He was discharged without any significant problems, and remains asymptomatic on regular follow-up.
Discussion
Endoscopic injection of a mixture of Histoacryl and Lipiodol has been reported to be an optimal and effective therapy for variceal bleeding.4) Reported complications of this treatment include fever, ulceration at the injection site, chest pain, and dysphagia.3) A few case reports have documented systemic embolization of sclerosant as one of the uncommon complications after sclerotherapy.1-3) In this report, intracardiac sclerosant located in the RA was demonstrated by echocardiography.
Histoacryl is a watery solution that polymerizes and hardens instantaneously on contact with blood.5) To prevent needle immobilization in a varix, Lipiodol serves as a diluent that delays Histoacryl polymerization.6) Delayed polymerization may increase the possibility of systemic migration,7) and rapid injection may increase intravariceal pressure and induce migration of the sclerosant before complete polymerization.8) In addition, a large injected volume of the Histoacryl and Lipiodol mixture may contribute to systemic migration. In patients with varices associated with a gastrosystemic venous shunt, endoscopic sclerotherapy presents a potential risk for migration of the sclerosant into the systemic venous circulation.9) However, it is not well known how sclerosant migration occurs, mainly because patients are not routinely imaged after sclerotherapy. In addition, sclerosant migration and embolization are difficult to diagnose using CT, because the sclerosant is masked by contrast.10)
In 2006, Lee et al.11) reported a rare case of acrylic cement foreign body in the RA and central veins after vertebroplasty, and suggested that an acrylic cement foreign body should be considered as a potential source of pulmonary embolism. There has been no report of an echocardiographic demonstration of intracardiac sclerosant in the RA following endoscopic sclerotherapy for varices, in addition to illustration of the entire sclerosant migration route. In the present case, portal-phase CT clearly visualized the entire sclerosant migration route along with thrombus on the sclerosant plug, thereby documenting that systemic migration of sclerosant occurs via a gastrosystemic venous shunt. This case indicates that systemic migration of sclerosant into an intracardiac chamber should be considered in patients with an intracardiac mass, especially with a history of previous sclerotherapy for variceal bleeding.
References
- 1.See A, Florent C, Lamy F, Levy VG, Bouvry M. Cerebrovascular accident after endoscopic obturation of esophageal varices with isobutyl-2-cyanoacylate in 2 patients. Gastroenterol Clin Biol. 1986;10:604–607. [PubMed] [Google Scholar]
- 2.Thakeb F, Kader S, Salama Z, Abdel Raouf T, Abdel Kader S, Abdel Hamid H. The value of the combined use of n-butyl-2-cyanoacrylate and ethanolamine oleate in the management of bleeding esophagogastric varices. Endoscopy. 1995;27:358–364. doi: 10.1055/s-2007-1005714. [DOI] [PubMed] [Google Scholar]
- 3.Moustafa I, Omar MM, Nooh A. Endoscopic control of gastric variceal bleeding with butyl cyanoacrylate in patients with schisiosomiasis. J Egypt Soc Parasitol. 1997;27:405–410. [PubMed] [Google Scholar]
- 4.Huang YH, Yeh HZ, Chen GH, et al. Endoscopic treatment of bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc. 2000;52:160–167. doi: 10.1067/mge.2000.104976. [DOI] [PubMed] [Google Scholar]
- 5.Anderson JM, Gibbons DF. The new generation of biochemical polymers. Biomater Med Devices Artif Organs. 1974;2:235–248. doi: 10.3109/10731197409118593. [DOI] [PubMed] [Google Scholar]
- 6.D'Imperio N, Piemontese A, Baroncini D, et al. Evaluation of undiluted N-butyl-2-cyanoacrylate in the endoscopic treatment of upper gastrointestinal tract varices. Endoscopy. 1996;28:239–243. doi: 10.1055/s-2007-1005435. [DOI] [PubMed] [Google Scholar]
- 7.Dhiman RK, Chawla Y, Taneja S, Biswas R, Sharma TR, Dilawari JB. Endoscopic sclerotherapy of gastric variceal bleeding with N-butyl-2-cyanoacrylate. J Clin Gastroenterol. 2002;35:222–227. doi: 10.1097/00004836-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Cheng PN, Sheu BS, Chen CY, Chang TT, Lin XZ. Splenic infarction after Histoacryl injection for bleeding gastric varices. Gastrointest Endosc. 1998;48:426–427. doi: 10.1016/s0016-5107(98)70018-5. [DOI] [PubMed] [Google Scholar]
- 9.Hwang SS, Kim HH, Park SH, et al. N-butyl-2-cyanoacrylate pulmonary embolism after endoscopic injection sclerotherapy for gastric variceal bleeding. J Comput Assist Tomogr. 2001;25:16–22. doi: 10.1097/00004728-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Javed A, Salamat A. N-butyl-2-cyanoacrylate and lipiodol pulmonary embolism (glue embolism) J Ayub Med Coll Abbottabad. 2008;20:143–145. [PubMed] [Google Scholar]
- 11.Lee SE, Chang SA, Kim MS, et al. Acrylic cement foreign body and thrombus in right atrium causing pulmonary embolism after percutaneous vertebroplasty. Korean Circ J. 2006;36:713–715. [Google Scholar]