Abstract
Introduction
We evaluated the local recurrence rate (LRR) of bone sarcoma along the core-needle biopsy (CNB) tract in patients who underwent limb Salvage Surgery (LSS) following a diagnostic CNB performed irrespective of the planned surgical incision site and for which surgery did not involve any biopsy tract removal.
Methods
A retrospective review of 10 pediatric patients diagnosed with bone sarcoma using a computed tomography-guided core-needle biopsy, with evaluation of medical records, pathological specimens and radiological films from the date of diagnosis until the most recent follow-up.
Results
None of the patients experienced local recurrence during their follow up, despite the lack of biopsy site resection. CT scans of the involved extremities were negative for any suspicious lesions in all patients up until the most recent follow-up.
Conclusions
Our study and review of the literature suggest that the incidence of tumor seeding the CNB tract in bone sarcoma patients is apparently low, and possibly negligible. CNB should be performed through the most direct approach to the tumor, and LSS can be performed safely through the standard approaches without excision of the biopsy tract.
INTRODUCTION
Bone sarcomas comprise around 1% of all malignancies diagnosed annually in the United States.1 The biopsy method of choice in these sarcomas remains controversial, since randomized controlled trials to compare core-needle biopsies (CNB) with the open biopsy procedure have not been conducted yet.2,3 However, in the era of minimally invasive intervention, several authors have advocated the use of CNB as an index diagnostic measure. This technique has provided accuracy rates ranging from 88% to 96% in bone sarcomas when adequate samples are obtained.3-6
The open biopsy technique has been associated with a significantly increased risk of tumor seeding along the biopsy tract when the scar is not removed en-bloc during surgical resection of the tumor.7 Similar experience with CNB remains limited. Nevertheless, it has been suggested that CNB must be performed along the standard surgical incision site and its tract should be excised during tumor resection. However, the majority of radiologists tend to choose the most optimal approach to the tumor, disregarding the standard incision site. This is to avoid multiple biopsy attempts and to attain the highest possible yield. Moreover, surgeons often cannot localize the needle site during definitive surgery which is usually scheduled following 12 weeks of neo-adjuvant chemotherapy.
We herein evaluate the local recurrence rate (LRR) of bone sarcoma along the CNB tract in patients who underwent Limb Salvage Surgery (LSS) following a diagnostic CNB performed irrespective of the planned surgical incision site and for which surgery did not involve any biopsy tract removal.
PATIENTS AND METHODS
This is a retrospective review of bone sarcoma cases in pediatric patients (≤ 21 years) diagnosed at the American University of Beirut Medical Center (AUBMC) between January 2001 and December 2005. After receiving approval for our study from the Institutional Review Board (IRB), we identified 22 patients, 10 of whom were diagnosed by CNB and underwent subsequent LSS for bone sarcoma of the extremities. These ten patients were included in this study. Medical records, pathological specimens and radiological films of these patients were reviewed from the date of diagnosis until the most recent follow-up.
The mean age of the patients at diagnosis was 12.5 years (range: 7 to 18 years) with a male to female ratio of 1:1 (see Table 1). All patients had stage IIB tumors at diagnosis.
TABLE 1.
Patients' characteristics
| Patient number | Age (yrs) | Gender | Follow-up (yrs) | Tumor site | CNB approach | Local recurrence | Distant relapse | Tumor necrosis |
|---|---|---|---|---|---|---|---|---|
| 1 | 12 | F | 6 | Tibia | Anteromedial | None | No | 91% |
| 2 | 11 | F | 6 | Tibia | 1. Anteromedial | |||
| 2. Anterolateral | None | No | 20% | |||||
| 3 | 12 | M | 5.5 | Femur | Anteromedial | None | Yes | 80% |
| 4 | 17 | M | 5 | Shoulder | Anterior | None | No | 100% |
| 5 | 14 | F | 3.5 | Tibia | Anteromedial | None | No | 100% |
| 6 | 18 | F | 3.5 | Femur | Lateral | None | No | 100% |
| 7 | 13 | M | 3.1 | Femur | Anteromedial | None | No | 100% |
| 8 | 11 | M | 3 | Femur | Anteromedial | None | Yes | 50% |
| 9 | 7 | F | 2 | Femur | 1. Anteromedial | |||
| 2. Lateral | None | No | 100% | |||||
| 10 | 8 | M | 6 | Femur | Lateral | None | No | 80% |
CNB = core-needle biopsy
Biopsy
All biopsies were performed under computed tomography (CT)-guidance using a 12-gauge coaxial cutting needle (Ackermann Bone Biopsy Needle Set, William Cook Europe). Biopsies were performed under local anesthesia by an experienced interventional radiologist without the presence of an orthopaedic surgeon. The most direct approach to the soft tissue mass was selected and used for CNB. The site of biopsy was recorded for each patient. After confirmation of the diagnosis, patients were started on neoadjuvant chemotherapy as per the St. Jude-Children's Research Hospital (Memphis, TN) protocols.
