Abstract
Objective
The aims of this study were to investigate psychophysiological changes associated with peritraumatic dissociation in female victims of recent rape and to assess the relation between these changes and symptoms of posttraumatic stress disorder (PTSD).
Method
Eighty-five rape victims were examined in a laboratory setting within 2 weeks after the rape, and measures of heart rate, skin conductance, and nonspecific movement were collected. Self-report indexes of reactions to the trauma and interviews to assess PTSD symptoms and peritraumatic dissociation were also completed. On the basis of their scores on the Peritraumatic Dissociation Index, the subjects were classified as having low or high levels of dissociation.
Results
Items from the index exhibited good internal consistency, and scores were approximately normally distributed. Individuals in the high peritraumatic dissociation group showed a significantly different pattern of physiological responses from those of the low dissociation group. In general, there was a suppression of autonomic physiological responses in the high dissociation group. This group also contained a larger proportion of subjects (94%) identified as meeting PTSD symptom criteria. Also, among the high dissociation subjects there was a discrepancy between self-reports of distress and objective physiological indicators of distress in the laboratory setting.
Conclusions
The results provide preliminary support for the idea that there is a dissociative subtype of persons with PTSD symptoms who exhibit diminished physiological reactivity. The results also underscore the importance of assessing dissociative symptoms in trauma survivors.
The importance of peritraumatic dissociation as a factor in the development of posttraumatic stress disorder (PTSD) has garnered increasing support in the past few years. Historically, the link between exposure to traumatic events and dissociation was proposed in the writings of Janet on hysteria (1). More recently, van der Kolk and colleagues (2, 3) have argued for a link between dissociative experiences at the time of a trauma and later posttrauma symptoms. Recent studies (4–7) have noted the relation between within-trauma dissociation and the later development of PTSD. For example, Koopman et al. (4) found that in survivors of the Oakland/Berkeley firestorm, peritraumatic dissociative symptoms accounted for the most variance in predicting subsequent PTSD. Similarly, Holen (7) found that in survivors of an oil rig disaster in the North Sea, self-reports of dissociation during the disaster were a significant predictor of later PTSD. Koopman et al. argued that dissociation may be adaptive during and immediately following a traumatic event; however, the chronic use of dissociative mechanisms as a means of dealing with the trauma may lead to a failure to process the trauma cognitively and emotionally and therefore result in more severe posttrauma reactions.
Other researchers have noted the similarity of PTSD dissociative symptoms and hypnotic phenomena. In fact, in comparing the level of hypnotizability of combat veterans who had PTSD with that of subjects who had other disorders and of a normal control group, Spiegel et al. (8) found that the subjects with PTSD were significantly different from all the other groups. Subjects with generalized anxiety disorder had a hypnotizability score below that of the normal control group and half that of the subjects with PTSD. These authors concluded that PTSD is predominantly a dissociative disorder as opposed to an anxiety-based disorder. Marmar et al. (5) studied both peritraumatic dissociation and current dissociation, as measured with the Dissociative Experiences Scale, in predicting PTSD in combat survivors. They found that both types of dissociation improved the prediction of current PTSD beyond that accounted for by level of exposure to war zone stress. They noted, however, that the assessment of peritraumatic dissociation in their combat veterans was retrospective by at least 20 years, leading to the possibility of alterations in memory of the amount of peritraumatic dissociation in the veterans with more severe PTSD. There is little research examining peritraumatic dissociation soon after a trauma, when self-reports would be most reliable. A notable exception is the recent findings of Shalev et al. (6), who used a path analytic model in a prospective design. Their findings from trauma survivors assessed 1 week and 6 months after trauma suggest that peritraumatic dissociation may be the single most important variable in explaining PTSD scores 6 months after trauma. Further examination of acutely traumatized subjects will be helpful in establishing the link between peritraumatic dissociation and subsequent development of PTSD symptoms.
There also has been a call for more objective measures of PTSD to gain a better understanding of the disorder (9). One of the chief functions that objective indicators may serve is to elucidate whether there are specific components of posttrauma pathology that inhibit recovery from trauma, leading to chronic PTSD. There is currently little information relating objective measures of dissociative symptoms to PTSD.
In the present study, self-report and interview measures of psychopathology and dissociation in rape victims assessed within 2 weeks of assault were collected. In addition, measures of physiological arousal (skin conductance and heart rate) were collected in a laboratory setting. The main goals of the study were 1) to assess peritraumatic dissociation and PTSD symptoms soon after a traumatic event and 2) to improve upon existing self-report assessments of dissociation and trauma pathology by examining various objective indexes.
