ABSTRACT
Purpose: To identify modifiable risk factors associated with the transition from non-faller to faller in community-dwelling older adults.
Method: A prospective study design was used. Adults aged 60 to 90 years (n=90, mean age=79.7 years, 63% male) who did not report falling in the past year were included. A comprehensive geriatric assessment was performed at study baseline, and daily falls data were collected monthly for 1 year. Multivariable regression using a modified Poisson model on fall status (yes/no) and a Cox proportional hazards model for time to first fall were used to identify risk factors.
Results: Twenty-four people (27%) fell. Modifiable risk factors were present in 67% of study participants, and fall risk increased as the number of risk factors increased. The most common activities performed prior to falling were walking and using stairs. Fall risk doubled ([relative risk=2.00; 95%CI: 1.13–3.56) per unit increase in the number of risk factors (lower-extremity weakness, balance impairment, and ≥4 prescription medications).
Conclusions: Among older adults who were self-reported non-fallers, falls were a common outcome, and modifiable risk factors were present in the majority of the sample. The absence of a fall history does not rule out the need to screen for other risk factors for falls. Functional lower-extremity weakness, balance impairment as measured by the Berg Balance Scale (score <50), and number of risk factors were independent predictors for the transition in status from non-faller to faller. Further research is required to define effective interventions to prevent first falls.
Key Words: accidental falls, aged, geriatric assessment, postural balance, prospective study, risk factors
RÉSUMÉ
Objectif : Identifier les facteurs de risque modifiables propres à réduire les risques de chutes chez les aînés qui vivent dans la communauté.
Méthode : Une étude prospective a été utilisée. Des adultes de 60 à 90 ans (n=90, âge moyen=79,7 ans, 63 % hommes) qui ont dit n'être jamais tombés au cours de la dernière année ont été inclus dans l'échantillon. Une évaluation gériatrique complète a été réalisée au début de l'étude et des données quotidiennes sur les chutes ont été recueillies chaque mois pendant un an. Une régression multivariable à l'aide d'un modèle de Poisson modifié sur l'état des chutes (oui/non) et un modèle de proportionnalité des risques de Cox pour le moment de la première chute ont été utilisés pour identifier les facteurs de risque.
Résultats : Vingt-quatre personnes (27 %) ont fait une chute. Des facteurs de risque modifiables étaient présents chez 67 % des participants à l'étude, et les risques de chutes se sont accrus avec l'augmentation des facteurs de risque. Les activités les plus usuelles accomplies avant les chutes étaient la marche ou l'utilisation d'escaliers. Les risques de chute ont doublé [risque relatif de 2,00 (95 % CI : 1,13–3,56)] par unité dans le nombre de facteurs de risque (faiblesse des membres inférieurs, déficience de l'équilibre et ≥4 médicaments sous ordonnance).
Conclusions : Parmi les aînés qui ont dit ne jamais être victimes de chutes, celles-ci se produisaient régulièrement et des facteurs de risque modifiables étaient présents chez la majorité des personnes de l'échantillon. L'absence d'antécédents de chute n'exclut pas la nécessité de détecter les autres facteurs de risques de chutes. Une faiblesse des membres inférieurs, une déficience de l'équilibre sur l'échelle d'équilibre de Berg (pointage <50), et un certain nombre d'autres facteurs de risque ont été des variables indépendantes pour la transition du statut de victime de chutes à personne non-victime de chutes. Des recherches supplémentaires seront nécessaires pour définir les interventions les plus efficaces pour prévenir les chutes initiales.
Mots clés : aînés, chutes accidentelles, équilibre postural, étude prospective, évaluation gériatrique, facteurs de risque
INTRODUCTION
Falls in older adults generally result from a multifactorial etiology involving intrinsic, pharmacological (i.e., prescription medications), behavioural, activity-related, and environmental factors.1 The most prominent risk factor for subsequent falls in prospective cohort studies of community-dwelling older adults is a recent fall history.2–8 A recent fall history is such a consistent marker for future fall risk that it appears as the first item in fall-prevention screening algorithms.1–5 The most prominent fall-prevention guidelines urge clinicians in primary care to ask all older adults about falls in the past year.1 The algorithm streams older adults with a negative fall history into a ‘no intervention’ arm that suggests yearly monitoring.
Most prospective cohort studies on fall risk in older adults either include a heterogeneous population of older adults (with and without a history of falling) or are restricted to people with a history of falling.6–8 This literature has been used to derive clinical practice guidelines for the secondary prevention of falls, but it has limited application to primary fall prevention. The limited scope of recommendations for people without a recent fall history may reflect a lack of evidence on which guidelines can be based.
Factors associated with the transition in status from non-faller to faller are less well understood. A review of the literature revealed a single prospective cohort study of fall risk factors that limited enrolment to non-fallers; furthermore, the sample comprised only women.9 There is a need to evaluate factors that are associated with the transition in status from non-faller to faller and to quantify the magnitude of risk for older adults. Finding a small number of easily identifiable and potentially modifiable risk factors for falls in those with a negative fall history would provide an evidence base for targeted assessment and intervention to reduce fall risk in this group.