Surgery
Surgical resection was performed through a medial standard incision in nine patients with knee tumors and through an anterior approach in one patient with tumor of the humerus, without any attempt at excision of the CNB tract. The surgical margins in all patients were either normal or had no viable tumor.
Follow-up
Postoperatively, patients were followed-up clinically and radiographically every three months for two years and then every six months up until the most recent follow-up. The average time for follow-up was four years (range, two to six years). The involved extremity was examined by the surgeon looking for any suspicious nodule or mass. A CT scan of the involved extremity was also performed. CT images were evaluated for any suspicious lesions suggestive of local recurrence in the bone or surrounding soft tissue. Metastatic workup was completed by a technetium bone scan for local and distant metastases and a CT scan of the chest for distant metastases. All patients were compliant to follow-up schedules.
RESULTS
Of the 10 patients reviewed, none experienced local recurrence during their follow-up, despite the lack of biopsy site resection. CT scans of the involved extremities were negative for any suspicious lesions in all patients up until the most recent follow-up. Two patients experienced distant relapse seen on CT scans of the chest during follow-up, not associated with any evidence of local recurrence. One (patient #3) had a lesion in the left upper lobe and underwent radical resection of the lobe. The other (patient #8) also had a lesion in the left upper lobe. This patient also had a relapse of the tumor in his spine seen on bone scans. He died on treatment for his metastatic disease. No other patients showed evidence of local or distant metastasis on bone scan up until the most recent follow-up.
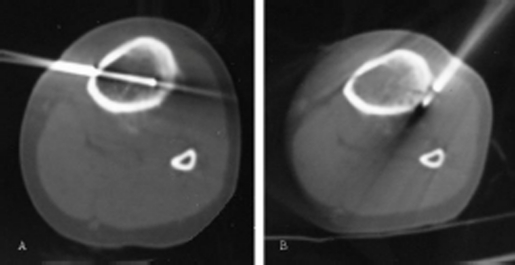
Of the 10 cases, final biopsies were performed from an anteromedial approach in five cases, one from an anterior approach, one from an anterolateral approach, and three from a lateral approach (see Table 1). In two of the patients, an initial attempt to perform the CNB from the anteromedial approach had resulted in an inconclusive sample, necessitating a second attempt from an anterolateral approach in one patient and a lateral approach in the other. In both cases a final diagnosis was made, one of Ewing's sarcoma and the other of osteosarcoma, from the second biopsy attempt. Figure 1 illustrates one of these cases in which (A) the first biopsy attempt was made from an anteromedial approach, while (B) the second was made from an anterolateral approach.
Figure 1.
Images from CT-guided biopsies of the left tibia taken from (A) an anteromedial approach, which was inconclusive, and (B) an anterolateral approach which retrieved a diagnosis of Ewing's sarcoma.
DISCUSSION
The prognosis of primary bone sarcomas of the extremities has significantly improved over the past three decades, particularly due to advancements in surgical techniques, imaging modalities, and chemotherapeutic protocols. These advancements have increased the 5-year survival rates from 10% to 70% during this time.8 Where previously orthopedic surgeons were amputating limbs, they are now able to perform LSS with preservation of function.9,10 Also, radiologists are able to perform CT-guided CNBs of bone lesions, which are accurate and reliable, in addition to being more cost-effective, less invasive, and carry fewer complications than open biopsies.6,11 In recent studies, CNBs have been shown to have accuracy rates ranging from 88% to 96% in bone sarcomas when adequate samples are obtained.3-6 Given its accuracy and rapidity (results within 24 hours), it has become an acceptable diagnostic tool for suspicious bone lesions especially since early diagnosis and management can greatly improve outcome.