METHOD
The subjects consisted of 85 rape victims recruited primarily from local police departments (84%) plus victim assistance agencies (15%) and hospitals (1%). These agencies provided postcards to rape victims to mail back to us if they were interested in participating in the study. The subjects were assessed within 2 weeks after rape (mean= 10.3 days, SD=3.1, range=6–14). They were primarily low-income (66% with annual income <$5000), single (62%), African American (66%) women. They ranged in age from 18 to 54 years (mean=28.7 years, SD=7.8) and had an average of 12.6 years of education. Subjects were paid $70 for participation in the study. Victims were excluded from the study if there were more than 16 days between the rape and the assessment, if they were under 18 years of age, if they were inebriated at the time of the assessment, or if they had apparent psychosis. Subjects were also screened for the use of drugs that might confound autonomic responses, such as anticholinergics, β blockers, and digitalis. After complete description of the study to the subjects, written informed consent was obtained.
Laboratory assessments were conducted in an 8-ft×10-ft room that was sound-insulated and temperature- and humidity-controlled. Physiological measures of heart rate and nonspecific electrodermal responses (skin conductance) were generated by means of a Coulbourn Instruments (Allentown, Pa.) modular system. Heart rate measurements were obtained with an optical blood flow transducer attached to the nondominant hand on the distal phalanx of the second finger. The optical transducer was connected to a pulse monitor (Coulbourn, model S71-40) attached to a tachometer (Coulbourn, model S77-26). Measurements of skin conductance were obtained with silver/silver chloride 9-mm electrodes filled with isotonic paste (10) and attached to the nondominant hand on the first and third fingers at the distal phalanx. Electrodes were attached to a skin conductance module (Coulbourn, model S71-22), which applied a constant voltage (0.5 V) and was used in the AC coupled (quick change) mode. In addition, nonspecific subject movement data were obtained through an inflated air cushion that was placed in the back of the chair in which the subject was sitting. The air cushion was attached to a pressure sensor (Newark Electronics, Chicago, model 174PC) that sent output to a differential amplifier (Newark, model MC3503). The pressure sensor used four piezoresistive bridges to detect changes in the pressure applied to the pillow, and a differential output voltage was generated that was proportional to the applied pressure. Analog outputs from the physiological devices were converted to digital signals by an analog-digital converter (Coulbourn, model S25-12). Digital outputs were interfaced with an IBM-compatible computer with the use of a Coulbourn LabLinc Interface, which allowed real-time waveform display of the data. All measurements were collected at a rate of five samples per second. The equipment was located in a separate room adjacent to the subject assessment room.
Procedure
After the subjects had been asked to give informed consent, they were given paper-and-pencil questionnaires and a laptop computer questionnaire consisting of a number of self-report scales. Among the self-report measures were the PTSD Symptom Scale (11), the Rape Aftermath Symptom Test (12), and the Beck Depression Inventory (13). After completion of these instruments, the laboratory assessments were conducted.
The subject was seated in a comfortable armchair in the laboratory room, and physiological monitoring devices were attached. The assessment began approximately 5 minutes later in order to allow physiological readings to stabilize. There were five 5-minute phases of the laboratory assessment. The first phase was an initial resting baseline during which the interviewer left the subject alone in the room. After 5 minutes the interviewer returned and prompted the subject to talk about a neutral topic for the next 5-minute phase. The subject was given a prompt sheet with a list of possible topics to talk about during the neutral phase. The prompts were topics that would require the subject to recall and describe some past event (e.g., “a special meal you have prepared”). The subject was instructed that the interviewer would not be able to speak during the phase, in order to record 5 minutes of just the subject speaking. At the end of the neutral phase the interviewer left again for a second resting baseline. Upon returning, the interviewer prompted the subject to talk about the rape for the next 5-minute “trauma” phase. During this phase the subject was asked to describe the rape in detail, including aspects such as where she was, what the assailant said and did, and what her thoughts and reactions were. Again, the subject was told that only she would be speaking during the trauma phase. At the end of this period the interviewer again left for a final 5-minute resting baseline period. Subjective Units of Distress Scale (unpublished) scores were obtained at the end of each phase; scores ranged from 0 (“as relaxed and calm as you have ever been”) to 10 (“as upset or uncomfortable as you have ever been”). Physiological measures were collected throughout the entire laboratory assessment. This laboratory procedure was used to enable us to examine physiological and nonverbal behavioral reactions concurrently. The nonverbal data will be reported at a later time.
Following the laboratory assessment, the subjects were given the Clinician-Administered PTSD Scale (Form 2) (14) to determine PTSD symptom status for the past week. Because all of these subjects were assessed within 2 weeks after rape, an official diagnosis of PTSD was not possible; therefore, subjects were diagnosed as having or not having PTSD symptoms. In addition, an interviewer-based trauma interview, which provided trauma-specific information about subjects’ reactions during the sexual assault, was administered. This interview contained eight questions that assessed the dissociative experiences of the subject during the assault. Six of these questions were from the Peritraumatic Dissociative Experiences Questionnaire—Rater Version (5). Two items from that questionnaire were not used because they were less appropriate for rape victims. They were replaced with questions about whether the subject felt “confused or disoriented” or “numb” during the sexual assault. The questions that were used for this index are presented in appendix 1. Each item was rated on a 5-point scale, with 0 indicating “none of the time” and 4 indicating “all of the time.” The eight items were summed to generate a peritraumatic dissociation score for each subject. Dissociation measured in this way ranges from scores indicating no dissociation or mild forms of dissociation to scores indicating more severe dissociation during the traumatic event. On the basis of the score on this index, each subject was classified into a high or low dissociation group as described below.
