Abstract
Objective
To explore whether standardized survey instruments and objective performance measures differentiate traditional constructs of sleepiness and fatigue among a sample of postpartum mothers. Additionally, we wanted to explore the independent associations among these measures with actigraphically measured nocturnal sleep variables.
Method
Seventy-nine postpartum mothers’ subjective sleepiness, fatigue, and performance measures (Stanford Sleepiness Scale [SSS], Epworth Sleepiness Scale [ESS], Visual Analogue of Fatigue Scale [VAS], Profile of Mood States [POMS] subscale items, and the Psychomotor Vigilance Test [PVT]) and objective actigraphically measured sleep were collected during postpartum week 11. A Principal Components Analysis was calculated, then regressions were calculated among resulting factors and among individual measures with total sleep time and sleep efficiency.
Results
Three factors accounted for 83.84% of model variance. Factor 1 (41.41%) included the SSS, ESS, and the VAS. Factor 2 (28.13%) included only PVT variables. Factor 3 (14.30%) included the two POMS subscale items. Factor 1 was associated with nocturnal sleep time and Factor 2 was associated with sleep efficiency. The ESS was independently associated with nocturnal sleep time, whereas, POMS-Vigor subscale and median reaction time, together, were associated with sleep efficiency.
Conclusion
Among postpartum mothers, standard instruments used to measure sleepiness, fatigue, and performance were distributed among three distinct factors that did not clearly identify traditional sleepiness and fatigue constructs. Objectively measured sleep time and sleep efficiency were associated with specific factors, as well as specific measures, that correspond to sleepiness and fatigue states.
Keywords: Sleepiness, fatigue, postpartum, sleep, actigraphy
INTRODUCTION
Within clinical, research, and applied settings the terms sleepiness and fatigue are often used interchangeably, yet the terms represents distinct constructs.1 Accurate use of these terms is important because they are thought to reflect different etiologies that may lead to increased morbidity and mortality among susceptible populations.
Sleepiness
Sleepiness has been operationally defined as a physiological need2 that reflects an increased drive for sleep when one intends to be awake3 and can be caused by any experience that prevents acquisition of needed sleep. Such experiences include self-imposed insufficient sleep, sleep disorders, and various extrinsic causes that disturb sleep (e.g. infant signaling during the night). Sleepiness and hours of sleep are inversely associated, such that less sleep leads to more sleepiness.4 Furthermore, the magnitude of sleepiness occurs in grades; the greater the magnitude of sleepiness, the more likely one is to fall asleep during waking activities.3 Sleepiness can be reliably and validly indexed objectively through use of assessments such as the Multiple Sleep Latency Test,5 or subjectively using standard instruments, such as the Stanford Sleepiness Scale6 and the Epworth Sleepiness Scale.7
Fatigue
In contrast, fatigue is operationally defined as the subjective report of exhaustion and decreased capacity for both physical and/or mental activity.8 Fatigue is a state thought to be comprised of multiple dimensions, such as physical and mental fatigue9 and is associated with fibromyalgia10 and chronic fatigue syndrome.11 In an assessment of sleep disorders, sleepiness, and fatigue among a sample diagnosed with Chronic Fatigue Syndrome, Le Bon and colleagues suggest that fatigue is neither a byproduct of sleep disorders, nor a likely expression of sleepiness.11 Fatigue can be subjectively assessed using various techniques such as a visual analogue scale.12
Though sleepiness and fatigue have been clearly identified as separate constructs, there are known relations between them. Among those with sleep disorders, perceived fatigue was unrelated to daytime sleepiness measured with the Multiple Sleep Latency Test.13 Lichstein and colleagues explain that sleepiness results from being awake, whereas fatigue is a result of exertion. However, they also explain that an interaction exists in which wakefulness can increase fatigue and exertion can increase sleepiness. Furthermore, individuals differ in their susceptibility to experiencing sleepiness and fatigue. In a large community sample of women, sleepiness and fatigue were significantly associated, but each had distinct risk factors.14
Sleepiness and Fatigue among Postpartum Mothers
The interaction between sleepiness and fatigue may be especially pronounced among postpartum women. Postpartum mothers are an ideal population among which to evaluate sleepiness and fatigue. Such women make up an ecologically valid, non-experimental population who often experience high levels of sleep disturbance in the absence of a sleep disorder. Fatigue has been shown to increase in association with sleep deprivation during the postpartum period.15 Furthermore, mothers experience increased levels of both sleepiness16 and fatigue17 during pregnancy and throughout the postpartum period.18 Postpartum fatigue levels may persist long into the postpartum period. Beyond the first postpartum year, primiparous women have been reported to be more fatigued than nulliparous women.19 Furthermore, these postpartum mothers were at least as fatigued when their infants were 14 to 19 months old as when their infants were 6 weeks old.19
Experiences that contribute to, and are results of postpartum sleepiness and fatigue have been well-described.17,20 Dennis and Ross21 found that infant sleep, maternal fatigue, and specifically maternal sleep disturbance are strongly associated with higher maternal depressive symptoms. Thus, identification of sleepiness and fatigue among postpartum women may be particularly important for appropriate identification of those at risk for psychopathology.22 The experiences of sleepiness and fatigue may have far reaching consequences for postpartum mothers, their families, and society because of both their childcare responsibilities and their presence in the workforce.
