Abstract
Bracing is a critical component of the current standard of treatment for clubfoot. Adherence to the bracing protocol is the main factor for the long-term success of the treatment The purpose of this paper is to provide a review of clubfoot braces, best practices in brace design and recommendations for bracing in order to improve adherence with the bracing phase of the clubfoot treatment. There are a number of designs and offerings of braces available in various regions of the world. Although many new brace designs are being proposed and developed, evidence in the literature regarding biomechanical effects, clinical outcomes, functionality and patient adherence is limited. The current research that is available regarding brace design focuses on increasing patient comfort and satisfaction to improve adherence. Although the currently available braces are widely distributed in developed countries, access is limited to many parts of the world. When considering the future of the clubfoot treatment and prevention of relapses, since 80% of the cases are in developing countries with limited resources, brace cost and availability needs to be assessed.
INTRODUCTION
Congenital talipes equinovarus, or clubfoot, is a common deformity where the affected foot is turned inward. It occurs in every 1.2 in 1000 live births and is the most common musculoskeletal congenital birth defect.3,20 Males are more commonly affected than females and up to 50% of cases are bilateral.23,24 The etiology of congenital clubfoot is largely idiopathic;10,17,23,24,26,31 however, it can be associated with other conditions such as spina bifida, arthrogryposis or other syndromes in approximately 20% of the cases.3
Over the past few decades, there has been extensive research regarding the appropriate treatment for clubfoot. Historically, surgical correction, specifically an extensive postero-medial soft tissue release, was the mainstay treatment option. This intervention, however, has been shown to result in severe scarring, joint stiffness, muscle weakness, gait disturbances and relapses. Additionally, complications including wound infections, skin necrosis and neurovascular injuries have been reported. Furthermore, the deformity can be over- or under-corrected and the talus may be flattened or even result in necrosis.2,8,9,15,16,20,23,27,29
Given the potential devastating complications and discouraging long-term results, treatment preferences have since changed to primarily a non-operative approach through the Ponseti method. The method has become the standard of care and completely eliminates the need for extensive operative correction in over 98% of patients if applied correctly.20 The treatment involves manipulation, a series of castings, percutaneous Achilles tenotomy and foot bracing. With correct application of the procedure and appropriate patient adherence, complete correction can be achieved in as little as 16 days with an accelerated casting protocol.21,22,25 Most importantly, long-term follow-ups have shown high patient satisfaction and functional outcomes.7,18,19,26
While the casting phase of the treatment is relatively short and has the most visible effect on the correction of the deformity, the bracing phase that last for 4-5 years is actually essential for the success of the method. Bracing must be done every night, is mainly the responsibility of the parents, and is done with limited clinical supervision. Importantly, adherence to the bracing protocol is critical for the long-term success of the treatment as demonstrated by the high relapse rate in non-adherent parents (10 times greater). Adherence to bracing is a better predictor for relapse than severity of the deformity at birth, which is not a reliable indicator of the odds of relapse.1,11,12,13,22 Because of the critical importance of bracing in the success of the Ponseti method, we will describe an overview of past and current clubfoot braces with specific information on the key points about design and wearing protocols. We believe a historical perspective combined with a scan of the current state of practice can be utilized to guide future directions of research, education and practice.
HISTORICAL PERSPECTIVES ON BRACING
The 1895 publication by Walsham and Hughes on the deformities of the foot provides an early account of bracing for the prevention of clubfoot relapse.30 In this book, the authors divide bracing into two categories, (1) instruments for use during the night, and (2) instruments for use during the day. They further breakdown the daytime bracing options into three subsets, including (a) instruments for holding the foot in a restored position, (b) those that, in addition to (a), are designed to overcome the tendency for the whole limb to roll inwards, and (c) those that have the purpose of further improving a partially corrected clubfoot.