Perception of life threat was also was measured during the trauma interview from two questions; the subject was asked, “During the incident did you think about being killed or seriously injured?” (responses ranged from 0=“not at all” to 4=“thought about it all the time”) and “During the incident how certain were you that you were going to be killed?” (0=“completely certain that I would not be killed,” 4=“completely certain that I would be killed”). The scores on these two items were summed, and thus the range of possible scores was 0–8. Depression diagnoses were assessed with use of the Structured Clinical Interview for DSM-III-R—Non-Patient Version (SCID-NP) (15).
Analyses
A computer scoring algorithm was written to evaluate the skin conductance waveforms. Any response in excess of 0.10 μS was counted as a valid skin conductance response, and frequency was tallied per phase. The amplitude of each valid response (trough to peak) was also determined, and an average amplitude expressed in microsiemens was calculated per phase. Heart rate was calculated as beats per minute, and averages were calculated per phase. The voltage outputs from the nonspecific movement data were reduced with the mean square successive difference statistic (δ2) (16). This statistic is related to the variance but gives a measure of the variability between successive points of data.
RESULTS
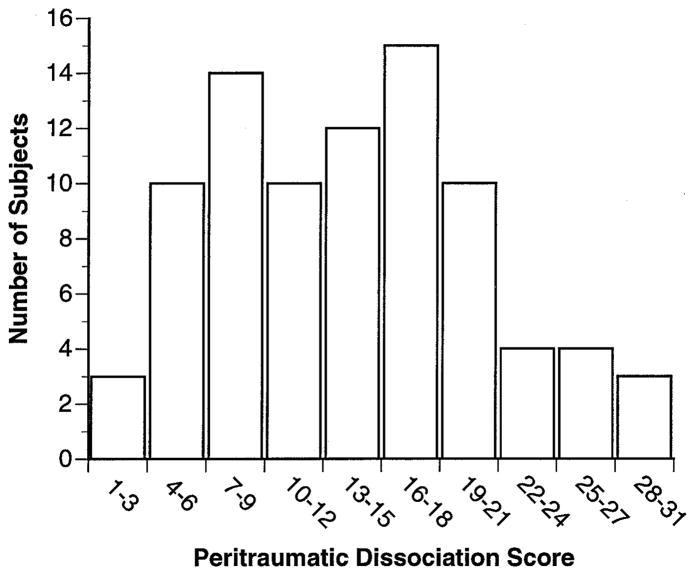
An initial assessment of the reliability of the Peritraumatic Dissociation Index was undertaken because it was modified from the published version of the Peritraumatic Dissociative Experiences Questionnaire—Rater Version (5). Cronbach’s alpha was 0.75 for the eight items constituting the dissociation index, indicating relatively good internal consistency for these items. The range of possible scores on this index was 0–32. The scores were approximately normally distributed (figure 1). On the basis of the scores from this index, subjects who scored more than 1 SD above the mean (scores from 21 to 32) were placed in the high dissociation group (N=16); those who scored more than 0.50 SD below the mean (scores from 1 to 10) were placed in the low dissociation group (N=31). Subjects with scores falling in the moderate range (scores of 11–20) were excluded from further analyses (N=38). The definitions for the high and low dissociation groups were based on the desire to have a high dissociation group that had clearly been dissociating most of the time during the trauma; hence our selection of a group that had a score 1 SD above the mean on the Peritraumatic Dissociation Index. We decided to use only 0.50 SD below the mean to define the cutoff for the low dissociation group because the distribution was positively skewed (skewness index=0.52; a score of 0.00 would indicate a perfectly symmetrical distribution). This procedure ensured that a group who clearly had experienced peritraumatic dissociation was compared with a group who clearly had not.
FIGURE 1. Frequency Distribution of Scores of 85 Rape Victims on the Peritraumatic Dissociation Index.
The frequencies of PTSD symptoms for the high and low dissociation groups are presented in table 1. Chi-square tests with Yates’s correction indicated a significant difference between expected and observed cell frequencies. The high dissociation group had a disproportionate number of subjects who met the symptom criteria for PTSD.
TABLE 1.