It has been shown that the rate of local recurrence increases from 7% to 38% in patients who have undergone open biopsies without removal of the biopsy tract en-bloc.7 The question was raised as to whether surgeons should identify and excise the needle tract of CNBs at the time of the definitive surgery to avoid possible seeding of the tumor. This is important since local recurrence has been shown to negatively impact the survival of patients with operable bone sarcoma.12
A recent publication recommended that the CNB approach be made along the plane of the standard surgical incision13. This would make the job of the surgeon much easier, yet this biopsy approach may not always yield the most appropriate sample for accurate diagnosis especially when the tumor bulk is arising from the far cortex. This was observed in two of our patients where an anteromedial approach retrieved an inconclusive sample, but an accurate diagnosis was made from an anterolateral approach in one and a lateral approach in the other. This is important because an early, accurate diagnosis can greatly improve the patient's prognosis and multiple biopsy attempts would delay the definitive diagnosis and treatment. Of note, both techniques did not affect retrieval of tissue specimens for additional testing, especially for molecular diagnosis of solid tumors, mainly Ewing's and synovial sarcoma.
Davies et al. (1993) were the first to describe a case in which there was recurrence of the osteosarcoma along the needle biopsy tract.14 Most studies of bone sarcomas have not identified any reports of recurrence along the needle biopsy tract.15,16 As mentioned in a recent review of the literature, there has not been any quantification of the risk of recurrence in patients undergoing CNB without en-bloc resection of the tract.13 Additionally, in breast carcinoma, where there is an abundance of experience with CNB, studies have failed to show that the possibility of needle tract seeding is of any clinical significance.17,18 However, there is a general consensus that the biopsy must be performed in coordination between the interventional radiologist and the orthopaedic surgical oncologist so that the tract may be removed during the definitive surgery. Our study and review of the literature suggest that the incidence of tumor seeding the biopsy tract in bone sarcoma patients diagnosed by CNB and after follow-up of LSS without excision of the biopsy tract may not be high enough to warrant excision of the entire tract. In fact, we have not found any patient in our center that has experienced local recurrence of tumor at the biopsy tract after several years of follow-up.
Our study has several drawbacks, including the small number of patients, the inclusion of two histological types of bone sarcoma (Ewing sarcoma and osteosarcoma), and the multiple tumor sites, but all patients were treated along a well-established protocol, operated on by the same surgical team, and followed strict follow-up protocols. Given the rarity of bone sarcomas, conducting large, multi-center studies with long-term follow-up in order to fully quantify the risk of tumors seeding the biopsy tract would be quite a difficult, albeit unlikely, undertaking. Yet, any significant change in current practice would only be brought about by such studies. However, from our small study it seems that the rate of recurrence in these patients is apparently low, and possibly negligible.