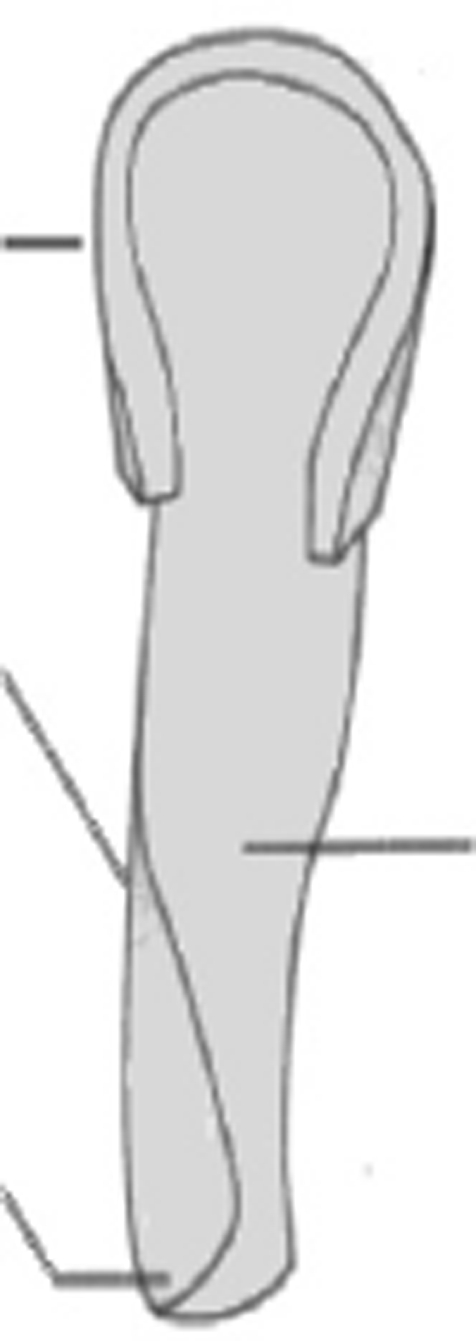
Figure 1 is an example of a category (1) brace for use at night. This brace was intended for the recently corrected clubfoot. The authors state a tendency for the weight of bedclothes to press back the foot to a deformed position.30 The brace consists of a calf-piece for the back and outer side of the calf, and a foot-piece, bent at right angles and turned up on the inner side to prevent the foot from rolling inwards. An oval hole is placed opposite the internal malleolus to prevent pressure at this spot. This splint was softly padded and covered with leather, the foot being held in place with bandage.
Figure 1.
Tin rectangular varus night-shoe.30
Figure 2 shows examples of category (2), subset (a) as described by the authors for holding the foot in a restored position. The authors suggest using such an apparatus only after varus has been completely overcome and dorsiflexion of 30 degrees is achieved.30
Figure 2.
Boot with inside leg-iron and varus T-strap (left) and boot with inside and outside leg-irons and varus T-strap (right).30
Figure 3 shows examples of category (2), subset (b) as described by the authors for not only the maintenance of corrected clubfoot, but to also control inversion of the limb. The authors state that after clubfoot correction, children beginning to walk still have their toes pointing inwards. They suggest that this may be due to the laxity of the ligaments of the knee joint, allowing the tibia to roll inwards on the femur, or, more often, from the whole lower limb rolling in at the hip joint due to a “faulty direction of the neck of the femur.”30
Figure 3.
From left to right: Walking apparatus with outer iron carried to pelvic girdle with T-strap on outer side; Mathieu's apparatus for producing eversion of the limb; Meusel's apparatus for correcting the inversion of the foot and leg after clubfoot correction.30
Also included in this category is Sayre's appliance for correcting inversion of bilateral clubfoot, shown in Figure 4. This is the only brace depicted in this nineteenth century book that resembles the standard-of-care bracing used today.
Figure 4.
Sayre's appliance for correcting inversion in bilateral clubfoot30
Figure 5 shows examples of category (2), subset (c) as described by the authors for having the purpose of further improving a partially corrected clubfoot. They further divide these braces into two categories, (i) those that retain the foot in a corrected position and for further correcting the equinus (plantarflexion); and (ii) those for continuing the eversion as well as dorsiflexion of the foot. They are shown in Figure 5 together, due to their similarity. Note that each employs a strategy (belt, spring, cable, etc.) for holding the foot in dorsiflexion, while some include additional leg irons for achieving eversion.30
Figure 5.
From left to right: Beely*s boot for further correcting equinus; Steel spring for overcoming equinus; Sayre's boot for correcting equinus and varus by rubber cords; Stillman's boot for correcting the tendency for the foot to roll inwards.