Self-Report and Diagnostic Interview Data of Rape Victims With Low or High Levels of Peritraumatic Dissociation
| Variable | Peritraumatic Dissociation Group |
Analysis | Correlation With Peritraumatic Dissociation Index Scorea | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Low (N=31) | High (N=16) | ||||||||
| N | % | N | % | χ2 | df | p | |||
| Clinician-Administered PTSD Scale diagnosis | 7.4 | 1 | 0.01 | ||||||
| No PTSD | 14 | 45 | 1 | 6 | |||||
| PTSD | 17 | 55 | 15 | 94 | |||||
| SCID-NP diagnosisb | 0.83 | 1 | n.s. | ||||||
| No depression | 22 | 71 | 8 | 57 | |||||
| Depression | 9 | 29 | 6 | 43 | |||||
| Mean | SD | Mean | SD | F | df | p | r | p | |
| Scores on self-report measures | |||||||||
| Peritraumatic Dissociation Index | 6.7 | 2.4 | 24.4 | 3.3 | — | — | — | — | — |
| PTSD Symptom Scale | |||||||||
| Reexperiencing | 5.9 | 2.6 | 7.7 | 3.1 | 4.6 | 1, 46 | 0.05 | 0.29 | 0.05 |
| Avoidance | 8.7 | 4.0 | 13.4 | 5.0 | 12.1 | 1, 46 | 0.001 | 0.40 | 0.01 |
| Arousal | 10.1 | 4.8 | 13.2 | 4.3 | 4.8 | 1, 46 | 0.05 | 0.30 | 0.05 |
| Total | 24.6 | 9.7 | 34.3 | 11.5 | 9.0 | 1, 46 | 0.005 | 0.38 | 0.05 |
| Beck Depression Inventory | 15.6 | 8.8 | 24.1 | 11.4 | 7.9 | 1, 45 | 0.005 | 0.32 | 0.05 |
| Global distress | 116.9 | 57.4 | 154.4 | 65.7 | 4.1 | 1, 45 | 0.05 | 0.31 | 0.05 |
| Life threat | 4.5 | 2.6 | 6.5 | 2.0 | 6.7 | 1, 46 | 0.01 | 0.24 | n.s. |
| Subjective Units of Distress Scale | 3.4 | 2.7 | 4.3 | 3.2 | 7.1 | 1, 225 | 0.01 | — | — |
Pearson zero-order correlation for the entire group of rape victims (N=85).
A depression diagnosis with the Structured Clinical Interview for DSM-III-R—Non-Patient Version was not obtained for two subjects in the high peritraumatic dissociation group.
Before analysis the physiological data were examined for univariate and multivariate outliers. Examination of detrended plots revealed two subjects with data for skin conductance responses that were more than 3.5 SD above the mean and two subjects with skin conductance amplitude that was more than 4.0 SD above the mean. These data were deemed to be outliers and were considered as missing. These subjects had peritraumatic dissociation scores that placed them in the low dissociation group. Evaluation of multivariate normality through Mahalanobis distance and homogeneity of variance-covariance matrices (17) after these deletions was satisfactory.
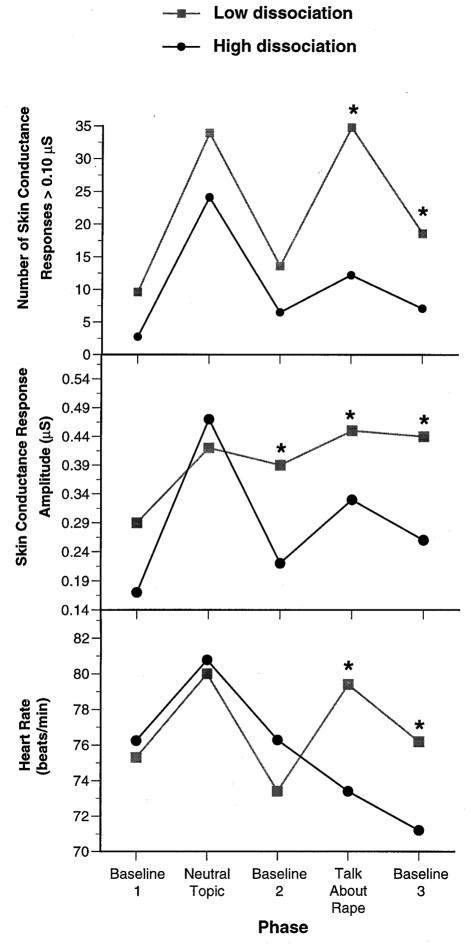
The main factors for the laboratory analyses were laboratory phase (initial resting baseline, neutral, second resting baseline, trauma, final resting baseline) as a repeated measures factor and group (high or low peritraumatic dissociation) as a between-subjects factor. A 2×5 mixed-design multivariate analysis of variance (MANOVA) was performed on the physiological variables: skin conductance responses, skin conductance amplitude, and heart rate. The independent variables were peritraumatic dissociation group and laboratory phase. The combined physiological variables showed a significant group-by-phase interaction (F= 2.1, df=12, 666, p<0.01; Pillai’s criterion [17]=0.11). Univariate analysis of variance for each physiological variable indicated a significant group-by-phase interaction for heart rate (F=14.6, df=4, 176, p<0.001), skin conductance responses (F=4.5, df=4, 176, p<0.005), and skin conductance amplitude (F=2.9, df=4, 176, p< 0.05). Follow-up analyses of simple main effects revealed significant differences between groups during the trauma phase (talk about the rape) and the final resting baseline (figure 2). A separate 2×5 mixed-design MANOVA was performed on the nonspecific subject movement data. Findings indicated no significant group main effects or group-by-phase interactions for the movement data.
