Abstract
Sea urchin injuries to the hand are uncommon. A variety of home remedies can be found on the internet and other sources for dealing with this problem in the acute setting. Many long term complications such as granulomas, arthritis, and tenosynovitis can result from a neglected sea urchin injury. We report an unusual case of a patient with a remote sea urchin injury who presented with ulnar digital nerve paresthesias. A traumatic neuroma was found on surgical exploration. We review the literature on injuries to the hand caused by sea urchins and their management. Management of sea urchin injuries to the hand with retained spines requires surgical debride-ment in order to prevent significant long term complications including stiffness, tenosynovitis, granulomas, and arthritis.
INTRODUCTION
Sea urchin injuries to the hand are more commonly seen in coastal regions of the world where humans may come into contact with the animals either accidentally or intentionally. Sea urchins are animals belonging to the class Echinoidea. They are found in salt water habitats throughout the world. There are over 600 unique species of which 80 are toxic to humans. The most common species around the western coast of the United States are Strongylocentrotus purpuratus and Strongylocentrotus franciscanus. Their spines are made of calcium carbonate and are not in themselves poisonous. The spines can contain poisons including histamine, serotonin, glycosides, steroids, cholinergic substances, and bradykinin-like substances.14 Hands unfortunately are often the point of contact between sea urchins and humans.
The initial injury results in pain, erythema, burning, edema, and inflammation at the site of injury.1,2 Spines are brittle and can often fragment and break off in the hand. Complete removal of the offending spines typically terminates this reaction.3 Retained spines can result in a variety of complications including granulomas,4,5,6,7 arthritis,2,8,9,10 and synovitis.2,11,12 We report an unusual case of a digital nerve neuroma secondary to a retained sea urchin spine. We also review the English language literature on sea urchin injuries to the hand following a Pubmed search using the terms “sea urchin hand."
CASE REPORT
A 55 year old right hand dominant woman was on vacation in Hawaii. She and her husband were snorkeling when a large wave pushed her up on the rocky shore. While attempting to brace herself, her right hand landed on a sea urchin. She noted the immediate onset of pain and saw several purple pigmented puncture wounds at the base of her right ring finger (Figure 1). She went to an urgent care clinic where she had some of the spines removed followed by application of a dry dressing. Over the next few months, she continued to be bothered by a foreign body sensation as well as stiffness of the ring finger and paresthesias in the ulnar digital nerve distribution.
Figure 1.
Initial injury to right hand demonstrating tattooing of the skin at sites of sea urchin spine penetration.
The patient presented to our clinic ten weeks after her initial injury with a chief complaint of a foreign body sensation at the base of the right ring finger. Several scars from puncture wounds were visible at the base of the ring finger. There was a palpable mass along the ulnar border of the ring finger at the level of the mid-proximal phalanx. The patient demonstrated significant stiffness with a pulp to palm distance of approximately one centimeter. She had diminished sensation to light touch along the ulnar aspect of her ring finger. There was no Tinel's sign present. MRI demonstrated a possible foreign body as well as extensive flexor tenosynovitis (Figure 2).
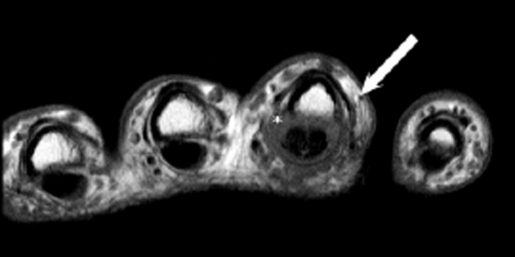
Figure 2.
A Tl-weighted axial MRI demonstrating significant flexor tenosynovitis of the ring finger (asterix) as well as a possible retained spine (tip of arrow).
The patient was taken to the operative theater for surgical exploration. A Bruner type surgical incision was made on the volar aspect of the ring finger.13 Multiple small fragments of what appeared to be sea urchin spines were embedded in the subcutaneous tissues, flexor tendon sheath, and flexor digitorum superficialis tendon. There were also multiple small fragments of foreign material embedded in a bulbous expansion of the ulnar digital nerve (Figure 3). All of the fragments were carefully removed from the tissues and an extensive flexor tenosynovectomy was carried out. The exploration was extended into the palm in order to fully release the adherent flexor digitorum profundus and superficialis tendons. Postoperatively, the patient was placed into an early motion therapy protocol.
Figure 3.
View of the volar aspect of the ring finger at the palmodigital crease demonstrating the ulnar digital neuroma (short arrow) and small retained fragments of sea urchin spine (long arrow).