Differentiating sleepiness and fatigue may be challenging.1,23,24 The psychometric properties of several sleep outcome measures are at the center of some scholarly debate, specifically regarding their identification of sleepiness versus fatigue.25 Current research indicates that operationalization of variables, assessment process, and symptom-specific interventions need to be established and implemented when dealing with the constructs of sleepiness and fatigue.26 Furthermore, there has been a call for further exploration of the relations among instruments used to identify sleepiness and fatigue.26
The primary purpose of the current study was to use a convenient dataset from a larger study of postpartum mothers to explore how standard instruments traditionally used to measure sleepiness, fatigue, and performance may be interrelated among this unique population. The secondary purpose was to explore the independent associations of sleepiness, fatigue, and performance measures with actigraphically measured nocturnal sleep time and sleep efficiency.
METHODS
The data are from a longitudinal study of postpartum sleep disturbance27 approved by the West Virginia University Office of Research Compliance (Institutional Review Board). Participants were administered informed consent and Health Insurance Portability and Accountability Act (HIPAA) authorization prior to participation.
Sample
Mothers were recruited via community advertisements. Potential participants were excluded on the basis of premature delivery, pregnancy with multiples, infant admission to the neonatal intensive care unit, history of or current treatment for major depressive disorder, or a score >16 on the Center for Epidemiologic Studies Depression Scale, a well-validated 20-item survey used to determine current risk for major depressive disorder.28 Data from 79 postpartum mothers during their 11th postpartum week were analyzed (24 women participated from postpartum week 8–16; 55 participated from postpartum week 1–12. Participant demographics are shown on Table 1.
Table 1.
Descriptive statistics for demographic, sleepiness, fatigue, psychomotor performance, and actigraphically measured sleep variables (N = 79)
| - | Mean | SD | Range |
|---|---|---|---|
| Age (years) | 27.4 | 4.7 | 18.4 – 40.1 |
| Education (years) | 16.2 | 2.8 | 10 – 22 |
| White | 92.2% | – | – |
| Married/Living with partner | 87.3% | – | – |
| Primiparious | 69.6% | – | – |
| ESS Total Score | 8.2 | 4.0 | 0.1 – 22.4 |
| SSS | 3.1 | 1.0 | 1.4 – 6.0 |
| VAS | 49.2 | 17.3 | 5.8 – 86.0 |
| Median RT (ms.) | 391.9 | 75.6 | 234.0 – 657.0 |
| Lapse Frequency | 9.2 | 6.1 | 0.2 – 27.8 |
| POMS: ‘Vigor’ | 17.1 | 5.6 | 3.0 – 28.0 |
| POMS: ‘Fatigue’ | 7.8 | 4.3 | 0.0 – 18.0 |
| * Sleep Time (min) | 436.1 | 51.9 | 273.0 – 543.4 |
| * Sleep Efficiency (%) | 86.4 | 6.0 | 69.1 – 96.2 |
Note. Descriptive data for all variables except for demographic information were averaged within postpartum weeks 11.
Indicates actigraphically-measured values calculated from the identified nocturnal sleep period. Total sleep time = minutes calculated as sleep within the sleep period (time from sleep onset to final morning awakening). Sleep efficiency = minutes of sleep during the sleep period divided by the sleep period length [minutes], multiplied by 100. Two participants were missing actigraphy data, two participants were missing PVT data, and one participant was missing experience sampling method data. ESS: Epworth Sleepiness Scale; SSS: Stanford Sleepiness Scale; VAS: Visual Analogue of Fatigue Scale; RT: Reaction Time; POMS: Profile of Mood States.