FIGURE 2. Physiological Data Across Laboratory Study Phases of Rape Victims With Low or High Levels of Peritraumatic Dissociationa.
aAn asterisk indicates a significant difference between groups within a given phase (p<0.05).
Analyses of race effects were conducted to compare African American and white subjects on the physiological variables. The data indicated that there were no significant race main effects or race-by-dissociation-level interactions for each of the three physiological variables.
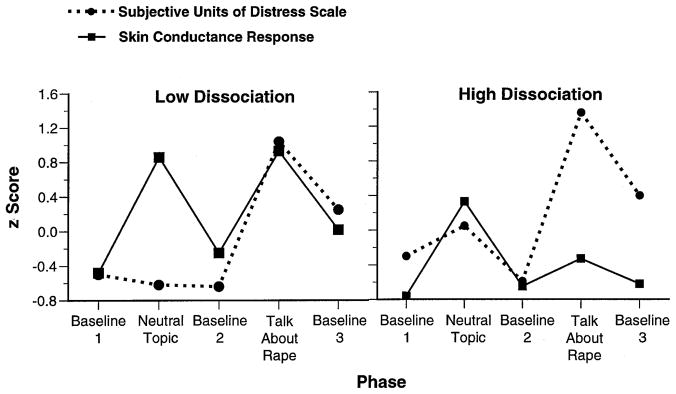
Subjects’ scores on the Subjective Units of Distress Scale at the end of each phase of the laboratory assessment were significantly higher in the high dissociation group than in the low dissociation group (table 1). We also compared the Subjective Units of Distress Scale scores with the physiological measure that provided the greatest difference between the high dissociation and low dissociation groups—skin conductance responses—by converting the data to z scores and then performing t tests with Bonferroni corrections for alpha level. For the high dissociation group, the results indicated a significant difference between the skin conductance response measure of distress and the self-reported distress scale scores during the trauma phase (talk about the rape) and the final baseline phase (t=5.7, df=15, p<0.001, and t=4.6, df=15, p<0.001, respectively) (figure 3). Both results indicated that these subjects’ self-report ratings of distress were significantly higher than their physiological measures of arousal. The low dissociation group’s self-reports of distress were in close agreement with their physiological measures of arousal except during the neutral phase, when self-reports of distress were significantly lower than the measures of physiological arousal (t=4.8, df=30, p<0.01) (figure 3).
FIGURE 3. Transformed Scores (z) on Skin Conductance Responses and the Subjective Units of Distress Scale Across Laboratory Study Phases of Rape Victims With Low or High Levels of Peritraumatic Dissociation.
Analyses of self-report data indicated significant group main effects on several measures of distress (table 1). The MANOVA of the subscales of the PTSD Symptom Scale revealed that the high dissociation group scored significantly higher than the low dissociation group on the combination of PTSD subscales (F=4.0, df=3, 43, p<0.05; Pillai’s criterion=0.22). Follow-up univariate analyses indicated that each subscale score (reexperiencing, avoidance, and arousal) was significantly greater for the high dissociation group. The high dissociation group also scored significantly higher on measures of global distress from the Rape Aftermath Symptom Test, the Beck Depression Inventory, and the index of perception of life threat during the rape.
To examine the role of peritraumatic dissociation in PTSD symptoms more closely, we conducted additional analyses of data from only the subjects who met the symptom criteria for PTSD. These subjects were divided into those with high dissociation scores (N=15) and those with low scores (N=17). This information is presented in table 2. A 2×5 mixed-design MANOVA was performed on the physiological data. The combined physiological variables showed a significant group-by-phase interaction (F=2.1, df=12, 666, p<0.01; Pillai’s criterion=0.11). Univariate analyses revealed significant group-by-phase interactions for heart rate (F=14.6, df=4, 176, p<0.001) and skin conductance response frequency (F=5.6, df=4, 176, p<0.005). For heart rate, examination of simple main effects revealed significant differences between groups during the trauma phase and final baseline phase, with the PTSD/high dissociation group displaying a significantly lower heart rate during these phases than the PTSD/low dissociation subjects. The high dissociation group displayed a significantly lower number of skin conductance responses than the low dissociation group during each phase except for the neutral phase. There was a trend for an overall group main effect on skin conductance amplitude.
TABLE 2.