The braces most commonly used today employ a connecting bar and are often referred to as a ‘Denis Browne Bar’ or ‘Denis Browne Splint’ regardless of manufacturer or setup specifications. These braces are likely an evolution and adaptation of that described by Denis Browne in his 1934 publication, ‘Talipes Equino-Varus.’4 Here Browne states that maintaining the clubfoot correction “can be obtained by connecting the feet horizontally at the desired angles to the Sagittal plane.” He describes, “the desired angles,” to be external rotations of 20-degrees for unaffected feet and up to 90-degrees for club-feet. His original brace included an L-shaped bracket to hold the foot, “bending up one side to clear the external malleolus and bear against the outer side of the leg.” The foot is also described by Browne to be held in significant dorsiflexion, connected to the bar via “sticking-plaster” for babies, and open-toe straight last boots for walking children.
In 1952, in The British Encyclopaedia of Medical Practice, Browne describes a “night-splint” or “calcaneus splint” in greater detail.5 The splint, he states, “consists of a central grip around the ankle, from which there runs forward an open-ended shoe to hold the foot, and upwards 2 struts to hold a band below the knee.” The front part of the shoe can be pulled upwards by a strap to the upper band, bringing the foot into calcaneus. Varus or valgus was adjusted by rotation of a lever through which a strap passed. Browne believed that equinus was the most common factor in all foot deformities, and that, “there is at present no other splint that will counter it.” He concludes, stating that, “If necessary, the feet can be turned outwards as well as held in calcaneo-valgus position by connecting the feet together with a jointed bar of metal.”5
In a correspondence written in the British Medical Journal in 1956, Browne claimed difficulty in getting his work on the splint published due the opposition of orthopaedic surgeons.6 He states in this correspondence that, ‘The splint was first described in the U.S.A. with the lateral lever cut down to useless proportions, and from thence copied into various English textbooks.” Browne was clearly upset by the modifications; stating that, “Before improving a technique, first find out what it actually is and how it developed.” He also states, “If the originator is still available, get his opinion on the modifications before publishing it.”
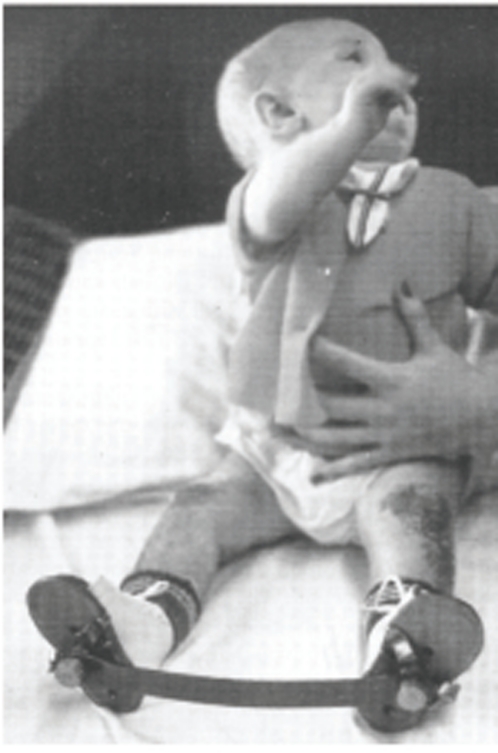
In the 1997 book, Atlas of Orthoses and Assistive Devices, a figure is shown under a section on clubfoot correction with the following caption, “Eleven-month-old child in reverse last shoes and Denis-Browne bar after bilateral clubfoot repair. The combination (of shoes and bar) helps maintain external rotation, the corrected abducted position, and prevents turning in of the feet.” (Figure 6).
Figure 6.
Child in a FAB.14
The brace from Figure 6 shown above is similar to that of the current standard-of-care brace. The standard of care brace and additional modern day clubfoot bracing are discussed in detail in the next section.
CURRENT BRACING DESIGNS
Presently, there are three major categories of brace designs: Ankle Foot Orthosis (AFO), Wheaton Brace or similar braces, and Foot Abduction Brace (FAB). The AFO design follows a similar concept to braces described in the historical review, such as the tin rectangular varus night shoe. It fully covers both the foot and ankle, thus providing only the dorsiflexion built into the brace, which is usually set at neutral. Importantly, it does not provide abduction, which is important for the stretching of the medial structures. In addition, because of the lack of motion at the ankle, it contributes to calf muscle atrophy which is already abnormal in clubfoot. In specific circumstances, an AFO can be useful in combination with an abduction brace, i.e., when the child's foot has relatively limited dorsiflexion (i.e., spina bifida, arthro-gryposis, neurologic dysfunction of the peroneal nerve, etc.). There is little muscular support in these conditions, so the brace provides the necessary structural support to the child's foot.