REFERENCES
- 1.Herzog CE. Overview of sarcomas in the adolescent and young adult population. J Pediatr Hematol Oncol. 2005;27(4):215–218. doi: 10.1097/01.mph.0000161762.53175.e4. [DOI] [PubMed] [Google Scholar]
- 2.Hoeber I, Spillane AJ, Fisher C, Thomas JM. Accuracy of biopsy techniques for limb and limb girdle soft tissue tumors. Ann Surg Oncol. 2001;8(1):80–87. doi: 10.1007/s10434-001-0080-y. [DOI] [PubMed] [Google Scholar]
- 3.Mitsuyoshi G, Naito N, Kawai A, Kunisada T, Yoshida A, Yanai H, Dendo S, Yoshino T, Kanazawa S, Ozaki T. Accurate diagnosis of musculoskeletal lesions by core needle biopsy. J Surg Oncol. 2006;94(1):21–27. doi: 10.1002/jso.20504. [DOI] [PubMed] [Google Scholar]
- 4.Ng CS, Salisbury JR, Darby AJ, Gishen P. Radiologically guided bone biopsy: results of 502 biopsies. 1998;21(2):122–128. doi: 10.1007/s002709900227. Cardiovasc Intervent Radiol. [DOI] [PubMed] [Google Scholar]
- 5.Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. Am J Roentgenol. 1998;171(3):759–762. doi: 10.2214/ajr.171.3.ajronline_171_3_001. [DOI] [PubMed] [Google Scholar]
- 6.Issakov J, Flusser G, Kollender Y, Merimsky O, Lifschitz-Mercer B, Meller I. Computed tomography-guided core needle biopsy for bone and soft tissue tumors. Isr Med Assoc J. 2003;5(1):28–30. [PubMed] [Google Scholar]
- 7.Cannon SR, Dyson PHP. Relationship of the site of open biopsy of malignant bone tumors to local recurrence following resection and prosthetic replacement. J Bone Joint Surg Br. 1987;69(492) [Google Scholar]
- 8.Longhi A, Errani C, De Paolis M, Mercuri M, Bacci G. Primary bone osteosarcoma in the pediatric age: state of the art. Cancer Treat Rev. 2006;32:423–436. doi: 10.1016/j.ctrv.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 9.DiCaprio MR, Friedlaender GE. Malignant bone tumors: limb sparing versus amputation. J Am Acad Orthop Surg. 2003;11(1):25–37. [PubMed] [Google Scholar]
- 10.Hosalkar HS, Dormans JP. Limb sparing surgery for pediatric musculoskeletal tumors. Pediatr Blood Cancer. 2004;42(4):295–310. doi: 10.1002/pbc.10406. [DOI] [PubMed] [Google Scholar]
- 11.Altuntas AO, Slavin J, Smith PJ, Schlict SM, Powell GJ, Ngan S, Toner G, Choong PF. Accuracy of computed tomography guided core needle biopsy of musculoskeletal tumours. ANZ J Surg. 2005;75(4):187–191. doi: 10.1111/j.1445-2197.2005.03332.x. [DOI] [PubMed] [Google Scholar]
- 12.Weeden S, Grimer RJ, Cannon SR, Taminiau AH, Uscinska BM. European Osteosarcoma Intergroup. The effect of local recurrence on survival in resected osteosarcoma. Eur J Cancer. 2001;37(1):39–46. doi: 10.1016/s0959-8049(00)00362-2. [DOI] [PubMed] [Google Scholar]
- 13.Liu PT, Valadez SD, Chivers FS, Roberts CC, Beauchamp CP. Anatomically based guidelines for core needle biopsy of bone tumors: implications for limb-sparing surgery. RadioGraphics. 2007;27:189–206. doi: 10.1148/rg.271065092. [DOI] [PubMed] [Google Scholar]
- 14.Davies NM, Livesley PJ, Cannon SR. Recurrence of an osteosarcoma in a needle biopsy track. J Bone Joint Surg Br. 1993;75(6):977–978. doi: 10.1302/0301-620X.75B6.8245097. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz HS, Spengler DM. Needle Tract recurrences after closed biopsy for sarcoma: three cases and review of the literature. Ann Surg Oncol. 1997;4(3):228–236. doi: 10.1007/BF02306615. [DOI] [PubMed] [Google Scholar]
- 16.Jelinek JS, Murphey MD, Welker JA, Henshaw RM, Kransdorf MJ, Shmookler BM, Malawer MM. Diagnosis of primary bone tumors with imageguided percutaneous biopsy: experience with 110 tumors. Radiology. 2002;223(3):731–737. doi: 10.1148/radiol.2233011050. [DOI] [PubMed] [Google Scholar]
- 17.Knight R, Horiuchi K, Parker SH, Ratzer ER, Fenoglio ME. Risk of needle-track seeding after diagnostic image-guided core needle biopsy in breast cancer. JSLS. 2002;6(3):207–209. [PMC free article] [PubMed] [Google Scholar]
- 18.Michalopoulos NV, Zagouri F, Sergentanis TN, Pararas N, Koulocheri D, Nonni A, Filippakis GM, Chatzipantelis P, Bramis J, Zografos GC. Needle tract seeding after vacuum-assisted breast biopsy. Acta Radiol. 2008;49(3):267–270. doi: 10.1080/02841850701775030. [DOI] [PubMed] [Google Scholar]