The primary objective of this study was to evaluate whether balance impairment and the related potentially modifiable risk factors of lower-extremity weakness, gait impairment, and number of prescription medications are independent predictors of the outcome any fall over a 1-year period among older adults with no recent fall history.
METHODS
Design
The study used prospective falls data collected during a field trial of a fall-prevention programme, the Project to Prevent Falls in Veterans (PPFV), carried out at the University of Western Ontario and funded jointly by Health Canada and Veterans' Affairs Canada (VAC). The PPFV was approved by the University of Western Ontario's Research Ethics Board for Health Sciences Research Involving Human Subjects. Written informed consent was obtained from all participants. The sampling and data-collection procedures for Phase I have been described in detail elsewhere.10
Briefly, Phase I of the PPFV was a mailed questionnaire sent to three simple random samples of addresses of 1,000 Canadian veterans of World War II and the Korean War living in southwestern Ontario. Canadian veterans of these two wars, as determined by VAC, and their spouses living independently in the community who were able to understand and provide responses to the questionnaire were eligible.
Phase I participants residing in two regions of southwestern Ontario were eligible for Phase II, a risk-factor modification trial. The intervention was randomized to people who self-reported at least one modifiable risk factor for falling on the mailed questionnaire. Randomization was to one of two groups: the Specialized Geriatric Services (SGS) group or the Family Physician (FP) group. People with no reported modifiable fall risk factors on the questionnaire formed an open arm (i.e., were not randomized to an intervention) in the Phase II study.
The SGS group received a comprehensive fall assessment performed by a geriatrician or physical therapist and was given individual recommendations to reduce fall risk factors. The study intervention consisted of the fall assessment and recommendations; the intervention did not involve providing any ongoing treatment. The FP group was sent a letter summarizing the risk factors identified on their mailed questionnaire; a similar letter was sent to the participant's family physician, and any treatment was left at the discretion of the family physician. Participants in the open arm of the study received the same comprehensive fall assessment as the SGS group and educational materials on fall prevention and healthy living.
There were no statistically or clinically significant differences between the study arms in the proportion of those who fell, the number of falls, or the time to first fall. Given these results, the opportunity existed to use the data collected to evaluate associations for the transition in status from non-faller to faller. The current study analyzed data obtained from participants in the SGS group and the no reported modifiable risk factors group who received the comprehensive geriatric assessment and reported no history of falls at baseline in Phase II.
Study Participants
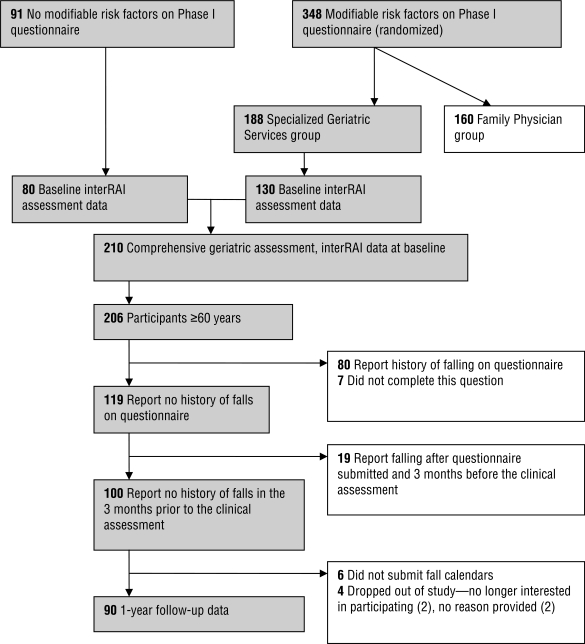
In Phase II of the PPFV, 210 people received the comprehensive geriatric assessment (80 people who reported no risk factors on the Phase I questionnaire and 130 people who reported at least one modifiable risk factor for falls who were randomized to the SGS group; see Figure 1). Four people under 60 years of age were excluded from the analysis. One hundred and twenty-six people (60%) reported no history of falls in the previous 12 months on the mailed questionnaire; seven did not complete this question and were therefore excluded from the analysis. The average interval between the questionnaire and the comprehensive geriatric assessment was 10 months. Nineteen people who reported falling between the questionnaire and the clinical assessment and 10 people who had incomplete follow-up information for falls over the duration of the study were also excluded from analysis, leaving a sample of 90 people age 60 years or older for the present study.
Figure 1.
Overview of study participant flow for inclusion in the present study from Phase II of the Project to Prevent Falls in Veterans
Demographic and Clinical Variables
The comprehensive fall assessment used the basic version of the interRAI Community Health Assessment, a subset of the Minimum Data Set for Home Care (MDS-HC) version 2.0.11,12 The MDS-HC covers several key domains, including demographics, cognition, service use, function, health, and social support. All items of the MDS-HC have demonstrated reliability and validity in community settings.13,14
No direct measure of lower-extremity strength was performed in the study. The ability to stand up from a seated position in a chair without using the chair arms served as a proxy measure, termed functional lower-extremity strength. An unsteady gait was assessed with an observational analysis of gait quality; an abnormality was defined as the presence of any one the following gait types: antalgic, ataxic, spastic, steppage, leg-length discrepancy, waddling, frontal lobe, vestibular, or Parkinsonian. In the observational gait assessment, the use of a mobility aid did not necessarily label an individual as having an unsteady gait if ambulation with a gait aid was unremarkable. Variables from the interRAI used to describe the study sample are presented in a footnote to Table 1.