Physiological and Self-Report Data of Rape Victims With PTSD Symptoms and Low or High Levels of Peritraumatic Dissociation
| Variable | PTSD Subjects With Low Dissociation (N=17) |
PTSD Subjects With High Dissociation (N=15) |
Analysis |
||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | F | df | p | |
| Physiological measures | |||||||
| Heart rate (bpm) | |||||||
| Baseline phase 1 | 73.6 | 10.9 | 76.2 | 7.8 | 0.5 | 1, 31 | n.s. |
| Neutral phase | 78.6 | 11.2 | 80.9 | 6.3 | 0.4 | 1, 31 | n.s. |
| Baseline phase 2 | 73.6 | 9.9 | 76.2 | 11.2 | 0.6 | 1, 30 | n.s. |
| Trauma phase | 80.8 | 9.4 | 72.7 | 5.4 | 3.4 | 1, 31 | 0.04 |
| Baseline phase 3 | 78.3 | 8.1 | 70.9 | 4.5 | 3.9 | 1, 31 | 0.03 |
| Skin conductance response (frequency) | |||||||
| Baseline phase 1 | 12.6 | 15.6 | 2.9 | 3.7 | 5.5 | 1, 31 | 0.03 |
| Neutral phase | 37.8 | 20.2 | 25.6 | 16.2 | 3.5 | 1, 30 | n.s. |
| Baseline phase 2 | 16.3 | 16.9 | 6.9 | 7.8 | 3.9 | 1, 31 | 0.05 |
| Trauma phase | 40.1 | 18.1 | 12.8 | 10.1 | 26.8 | 1, 31 | 0.001 |
| Baseline phase 3 | 23.7 | 15.2 | 7.0 | 6.5 | 15.6 | 1, 31 | 0.001 |
| Scores on self-report measures | |||||||
| Peritraumatic Dissociation Index | 7.5 | 2.4 | 24.3 | 3.5 | — | — | — |
| PTSD Symptom Scale | |||||||
| Reexperiencing | 6.7 | 2.6 | 8.2 | 2.4 | 2.9 | 1, 31 | 0.10 |
| Avoidance | 10.0 | 3.4 | 14.3 | 3.7 | 11.6 | 1, 31 | 0.002 |
| Arousal | 11.6 | 4.2 | 14.1 | 2.6 | 3.7 | 1, 31 | 0.06 |
| Total | 28.4 | 8.8 | 36.5 | 7.2 | 8.1 | 1, 31 | 0.01 |
| Beck Depression Inventory | 18.8 | 7.9 | 25.7 | 9.7 | 4.9 | 1, 30 | 0.05 |
| Global distress | 139.3 | 50.0 | 164.7 | 52.9 | 1.9 | 1, 30 | n.s. |
| Life threat | 3.8 | 2.9 | 6.4 | 2.1 | 8.3 | 1, 31 | 0.01 |
DISCUSSION
The results indicate that there is a relatively normal distribution of peritraumatic dissociative symptoms during rape-related trauma. The Peritraumatic Dissociation Index demonstrated good internal consistency in a group of recent rape victims, which supports the use of this type of scale for assessing peritraumatic dissociation in trauma victims. The subjects identified as the high peritraumatic dissociation group were more likely to have PTSD symptoms than those who did not dissociate during the rape. This is compelling evidence for a link between dissociation and the genesis of PTSD, supporting previous theory (18). This finding is in agreement with previous studies of other trauma populations (6, 19) and suggests that peritraumatic dissociation may be a risk factor for the development of PTSD rather than an adaptive coping mechanism as previously suggested (4).
The finding that the high dissociation group had a higher perception of life threat during the rape than the low dissociation group supports the suggestion that peritraumatic dissociation is a coping strategy for severe trauma. The evidence suggests, however, that it may have maladaptive consequences that take the form of an enhanced risk of PTSD. It may be that dissociation during the trauma is a mechanism used to deal with extreme anxiety (20), as would be likely under conditions of life threat. Our findings suggest that this dissociative mechanism may come to be used in future situations when the traumatic material is brought back to consciousness. Given that therapy techniques for treatment of PTSD typically have an exposure component (21, 22), these results have important implications for treatment. Dissociation during therapeutic exposure will likely reduce the efficacy of these procedures.
Peritraumatic dissociation appears to have a global effect on PTSD symptoms, with an impact across the symptom clusters. The self-report data suggest that the high dissociation subjects were more distressed than the low dissociation subjects, with indications of greater disruptions emerging on each of the PTSD subscale dimensions. Of interest, the biggest difference between the high and low dissociation groups was on the avoidance subscale. This was true when we compared all the high dissociation and low dissociation subjects (table 1) and when we compared only the subjects who had PTSD symptoms (table 2). Further, there was a strong correlation (0.40) between PTSD Symptom Scale avoidance scores and Peritraumatic Dissociation Index scores. Marmar et al. (5) also found a strong relationship between peritraumatic dissociation and avoidance as measured by the Impact of Event Scale in combat veterans. It appears that persons with high levels of dissociation are more likely to use avoidance strategies to deal with the trauma. The link between dissociation and general avoidance of the trauma deserves further study. Other self-report data indicated that the high dissociation group was more globally distressed and depressed than the low dissociation group.