Measures
Computerized Experienced Sampling Method
Participants used computerized experience sampling method29 to self-administer the visual analogue of fatigue (VAS) scale,12 the Stanford Sleepiness Scale (SSS),6 and the Epworth Sleepiness Scale (ESS)7 using a Palm Zire 72 personal digital assistant (PDA) with customized software (Bruner Consulting Co.). The 100-point VAS was a single item fatigue scale to examine tiredness/fatigue.12 The VAS was usedto rate, “How tired/fatigued do you feel RIGHT NOW?” (0 = not at all tired/fatigued, 100 = very tired/fatigued). The SSS measures how sleepy one feels in their current state; the scale is 1–7 and higher scores represent greater sleepiness. The ESS measures the susceptibility of falling asleep, on a scale of 0–3, in 8 different real-life situations. Total scores on this scale can range from 0–24 where higher scores represent greater sleepiness. The ESS is typically used to reflect one’s general state, but for the current study was used to reflect one’s current state.
Psychomotor Vigilance Test
The psychomotor vigilance test (PVT)30 was self-administered using customized software (Bruner Consulting, Longmont, CO) on the PDA, similar to previous versions31 This PVT is a simple reaction time (RT) task developed to measure sustained attention using a bull’s-eye stimulus and has a 10 ms sensitivity resolution. Each 5-minute trial consists of the presentation of approximately 39–56 stimuli at random interstimulus intervals. RT measured using the PVT is a valid index of performance impairment due to sleep loss (for a review see Lim and Dinges32). PVT trial measures included median RT and frequency of lapses (i.e. the number of RTs per trial ≥ 500 msec.).
Prior to the calculation of reaction time values, a response time parameter was set to minimize the effect of extreme reaction time responses that may have resulted from the field-based self-administration of the PVT.33 Based on preliminary work, a criterion cutoff value was established at two standard deviations above the mean for all response data; that is, reaction time responses ≥1,314 msec. were excluded from the calculation of reaction time values for each trial. This criterion cutoff value resulted in removal of < 2% of all responses within all trials.
The Profile of Mood States
The Profile of Mood States (POMS)34 measures six dimensions of mood: tension-anxiety, depression-dejection, anger-hostility, vigor-activity, fatigue-inertia, and confusion-bewilderment. The POMS yields a total mood disturbance score as well as subscales for each dimension of mood, and all items have an internal consistency of ≥ .90.34 Respondents for this study were instructed to rate 65 adjectives on a scale of 0 = not at all to 4 = extremely, based on how they felt during the previous week; a higher number for a subscale represents a higher level of the reported mood. The POMS has been used extensively in sleep research.35 For the current study only the Vigor-Activity and Fatigue-Inertia subscales were examined.
Actigraphy
Wrist actigraphy is a valid system for non-intrusive measurement and analysis of sleep/wake periods among adults.36 Actigraphy data were collected using a commercially available system (Mini Mitter Actiwatch-64) with 15-second recording epochs and a standard wake threshold value setting = 40. Siginals were analyzed using Actiware software.
It is recommended that simultaneous behavioral diaries be kept with actigraphy to identify bedtimes, rise times, and times when the actigraph is off.37 Our sleep and actigraph off diary was also PDA-based. The sleep diary and actigraphy signal were corroborated so that the beginning of a sleep period was identified at the beginning of the first eight consecutive epochs (2 minutes) of inactivity following the sleep diary-reported bedtime; the end of a sleep period was identified as the end of the last two consecutive minutes of inactivity preceding the diary-reported wake time. Total sleep time (minutes) and sleep efficiency (minutes of sleep during the sleep period divided by minutes in the sleep period, multiplied by 100) were derived from actigraphy signals during nocturnal sleep periods. To reduce participant burden, participants were not instructed to identify the exact moments of lights-out; therefore, there was no attempt in our study to determine sleep onset latency. Furthermore, participants recorded their time of morning wake which was later corroborated with actigraphy signals.
Procedure
Mothers were asked to wear their actigraph continuously (except when it might get wet), to use their PDA to report their sleep and watch-off diary as events occurred, and to self-administer PVT, sleepiness, and fatigue measures via the PDA. The PVT was self-administered once each day within two hours of awakening and before any caffeine consumption. The PDA-based VAS, SSS, and ESS were completed whenever the mother fed her baby, or following a similar pattern if she returned to work. At the end of postpartum week 11 the POMS was administered, reflecting mood during that week.
Statistical Analyses
Data were analyzed using SPSS version 14.0; a p < 0.05 was considered statistically significant.