Table 1.
Baseline Characteristics of Study Participants by Fall Status Attained at End of Study Follow-Up Period (n=90)
| Variable |
Frequency by fall status at the end of the study |
|||
|---|---|---|---|---|
|
Complete Sample (n=90) |
Fallers (n=24) |
Non-fallers (n=66) |
||
| Mean age (SD) | 79.7 (4.8) | 80.8 (2.5) | 79.2 (5.3) | |
| Gender (% male) | 63% | 67% | 62% | |
| (a) | Questionnaire: | |||
| Self-rated health (reported as good, very good, or excellent) | 73 (81%) | 20 (83%) | 53 (79%) | |
| Vision checked in last year | 71 (79%) | 21 (88%) | 51 (77%) | |
| Self-reported balance problems | 15 (17%) | 6 (25%) | 9 (13%) | |
| Self-reported lower-extremity weakness (difficulty with sit to stand) | 14 (16%) | 5 (21%) | 9 (13%) | |
| Self-reported serious foot problems | 6 (7%) | 1 (4%) | 5 (9%) | |
| (b) | Clinical Assessment: | |||
| BBS (SD) | 53.8 (3.2) | 53.1 (3.8) | 53.6 (3.8) | |
| Functional LE weakness | 2 (2%) | 2 (4%) | 0 (0%) | |
| Four or more prescription medications | 53 (59%) | 16 (67%) | 37 (56%) | |
| Impaired vision* | 8 (8%) | 2 (8%) | 6 (9%) | |
| Unsteady gait* | 1 (1%) | 0 (0%) | 1 (2%) | |
| Use of a mobility aid (cane or 4 wheeled walker) | 5 (6%) | 1 (4%) | 4 (6%) | |
| Cognitive impairment* | 2 (2%) | 0 (0%) | 2 (3%) | |
| Limits activity due to fear of falling | 3 (3%) | 1 (4%) | 2 (3%) | |
| Dependency in basic ADL* | 1 (1%) | 1 (4%) | 0 (0%) | |
BBS=Berg Balance Scale; LE=lower extremity; ADL=activities of daily living
Definitions of variables from interRAI Community Health Assessment: impaired vision: the inability to read fine detail in adequate light with glasses if needed, or the presence of eye pathology (cataracts or glaucoma); unsteady gait: abnormality on observational gait; cognitive impairment: participant unable to make independent decisions that are consistent, reasonable, and safe in organizing his or her day; dependency in basic activities of daily living: anything less than fully independent in the activities of bed mobility, locomotion at home, dressing of upper body, dressing of lower body, personal hygiene, eating, and bathing.
An additional study assessment included the number of prescription medications and the Berg Balance Scale (BBS), a valid and reliable scale for the assessment of balance in older adults.15–17 The BBS consists of 14 balance tasks, each scored on a scale of 0 to 4 (0=unable to perform the task; 4=the task is performed independently). The maximum possible score of 56 indicates no identified balance difficulties; lower scores represent increasing balance impairment, associated with greater risk of falling. Prescription medication, in particular the threshold of four or more medications, is also a prominent risk factor for falls.1–3
Independent Variables
All independent variables of interest were identified a priori and were recoded to dichotomous form. These variables were as follows: impaired balance as indicated by BBS score (a threshold of 50/56 was selected based on clinical judgment to represent balance deficit); functional lower-extremity weakness (inability to stand up from a chair without using the arms of the chair); number of prescription medications (threshold of ≥4); and unsteady gait (the presence of any abnormalities on an observational analysis of gait quality).
As a single risk factor is not used clinically in isolation from the presence or absence of other factors, a new variable was created, representing the sum of the risk factors (≥4 prescription medications, functional lower-extremity weakness, impaired balance, and unsteady gait), with a range of possible values from 0 to 4. This variable was treated as an interval variable, assuming that the transition between levels was equal. An analysis of the pattern of the component risk factors in the sum variable was performed to evaluate the distribution of the individual risk factors within each score level.
Outcome
Prospective information on daily falls was collected for 12 months for each participant via a monthly falls log. A “fall” was defined as the person coming to rest unintentionally on the floor or ground. Participants who returned a log indicating a fall were interviewed by telephone by research personnel to obtain detailed information about the specifics of the fall. Data collection for the comprehensive geriatric assessment began in May 2002, and the prospective collection of 1-year follow-up information on falls was completed in January 2004.
Data Analysis
Descriptive statistics from the questionnaire completed in Phase I and from the comprehensive geriatric assessment in Phase II included demographics and measures of functional ability. Information about falls, obtained from fall logs and follow-up telephone interviews—including activities being performed at the time the person fell, time of day, type of injury sustained, and whether medical attention was sought—are presented as descriptive statistics.