The Wheaton Brace (Figure 7), and other similar devices based on the same construct, can provide some abduction of the foot. A Velcro strap is tightened against the apex of the deformity. The brace comes in two types, with the ankle at 15 degrees plantar flexion and with the angle at 90 degrees dorsiflexion. Because the brace is worn up to the thigh, it contributes not only to some calf muscle atrophy but also to thigh muscle atrophy.
Figure 7.
32
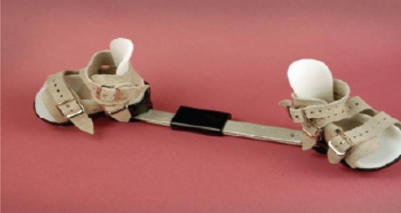
Under the Ponseti method recommendations, the corrected foot should be held in an abducted and dor-siflexed position to prevent relapses. This is the most important criteria to ensure that there is maintenance of the clubfoot correction and is best achieved by using a well-designed Foot Abduction Brace (FAB). A FAB consists of two shoes connected by a bar. If the deformity is unilateral, the external rotation on the affected foot should be set to 60/70° and on the unaffected foot to 30/40°. The bar should be of the length between the child's shoulders and should be bent to allow for 10-15° of dorsiflexion. Ideally, the bar can be lengthened over time as the child grows. The shoes should be comfortable and straight laced (no curves and can fit both feet). To increase the ease and adherence of use, a brace with shoes that can clip into and out of the bar seems to be preferred by the parents.
Traditionally these bars have been known as the “Denis Browne Split.” The Denis Browne Split utilizes an L-shaped bracket to hold the foot in significant dorsiflexion and is connected to open-toe boots. There is some concern when the child's feet are still small that it may be difficult to prevent movement in the shoe. The Denis Browne Split is available in many countries and it paved the way for the new style of braces seen today.
Although many modern clubfoot braces are available in the market, their use across the world is uneven given that the cost may be prohibitive for many patients, especially in developing countries. The Steenbeek brace (Figure 8), developed in Uganda by Michiel Steenbeek and David Okello, is made with local tools (leather sewing machine, metal-working equipment, welding tools) and materials (leather, lining, plywood, mild steel rod stock). The cost is under 10 US dollars and matches the recommendations provided by Dr. Ponseti.33
Figure 8.
34
Other locally produced FABs are available, such as in Sweden, Vietnam and Armenia. In Sweden, the brace developed by Dr. Romanus in Gothenburg, uses malleable plastic to mold the shoes that shape to the child's foot. The shoes are fixed to the bar with screws. In Vietnam, the Prosthetics Outreach Foundation works with Ha Troy OTRC workshop to produce a brace in line with Ponseti recommendations. It must be mentioned that some parents have produced their own home made braces that consist in most cases of a wood or metal bar with shoes attached at the recommended angles. Interestingly, in the patients that these devices have been used there has been a good control of relapses.
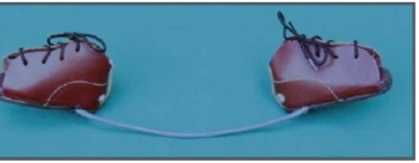
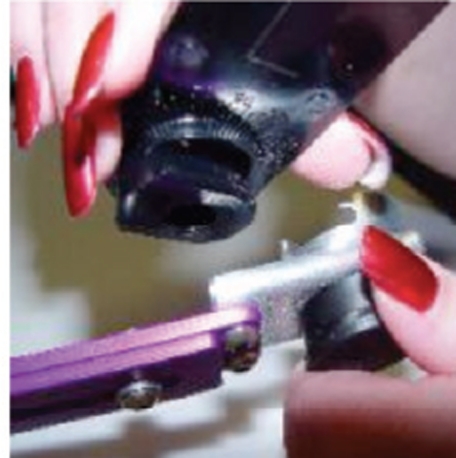
FABs are constantly being redesigned to improve comfort and to increase adherence to therapeutic recommendations. Although the functional aspects of most FABs are aligned with the Ponseti method recommendations, different materials are used to attempt an increase in patient utilization and satisfaction. For example, the Kessler Brace (Figure 9) closely follows the angles recommended by the Ponseti method, but the bar has some flexibility to allow the child some ability for plantar flexion during kicking. The bar returns to the original dorsiflexed position once the child stops kicking.18 The Horton Click brace utilizes a shoe that can be easily “clicked” onto the bar. However, this design allows both internal and external rotation of the foot (Figure 10). The Dobb's Dynamic Clubfoot Brace utilizes a bar that allows the child to move both legs independently and shoes that reduce heel friction, however due to the articulation design, dorsiflexion may be difficult to achieve (Figure 11). The bar component can also be attached to Markell, Mitchell or custom made shoes. The ALFA-Flex shoe is an FAB produced in Europe that has a large focus on the comfort and fit of the shoe. It uses non-toxic and biocompatible materials (Figure 12). An “intelligent” foam mould for the shoe allows a close, firm fit for the child's foot and provides proper distribution of pressure in the brace. The foam material has both viscous and elastic components. The shoes are easy to put on due to step-in straps.37
Figure 9.