Daily PVT, and multi-daily VAS, SSS and ESS measures were each averaged within the study week to provide stable measures and to allow comparison with the POMS subscales. To examine the potential influence of sleep inertia on PVT performance, correlations were calculated between the latency from morning wake until PVT administration and median reaction time and frequency of lapses.
To examine whether these individual subjective and performance measures identify the traditional constructs of sleepiness and fatigue among postpartum women, a principal components analysis (PCA) was conducted with all variables entered into the model. The PCA was conducted with an oblique rotation (Direct Oblimin). An oblique rotation was used because correlations were expected among the sleepiness and fatigue measures; regardless, if the factors were uncorrelated, oblique and orthogonal rotations characteristically yield similar results.38
Once factors were identified by the PCA those factors were used as variables by creating factor values. Since the variables that loaded on the factors were on different measurement scales, the variables in each factor were standardized and the standardized variables that loaded on each factor were averaged to create that factor value.
Four stepwise linear regressions were calculated to examine which PCA factor, as well as which individual measures were most strongly associated with nocturnal sleep time and sleep efficiency. The PCA factors, and the ESS, SSS, VAS, PVT variables, and POMS subscales were entered as independent variables; nocturnal sleep time and sleep efficiency were entered separately as dependent variables. Stepwise regressions were calculated because this analysis was exploratory.
RESULTS
Data from three women were not included in analyses due to actigraph or Palm Pilot malfunction, these women still provided POMS data. Therefore, 79 women were included in the analyses and 76 women contributed complete data. Participant demographics are shown on Table 1. Self-administration of the computerized VAS, SSS, and ESS measures occurred an average of 2.57 (SD = 0.96) times each day. There was no appearance of profile reporting for the VAS, SSS, or ESS; the within subject variability (i.e. average SD from week 11 study weeks) for these measures was VAS = 21.56; SSS = 1.23; ESS = 4.81. For the PVT, there was no evidence of a sleep inertia effect; latency from wake to administration was not significantly correlated with median reaction time (r = .03, p = .80), or frequency of lapses (r = .05, p = .69). Descriptive statistics for the VAS, SSS, ESS, PVT, and actigraphically measured sleep variables are shown on Table 1.
The sample size used for the PCA was adequate38; the participant to item ratio was > 10:1, almost all communalities were >.80, and no minimum loading of any item was lower than .32. Furthermore, the PCA explained a large proportion of variance among this sample.
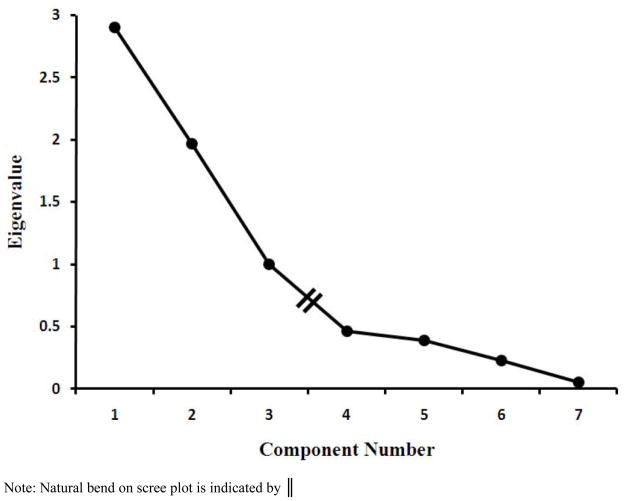
Based on visual inspection of the natural bend on the scree plot (Figure 1), the PCA revealed three factors that explained 83.84% of the total variance in the model (Table 2). Factor one – which explained the most variance – was composed of the VAS, SSS, and ESS, and was labeled ‘subjective report of sleepiness/fatigue’. Factor two was composed of the two PVT variables and was labeled ‘psychomotor performance’. Factor 3 was composed of the POMS subscales and was labeled ‘POMS: Vigor/Fatigue’.
Figure 1.
Scree plot from Principal Components Analysis with seven subjective and performance measures entered into the model.
Table 2.