For the dichotomous outcome any fall, a modified Poisson regression model was used to generate unadjusted and adjusted risk ratio (RR) estimates (see Appendix).18 In the adjusted analyses, a separate regression model for each variable was applied, with age, sex, and study treatment arm treated as confounders. The study arm of the PPFV was used as a variable for adjustment in the multivariable analysis, as the analysis included both individuals from the SGS arm of the intervention study (Phase II) and individuals who reported no modifiable risk factors for falling on the questionnaire (open arm in Phase II). The inclusion of this variable was intended to address potential residual confounding by study arm, even though there was no overall treatment effect in Phase II. The presence of effect-measure modification was evaluated for each model prior to the estimation of the adjusted RR estimates.
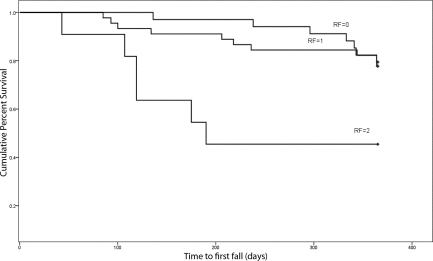
A Kaplan-Meier curve of cumulative survival for time to first fall, measured in days and stratified by number of risk factors, was plotted. A Cox proportional hazard analysis was performed to evaluate time to first fall (in days), generating unadjusted and adjusted hazard ratio (HR) estimates. A separate regression model was applied for each risk-factor variable, with age, sex, and study treatment arm as confounders. The presence of effect-measure modification was evaluated for each model prior to estimation of adjusted HR estimates. Regression diagnostics for the proportional hazards assumption were performed using Schoenfeld residuals.19
RESULTS
Baseline characteristics of the sample are presented in Table 1. Over a 1-year period, 24 people (27%) fell, 8 (9%) of whom sustained recurrent falls (≥2 falls), for a total of 35 falls. The most common activities that participants were performing at the time they fell were walking on the level (31%), negotiating stairs (17%), and sleeping (i.e., participant fell out of bed while asleep; 8%). The most common time for falling was morning (31%), and the most common type of injury reported was “bruises, scrapes, or cuts” (40%). Only one fracture was reported, and the majority of people (69%) were able to get up independently after falling. The average time to first fall was 214 days, with a range of 43 to 364 days. The 25th percentile was 119 days, and the 75th percentile was 333 days, for an interquartile range of 214 days. The Kaplan-Meier survival curve indicates that the time to first fall decreased as the number of risk factors increased and that the percentage of people who fell increased with increasing number of risk factors (see Figure 2). Fall risk over the 12-month period was 21% for zero risk factors, 22% for one risk factor, 60% for two risk factors, and 100% for three risk factors.
Figure 2.
Kaplan-Meier survival curve showing time to first fall (in days), over a 1-year period, in a sample of community-dwelling older adults without a history of falls (n=90), stratified by number of risk factors (RF)—functional lower-extremity weakness, balance impairment, and ≥4 prescription medications—identified on a comprehensive geriatric assessment
The variable for total number of risk factors of interest in the sample showed that 30 (33%) people had zero risk factors, 44 (49%) had one, 15 (17%) had two, and a single individual (1%) had all three risk factors present. Four or more prescription medications dominated the category of one risk factor (89%), while impaired balance and prescription medications (≥4) dominated the category of two risk factors (60%); 79% of participants with a new fall had one or more of the risk factors identified at the baseline clinical assessment.
BBS scores ranged from 43 to 56; 13 people (14%) had scores below 50. Of these 13, 7 (8%) fell and 6 (7%) did not fall during the follow-up period. Of the total sample, 67% had BBS values at 55 or 56, representing a ceiling effect among this high-functioning group of older adults. Average and median BBS scores were identical for fallers and non-fallers.
Results from the regression analyses are presented in Tables 2 and 3. Effect-measure modification was not statistically significant using either regression-modelling technique. The magnitude and statistical significance of associations were consistent between the Poisson and Cox proportional hazards regression analyses, except for functional lower-extremity weakness, reflecting the small number of people identified with this impairment, which led to unstable estimates. For the individual risk factors in the adjusted analyses, increased risk of any fall and decreased time to first fall showed statistically significant associations with functional lower-extremity weakness and BBS score (<50/56). The number of prescription medications (≥4) also demonstrated an increased association with falling, though this association was not statistically significant in adjusted analyses. An unsteady gait was not associated with an increased risk of falling in any analysis (data not presented).
Table 2.
Unadjusted and Adjusted Relative Risk Estimates and 95% Confidence Intervals for Fall Risk Factors Determined during a Comprehensive Geriatric Assessment for the Outcome Any Fall over 12 Months of Follow-Up (each risk factor was analyzed in a separate regression analysis)
| Relative Risk for Falling Over 12 Months (95% CI) |
|||||
|---|---|---|---|---|---|
| Regression Model |
Risk Factor Variable | Unadjusted | p | Adjusted* | p |
| 1. | Functional LE weakness | 4.00 (1.30–5.84) | <0.0001 | 5.21 (2.22–12.22) | 0.0001 |
| 2. | BBS score (<50/56) | 2.44 (1.18–4.28) | 0.008 | 4.12 (1.32–12.80) | 0.01 |
| 3. | Number of prescription medications (≥4) | 1.40 (0.70–2.92) | 0.38 | 1.31 (0.63–2.75) | 0.47 |
| 4. | Number of risk factors score† (per unit increase in score) | 1.73 (1.14–2.62) | 0.01 | 2.00 (1.13–3.56) | 0.02 |
CI=confidence interval; LE=lower extremity; BBS=Berg Balance Scale
Adjusted for age, gender, and treatment arm of the Project to Prevent Falls in Veterans study
Sum of dichotomous variables: balance impairment (BBS score <50/56), functional LE weakness (unable to stand up from chair without using the arms of the chair), and number of prescription medications (≥4)
Table 3.