Figure 10.
35
Figure 11.
36
Figure 12.
38
The Mitchell Brace is widely distributed in developed countries; however it is also quite expensive. The brace was designed under the direction of Dr. Ponseti for the treatment of Complex Clubfeet given the difficulty maintaining a good correction with the Markell shoes (Figure 13). Given that the shoes are very comfortable for the child, this brace is in use now for any clubfeet.
Figure 13.
Open-toed shoes with straps last approximately 4-6 months. The bar is adjustable and comes in two sizes (range: 19.5-37.0cm).39
To note, although many current braces have been described, there is a lack of evidence in the literature regarding biomechanical effects on soft-tissues, functionality, patient adherence, and outcomes (Table 1).
TABLE 1.
Literature Review of Currently Available Clubfoot Braces
| Brace | Studies |
|---|---|
| Wheaton Brace | None |
| Steenbeek Brace | J Pediatr Orthop B. 2008 May;17(3):134-8. Int Orthop. 2008 Feb;32(l):75-9. Epub 2006 Nov 18. |
| Romanus Brace | None |
| Locally Produced - Vietnam | None |
| Locally Produced - Armenia | Garen Koloyan, MD, Vahe Yavryan, MD, Ara Tekgezian, CPO: “Club Foot Brace”. 4th International Clubfoot Congress. International Federation of Pediatric Orthopaedic Societies. Istanbul Convention and Exhibition Centre, Tokpaki A. Istanbul, Turkey, September 5-6, 2005; Paper No. 24. Garen Koloyan, MD; Vahe Yavrian, MD; Ara Tekgezian, CPO. : “A Unique Design for a Clubfoot Brace”. ACPOC, Association of Children's Prosthetic-Orthotic Clinics, 2004 Annual Meeting, March 24-27, Banff, Alberta, Canada; p.38. |
| Kessler Brace | Kessler JI. A new flexible brace used in the Ponseti treatment of talipes equinovarus. |
| Horton Click | None |
| Dobb's Dynamic Clubfoot Bar | J Child Orthop. 2009 Aug;3(4):271-6. J Pediatr Orthop. 2007 Jul-Aug;27(5):522-8. |
| ALFA -Flex Brace | None |
| Markell Brace | J Pediatr Orthop. 2005 Mar-Apr;25(2):225-8. |
| Mitchell Brace | None |
BRACE WEARING SCHEDULE
The FAB is used only after the clubfoot has been completely corrected by manipulation, serial casting, and possibly the heel cord tenotomy. All current braces described will provide appropriate maintenance of the clubfoot correction as long as the feet are held in the suggested abducted and dorsiflexed positions and the appropriate bracing schedule is followed. Bracing protocol needs to be tailored to the individual patient based on age, relapse rate associated with that age, and when the correction was finished. For example, bracing hours will be longer for a newborn that was corrected in three weeks as opposed to an older child that is already walking when correction is achieved. Importantly, since the underlying cause of clubfoot results clinically in a muscle growth and development problem, it is very important that children using a brace maintain a degree of mobility during the day (Table 2).
TABLE 2.