Rotated factor loadings (Pattern Matrix) for VAS, ESS, SSS, PVT measures, and POMS subscales
| Factor | |||
|---|---|---|---|
| Variable | F 1 | F 2 | F 3 |
| VAS | .90 | .03 | .11 |
| ESS | .88 | −.04 | −.04 |
| SSS | .84 | .12 | −.12 |
| Median RT | .03 | .98 | .01 |
| Lapse Frequency | .07 | .97 | −.05 |
| POMS ‘Vigor’ | .09 | −.17 | .94 |
| POMS ‘Fatigue’ | .24 | −.29 | −.70 |
| Eigenvalue | 2.90 | 1.97 | 1.00 |
| Cumulative variance | 41.41 | 69.54 | 83.84 |
Note. Items in bold indicate significant loading of the variable on the factor. F 1 = Factor 1: subjective report of sleepiness/fatigue; F 2 = Factor 2: psychomotor performance; F 3 = Factor 3: POMS: Vigor/Fatigue. ESS: Epworth Sleepiness Scale; SSS: Stanford Sleepiness Scale; VAS: Visual Analogue of Fatigue Scale; RT: Reaction Time; POMS: Profile of Mood States.
When the 3 factors were entered into two regression models to predict either nocturnal sleep time or sleep efficiency, the ‘subjective report of sleepiness/fatigue’ (β = −.40) was independently associated with nocturnal sleep time (R = .40, F [1,75] = 14.37, p < 0.001); ‘psychomotor performance’ (β = −.30) was independently associated with sleep efficiency (R = . 30, F [1,74] = 7.28, p < 0.01). When all individual variables were entered into the regression models, the ESS (β = −.40) was independently associated with nocturnal sleep time (R = .40, F [1,74] = 13.99, p < 0.001), and together the POMS Vigor subscale (β = .29), and median reaction time (β = −.27) were associated with sleep efficiency (R = .42, F [2, 73] = 7.66, p < 0.01).
DISCUSSION
Exploratory Principal Components Analysis
Standard instruments used to measure sleepiness (SSS, ESS), fatigue (VAS, POMS: Vigor-Activity, POMS: Fatigue-Inertia), and performance (PVT) did not clearly identify traditional sleepiness and fatigue constructs among postpartum mothers. The SSS and the ESS were expected to separate onto one sleepiness factor by themselves; instead, these measures loaded on the same factor with the VAS, which was expected to measure fatigue, not sleepiness. The VAS and the POMS subscales were expected to separate onto a single fatigue factor because previous reports indicate that both POMS subscales ‘Vigor-Activity’ and ‘Fatigue-Inertia’ were significantly associated with visual analogue scales of ‘Energetic’ and ‘Tired’ among a normative sample.39 If the factor that only contained the POMS subscales indicated fatigue, it would be expected to include the VAS. The PVT variables were entered into the PCA to examine their potential relations with the subjective constructs of sleepiness and fatigue among postpartum mothers. The PVT items loaded together; this was somewhat expected, previous reports found that PVT performance is generally a separate construct from other neurobehavioral measures that are sensitive to sleep deprivation40; and more specifically, PVT variables may be distinct from subjective sleepiness and fatigue reports.41
The lack of clearly discrete sleepiness and fatigue factors among postpartum women may reflect their high levels of sleepiness and/or fatigue. Overall, the descriptive statistics revealed that this sample of new mothers demonstrated high levels of impairment on standard instruments that are traditionally used to measure sleepiness, fatigue, and performance. Previous research indicates that as sleep deprivation increases, participants have a blurring of their distinction between state and behavior dimensions of sleepiness.42 Furthermore, some standardized sleep-outcome measures may not clearly identify constructs of sleepiness and fatigue; specifically, standard sleep-outcome measurement instruments—including the SSS and the ESS— are reported to confound the constructs of sleepiness and fatigue.25 Furthermore, the SSS has been found more strongly correlated with fatigue measures than with sleepiness measures.25 The characteristics of these instruments may therefore influence our inability to identify clear constructs of sleepiness and fatigue in the current study.
The method of assessment administration must be carefully considered or tightly controlled when examining sleepiness and fatigue. The three independent factors that emerged from our PCA may have formed based on the mode used for administration of each instrument. Specifically, the three variables administered using ‘computerized experience sampling method’ loaded together, both PVT variables loaded together, and both POMS variables loaded together. This finding suggests that researchers and clinicians who deal with the complex nature of sleepiness or fatigue should be cognizant of the effect that sampling methodology has on data collection and symptom report.
Furthermore, although the difference between the terms sleepiness and fatigue may be apparent to the scientific reader, the terms may seem synonymous to the study participants. The semantic similarity among terms may have contributed to our inability to clearly identify constructs of sleepiness of fatigue; this is considered a general issue within our field.