Unadjusted and Adjusted Hazard Ratio Estimates and 95% Confidence Intervals for Fall Risk Factors Determined during a Comprehensive Geriatric Assessment for the Outcome Any Fall over 12 Months of Follow-Up (each risk factor was analyzed in a separate regression analysis)
| Hazard Ratio for Time to First Fall (95% CI) |
|||||
|---|---|---|---|---|---|
| Regression Model |
Risk Factor Variable | Unadjusted | p | Adjusted* | p |
| 1. | Functional LE weakness | 11.58 (2.48–54.09) | 0.002 | 15.00 (2.58–87.26) | 0.003 |
| 2. | BBS score (<50/56) | 3.51 (1.45–8.49) | 0.005 | 6.41 (1.68–22.46) | 0.006 |
| 3. | Number of prescription medications (≥4) | 1.55 (0.66–3.62) | 0.31 | 1.45 (0.61–3.42) | 0.40 |
| 4. | Number of Risk Factors score† (per unit increase in score) | 2.25 (1.28–3.97) | 0.005 | 2.58 (1.30–5.15) | 0.007 |
CI=confidence interval; LE=lower extremity; BBS=Berg Balance Scale
Adjusted for age, gender, and treatment arm of the Project to Prevent Falls in Veterans study
Sum of dichotomous variables: balance impairment (BBS score <50/56), functional LE weakness (unable to stand up from chair without using their arms), and number of prescription medications (≥4).
Because of the small number of study participants demonstrating deficits in gait, the results presented for the total number of risk factors include only functional lower-extremity weakness, impaired balance (BBS score<50), and ≥4 prescription medications. This variable was analyzed in the categories of 0, 1, and 2+ risk factors. In adjusted analyses, the RR for sustaining any fall over 12 months was 2.00 (95% CI: 1.13–3,56) for each unit increase in the number of risk factors. The adjusted HR was 2.58 (95% CI: 1.30–5.15) for each unit increase in the risk-factor score.
DISCUSSION
Current clinical practice guidelines recommend no more than yearly monitoring for fall risk among older adults with a negative recent fall history.1,2,4 The important contribution of this study is the finding that the absence of a recent fall history does not preclude identification of known risk factors for falling by clinical assessment. This study identified functional lower-extremity weakness and impaired balance in isolation as being associated with the transition in status from non-faller to faller. When the effect of all risk factors in the presence of one another was evaluated, fall risk doubled, and time to first fall decreased for each risk factor present. These findings are consistent with previous work that has demonstrated increased fall risk with an increase in the number of risk factors among general populations of older adults,6,8,20–22 but the present study found a larger magnitude of effect.
Prospective studies evaluating fall risk in older adults without a recent fall history are limited. Hill et al.,9 whose study included only healthy community-dwelling older women without a history of falling over a 12-month period, found an annual fall risk of 49%, as compared to the current study's finding of 27%. The variation may be partially explained by the fact that their sample was limited to women, who are at increased risk of falling compared to men.23,24
In the present study, only one of the participants who fell had a finding of “unsteady gait.” This individual also had a BBS score below 50 and was taking multiple medications. None of the participants using a mobility aid was assessed as having an unsteady gait. It may be argued that the use of a mobility aid is indicative of an underlying problem with gait. A sensitivity analysis with “gait impairment” defined as the use of a mobility aid and/or an unsteady gait produced a RR and HR with a protective effect, although this effect was not statistically significant (results not presented). This expanded definition of gait impairment may exert a protective effect, as use of a mobility aid may limit participation in activities or make a person more aware of potentially hazardous situations; the end result is that function is better matched to the person's physical abilities, which helps in avoiding falls.
A systematic review and meta-analysis by Moreland et al.25 reported a pooled odds ratio estimate for lower-extremity weakness of 1.66 (95%CI: 1.20–2.29) for any fall in community-dwelling older adults. Studies included in the analysis represented a heterogeneous population of community-dwelling older adults with and without a history of falling. This review demonstrated the importance of lower-extremity weakness in identifying fallers, but it did not demonstrate whether this is a significant factor in the transition from non-faller to faller status.
Participants in the present study represented a relatively high-functioning group of older adults with few limitations, though fall events were still common over the period of follow-up. Interestingly, the activities being performed at the time of these falls were not high-risk activities but those necessary for normal daily functioning, such as walking on level surfaces and negotiating stairs. The same finding was reported by Hill et al.9 In contrast, Speechley and Tinetti26 found that people with high function were more likely to fall during displacing activities and in the presence of environmental hazards, an association that was not replicated here.