Recommendations for Clubfoot Bracing Schedules (based on current knowledge)
| a. Final correction in the first few months of life |
| i. Wear brace 23 hours/day for first three months |
| ii. Follow a gradual weaning schedule*: one month 20-22 hours/day, one month 18-20 hours/day, one month 16-18 hours/day, |
| and one month 14-16 hours/day |
| iii. Maintain night-time wearing of the brace (12-14 hours/day) as the child grows and is walking full time for up to age 4-5 years |
| b. Final correction achieved after 8-9 months of age and child is ready for crawling or walking |
| i. Allow some mobility to help in the development of the weak muscles. |
| ii. Begin initial bracing with 18-20 hours/day for 2 months and then 16 hours a day for 3-4 months |
| iii. Follow standard maintenance protocol (a. iii.) |
| c. Final correction at age 2 to 4 years of age |
| i. Use the brace at night as per standard protocol (a.iii) |
| d. Final Correction after 4 years of age |
| i. Some patients may still tolerate the brace at night for 1-2 years. |
| ii. In some patients, the use of an AFO will be more acceptable. |
| e. Children with loose joints (approximately 2-3% of cases) |
| i. Set the shoe to 30-40% abduction (abduction of 60 to 70 degrees may lead to flat foot, usually presenting when the patient |
| starts walking at 10-16 months of age and after) |
| ii. Do not stop using the brace as there is a risk of relapse. |
| f.Children with has atypical/complex clubfoot |
| i. Set the shoe for the affected foot at 20-30 degrees. |
| ii. Do not bend the bar unless there is 10-15 degrees of dorsiflexion with the last cast. |
| iii. Change the angle of the shoe to 40-50 degrees as the foot becomes more normal looking and add the bend in the far to |
| allow 10-15 degrees of dorsiflexion. |
The time in the brace does not need to be consecutive, but it is important for the child to wear the brace while sleeping (e.g., at night, during naps) to encourage mobility during waking hours. If the child attends daycare, consider leaving the brace on in the morning and instructing the daycare as to what time each day that the brace should be removed. If possible, instruct them how to remove and reapply the brace for nap times.
A brace should be measured and order for the child before the last cast is removed due to the high chance of regression leading to discomfort and non-adherence with the brace if the brace is not placed immediately after the cast is removed. If the brace is not ready, a holding cast should be applied to maintain final correction. It is also important not to end treatment early. Based on current information, there is a tendency for relapses up to the age of 4-5 years. Unfortunately, it is not possible using current clinical evaluation to know which patients would have a relapse during this time if the brace is stopped, so it is recommended for the brace to be used for all this period.
IMPROVING BRACING ADHERENCE
Since adherence to brace wearing protocols is essential for preventing relapses, it is important for health care providers to communicate with patients regarding brace wearing to set proper expectations and ensure accurate use. Table 3 describes current recommendations that can be presented to parents by physicians, nurses, counselors or other health professionals in order to improve adherence with brace wear.
TABLE 3.
Recommendations for Parents (based on current knowledge)
| a. Expect your child to fuss in the brace for the first 2-3 days. |
| i. This is not because the brace is painful, but because it is something new and different. |
| ii. The child may have skin sensitivity as a result of the casting |
| ii. If your child is completely inconsolable and you believe that they are in pain, contact your physician immediately. |
| b.Play with your child in the brace. This is a key to getting quickly over the child's irritability. |
| i. Since the child is unable to move his/her legs independent of each other in the brace, you must teach your child that he/she can |
| kick and swing the legs simultaneously. |
| ii. Gently flex and extend the knees by pushing and pulling on the bar of the brace. |
| iii. Try making a game of the motions by singing and/or talking to your child in an encouraging manner. |
| c. Make the treatment a routine. |
| i. Your child is less likely to fuss if you make the use of this brace as a routine, non-negotiable part of their daily activities, just like |
| putting on their pajamas, brushing their teeth, and reading books at night. |
| ii. When the child is only wearing the brace while sleeping, put the brace on any time your child goes to the “sleeping spot.” |
| iii. Some parents have made a brace for the child's favorite stuffed animal or doll. |
| iv. Some parents call the brace “Nite-Nite shoes” or “Magic Shoes” |
| d. Show your child pictures of other children with clubfoot wearing their brace. |
| e. Use rewards and incentives to help your child understand the importance of the brace. |
| f. For older children, ask your physician to talk to the child at follow up appointments about their brace and how it helps them maintain |
| the correction. |
| g. Pad the bar. This will protect your child, yourself, and your furniture from being hit by the bar when the child is wearing the brace. |
| i. A bicycle handle bar pad or foam pipe insulation covered with fabric or tape works well. |
| ii. Placing a sleep sack on the child at night will also help with padding and keep the baby from pulling at the straps and laces |
| with their hands. |
| h. If you notice any bright red spots or blistering contact your health care provider. |
| i. Some mild redness is normal with use. |
| ii. Bright red spots or blisters, especially on the back of the heel, usually indicate that the shoe was not worn tightly enough. |
| Make sure that the heel stays down in the shoe. |
| iii. Tighten the strap by one more hole or tighten the laces |
| iv. Remove the tongue of the shoe. Use of the brace without the tongue will not harm your child. |
| v. If the brace shoe has laces, lace the shoes from top to bottom, so the bow is by the toes. |
| vi. Check the width of the brace and widen if necessary. |
| vii. Never use lotion on any red spots on the skin. Lotion will make the problem worse. |
| viii. If persistent and the foot comes out of the shoe, it may be a sign of early relapse. |
CONCLUSIONS
Although many new brace designs are being proposed and developed, evidence in the literature regarding bio-mechanical effects, clinical outcomes, functionality and patient adherence is limited. Most braces follow most of the aspects of the Ponseti method recommendations; however, any deviations form this clinical practice and experience should be studied to determine if success rates are similar or improved.
