Abstract
Background
In cases of suspected isolated greater trochanteric fracture, difficulty exists in establishing a definitive diagnosis when plain film is equivocal for fracture extension. There are reports of magnetic resonance imaging (MRI) being used to diagnose greater trochanter fractures, with varying treatment and follow-up, however validation of treatment based on MRI findings is lacking. To date, there is no consensus on the best way to manage isolated greater trochanteric fractures. Current treatment protocols are based on plain films. The purpose of this study is to offer a more effective means of treating patients with these fractures, and to stimulate further study of isolated greater trochanteric fractures based on MRI interpretation.
Methods
Patients from May 2001 to May 2003 with a clinical picture consistent with that of a hip fracture who had equivocal plain film evidence of an isolated greater trochanteric fracture received MRI scanning. Ten patients (five male and five female) ranging in age from 59-90 (mean age 79) showed a presumed isolated greater trochanteric fracture on MRI defined as a linear, vertical band of decreased signal (Tl-weighted) extending from the greater trochanter that did not cross the mid-line. These patients were allowed immediate weight bearing as tolerated and followed for an average of 15 months. Patients were contacted by telephone during this period and any problems were noted. Problems were defined as any limitations (pain, inability to ambulate) due to the presumed hip fracture.
Results
All ten patients diagnosed with an isolated greater trochanteric fracture on MRI reported no limitations during the follow-up period.
Conclusions
The linear, vertical bands of decreased signal (T1-weighted) extending from the greater trochanter and not crossing the midline on MRI can be considered isolated greater trochanteric avulsions, and can be managed with immediate weight-bearing.
INTRODUCTION
The greater availability of MRI has had an increasing role in the diagnosis and treatment of hip fractures. It has been recommended that in cases of suspected occult hip fractures, MRI should be performed if plain radiographs are not diagnostic.1,2,3,4,5,6,7 MRI has also been indicated when plain film radiographs show a fracture of the greater trochanter, due to plain film's inability to show the extent of the lesion, leading to questions about safe treatment.8,9,10 Since CT scans may be inaccurate7 and bone scans are less cost effective,11 a better understanding of MRI findings is indicated.
Fractures isolated to the greater trochanter region are rare.12 Recommended treatments for greater trochanteric fractures can include bedrest,13 taping,14 hip spica casting,15 and internal fixation.15 Recently, Omura employed only bed rest in a single patient, but no follow-up outcome was reported.8 Craig used unspecified non-operative treatment in three patients, also with no clinical outcomes reported.9 Feldman employed bed rest for patients, with clinical and radiographic healing at two months follow-up.10
To date, however, there has been no definition of what constitutes an isolated greater trochanter fracture on MRI. Ingari found that a low signal on MRI (typically black in appearance) indicated an impaction of the trabecular bone.16 The literature has focused on MRI's ability to detect previously overlooked fractures, but has neglected definitive lesion description.7,8,9,10,11,12,17,18,19,20 Although the consensus is that MRI can detect the presence of a lesion with great accuracy,7,8-9,10,11,12,17,18,19,20 there has been no definition of the appearance of suspected greater trochanteric fractures on MRI, and what differentiates them from intertrochanteric fractures. Despite this lack of knowledge, work has been done using presumed criteria17 to make diagnoses of isolated greater trochanter fractures, and treatments have been recommended.
The primary hypothesis we tested is that a linear, vertical band of decreased signal (Tl-weighted) extending from the greater trochanter without crossing the midline is consistent with an isolated greater trochanteric avulsion. Schultz states that intertrochanteric fractures that do not cross the midline on MRI may be treated conservatively.17 Therefore, we allowed immediate weight-bearing in our cohort of patients presumed to have isolated greater trochanteric fractures. Because there was no progression of fractures despite weight bearing, we can offer both a more effective treatment for presumed greater trochanter fractures and describe the appearance of a presumed isolated greater trochanter fracture as seen on MRI.
MATERIALS AND METHODS
Patients from May 2001 to May 2003 who were admitted due to an initial diagnosis of hip fracture were scanned by MRI. Initial diagnoses were made by the following criteria: hip pain, difficulty with weight bearing and irritable passive range of motion of that joint. Study patients had plain films which were interpreted as showing a greater trochanteric fracture but which were equivocal for the degree of extension into the intertrochanteric region (Figure 1). Inclusion criteria for the study required a presumed isolated greater trochanter fracture on MRI. The fracture was defined as a linear, vertical band of decreased signal extending from the greater trochanter that did not cross the midline on MRI. There were five males and five females who met the inclusion criteria, with a mean age of 79 (range, 53-90). MRIs were taken using a GE 1.5 Tesla Signa scanner running on 5.4.2 software. Coronal Tl images were taken with a slice thickness of 4mm, and an inter-slice gap of lmm. Repetition time was 633 and echo time was 14.