DISCUSSION
Immediately following a sea urchin injury, patients typically will complain of significant pain at the site of injury. Systemic symptoms including hypotension, pares-thesias, and weakness can result from a bolus of toxin. The flower sea urchin Toxopneustes pileolus contains a dangerous neurotoxin which can produce numbness, muscle paralysis, respiratory distress and death.15 Examination of the affected hand will often reveal puncture wounds and purplish tattoo-like coloration at the site of spine entry. A variety of “home remedies” for sea urchin injuries can easily be found on the internet. These in-elude removal of visible spines, hot water soaks, vinegar soaks, and ammonia soaks among others. There is little in the medical literature on the acute management of these injuries. It has been reported that the complete removal of the spines will cause the local reaction to subside.3 A reasonable approach dictates the removal of easily accessible spines and a careful physical examination for possible joint involvement.7,16 A low threshold for surgical exploration should be present if there is concern for a traumatic arthrotomy. The majority of patients, at least initially after a sea urchin injury, will unfortunately not be seen by a hand surgeon.
If the patient is evaluated by a hand surgeon, it is imperative that a complete workup is carried out. The surgeon should first be certain that the patient has received a tetanus booster if needed. An accurate history documenting the date of the injury as well as any treatment rendered should be obtained. A thorough physical examination should follow documenting any visible scars, joint deformity, range of motion deficits, and neurovascular status. Plain radiography should be performed as the calcium in spines should render them radiopaque.2 However, a report by Wada noted that no spines were visible on plain radiography in their series of five patients.10 Ultrasonography is an affordable next step in the diagnostic imaging work-up of sea urchin injuries.2 A report by Groleau et al. describes the use of ultrasound to identify several spines and tenosynovitis in the case of sea urchin injury to the hand.17 As in our case, MRI can also identify pathology associated with the sea urchin injury such as spine location and any associated bone and soft tissue changes.2,9
Surgical options should be dictated by the patient's clinical presentation and the results of the workup. If a patient presents early with only a minimally debilitating foreign body sensation, simple removal of the offending spine versus observation may be chosen. The surgeon should also be aware of the potential for septic arthritis and infectious flexor tenosynovitis. If, as in our case, the patient presents with stiffness and a foreign body sensation, the surgeon should be prepared for exploration including careful inspection of the flexor tendon sheath. Intra-operative aerobic, anaerobic, mycobacterial and fungal cultures should be routinely obtained. Surprisingly, reports in the literature cite no evidence for active infection in chronic sea urchin injuries.2,10
Complications of untreated sea urchin injuries to the hand include arthritis, granuloma formation, flexor tenosynovitis, and persistent dorsal edema.18 Arthritis from sea urchin injuries has been described in the literature.2,10 The arthritis seen in association with sea urchin granulomas demonstrates joint space narrowing, osteolysis, subchondral sclerosis, and periosteal reaction on plain radiographs. The progression of arthritis is often slow when compared to that associated with the septic arthitidies.2 If neglected, this arthritis can progress to total joint destruction. Wada et al reported on 5 patients with sea urchin spine arthritis.10 They recommended a thorough synovectomy and joint debridement for patients with chronic irritation.10 Cooper and Wakefield reported a patient with granulomatous synovitis and arthritis that ultimately required an amputation due to loss of motion.8 It is thought that the arthritis seen in sea urchin injuries is a result of synovitis and granuloma
formation. Granuloma formation after sea urchin injury was first reported by Gate in 1936.19
Inflammatory or infectious tenosynovitis is another known complication of sea urchin injuries. Infectious tenosynovitis appears shortly after the initial injury.20 A patient presenting with the classic Kanavel signs21 should undergo emergent operative debridement and culture-guided antibiotic therapy though cultures are often negative.20 A more indolent course is associated with inflammatory tenosynovitis. This patient may recover from the initial insult and have a period of minimal to no symptomatology.2 They then typically notice a gradual increase in swelling and diminished range of motion in the affected finger or fingers. As noted in our case, and those presented by Lamir and Groleau, MRI or ultrasound can reveal the soft tissue swelling and tenosynovitis associated with chronic inflammation.9,17 These patients benefit from a thorough tenosynovectomy and removal of any offending foreign material.2,10 Antibiotics and anti-inflammatories are not useful in these cases.2,10
Our case is unusual in that our patient had a neuroma secondary to sea urchin spine penetration of the ulnar digital nerve. Our case highlights the appropriate measures that need to be taken in order to successfully address a chronic injury resulting from a sea urchin injury. These include a thorough pre-operative workup including history and physical examination and the use of appropriate imaging modalities including plain radiographs, ultrasound, and MRI if needed. Surgical exploration can then be undertaken including spine removal, tenosynovectomy and, if indicated, appropriate sampling for cultures and pathology. This should be followed by early motion therapy protocol postoperatively. If these steps are followed, successful return of function is possible even for patients with chronic hand injuries from sea urchins provided that irreversible changes such as arthritis or bone loss have not occurred.
