Abstract
Background
Though pedestrian versus motor vehicle (PVMV) accidents are a common cause of trauma admission and subsequent orthopaedic consult, the prevalence of upper extremity fracture (UEF) in such events and its association with lower extremity injury (LEI) is unknown. We sought to describe UEF in PVMV accident patients at the time of orthopaedic consult.
Methods
A retrospective chart review was conducted for all pedestrian hit by motor vehicle cases for which an orthopaedic consult was performed at Jackson Memorial Hospital between July 2006 and January 2008. Fractures were recorded by location along with relevant clinical information. Logistic regression was used to calculate odds ratios (O.R.) and 95% confidence intervals (C.I.) for variables associated with UEF.
Results
336 cases were identified and reviewed. LEI was the most frequent injury type (67% of cases). UEF was also common, found in 25% of cases (humerus 11%, ulna 7%, radius 6%, hand 4%, and wrist 2%). Tibia or fibula fracture, femur fracture, and spine fracture were negatively associated with UEF in univariate analyses and after controlling for other associated factors.
Conclusions
In PVMV accident populations, UEF is a frequent injury often seen in the absence of any LEI. These findings emphasize the importance of carefully screening all PVMV accident patients for UEF and may call into question the usefulness of currently discussed injury pattern.
INTRODUCTION
Pedestrian versus motor vehicle (PVMV) accidents are a common cause of mortality and morbidity worldwide. In 2007 alone, 70,000 pedestrians were injured and another 4,654 killed in PVMV accidents in the United States.9 Despite these staggering numbers, PVMV accidents are an even larger problem in the developing world with mortality rates as high as 40 per 100,000 persons per year in some countries.1
Clinically the diagnosis of both orthopaedic and non-orthopaedic injuries is often complicated in PVMV cases by a loss of consciousness, the presence of multiple injuries, and high injury severity. The administration of pain medications, lack of symptoms from immobility, lack of associated lab abnormalities and reduced access to imaging can further complicate the diagnosis of orthopaedic injuries. For these reasons, clinical research efforts have employed biodynamic constructions and epidemiologi-cal review to identify predictors of orthopaedic injury following PVMV accidents.6,11,12
Biodynamic constructions describe the relationships between physical objects in an event. These models of PVMV accidents most often assume lower extremity vehicle contact is the initiating event and predict an injury sequence consisting of a lower extremity injury followed by injury to the body, head and upper extremities.4,7 Fitting with these predictions, epidemiological reviews of PVMV accidents have shown lower extremity injury to be the most prevalent injury type; however, there is little evidence to support the clinical utility of other injury associations. One examination of the existence of such a pattern found the triad of head, pelvis, and knee in only 10 of 115 patients.2
Epidemiological review of PVMV accidents is complicated by the heterogeneity and uniqueness of many such cases as well as variations in referral patterns.5,8 Despite these challenges, the discovery of orthopaedic injury predictors could lead to improved patient care and resource utilization. This is especially true for injuries such as upper extremity fractures (UEF) which can be difficult to diagnose, are traditionally underappreciated in PVMV accidents, and are associated with increasing morbidity such as impaired function, pain, and deformity. We, therefore, sought to describe the relative frequency and clinical associations of UEF in PVMV accident at the time of orthopaedic consults through a retrospective review of over 300 such cases.
MATERIALS AND METHODS
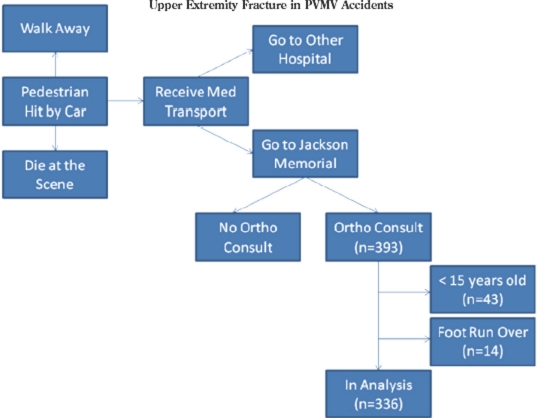
A retrospective chart review was conducted for all PVMV accident cases for which the pedestrian was brought to Jackson Memorial Hospital, a level I trauma center with multiple emergency rooms, and for which an orthopaedic consult was performed between July 2006 and January 2008 (Figure 1). A team of medical students, an orthopaedic resident and an orthopaedic attending reviewed medical records. All fractures were recorded by location along with relevant clinical information including age, gender, length of hospital stay, chest injuries, abdominal injuries, and neurological injuries. Patients less than 15 years of age were excluded and those involved in a foot run over by vehicle incident (Figure 1). A database was constructed to allow for the grouping of variables and statistical analysis using STATA 9.0. IRB approval for this project was obtained from the University of Miami's IRB.
Figure 1.
Identification of Cases and Selection for Analysis
Humerus, ulna, radius, wrist, and hand fractures were grouped together as UEF. Femur, tibia, fibula, ankle, and foot fractures were grouped with knee fractures and ligament tears as lower extremity injuries (LEI).