The results of the physiological assessment indicate a suppression of autonomic responses in the high dissociation group compared with the low dissociation group. This finding appears to be rather trauma-specific: significant differences between groups emerged at the trauma and posttrauma baseline phases for each of the physiological measures. Lower physiological reactivity in the high dissociation group is surprising in light of the fact that most of the members of this group had PTSD symptoms. This finding contrasts with previous findings of generally higher physiological reactivity in subjects with PTSD (23–26). The response of subjects in the high dissociation group may provide evidence of a specific PTSD subtype of highly dissociative individuals who may respond with a general physiological numbness. The direct comparisons of subjects with PTSD symptoms who scored either high or low on the Peritraumatic Dissociation Index support the idea that there is a subgroup of persons with PTSD who fail to respond to trauma-related stimuli. The existence of a physiologically nonreactive PTSD subgroup may provide an explanation for the equivocal results in some PTSD physiological studies (27). This dissociative subgroup of PTSD subjects may mask the differences in the PTSD group as a whole. It is interesting that comparison of the self-reports of distress in the laboratory interviews contradicted the physiological responses. Subjects in the high dissociation group reported feeling subjectively aroused and upset when talking about the rape and immediately after; however, their physiological responses showed a marked suppression during these phases of the laboratory assessment. This incongruity deserves further exploration, because it is unclear whether subjects in the high dissociation group are responding in a socially accepted way when they report that they are distressed and upset after talking about the trauma or whether they truly subjectively feel upset yet show physiological evidence of being shut down (lack of association between affect and physical reactivity).
A strength of the present study was the short period of time between the traumatic event and the start of the assessment (approximately 10 days). Memory loss and/or pathology-induced memory reconstruction, which are likely with long delays between trauma and assessment, are unlikely to have contaminated our findings. However, the limitation that this short time period imposes is the inability to make an official diagnosis of PTSD. Future research should prospectively assess trauma survivors soon after the trauma and then follow up at some point when a PTSD diagnosis can be made. This will allow an examination of the long-term effects of peritraumatic dissociation on chronic PTSD.
Another difficulty with the present data is that the high dissociation subjects scored significantly higher on the Beck Depression Inventory than the low dissociation subjects. The mean Beck inventory score for the high dissociation group placed them in the moderately depressed category. This raises the issue of greater depression in the high dissociation subjects, and perhaps this explains their suppressed physiological response to the trauma. However, at least with regard to the physiological data, previous findings do not support this conclusion. Orr et al. (23) found physiological differences between combat veterans with PTSD and those without PTSD. The mean Beck Depression Inventory scores of their PTSD subjects were comparable to the Beck inventory scores of the subjects in our high dissociation group.
In sum, the findings support the idea that there is a dissociative subtype of persons with PTSD who may not process traumatic information, which may lead to greater levels of PTSD symptoms. This dissociative PTSD group also responds with a suppression of physiological responsiveness in a laboratory setting. These findings indicate the importance of dissociative symptoms in posttrauma reactions and suggests the need to screen for level of peritraumatic dissociation in psychophysiological studies of PTSD. Treatment studies may also need to examine level of dissociation during therapeutic exposure as an impediment to successful outcome.
Acknowledgments
Supported by NIMH grant MH-46992 to Dr. Resick.
The authors thank John Stern, Ph.D., and Mary Uhlmansiek for consultation and assistance with the psychophysiology measures and Lisa Black, Katie Berezniak, Dana Cason, Lisa Ellis, Terese Evans, Michelle Myers, Gail Pickett, and Monica Schnicke for assistance with diagnostic interviews.
APPENDIX 1. The Peritraumatic Dissociation Indexa
During the assault
Did you feel confused or disoriented?
Did you feel numb?
Did you have moments of losing track of what was going on—that is, did you “blank out” or in some other way not feel you were part of the experience?
Did you find yourself going on “automatic pilot”—that is, doing something that you later realized you had done but had not actively decided to do?
Did your sense of time change during the event—that is, did things seem unusually speeded up or slowed down?
Did what was happening seem unreal to you, as though you were in a dream or watching a movie or a play?
Were there moments when you felt like you were a spectator, watching what was happening to you—that is, did you feel as if you were floating above the scene or observing it as an outsider?
Were there moments when your sense of your own body seemed distorted or changed—that is, did you feel yourself to be unusually large or small, or did you feel disconnected from your body?
Footnotes
Presented in part at the 10th annual meeting of the International Society for Traumatic Stress Studies, Chicago, Nov. 5–9, 1994.
Items used to assess the level of peritraumatic dissociation in rape victims. Items 3–8 were adopted from the Peritraumatic Dissociative Experiences Questionnaire—Rater Version (5).
