Abstract
An understanding of functional responses in oral bone is a crucial component of dental biomechanics. The purpose of this study was to investigate the potential biological remodelling response during mastication on the mandibular pre- and post-insertion of a fixed partial denture (FPD). A series of three-dimensional (3D) finite element analysis (FEA) models were presented pre- and postextraction to determine the biomechanical responses to masticatory loading in the anterior mandible. Equivalent strains were analysed at lingual/buccal and mesial/distal areas of the premolar to molar region and quantified to anticipate bone remodelling response. Mandibular bone incorporating an FPD experienced substantially greater stress/strain magnitudes than that prior to placement of fixed prosthodontics, which is suggestive of engagements of bone remodelling. The results suggest similar outcomes to those reported clinically. Developing a simulation reflecting the outcomes of restorative treatment can provide meaningful insight into restorative treatment planning, clinical outcomes, and fixed prosthodontics designs.
1. Introduction
Stress/strain redistributions occurring within mandibular bone as a result of prosthodontic treatments are highly complex and an understanding of the biomechanical factors (strains) initiating bone remodelling due to prosthodontic procedures has not been conclusive so far [1]. For this reason an in-depth understanding of the biological activity in the supporting abutments and bone structures is required as a means for possible improving the outcomes of such restorations. Therefore a detailed biomechanical model becomes essential, especially in typical clinical cases, in order to develop a computational biomechanical simulation capable of identifying the quantitative mechanical response to fixed prosthodontic treatment.
Fixed Partial Dentures are commonly used as a conservative prosthodontic treatment option in restorative dentistry with proven clinical reliability [2, 3] and have played an integral role in the rehabilitation of oral function for years. However, the rigid construction of FPD systems changes the local biomechanical status, whereby bone may model and remodel to accommodate a new loading environment. Thus a critical factor that determines the long-term success of FPDs is how occlusal forces are transferred to the surrounding root abutments, periodontal ligament (PDL), and bone. Bone remodelling is dependent on the maximum load experienced throughout its load history [4]; however, remodelling is also characterised by the number of daily cycles that are consistent with mastication [5, 6]. In typical three-unit fixed partial dentures, the tooth root abutment-bone interface must be able to tolerate changes in occlusal force behaviour without instigating adverse bone tissue responses. In this sense, understanding the effect of biomechanics on biological response is a key step to optimal design of an FPD. In general, the three main biomechanical issues related to an FPD are ( 1) mechanical loading, ( 2) transmission of the load to the interfacial tissues, and ( 3) biological reactions of surrounding tissues to the transmitted load [7].
The quantity and quality of bone depend on its functionality and remodelling responses [8]. There have been a number of phenomenological remodelling theories available for different bone sites [9]. Frost's mechanostat theory is one of such which defines a threshold Minimum Effective Strain (MES) as a mechanical stimulus to trigger bone remodelling [10]. Frost's theory has been applied to various studies [11, 12]. An MES remodelling threshold has been suggested in the range of 0.0008–0.002 unit bone surface strain, below which it is suggestive of bone resorption and above which it is indicative of bone apposition.
Clinically, an FPD can be established immediately upon tooth extraction or more often upon extraction socket healing. Resorption is an inevitable consequence of extraction of a natural tooth due to local bone disuse. Although the resorption may not be eliminated completely, its severity can be reduced by ensuring that the prosthesis transmits mechanical loads to the underlying bone structure properly [13, 14].
Previous investigations [15, 16] conducted on fixed prosthodontics have mainly focused on technical complications and stress peaks within the prosthetic devices. While in other clinical scenarios, tooth-implant systems incorporating an FPD has been evaluated [17–19] for assessing bone-implant osseointegration. Despite their relevance, limited studies have been reported on the biomechanical responses of mandibular bone as a consequence of fixed prosthodontics. Indeed, the complexity of biological reactions surrounding an FPD have made it very difficult to draw general conclusions about the prognosis of restorative treatments with FPDs in general dental practice [20].