The current research that is available regarding brace design focuses on increasing patient comfort and satisfaction to improve adherence. However, when looking to the future of the Ponseti method and prevention of relapse, brace cost also needs to be assessed. Although the currently available braces are widely distributed in developed countries, access is limited to many parts of the world. This is mostly due to the prohibitive cost of most bracing options (>$300 US dollars). Locally produced orthotics with low cost materials, such as the Steenbeek brace, can provide an option to patients in underprivileged areas and increase adherence and success rate of the treatment.
IMAGES
Wheaton Brace: http://www.wheatonbrace.com/products/wbrace.html
Steenbeck Brace: http://www.global-help.org/publications/books/help_cfponseti.pdf
Steenbeck Brace (image): http://www.global-help.org/publications/books/help_steenbeekbrace.pdf
Horton Click Brace: http://www.hortontechnology.com/index.html
Dobb's Brace: http://www.dobbsbrace.com/
ALFA-Flex Brace: http://www.semeda.de/25-1-alfa-flex.html
ALFA-Flex Brace (image): http://institutsantjoan.com/pie-zambo/
REFERENCES
- 1.Abdelgawad AA, et al. Treatment of idiopathic clubfoot using the Ponseti method: minimum 2-year follow-up. Journal of Pediatric Orthopaedics B. 2007;16(2):98–105. doi: 10.1097/BPB.0b013e32801048bb. [DOI] [PubMed] [Google Scholar]
- 2.Atar D, Lehman WB, Grant AD. Complications in clubfoot surgery. Orthop Rev. 1991;20:233–239. [PubMed] [Google Scholar]
- 3.Bridgens J, Kiely N. Current management of clubfoot (congenital talipes equinovarus) BMJ. 2010;340:c355. doi: 10.1136/bmj.c355. [DOI] [PubMed] [Google Scholar]
- 4.Browne D. Talipes Equino-Varus. Lancet. 1934;2:969–974. [Google Scholar]
- 5.Browne D. The British Encyclopaedia of Medical Practice. Vol. 12. London: Butterworth; 1952. Talipes; pp. 1–9. [Google Scholar]
- 6.Browne D. Splint for Talipes Equinovarus. British Medical Journal. 1956;1(4965):516. doi: 10.1136/bmj.1.4959.168-b. [DOI] [PubMed] [Google Scholar]
- 7.Cooper DM, Dietz FR. Treatment of Idiopathic Clubfoot. A thirty-year follow- up. J Bone Joint Surg Am. 1995;77:1477–1489. doi: 10.2106/00004623-199510000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Crawford AH, Gupta AK. Clubfoot controversies: complications and causes for failure. Instr Course Lect. 1991;45:339–346. [PubMed] [Google Scholar]
- 9.Dewaele J, Zachee B, De Vleeschauwer P, Fabry G. Treatment of idiopathic clubfoot: critical evaluation of different types of treatment programs. J Pediatr Ortho. 1994;3:89–95. [Google Scholar]
- 10.Dietz FR. The genetics of idiopathic clubfoot. Clin Orthop Rel Res. 2002;401:39–48. doi: 10.1097/00003086-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Dobbs MB, et al. Factors Predictive of Outcome After Use of the Ponseti Method for the Treatment of Idiopathic Clubfeet. The Journal of Bone & Joint Surgery. 2004;86-A(1):22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Dobbs MB, Corley CL, Morcuende JA, Ponseti IV. Late Recurrence of Clubfoot Deformity: A 45-Year Followup. Clinical Orthopaedics and Related Research. 2003;411:188–192. doi: 10.1097/01.blo.0000065837.77325.19. [DOI] [PubMed] [Google Scholar]