Independent Associations among Sleep-Outcome Measures and Objective Sleep Indices
The relations between sleep outcome measures and objective sleep were all in their expected directions. These relations indicate that among postpartum women, subjective reports of sleepiness, fatigue, and objective performance measures were associated with specific objective measures of sleep. The ‘subjective report of sleepiness/fatigue’ factor was associated with nocturnal sleep time and the ‘psychomotor performance’ factor was associated with sleep efficiency. Furthermore, the ESS was independently associated with nocturnal sleep time; whereas, POMS: Vigor-Activity subscale and median reaction time were independently associated with sleep efficiency. Together, as sleep disturbance increased (i.e. less total sleep time and efficiency), sleepiness, fatigue, and performance got worse.
This finding indicates that some sleep outcome measures, as well as their combination into factors, may have discriminate abilities to identify specific sleep behaviors. Furthermore, these results lead us to speculate that certain distinct sleep profiles (e.g. discrete deprivation, fragmentation) may lead to specific daytime consequences (e.g. daytime sleepiness, fatigue, and poor psychomotor performance). Although this finding requires further temporal investigation, shared variance among these factors may infer that specific adverse daytime complications, such as sleepiness or fatigue, could potentially be countered by behavioral interventions that focus on a specific aspect of sleep, such as sleep consolidation.
Limitations
Not all possible measures of sleepiness and fatigue were included; for a review of sleepiness and fatigue measures see the review by Shen and colleagues.1 However, for the present longitudinal study in which early postpartum participants were expected to report frequent subjective events, it was important to keep subject burden to a minimum.
Since the current sample comes from a field-based study, participants were unsupervised during PVT administration. Although participants were instructed to terminate and readminister the PVT if a distracting event occurred, unanticipated minor distractions may have played a role in inflating psychomotor performance values, below the criterion cutoff value, which may have reduced their associations with other sleep-outcome measures, as well as actigraphically recorded sleep values. However, the field-based design of this protocol bolsters the ecologically validity of this study and may be seen as one of the study’s strengths. Further, the PVT measures demonstrated high variance that was collapsed across weeks, potentially washing out within subject variability.
The cross-sectional research design of the current study does not allow inference about directionality among variables. However, the current study provides foundational information for future investigations to identify temporal sequences among specific sleep profiles and specific daytime complications among postpartum women.
The current study contains several psychometric limitations that must be noted. The SSS is a scale (widely used) to measure sleepiness, but previous research on this instrument indicated that sleepiness is not unidimensional.43 We therefore cannot extrapolate unequivocally on how the different dimensions of sleepiness, as measured by the SSS, influence the current results. The ESS was administered as a state measure; however, it has only been psychometrically validated as a measure of trait. As reviewed above, fatigue has multiple dimensions, yet the VAS used in the current study only examined a tiredness/fatigue state and the meaning of this state was left to interpretation by the participants. This does not allow for examination of the separate constructs of physical and mental fatigue.
The psychometric limitations reflect constraints that were imposed by using a convenience sample from a larger longitudinal research project, and these limitations may influence the results of the subsequent PCA. Although the measures utilized in the current study do not thoroughly examine the intricacies of sleepiness and fatigue, they have been used to describe these states, and most importantly, demonstrate informative relations with objectively recorded sleep profiles among postpartum women.
CONCLUSION
The current work is in line with the literature that sleepiness and fatigue are puzzling constructs. However, different research approaches help to better conceptualize its features, and therefore guide potential treatments to reduce these experiences.45 Notably, the current work identified that among postpartum women standard sleepiness, fatigue, and performance measures did not unequivocally identify the traditional constructs of sleepiness and fatigue. These measures did however clearly separate into distinct factors; specific factors, as well as individual measures, were associated with distinct objectively measured sleep profiles. The finding that certain sleepiness, fatigue, and performance variables are associated with specific sleep profiles may help guide future investigations and treatments that target specific populations with high levels of daytime sleepiness and/or fatigue.
Acknowledgments
The authors thank the new mothers who participated in the larger study of maternal sleep disturbance. Data collection and processing were carried out with assistance from Megan Clegg-Kraynok, Kayla Williams, Chelsea Costello, Eleanor Santy, Sierra Glowacki, Timothy Dohm, Christine Gould, Aryn Karpinski, Jose Sanchez, Amber Smith, and Mike Verzino. We also thank the anonymous journal Reviewers whose comments and suggestions substantially improved our work. Support: National Institutes of Health Grant R21HD053836 (HMD).