STATISTICAL METHODS
A series of Fisher's Exact tests were performed to identify if any of the recorded injuries or groups of injuries was associated with a UEF. Variables associated with UEF at a two sided alpha of less than 0.05 on univariate analysis were used in a logistic regression model. Odds ratios (O.R.) and 95% confidence intervals (C.I.) are reported for all variables associated with UEF at alpha less than 0.05 with logistic regression. Due to the frequency of both femur and tibia-fibula fractures, Fisher's exact test was performed to examine the statistical significance of the relationship with P value reported.
RESULTS
393 PVMV accident cases were initially identified and reviewed. Forty-three cases were excluded because the patient was less than 15 years of age and 14 more were excluded as foot run over by vehicle cases leaving a total sample of 336 PVMV accident cases (Figure 1). Of 336 cases, 225 (67%) were male, 265 (79%) were less than 65 years of age, and 115 (34%) spent over 10 days in the hospital (Table 1). Death occurred in only 9 cases (3%).
TABLE 1.
Patient Characteristics of 336 Adult PVMV Accident Orthopaedic Consult Cases
| Characteristic | N(%) |
|---|---|
| Gender | |
| Male | 225 (67) |
| Female | 111 (33) |
| Age by Trauma Groups | |
| 15-65 Years | 265 (79) |
| >65 Years | 67(20) |
| Missing | 4 (1) |
| Hospital Stay | |
| <1 Day | 53 (16) |
| 1-3 Days | 92 (27) |
| 4-10 Days | 76 (23) |
| 11-30 Days | 70 (21) |
| >30 Days | 45 (13) |
UEF's were found in 85 cases (25%) and were distributed throughout the extremity: humerus 38 (11%), ulna 24(7%), radius 20 (6%), hand 14 (4%), and wrist 7 (2%) (Table 2). Of the 85 cases with an UEF, 15 (18%) had multiple UEF's: 7 cases of both ulna and radius fractures, 1 cases of both ulna and radius plus wrist fractures, 3 cases of either an ulna or radius fracture and hand or wrist fracture, 2 cases of humerus and forearm fractures, 2 cases of humerus and either hand or wrist fractures. For a description of the frequency of all injuries please see Appendix.
TABLE 2.
Prevalence of UEF in 336 PVMV Accident Orthopaedic Consult Cases
| Injury | N (%) |
|---|---|
| Upper Extremity | 85 (25)* |
| Humerus Fracture | 38 (11)* |
| Ulna Fracture | 24 (7)* |
| Radius Fracture | 20 (6)* |
| Hand Fracture | 14 (4)* |
| Wrist Fracture | 7 (2)* |
15 cases had multiple UEF's
Univariate analysis found tibia or fibula fracture, femur fracture, and spine fracture to all be negatively as-sociated with UEF (Appendix 1). All were still negatively associated with UEF on logistic regression: tibia or fibula fracture (O.R. = 0.46, 95%C.I. = 0.27-0.78), femur fracture (O.R. = 0.30, 95%C.I. = 0.11-0.80), and spine fracture (O.R. = 0.42, 95%C.I. = 0.19-0.90). Odds ratios and adjusted odds ratios are presented in Table 3.
TABLE 3.
UEF Associated Injuries with Adjustments for 336 PVMV Accident Orthopaedic Consult Cases
| Absence of Injury | O.R. (95%C.I.) | Adjusted O.R. (95%C.I.) |
|---|---|---|
| Tibia or Fibula Fracture | 0.54 (0.32-0.90) | 0.46 (0.27-0.78) |
| Spine Fracture | 0.46 (0.22-0.99) | 0.42 (0.19-0.90) |
| Femur Fracture | 0.35 (0.13-0.92) | 0.30 (0.11-0.80) |
LEI's were the most common injury, encountered in 226 cases (67%). Amongst LEI's tibia and or fibula fractures were the most common injury occurring in 148 cases (44%). Fractures of the femur were also common occurring in 43 cases (13%) and negatively related to the tibia-fibula fractures. Femur fracture occurred in just 8% of cases without a tibia-fibula fracture as compared to 16% of cases without, p = 0.03. LEI were negatively associated with UEF (O.R. = 0.33, 95%C.I. = 0.20-0.55).
DISCUSSION
In a review of 336 PVMV accident cases for which an orthopedic consult was called, UEF was found in 25% of cases, suggesting this is a common injury following such events. Consistent with previous epidemiological reviews and biodynamic models, LEI was the most common injury overall. Though we found no positive clinical associations with UEF, negative associations existed between UEF and both LEI and spinal fractures. These finding highlight the heterogeneity of PVMV accident cases and the need for careful screening of patients involved in such events. The results also demonstrate that many PVMV accidents likely do not involve lower extremity contact as the initiating event.