While a fall resulting from an overwhelming hazard can happen to any individual, not just the older adult, a fall that occurs during the performance of normal activities, without reported hazards, by an older adult may indicate that the person is early in the transition to functional frailty. The high percentage of participants in the present study who self-reported good health may indicate continued participation in their usual activities, which may have exposed them to more situations more likely to result in a fall. This finding highlights the importance of evaluating fall risk before mobility and overall functional ability have started to deteriorate.
While the complement of risk factors for the transition in status from non-faller to faller was not different within the study sample than among the general population of community-dwelling older adults, the magnitude of risk was elevated. In particular, a recent systematic review and meta-analysis provided a summary estimate for falls due to balance impairment at a relative risk of 1.42 (95% CI: 1.08–1.85).27 The calculated risk in this study due to balance impairment was 2.44 (95% CI: 1.18–4.28), meaning that the impairment precedes falls and is not just a consequence of falling.
In their systematic review, Ganz et al.28 recommended adding assessment of balance and gait for older adults without a history of falling. Lamb et al.29 found that self-report of balance problems while walking followed by a clinical assessment of lower-extremity strength was the most effective sequence for fall screening of older women with a disability and a negative fall history. The present results strengthen support for these recommendations and reinforce the value of investing the extra time to perform the BBS in conjunction with the sit-to-stand test for the functional evaluation of lower-extremity strength. Interestingly, the latest Cochrane review of interventions to prevent falls in community-dwelling older adults does not make any recommendations for people who are identified with risk factors but have no history of falling.30
Previous research has demonstrated that the BBS does not perform well in a dichotomous format in a heterogeneous sample of community-dwelling older adults with and without a history of falling.31 The threshold BBS score of 50 used in the present study was chosen a priori, and a subsequent post hoc sensitivity analysis found that this value optimized the RR for the outcome any fall in both unadjusted and adjusted analyses The sample was homogeneous for no recent fall history; a threshold value of 50 cannot be extrapolated to other populations without further confirmatory evaluation of its utility in a larger prospective study.
An important strength of this study is that the selection of variables was not dictated by the statistical significance of variables in the bivariate analyses. The a priori specification of variables known to be potentially modifiable fall risk factors is a strength of this analysis because it was grounded in previous research with community-dwelling older adults1–9 and framed within a theory of factors that contribute to the functioning of postural stability.32
The prospective design of the original study, with a comprehensive geriatric assessment at baseline for all participants and the use of fall logs to collect falls data, optimized the reporting of fall events.33 Contact with study participants when falls were reported enhanced data collection, and contact with participants who did not submit calendars helped to maximize follow-up of study participants. As all participants had volunteered to take part in the study, it was felt that there would not be a reporting bias by gender. Participants were aware that the study was supported by VAC, and this partnership may have encouraged accurate reporting of events.
LIMITATIONS
Falls were a common event in this study and represent an important public health concern. From a mathematical and regression modelling perspective, however, the number of fallers was small; the absolute number of people who fell limited the maximum number of variables that could be entered into the regression models to preserve statistical power.34–38 The variable number of risk factors was used to evaluate the magnitude of fall risk when the risk factors are considered in the presence of one another.
In addition, measures of absolute risk, such as attributable risk percentage and population risk percentage, can provide valuable information that can be useful in establishing how many falls could be prevented by eliminating exposure to risk factors.37 The calculation of absolute risk values with meaningful confidence intervals was not possible in the current study, however. Nonetheless, considering the limited research on the transition of non-fallers to fallers, this study represents a valuable contribution to the literature. Studies conducted on larger samples will add valuable public-health information on the impact of risk factors and confirm the robustness of the associations reported here.
The use of prospective falls data derived from an intervention study might be viewed as a limitation. The intervention—specific information on preventing falls—was provided to participants based on the risk factors identified by the questionnaire and the geriatric assessment. Since all groups were exposed to fall-prevention information, this exposure may have produced a uniform decrease in the number of falls over the 1-year follow-up period across groups. The results may therefore underestimate the association between the baseline risk factors and future fall risk, producing conservative estimates of association. The use of data from two of the three arms of an intervention study is not a design flaw, however: there was no detected treatment effect from the intervention, which provided reasonable grounds to combine data for prognostic research.38 The PPFV treatment group was included as a covariate in the adjusted analyses to account fully for any differences that the intervention may have introduced. Sensitivity analysis including and excluding the PPFV treatment group variable (data not presented) did not change either the statistical significance or the magnitude of association in any significant way (<10%).
CONCLUSIONS
Falls were a common outcome in this sample of community-dwelling older adults who reported no history of falling at the beginning of the study. Known and potentially modifiable risk factors for falling were present in the majority of people who fell. Both functional lower-extremity muscle weakness (identified by a simple clinical assessment procedure) and a BBS score below 50/56 were associated with the transition from non-faller to faller over 1 year and with decreased time to first fall. Fall risk doubled for each unit increase in the number of risk factors identified through the clinical assessment, which provides a means of identifying individuals at risk for falling in this population of community-dwelling older adults. Ongoing research is required to identify additional risk factors associated with the transition from non-faller to faller status and effective interventions that can modify this progression.