Figure 1.
Equivocal plain film of greater trochanteric fracture.
All patients showing a presumed isolated greater trochanteric fracture were then permitted immediate weight bearing as tolerated, often with the assistance of a walker. Patients were followed for an average of 15 months (range, 6-31 months). Patients were contacted by telephone during this period and any problems were noted. Problems were defined as any limitations (pain, inability to ambulate) due to the hip fracture.
RESULTS
Examples of presumed greater trochanteric fractures which met our inclusion criteria are depicted in Figure 2. All ten patients diagnosed with a presumed isolated greater trochanteric fracture reported no limitations during the follow-up period. One patient passed away during this period, but reported no problems with the hip prior to death.
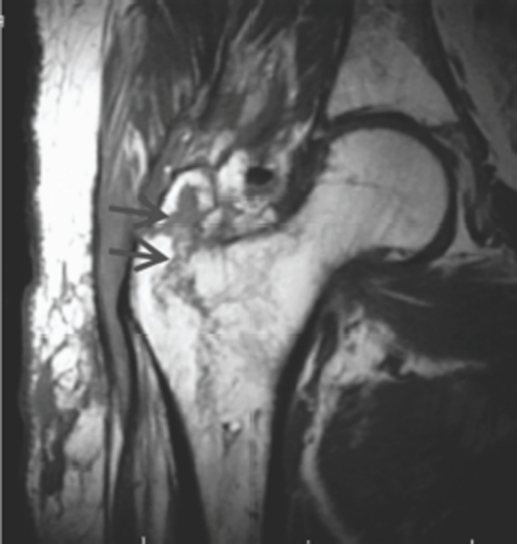
Figure 2.
Characteristic T1 MRI of greater trochanter fracture. Note the black vertical band extending from the greater trochanter which does not cross the midline
DISCUSSION
Suspected hip fractures in the Emergency Department can be challenging. In our study, patients complained of hip pain and had difficulty weight bearing, but had equivocal plain films for a diagnosis of an isolated greater trochanteric fracture. Hip fractures are now being diagnosed by MRI even when they are not demonstrated by plain films,1,2,3,4 bone scans12 or CT.2 MRI also more accurately defines the true extent of the injury.8,9,10 With the ever-increasing availability of MRI it is widely believed that isolated greater trochanter fractures (a linear vertical band of decreased signal extending from the greater trochanter and not crossing the midline) will be better identified.
We used Ingari's work in defining the appearance of hip fractures on MRI to make a presumed diagnosis of isolated greater trochanter fractures in our patients.16 Shultz reported that conservative treatment for incomplete intertrochanteric fractures, based on abnormal signal on MRI, yielded good outcomes with no reported complications. Therefore, we treated our patients who had a presumed diagnosis of isolated greater trochanter fractures with immediate weight-bearing.
Our study suffers from a small patient population which makes definitive assertions difficult. In addition, our conclusion is based solely on clinical data, as our goal of better treatment preclude surgical and pathological confirmation of the fracture. This problem means that we cannot make any conclusions about a link between the abnormal MRI signal and a pathologic diagnosis of greater trochanter fracture.
We allowed immediate weight bearing also because it possibly shorted hospitalization and decreased morbidity/mortality.21 Our results indicate that the linear, vertical bands of decreased signal (Tl-weighted) extending from the greater trochanter on MRI suggest an isolated greater trochanteric avulsion rather than an intertrochanteric fracture and that these fractures can be managed conservatively.