References
- 1.Janet P. The Major Symptoms of Hysteria. New York: Macmillan; 1920. [Google Scholar]
- 2.van der Kolk BA, Brown P, van der Hart O. Pierre Janet on post-traumatic stress. J Trauma Stress. 1989;2:365–378. [Google Scholar]
- 3.van der Kolk BA, van der Hart O. Pierre Janet and the breakdown of adaptation in psychological trauma. Am J Psychiatry. 1989;146:1530–1540. doi: 10.1176/ajp.146.12.1530. [DOI] [PubMed] [Google Scholar]
- 4.Koopman C, Classen C, Spiegel D. Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif, firestorm. Am J Psychiatry. 1994;151:888–894. doi: 10.1176/ajp.151.6.888. [DOI] [PubMed] [Google Scholar]
- 5.Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL. Peritraumatic dissociation and posttraumatic stress disorder in male Vietnam theater veterans. Am J Psychiatry. 1994;151:902–907. doi: 10.1176/ajp.151.6.902. [DOI] [PubMed] [Google Scholar]
- 6.Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry. 1996;153:219–225. doi: 10.1176/ajp.153.2.219. [DOI] [PubMed] [Google Scholar]
- 7.Holen A. The North Sea oil rig disaster. In: Wilson JP, Raphael B, editors. International Handbook of Traumatic Stress Syndromes. New York: Plenum; 1993. pp. 138–154. [Google Scholar]
- 8.Spiegel D, Hunt T, Dondershine HE. Dissociation and hypnotizability in posttraumatic stress disorder. Am J Psychiatry. 1988;145:301–305. doi: 10.1176/ajp.145.3.301. [DOI] [PubMed] [Google Scholar]
- 9.Orr SP. Psychophysiologic studies of posttraumatic stress disorder. In: Giller EL Jr, editor. Biological Assessment and Treatment of Posttraumatic Stress Disorder. Washington DC: American Psychiatric Press; 1990. pp. 135–157. [Google Scholar]
- 10.Fowles DC, Christie MJ, Edelberg R, Grings WW, Lykken DT, Venables PH. Publication recommendations for electrodermal measurements. Psychophysiology. 1981;18:232–239. doi: 10.1111/j.1469-8986.1981.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 11.Foa EB, Riggs DS, Dancu C, Rothbaum BO. Reliability and validity of a brief instrument for assessing PTSD. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 12.Kilpatrick DG. Rape Aftermath Symptom Test. In: Hersen M, Bellack AS, editors. Dictionary of Behavioral Assessment Techniques. New York: Pergamon Press; 1988. pp. 366–367. [Google Scholar]
- 13.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 14.Blake DD, Weathers FW, Nay LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behavior Therapist. 1990;18:187–188. [Google Scholar]
- 15.Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R—Non-Patient Version (SCID-NP) New York: New York State Psychiatric Institute, Biometrics Research; 1989. [Google Scholar]
- 16.Leiderman PH, Shapiro D. Application of a time series statistic to physiology and psychology. Science. 1962;138:141–142. doi: 10.1126/science.138.3537.141. [DOI] [PubMed] [Google Scholar]
- 17.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 3. New York: Harper-Collins; 1996. [Google Scholar]
- 18.Spiegel D, Cardeña E. Disintegrated experience: the dissociative disorders revisited. J Abnorm Psychol. 1991;100:366–378. doi: 10.1037//0021-843x.100.3.366. [DOI] [PubMed] [Google Scholar]
- 19.Bremner JD, Southwick S, Brett E, Fontana A, Rosenheck R, Charney DS. Dissociation and posttraumatic stress disorder in Vietnam combat veterans. Am J Psychiatry. 1992;149:328–332. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- 20.Moleman N, van der Hart O, van der Kolk BA. The partus stress reaction: a neglected etiological factor in postpartum psychiatric disorders. J Nerv Ment Dis. 1992;180:271–272. doi: 10.1097/00005053-199204000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Foa EB, Kozak MJ. Emotional processing of fear: exposure to corrective information. Psychol Bull. 1986;99:20–35. [PubMed] [Google Scholar]
- 22.Resick PA, Schnicke MK. Cognitive Processing Therapy for Rape Victims: A Treatment Manual. Newbury Park, Calif: Sage Publications; 1993. [Google Scholar]
- 23.Orr SP, Claiborn JM, Altman B, Forgue DF, deJong JB, Pitman RK, Herz LR. Psychometric profile of posttraumatic stress disorder, anxious, and healthy Vietnam veterans: correlations with psychophysiologic responses. J Consult Clin Psychol. 1990;58:329–335. doi: 10.1037//0022-006x.58.3.329. [DOI] [PubMed] [Google Scholar]
- 24.Orr SP, Pitman RK, Lasko NB, Herz LR. Psychophysiological assessment of posttraumatic stress disorder imagery in World War II and Korean combat veterans. J Abnorm Psychol. 1993;102:152–159. doi: 10.1037//0021-843x.102.1.152. [DOI] [PubMed] [Google Scholar]
- 25.Pitman RK, Orr SP, Forgue DF, Altman B, de Jong JB, Herz LR. Psychophysiologic responses to combat imagery of Vietnam veterans with posttraumatic stress disorder versus other anxiety disorders. J Abnorm Psychol. 1990;99:49–54. doi: 10.1037//0021-843x.99.1.49. [DOI] [PubMed] [Google Scholar]
- 26.Shalev AY, Orr SP, Pitman RK. Psychophysiologic response during script-driven imagery as an outcome measure in posttraumatic stress disorder. J Clin Psychiatry. 1992;53:324–326. [PubMed] [Google Scholar]
- 27.Prins A, Kaloupek DG, Keane TM. Psychophysiological evidence for autonomic arousal and startle in traumatized adult populations. In: Friedman MJ, Charney DS, Deutch AY, editors. Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to PTSD. Philadelphia: Lippincott-Raven; 1995. pp. 291–314. [Google Scholar]