This paper aims to establish the stress/strain patterns in mandibular bone to identify the initial status of remodelling stimulus, thereby correlating the finite element (FE) results with clinical observation. In order to achieve a precise quantitative analysis of the initial mechanical responses to loading on an FPD, a biomechanical model is essential as the detailed anatomical configuration of dental structures could largely affect their behaviours [21, 22]. For this reason, computerized-tomograph- (CT-) based 3D finite element analysis (FEA) techniques will be employed in this study to understand the biomechanics in the PDL-bone interface contiguous to abutments of an FPD. It is expected that an increased knowledge in this region can help establish a quantitative relationship associated with biological reactions such as bone remodelling.
2. Material and Methods
This study primarily focuses upon mandibular bone predictive or modelled strain responses as a direct result of mastication. Three-dimensional computational models of a section of the mandible with teeth were established in this study, representing the right mandibular premolar, first and second molars, and their supporting dental apparatus with/without a three-unit fixed partial denture. The finite element models employed in this study were constructed primarily using Computerized Tomography (CT) images, digital edge detection technique, and computer aided design (CAD) methods [23–25].
In the present paper, Models A and B are of prefixed prosthodontics initially upon first molar extraction and following a healing period of 12-months without FPD construction, respectively. Models C and D are presented following the three-unit FPD established upon initial tooth extraction and after a 12 month healing period. The extracted tooth model (Models A and C) simulated the removal of the first right molar and the wounded bone structure, immediately after extraction. Bone morphology upon extraction results in the localised extraction sockets which vary between 2.0 and 4.5 mm [26] with a width decrease up to approximately 50% as well as an unchanged the mesial/distal attachment [27]. The healed tooth model (Models B and D) incorporates the first right molar bone socket area of extraction after a 12-month healing period. The fresh bone socket is healed with a pocket depth of 1.1 mm, width of 7.6 mm, and mesial/distal attachment levels of 0.3 mm [27]. This study will compare the mechanical strains within mandibular bone between the extracted and healed scenarios with prefixed prosthodontics and FPD situations.
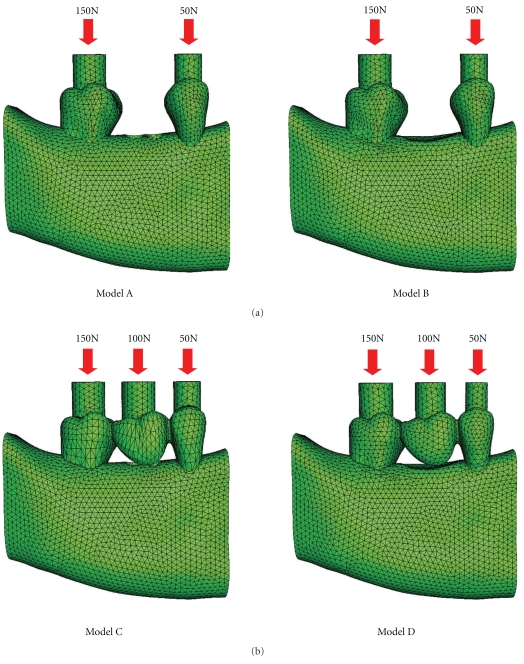
Models A, B, C, and D (Figure 1) were the basis for the comparative FE analyses that were conducted in ABAQUS 6.6.1 (ABAQUS, Inc, Providence, RI). The models consisted of a 10-node quadratic tetrahedral solid mesh. To establish these four models, relevant convergence tests were performed to determine the best balanced accuracy and efficiency of numerical simulation, as in [24], which led to a global element edge length of 1 mm to ensure the sophistication of the models and an optimal computational cost. Finally, Models A, B, C, and D consisted of 124 196 (DOF: 897 516), 115 675 (DOF: 836 202), 124 520 (DOF: 900 975) and 116 781 (DOF: 847 851) quadratic elements, respectively.
Figure 1.
Load Cases for (a) prebridgework models and (b) FPD models.