REFERENCES
- 1.Rizzo PF, Gould ES, Lyden JP, Asnis SE. Diagnosis of occult fractures about the hip. Magnetic resonance imaging compared with bone-scanning. J of Bone and Joint Surgery. 1993;75:395–401. doi: 10.2106/00004623-199303000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Deutsch AL, Mink JH, Waxman AD. Occult fractures of the proximal femur: MR imaging. Radiology. 1989;170:113–116. doi: 10.1148/radiology.170.1.2909083. [DOI] [PubMed] [Google Scholar]
- 3.Pandey R, McNally E, Ali A, BLustrode C. The role of MRI in the diagnosis of occult hip fractures. Injury. 1998;29:61–63. doi: 10.1016/s0020-1383(97)00165-4. [DOI] [PubMed] [Google Scholar]
- 4.Quinn SF, McCarthy Prospective evaluation of patients with suspected hip fracture and indeterminate radiographs: use of T1-weighted MR images. Radiology. 1993;187:469–471. doi: 10.1148/radiology.187.2.8475292. [DOI] [PubMed] [Google Scholar]
- 5.Newberg AH, Newman JS. Imaging the painful hip. Clin Orthop. 2003;406:1928. doi: 10.1097/01.blo.0000043040.84315.85. [DOI] [PubMed] [Google Scholar]
- 6.Zuckerman JD. Hip Fracture. New England Jof Med. 1996;334:1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 7.Lubovsky O, Liebergall M, Mattan Y, Weil Y, Mosheiff R. Early diagnosis of occult hip fractures MRI versus CT scan. Injury J. Care Injured. 2005;36:788–792. doi: 10.1016/j.injury.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Omura T, et al. Evaluation of isolated fractures of the greater trochanter with magnetic resonance imaging. Arch ofOrtho and Trauma Surgery. 2000;120:195–197. doi: 10.1007/s004020050042. [DOI] [PubMed] [Google Scholar]
- 9.Craig JG, Moed BR, Eyler WR, Holsbeeck MV. Fractures of the greater trochanter: intertrochanteric extension shown by MR imaging. Skeletal Radiol. 2000;29:572–576. doi: 10.1007/s002560000250. [DOI] [PubMed] [Google Scholar]
- 10.Feldman F, Staron RB. MRI of Seemingly Isolated Greater Trochanteric Fractures. AJR. 2004;183:323–329. doi: 10.2214/ajr.183.2.1830323. [DOI] [PubMed] [Google Scholar]
- 11.Rubin SJ, et al. Magnetic resonance imaging: a cost-effective alternative to bone scintigraphy in the evaluation of patients with suspected hip fractures. Skeletal Radiol. 1998;27:199–204. doi: 10.1007/s002560050365. [DOI] [PubMed] [Google Scholar]
- 12.Learch TJ, Pathria MN. Greater trochanter fractures: MR assessment and its influence on patient management. Emergency Radiology. 2000;7:89–92. [Google Scholar]
- 13.Merlino AF, Nixon JE. Isolated fractures of the greater trochanter. Report of twelve cases. International Surgery. 1969;52:117–124. [PubMed] [Google Scholar]
- 14.Ratzan MC. Isolated fracture of the greater trochanter of the femur. J Int Coll Surg. 1958;29:359–363. [PubMed] [Google Scholar]
- 15.Armstrong GE. Isolated fractures of the greater trochanter. Ann Surg. 1907;45:292–297. doi: 10.1097/00000658-190708000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ingari JV, Smith DK, Aufdemorte TB, Yaszemski MJ. Anatomic Significance of Magnetic Resonance Imaging Findings in Hip Fracture. Clin Ortho and related Research. Lippincott-Raven. 1996;332:209–214. doi: 10.1097/00003086-199611000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Shultz E, Miller TT, Boruchov SD, Schmell EB, Toledana B. Incomplete Intertrochanteric Fractures: Imaging Features and Clinical Management. Radiology. 1999;211:237–240. doi: 10.1148/radiology.211.1.r99mr24237. [DOI] [PubMed] [Google Scholar]
- 18.Hossain M, Barwick C, Sinha AK, Andrew JG. Is magnetic resonance imaging (MRI) necessary to exclude occult hip fracture? Injury J. Care Injured. 2007;38:1204–1208. doi: 10.1016/j.injury.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 19.Oka M, Monu JU. Prevalence and Patterns of Occult Hip Fractures and Mimics Revealed by MRI. AJR. 2004;182:283–288. doi: 10.2214/ajr.182.2.1820283. [DOI] [PubMed] [Google Scholar]
- 20.Verbeeten KM, et al. The advantage of MRI in the detection of occult hip fractures. Eur Radiol. 2005;15:165–169. doi: 10.1007/s00330-004-2421-2. [DOI] [PubMed] [Google Scholar]
- 21.Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison S. Early ambulation after hip fracture: Effects on function and mortality. Arch Intern Med. 2006;166:766–771. doi: 10.1001/archinte.166.7.766. [DOI] [PMC free article] [PubMed] [Google Scholar]