These findings should be viewed in relation to other previously described samples of PVMV accidents. Peng et al. examined a sample in which a lower extremity fracture was found in just 24% of adult cases fitting with their case identification from 13 different trauma centers (5 level I, 7 level II) throughout Los Angeles County.10 In this mix of cases which may have included increased numbers of less severe cases, only 8% of adult patients had an UEF. Brainard et al. examined cases brought to a single level I trauma facility in Arizona.3 Their sample had a mortality rate of 22% and tibia-fibula fractures in 39% of cases. In this group of more severe cases, 30% of patients had an UEF. In contrast to our findings, however, they reported a statistically significant positive relationship between upper extremity fracture and an ipsilateral lower extremity fracture, the “Ipsilateral dyad".
The frequency of UEF and negative relationship between UEF and both LEI and spine fractures should be interpreted with caution as our selection strategy may have underrepresented the least and most severe cases. As Jackson Memorial Hospital is home to the region's only level one trauma center, it is likely a greater proportion of more severe cases were brought in. It is also possible that for some of the less severe cases that were brought in, no orthopedic consult was ordered. At the same time, the most severe cases may have been missed as death may have preempted the orthopaedic consult. Figure 1 provides a representation of the logistics challenges in identifying and defining cases from PVMV accidents. A second limitation to this study is the retrospective design and subsequent lack of systematic protocol for the identification of injuries including orthopaedic injuries. Finally, with only 336 cases used in the analysis and the low frequency of certain injuries, it is possible the statistical comparisons could have been underpowered.
In conclusion, there are likely many PVMV accident cases that do not resemble the currently proposed biodynamic models. This accident heterogeneity likely explains the difficulty researchers have in finding clinically useful predictors of PVMV accidents from epide-miological reviews. The large number of UEF cases we found and the negative relationship between UEF and LEI suggest not only that the initiating event in many PVMV accidents may not involve the lower extremity but also that UEF may be a more frequent consequence of PVMV accidents than previously appreciated. Physicians responsible for PVMV accident cases should be careful to consider the possibility of UEF in all patients regardless of LEI status.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
REFERENCES
- 1.Ameratunga S, Hijar M, Norton R. Road-traffic injuries: confronting disparities to address a global-health problem. Lancet. 2006;367:1533–40. doi: 10.1016/S0140-6736(06)68654-6. [DOI] [PubMed] [Google Scholar]
- 2.Brainard BJ, Slauterbeck J, Benjamin JB, Hag-man RM, Higie S. Injury profiles in pedestrian motor vehicle trauma. Ann EmergMed. 1989;18:881–3. doi: 10.1016/s0196-0644(89)80218-5. [DOI] [PubMed] [Google Scholar]
- 3.Brainard BJ, Slauterbeck J, Benjamin JB. Fracture patterns and mechanisms in pedestrian motor-vehicle trauma: the ipsilateral dyad. JOrthop Trauma. 1992;6:279–82. doi: 10.1097/00005131-199209000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Crandall JR, Bhalla KS, Madeley NJ. Designing road vehicles for pedestrian protection. Br Med J. 2002;324:1145–8. doi: 10.1136/bmj.324.7346.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeAngelis JP, Aubin M, Krompinger WJ. Open fracture dislocation of the thoracic spine: a case re port. Spine J. 2007;7:491–4. doi: 10.1016/j.spinee.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Demetriades D, Murray J, Martin M, Velmahos G, Salim A, Alo K, Rhee P. Pedestrians injured by automobiles: relationship of to injury type and sever ity. JAm Coll Surg. 2004;199:382–7. doi: 10.1016/j.jamcollsurg.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 7.Eid HO, Abu-Zidan FM. Biomechanics of road traffic collision injuries: a clinician's perspective. Singapore Med J. 2007;48:693–700. [PubMed] [Google Scholar]
- 8.Galloway DJ, Patel AR. The pedestrian problem: a 12-month review of pedestrian accidents. Injury. 1982;13:294–8. doi: 10.1016/0020-1383(82)90324-2. [DOI] [PubMed] [Google Scholar]
- 9. National Highway Traffic Safety Administration (2008) Traffic Safety Facts 2007: Pedestrians. Pub lication DOT-HS-810-994. Available at: http://www.nhtsa.dot.gov. Accessed February 25, 2009.
- 10.Peng RY, Bongard FS. Pedestrian versus motor vehicle accidents: an analysis of 5,000 patients. J Am Coll Surg. 1999;189:343–8. doi: 10.1016/s1072-7515(99)00166-0. [DOI] [PubMed] [Google Scholar]
- 11.Starnes MJ, Hadjizacharia P, Chan LS, Demetriades D. Automobile versus pedestrian injuries: does gender matter? JEmerg Med. 2008;23:507–12. doi: 10.1016/j.jemermed.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 12.Yanar H, Demetriades D, Hatzizacharia P, Nomoto S, Salim A, Inaba K, Rhee P. Pedestrians injured by automobiles: risk factors for cervical spine injuries. JAm Coll Surg. 2007;205:794–9. doi: 10.1016/j.jamcollsurg.2007.06.280. [DOI] [PubMed] [Google Scholar]