The models were subjected to occlusal forces which functionally varied for each tooth and the FPD. Loads of 50 N, 100 N, and 150 N were applied to the second premolar, first molar, and second molar, respectively (Figure 1). Vaillancourt [28] suggested that an adequate functional loading of 50 N is sufficient for a premolar. Schwarz [29] stated that the molar region can endure mastication forces of up to 3 times greater than the force experienced in the canine region. Thus, mastication forces in this study are classified within an upper range of normal bitting forces [30, 31]. Three-dimensional surface-to-surface contact with solid foods was modelled with a friction coefficient of 0.2 [32], as defined in ABAQUS (Figure 1).
All the materials were presumed linear, elastic, homogeneous, and isotropic for the analyses as widely adopted in existing literature [33, 34] (Table 1). The periodontal ligament (PDL) stress-strain experienced in this paper is well fitted to the linear elastic range for the strains of higher than 5% but less than 20% [35]. Although PDL is viscoelastic in nature, the isotropic elastic properties were assigned as the load response lies within the linear elastic range. Bone in this study is also modelled isotropically like previous studies [26, 36]. Isotropic models of the mandible were able to distinguish meaningful strain differences when replicating functional loading [23], which have been widely accepted by clinicians when evaluating patients [37].
Table 1.
Material properties required within the FEA models [25].
| Material | Young's modulus (MPa) | Poisson's ratio |
|---|---|---|
| Enamel | 84 100 | 0.20 |
| Dentin | 18 600 | 0.31 |
| PDL | 70.3 | 0.45 |
| Cancellous bone | 1500 | 0.30 |
| Cortical bone | 15 000 | 0.30 |
| All ceramic FPD | 140 000 | 0.28 |
The FE analyses of Models A, B, C, and D primarily focused upon the stresses and strains within the alveolar and cortical bony tissues. The biomechanical differences due to mastication in the pre-FPD and FPD cases are evident within the contiguous bone. Numerical values for strains in the extracted and healed cases were taken from distal, mesial, lingual, and buccal sites. Each site contained five representative reading points. Comparisons between the models were made through the von Mises stresses, principal stresses, and equivalent strains. Firstly, von Mises stresses were evaluated to provide distortion energies as an indicator to overall tissue deformation. Then, the first and third principal stresses were characterised to highlight tension and compression behaviours in these specific sites, where the nature of these stresses may affect bone remodelling. Finally, the equivalent strains were acquired to enable a measure of quantifying instigators into bone remodelling. Equivalent strain represents an aggregate elastic distortion within the bony tissues, which can be calculated from components of principal strains (e 1, e 2, e 3) as follows [38]:
| (1) |
According to Frost's remodelling theory [39], the equivalent strain is considered one of the most appropriate indicators of effectively predicting bone remodelling.
3. Results
The finite element analyses indicated that the elevated von Mises stresses occurred in the cortical ridges of functionally loaded teeth, suggesting high distortion energy distributions there. The maximum von Mises stresses are located around the second molar roots at the lingual site in Model A and the distal region in Models B, C, and D. Their corresponding values are 37.5 MPa, 36.2 MPa, 27.3 MPa, and 23.3 MPa, respectively.
The maximum first principal stresses in mandibular bone of Models A and B (without FPD) were situated at the cortical ridge about the mesial aspect of the second molar, which were 10.2 MPa and 11.5 MPa, respectively. It is noted that the freshly extracted case has a slightly lower tensile stress peak than the healed case. The maximum first principal stresses in Models C and D (with FPD) were located about the distal region of the second molar and were 25.1 MPa and 21.9 MPa, respectively, in which the FPD in the healed case presents a 15% lower tensile stress peak. It is noted that all these first principal stress peaks are positive, indicating a tension in the surrounding areas.
The maximum third principal stresses in the mandibular bone were situated in the lingual region of the cortical ridge in Models A, B, C, and D, where the peak values were −58.1 MPa, −57.7 MPa, −16.9 MPa, and −15.5 MPa, respectively. It is noted that all these third principal stress peaks are consistently negative, indicating a compressive nature at these sites. A comparison of the first and third principal stress peaks about the first molar are summarised in Table 2.
Table 2.