REFERENCES
- 1.McWilliams LJ, et al. Spinous injury caused by a sea urchin. J Clin Pathol. 1991;44:428. doi: 10.1136/jcp.44.5.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guyot-Drouot MH, et al. Arthritis, tenosynovitis, fasciitis, and bursitis due to sea urchin spines. A series of 12 cases in Reunion Island. Joint Bone Spine. 2000;67:94–100. [PubMed] [Google Scholar]
- 3.Baden HP. Injuries from sea urchins. Clin Dermatol. 1987;5:112–117. doi: 10.1016/s0738-081x(87)80017-2. [DOI] [PubMed] [Google Scholar]
- 4.De la Torre CC, Toribio JJ. Sea-urchin granu-loma:histologic profile. A pathologic study of 50 biopsies. J Cutan Pathol. 2001;28:223–228. doi: 10.1034/j.1600-0560.2001.028005223.x. [DOI] [PubMed] [Google Scholar]
- 5.Kabigting FD, et al. Sea urchin granuloma secondary to Strongylocentrous purpuratus and Strongylocentrous franciscanus. Derm Online J. 2009;15(5):9. [PubMed] [Google Scholar]
- 6.Rossetto AL, et al. Sea urchin granuloma. Rev Med.Trop Sao Paulo. 2006;48(5):303–306. doi: 10.1590/s0036-46652006000500013. [DOI] [PubMed] [Google Scholar]
- 7.Strauss MB, MacDonald RI. Hand injuries from sea urchin spines. Clin Orthop Relat Res. 1976;114:216–218. [PubMed] [Google Scholar]
- 8.Cooper PP, Wakefield MMC. A sarcoid reaction to injury by sea urchin spines. J Pathol. 1974;112:33–36. doi: 10.1002/path.1711120107. [DOI] [PubMed] [Google Scholar]
- 9.Liram H, et al. Sea urchin puncture resulting in PIP joint synovial arthritis: case report and MPJ study. J Travel Med. 2000;7:43–45. doi: 10.2310/7060.2000.00015. [DOI] [PubMed] [Google Scholar]
- 10.Wada T, et al. Sea urchin spine arthritis of the hand. J Hand Surg. 2008;33A:398–401. doi: 10.1016/j.jhsa.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 11.Cracchiolo AA, Goldberg LL. Local and systemic reactions to puncture by the sea urchin spine and the date palm thorn. Arthritis Rheum. 1977;20:1206–1212. doi: 10.1002/art.1780200608. [DOI] [PubMed] [Google Scholar]
- 12.Reginato AJ, et al. Clinical and pathologic studies of twenty-six patients with penetrating foreign body injury to the joints, bursae, and tendon sheaths. Arthritis Rheum. 1990;33:1753–1762. doi: 10.1002/art.1780331201. [DOI] [PubMed] [Google Scholar]
- 13.Bruner JM. The zig-zag volar-digital incision for flexor-tendon surgery. Plast Reconstr Surg. 1967;40(6):571–574. doi: 10.1097/00006534-196740060-00010. [DOI] [PubMed] [Google Scholar]
- 14.Rocha G, Fraga S. Sea urchin granuloma of the skin. Arch. Derm. 1962;85:406–408. doi: 10.1001/archderm.1962.01590030104017. [DOI] [PubMed] [Google Scholar]
- 15.Michael LS. Skin problems from marine echinoderms. Derm Ther. 2002;15:30–33. [Google Scholar]
- 16.Nassab R., at al The management of hand injuries caused by sea urchin spines. J Hand Surg Europ. 2005;30B(4):432–433. doi: 10.1016/j.jhsb.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Groleau S, et al. Ultrasonography of foreign-body tenosynovitis. Can Assoc Radiol J. 1992;43(6):454–6. [PubMed] [Google Scholar]
- 18.Angelini G, Vena GA, Meneghini CL. Occupational traumatic lymphedema of the hands. Dermatol. Clin. 1990;8(1):205–208. [PubMed] [Google Scholar]
- 19.Gaté J, et al. Lésions papulo-necrotiques a reaction histologique tuberculoi'de dues a l'inclusion d'epines d'oursins. Bull. Soc,Frang. Derm. Syph. 1936;43:937. [Google Scholar]
- 20.Coombs CJ, Mutimer KL. Echinoidea tenosynovitis. Aust. N. Z.J. Surg. 1993;63:309–311. doi: 10.1111/j.1445-2197.1993.tb00389.x. [DOI] [PubMed] [Google Scholar]
- 21.Kanavel AB. A guide to the surgical treatment of acute and chronic suppurative processes in the fingers, hand, and forearm. 7th edition. Philadelphia, USA: Lea and Febiger; 1943. Infections in the hand. [Google Scholar]