KEY MESSAGES
What Is Already Known on This Topic
The risk factors for falls among community-dwelling older adults are well established in the literature. Less well understood are the risk factors associated with the transition from non-faller to faller status. The majority of studies on fall risk factors include people with and without a history of falling, and clinical practice guidelines on fall prevention provide minimal recommendations for people without a history of falling. Because even a single fall can have serious consequences (morbidity, mortality, and disability) in an older adult's life, the prevention of first falls has important implications for public health.
What This Study Adds
This prospective study found that falls were common among high-functioning community-dwelling older adults. The majority of activities participants were performing at the time of their falls were not high-risk activities but those necessary for normal daily functioning, such as walking and using stairs. The risk factors of functional lower-extremity weakness and balance impairment in isolation were associated with an increased risk of falling and decreased time to first fall. When the impact of all risk factors was considered together, fall risk doubled for each unit increase in the number of risk factors (functional lower-extremity weakness, balance impairment, and ≥4 prescription medications). Older adults who do not report a history of falling in the previous 12 months should be screened for the presence of these potentially modifiable risk factors.
Appendix
Calculation of unadjusted relative risk estimates using 2×2 contingency tables. The relative risk is defined as the risk of the outcome of interest among the exposed compared to the risk of the outcome of interest among the unexposed.
For example, unadjusted relative risk calculation for the variable prescription medications (≥4) is as follows:
| Outcome | |||
| Positive (Fallers) |
Negative (Non-fallers) |
||
| Exposure | Positive (≥4) | 16 |
37 |
| Negative (<4) | 8 |
||
| Totals | 24 | 66 | |
| Relative risk = | risk of being a faller among the exposed (≥4 prescription medications) |
||
| risk of being a faller among the un-exposed (<4 prescription medications) | |||
| = | (16/(16+37)) |
||
| (8/(8+29)) | |||
| = | 0.3019 / 0.2162 | ||
| = | 1.3970 | ||
| = | 1.40 | ||
Muir SW, Berg K, Chesworth BM, Klar N, Speechley M. Modifiable risk factors identify people who transition from non-fallers to fallers in community-dwelling older adults: a prospective study. Physiother Can. 2010;62:358–367
References
- 1.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls: a prospective study. J Am Med Assoc. 1989;261:2663–8. doi: 10.1001/jama.261.18.2663. [PubMed] [Google Scholar]
- 2.American Geriatrics Society; British Geriatrics Society; American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;43:664–72. doi: 10.1046/j.1532-5415.2001.49115.x. [PubMed] [Google Scholar]
- 3.National Institute of Clinical Excellence [NICE] Clinical guideline 21: the assessment and prevention of falls in older people [Internet] London: The Institute; 2004. [cited 2005 Jun 21]. Available from: http://guidance.nice.org.uk/CG21/Guidance/pdf/English. [Google Scholar]
- 4.Moreland J, Richardson J, Chan DH, O'Neill J, Bellissimo A, Grum RM, et al. Evidence-based guidelines for the secondary prevention of falls in older adults. Gerontology. 2003;49:93–116. doi: 10.1159/000067948. doi: 10.1159/000067948. [DOI] [PubMed] [Google Scholar]
- 5.Moylan KC, Binder EF. Falls in older adults: risk assessment, management and prevention. Am J Med. 2007;120:493–7. doi: 10.1016/j.amjmed.2006.07.022. doi: 10.1016/j.amjmed.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Thurman DJ, Stevens JA, Jaya KR. Assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70:473–9. doi: 10.1212/01.wnl.0000299085.18976.20. doi: 10.1212/01.wnl.0000299085.18976.20. [DOI] [PubMed] [Google Scholar]
- 7.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 8.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 year and older. J Gerontol. 1989;44(4):M112–7. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 9.Hill K, Schwarz J, Flicker L, Carroll S. Falls among healthy, community-dwelling older women: a prospective study of frequency, circumstances, consequences and prediction accuracy. Aust N Z J Public Health. 1999;23(1):41–8. doi: 10.1111/j.1467-842x.1999.tb01203.x. doi: 10.1111/j.1467-842X.1999.tb01203.x. [DOI] [PubMed] [Google Scholar]
- 10.Speechley M, Belfry S, Borrie MJ, Jenkyn KB, Crilly R, Gill DP, et al. Risk factors for falling among community-dwelling veterans and their caregivers. Can J Aging. 2005;24:261–74. doi: 10.1353/cja.2005.0083. doi: 10.1353/cja.2005.0083. [DOI] [PubMed] [Google Scholar]
- 11.interRAI. Institute of Gerontology University of Michigan [homepage on the Internet] Ann Arbor, MI: interRAI; c2006. [cited 2007 May 6]. Available from: http://www.interrai.org. [Google Scholar]