Support: NIH grant R21HD053836(HM-D)
Acronyms
- ESS
Epworth Sleepiness Scale
- SSS
Stanford Sleepiness Scale
- VAS
Visual Analogue of Fatigue Scale
- POMS
Profile of Mood States
- PDA
Personal Digital Assistant
- PVT
Psychomotor Vigilance Test
- RT
Reaction Time
- PCA
Principal Components Analysis
Footnotes
The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shen J, Barbera J, Shapiro CM. Distinguishing sleepiness and fatigue: focus on definition and measurement. Sleep Med Rev. 2006;10:63–76. doi: 10.1016/j.smrv.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Roehrs T, Carskadon MA, Dement WC, Roth T. Daytime sleepiness and alertness. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. Philadelphia: Elsevier Saunders; 2005. pp. 39–50. [Google Scholar]
- 3.Vaughn BV, D’Cruz OF. Cardinal manifestations of sleep disorders. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4. Philadelphia: Elsevier Saunders; 2005. pp. 594–601. [Google Scholar]
- 4.Breslau N, Roth T, Rosenthal L, Andreski MA. Daytime sleepiness: an epidemiological study of young adults. Am J Public Health. 1997;87:1649–1653. doi: 10.2105/ajph.87.10.1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carskadon MA, Dement WC. Sleep studies on a 90-minute day. Electroencephalogr Clin Neurophysiol. 1975;39:145–155. doi: 10.1016/0013-4694(75)90004-8. [DOI] [PubMed] [Google Scholar]
- 6.Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: A new approach. Psychophysiology. 1973;10:431–436. doi: 10.1111/j.1469-8986.1973.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 7.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 8.Libbus K, Baker JL, Osgood JM, Phillips TC, Valentine DM. Persistent fatigue in well women. Women health. 1995;23:57–72. doi: 10.1300/J013v23n01_04. [DOI] [PubMed] [Google Scholar]
- 9.Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37:147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- 10.Affleck G, Tennen H, Urrows S, et al. Fibromyalgia and women’s pursuit of personal goals: a daily process analysis. Health Psychol. 1998;17:40–47. doi: 10.1037//0278-6133.17.1.40. [DOI] [PubMed] [Google Scholar]
- 11.Le Bon O, Fischler B, Hoffmann F, et al. How significant are primary sleep disorders and sleepiness in the chronic fatigue syndrome? Sleep Res Online. 2000;3:43–48. [PubMed] [Google Scholar]
- 12.Monk TH. A visual analogue scale technique to measure global vigor and affect. Psychiatry Res. 1989;27:89–99. doi: 10.1016/0165-1781(89)90013-9. [DOI] [PubMed] [Google Scholar]
- 13.Lichstein KL, Means MK, Noe SL, Aguillard RN. Fatigue and sleep disorders. Behav Res Ther. 1997;35:733–740. doi: 10.1016/s0005-7967(97)00029-6. [DOI] [PubMed] [Google Scholar]
- 14.Theorell-Haglow J, Lindberg E, Janson C. What are the important risk factors for daytime sleepiness and fatigue in women? Sleep. 2006;29:751–757. doi: 10.1093/sleep/29.6.751. [DOI] [PubMed] [Google Scholar]
- 15.Lee KA, Zaffke ME. Longitudinal changes in fatigue and energy during pregnancy and the postpartum period. J Obstet Gynecol Neonatal Nurs. 1999;28:183–191. doi: 10.1111/j.1552-6909.1999.tb01983.x. [DOI] [PubMed] [Google Scholar]
- 16.Wolfson AR, Lee KA. Pregnancy and the postpartum period. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4. Philadelphia: Elsevier Saunders; 2005. pp. 1278–1286. [Google Scholar]
- 17.Troy NW. Is the significance of postpartum fatigue being overlooked in the lives of women? Am J Matern Child Nurs. 2003;28:252–257. doi: 10.1097/00005721-200307000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Gay CL, Lee KA, Lee S. Sleep patterns and fatigue in new mothers and fathers. Biol Res Nurs. 2004;5:311–318. doi: 10.1177/1099800403262142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Troy NW. A comparison of fatigue and energy levels at 6 weeks and 14 to 19 months postpartum. Clin Nurs Res. 1999;8:135–152. doi: 10.1177/10547739922158205. [DOI] [PubMed] [Google Scholar]
- 20.Ross LE, Murray BJ, Steiner M. Sleep and perinatal mood disorders: a critical review. J Psychiatry Neurosci. 2005;30:247–256. [PMC free article] [PubMed] [Google Scholar]
- 21.Dennis CL, Ross L. Relationships among infant sleep patterns, maternal fatigue and development of depressive symptomology. Birth. 2005;32:187–193.23. doi: 10.1111/j.0730-7659.2005.00368.x. [DOI] [PubMed] [Google Scholar]