- 13.Goksan SB, et al. Ponseti technique for the correction of idiopathic clubfeet presenting up to 1 year of age. A preliminary study in children with untreated or complex deformities. Archives of Orthopaedic and Trauma Surgery. 2006;126:15–21. doi: 10.1007/s00402-005-0070-9. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg B, Hsu JD. Atlas of Orthoses and Assistive Devices. Mosby-Year Book, Inc.; 1997. [Google Scholar]
- 15.Grayev AM, Boal DK, Wallach DM, Segal LS. Metaphyseal fractures mimicking abuse during treatment for clubfoot. Pediatr Radiol. 2001;31:559–563. doi: 10.1007/s002470100497. [DOI] [PubMed] [Google Scholar]
- 16.Huber H, Galanty R, Dutoit M. Avascular necrosis after osteotomy of the talar neck to correct residual club-foot deformity in children. A long-term review. J Bone Joint Surg [B] 2002;84:426–430. doi: 10.1302/0301-620x.84b3.12206. [DOI] [PubMed] [Google Scholar]
- 17.Hutchins PM, Foster BK, Paterson DC, Cole EA. Long-term results of early surgical release in clubfeet. J Bone Joint Surg [Br]. 1985;67:791–799. doi: 10.1302/0301-620X.67B5.4055883. [DOI] [PubMed] [Google Scholar]
- 18.Kessler JI. A new flexible brace used in the Ponseti treatment of talipes equinovarus. J Pediatr Orthop B. 2008;17(5):247–50. doi: 10.1097/BPB.0b013e32830cc3e5. [DOI] [PubMed] [Google Scholar]
- 19.Laaveg SJ, Ponseti IV. Lon-term results of treatment of congenital clubfoot. J Bone Joint Surg [Am]. 1980;62:23–31. [PubMed] [Google Scholar]
- 20.Morcuende JA. Congenital idiopathic clubfoot: prevention of late deformity and disability by conservative treatment with the Ponseti technique. Pediatr Ann. 2006;35(2):128–30. 132–6. doi: 10.3928/0090-4481-20060201-13. [DOI] [PubMed] [Google Scholar]
- 21.Morcuende JA, Abbasi D, Dolan L, Ponseti IV. Results of an accelerated Ponseti protocol for clubfoot. J Pediatr Orthop. 2005;25:623–626. doi: 10.1097/01.bpo.0000162015.44865.5e. [DOI] [PubMed] [Google Scholar]
- 22.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113:376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 23.Mosca V. The foot. In: Morrissy RT, Weinstein SL, editors. Lovell and Winter's Pediatric Orthopaedics. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 1151–1161. [Google Scholar]
- 24.Ponseti IV. Congenital Clubfoot: Fundamentals of Treatment. Oxford, England: Oxford University Press; 1996. [Google Scholar]
- 25.Ponseti IV, Smoley EN. Congenital Clubfoot: the results of treatment. J Bone Joint Surg [Am]. 1963;45:261–275. [Google Scholar]
- 26.Ponseti IV, Campos J. Observations on pathogenesis and treatment of congenital clubfoot. Clin Orthop Rel Res. 1972;84:50–60. doi: 10.1097/00003086-197205000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Tarraf YN, Carroll NC. Analysis of the components of residual deformity in clubfeet presenting for reoperation. J Pediatr Orthop. 1992;20:233–239. doi: 10.1097/01241398-199203000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Uglow MG, Clarke NM. Relapse in staged surgery for congenital talipes equinovarus. J Bone Joint Surg [Br] 2000;82:739–743. doi: 10.1302/0301-620x.82b5.9413. [DOI] [PubMed] [Google Scholar]
- 29.Vizkelety T, Szepesi K. Reoperation in treatment of clubfoot. J Pediatr Orthop. 1989;9:144–147. [PubMed] [Google Scholar]
- 30.Walsham WJ, Hughes WK. The Deformities of the Human Foot: With Their Treatment. New York: William Wood & Company; 1895. [Google Scholar]
- 31.Wynne-Davies R. Genetic and environmental factors in the etiology of Talipes Equinovarus. Clin Orthop Rel Res. 1972;84:9–13. doi: 10.1097/00003086-197205000-00003. [DOI] [PubMed] [Google Scholar]