- 12.Morris JN, Bernabei R, Ikegami N, Gilgen R, Frijters D, Hirdes JP, et al. RAI-HOME CARE (RAI-HC) assessment manual for version 2.0: primer on use of the Minimum Data Set-Home Care (MDS-HC) version 2.0 and the Client Assessment Protocols (CAPS)—for use in Canada and the United States. Washington, DC: interRAI; 2002. [Google Scholar]
- 13.Landi F, Tua E, Onder G, Carrara B, Sgadari A, Rinaldi C, et al. Minimum Data Set for Home Care: a valid instrument to assess frail older people living in the community. Med Care. 2000;38:1184–90. doi: 10.1097/00005650-200012000-00005. doi: 10.1353/cja.2005.0083. [DOI] [PubMed] [Google Scholar]
- 14.Morris JN, Fries BE, Steel K, Ikegami N, Bernabei R, Carpenter GI, et al. Comprehensive clinical assessment in community setting: applicability of the MDS-HC. J Am Geriatr Soc. 1997;45:1017–24. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- 15.Berg KO, Wood-Dauphinee SL, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–11. doi: 10.3138/ptc.41.6.304. [Google Scholar]
- 16.Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73:1073–80. [PubMed] [Google Scholar]
- 17.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;S2:S7–11. [PubMed] [Google Scholar]
- 18.Zou GY. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 19.Kleinbaum DG, Klein M. Survival analysis: a self-learning text. 2nd ed. New York: Springer; 2005. [Google Scholar]
- 20.vanBemmel T, Vandenbroucke JP, Westendorp RGJ, Gussekloo J. In an observational study elderly patients had an increased risk of falling due to home hazards. J Clin Epidemiol. 2005;58:63–7. doi: 10.1016/j.jclinepi.2004.06.007. doi: 10.1016/j.jclinepi.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. 1986;80:429–34. doi: 10.1016/0002-9343(86)90717-5. [DOI] [PubMed] [Google Scholar]
- 22.Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43:1214–21. doi: 10.1111/j.1532-5415.1995.tb07396.x. doi: 10.1016/0002-9343(86)90717-5. [DOI] [PubMed] [Google Scholar]
- 23.Campbell AJ, Spears GF, Borrie MJ. Examination by logistic modeling of the variables which increase the relative risk of elderly women falling compared to elderly men. J Clin Epidemiol. 1990;43:1415–20. doi: 10.1016/0895-4356(90)90110-b. doi: 10.1016/0895-4356(90)90110-B. [DOI] [PubMed] [Google Scholar]
- 24.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005;11:115–9. doi: 10.1136/ip.2004.005835. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52:1121–9. doi: 10.1111/j.1532-5415.2004.52310.x. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- 26.Speechley M, Tinetti ME. Falls and injuries in frail and vigorous community elderly persons. J Am Geriatr Soc. 1991;39:46–52. doi: 10.1111/j.1532-5415.1991.tb05905.x. [DOI] [PubMed] [Google Scholar]
- 27.Muir SW, Berg K, Chesworth B, Klar N, Speechley M. Quantifying the magnitude of risk for balance impairment on falls in community-dwelling older adults: a systematic review and meta-analysis. J Clin Epidemiol. 2010;63:389–406. doi: 10.1016/j.jclinepi.2009.06.010. doi: 10.1016/j.jclinepi.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 28.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? J Am Med Assoc. 2007;297:77–86. doi: 10.1001/jama.297.1.77. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 29.Lamb SE, McCabe C, Becker C, Fried LP, Guralnik JM. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: the Women's Health and Aging Study. J Gerontol A-Biol. 2008;63A:1082–8. doi: 10.1093/gerona/63.10.1082. [DOI] [PubMed] [Google Scholar]
- 30.Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Db Syst Rev. 2009;2 doi: 10.1002/14651858.CD007146.pub2. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88:449–59. doi: 10.2522/ptj.20070251. doi: 10.2522/ptj.20070251. [DOI] [PubMed] [Google Scholar]
- 32.Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(S2):ii7–11. doi: 10.1093/ageing/afl077. doi: 10.1093/ageing/afl077. [DOI] [PubMed] [Google Scholar]
- 33.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53:2190–4. doi: 10.1111/j.1532-5415.2005.00509.x. doi: 10.1111/j.1532-5415.2005.00509.x. [DOI] [PubMed] [Google Scholar]
- 34.Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 35.Steyerberg EW, Eijkemans MJC, Harrell FE, Habbema JDF. Prognostic modeling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Stat Med. 2000;19:1059–79. doi: 10.1002/(sici)1097-0258(20000430)19:8<1059::aid-sim412>3.0.co;2-0. doi: 10.1002/(SICI)1097-0258(20000430)19:8<1059::AID-SIM412>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 36.Sun GW, Shook TL, Kay GL. Inappropriate use of bivariate analysis to screen for risk factors use in multivariable analysis. J Clin Epidemiol. 1996;49:907–16. doi: 10.1016/0895-4356(96)00025-x. doi: 10.1016/0895-4356(96)00025-X. [DOI] [PubMed] [Google Scholar]
- 37.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:W163–94. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. doi: 10.1371/journal.pmed.0040297. [DOI] [PubMed] [Google Scholar]
- 38.Moons KGM, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? Brit Med J. 2009;338:1317–20. doi: 10.1136/bmj.b375. doi: 10.1136/bmj.b375. [DOI] [PubMed] [Google Scholar]