- 22.Atkinson LS, Baxley EG. Postpartum fatigue. Am Fam Physician. 1994;50:113–118. [PubMed] [Google Scholar]
- 23.Benbadis SR. Questionnaires and Rating Scales. In: Kushida CA, editor. Sleep Deprivation: Clinical Issues, Pharmacology, and Sleep Loss Effects. New York: Marcel Dekker; 2005. pp. 1–9. [Google Scholar]
- 24.Partinen M, Hublin C. Epidemiology of sleep disorders. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4. Philadelphia: Elsevier Saunders; 2005. pp. 626–646. [Google Scholar]
- 25.Bailes S, Liberman W, Baltzan M, Amsel R, Schondorf R, Fichten CS. Brief and distinct empirical sleepiness and fatigue scales. J Psychosom Res. 2006;60:605–613. doi: 10.1016/j.jpsychores.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Pigeon WR, Sateia MJ, Ferguson RJ. Distinguishing between excessive daytime sleepiness and fatigue toward improved detection and treatment. J Psychosom Res. 2003;54:61–69. doi: 10.1016/s0022-3999(02)00542-1. [DOI] [PubMed] [Google Scholar]
- 27.Montgomery-Downs HE, Insana SI, Clegg-Kraynok M, Mancini LM. Normative Longitudinal Maternal Sleep: First Four Postpartum Months. Am J Obstet Gynecol. 2010 doi: 10.1016/j.ajog.2010.06.057. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radloff LA. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 29.Barrett LF, Barrett DJ. An introduction to computerized experience sampling in psychology. Soc Sci Comput Rev. 2001;19:175–185. [Google Scholar]
- 30.Dinges DF, Powell JW. Micorcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput. 1985;17:652–655. [Google Scholar]
- 31.Thorne DR, Johnson DE, Redmond DP, Sing HC, Belenky G. The Walter Reed palm- held psychomotor vigilance test. Behav Res Methods. 2005;37:111–118. doi: 10.3758/bf03206404. [DOI] [PubMed] [Google Scholar]
- 32.Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci. 2008;1129:305–322. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- 33.Radcliff R. Methods for dealing with reaction time outliers. Psychol Bull. 1993;114:510–532. doi: 10.1037/0033-2909.114.3.510. [DOI] [PubMed] [Google Scholar]
- 34.McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States (POMS) San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 35.McNair DM, Heuchert JWP, Shilony E. Profile of Mood States Bibliography 1964–2002. North Tonawanda, NY: Multi-Helath Systems Inc; 2003. [Google Scholar]
- 36.Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Med Rev. 2002;6:113–124. doi: 10.1053/smrv.2001.0182. [DOI] [PubMed] [Google Scholar]
- 37.Acebo C, LeBourgeois MK. Actigraphy. Respir Care Clin N Am. 2006;12:23–30. doi: 10.1016/j.rcc.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 38.Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. PARE. 2005;10:1–9. [Google Scholar]
- 39.Nyenhuis DL, Yamamoto C, Luchetta T, Terrien A, Parmentier A. Adult and geriatric normative data and validation of the Profile of Moods States. J Clin Psychol. 1999;55:79–86. doi: 10.1002/(sici)1097-4679(199901)55:1<79::aid-jclp8>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 40.Frey DJ, Badia P, Wright KP. Inter- and intra-individual variability in performance near the cirdadian nadir during sleep deprivation. J Sleep Res. 2004;13:305–315. doi: 10.1111/j.1365-2869.2004.00429.x. [DOI] [PubMed] [Google Scholar]
- 41.Van Dongen HPA, Baynard M, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: Evidence of Trait-Like differential vulnerability. Sleep. 2004;27:423–433. [PubMed] [Google Scholar]
- 42.McClelland LE, Pilcher JJ. Assessing subjective sleepiness during a night of sleep deprivation: examining the internal state and behavioral dimensions of sleepiness. Behav Med. 2007;33:17–26. doi: 10.3200/BMED.33.1.17-28. [DOI] [PubMed] [Google Scholar]
- 43.MacLean AW, Fekken GC, Saskin P, Knowles JB. Psychometric evaluation of the Stanford Sleepiness Scale. J Sleep Res. 1992;1:35–39. doi: 10.1111/j.1365-2869.1992.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 44.Shapiro C. Chronic fatigue—chronically confusing but growing information. J Psychosom Res. 2004;56:153–155. doi: 10.1016/S0022-3999(04)00002-9. [DOI] [PubMed] [Google Scholar]