Principal stress distributions within mandibular bone about the first molar.
| Models | Model A | Model B | Model C | Model D | ||||
|---|---|---|---|---|---|---|---|---|
| Mandibular regions | 1st Principal | 3rd Principal | 1st Principal | 3rd Principal | 1st Principal | 3rd Principal | 1st Principal | 3rd Principal |
| MPa | MPa | MPa | MPa | MPa | MPa | MPa | MPa | |
| Mesial | 0.0678 | −0.6858 | 0.5682 | −1.1842 | 0.5683 | −1.2497 | 0.0476 | −2.9229 |
| Distal | 0.3240 | −1.4606 | 0.3873 | −2.9878 | 0.1401 | −3.4564 | 0.8327 | −4.4230 |
| Lingual | 0.4605 | −0.2243 | 1.0551 | −0.1918 | 0.7376 | −0.3386 | 0.9415 | −0.1087 |
| Buccal | 0.1805 | −0.2521 | 0.3399 | −0.8702 | 0.2673 | −0.7362 | 0.5908 | −2.1959 |
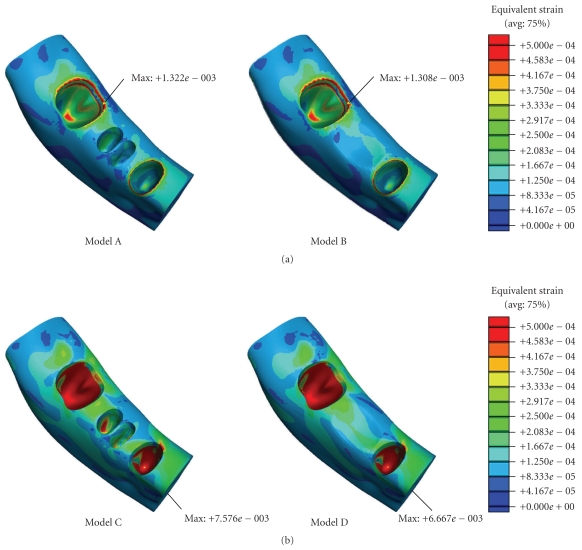
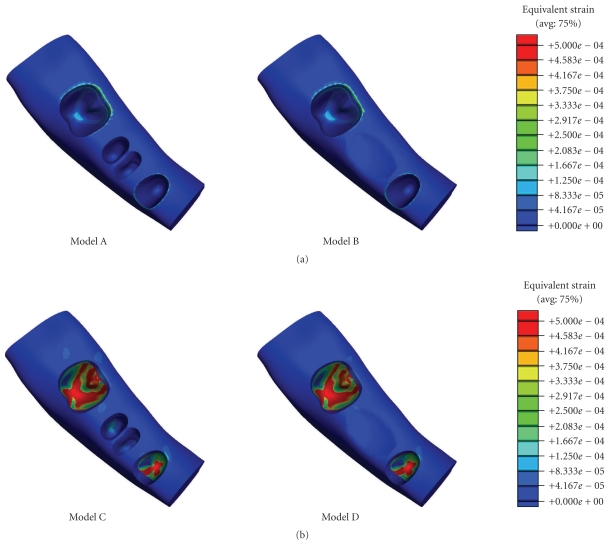
As shown in Figure 2, the peak equivalent strains on the ridged regions of the cortical bone were located in the lingual area in Models A and B (without FPD), showing 0.00132ε and 0.00131ε, respectively. In Models C and D (with FPD), the maximum equivalent strains were situated around the root apex of the second premolar, yielding 0.00785ε and 0.00667ε, respectively. The minimum equivalent strains Models A, B, C, and D are 9.46 × 10−5ε, 1.334 × 10−5ε, 9.48 × 10−5ε, and 2.267 × 10−5ε. It is noted that the equivalent strain in the ridged regions of the cortical bone is of primary interest in determining initiation of bone remodelling. The corresponding average values for the equivalent strain in the mesial sides around the first molar region in Models A, B, C, and D were 0.0002ε, 0.0006ε, 0.0005ε, and 0.0012ε, respectively, while they were 0.0006ε, 0.0008ε, 0.0013ε, and 0.002ε on the distal sides, respectively.
Figure 2.
Equivalent strain contours in mandibular bone (a) prebridgework models and (b) FPD models.
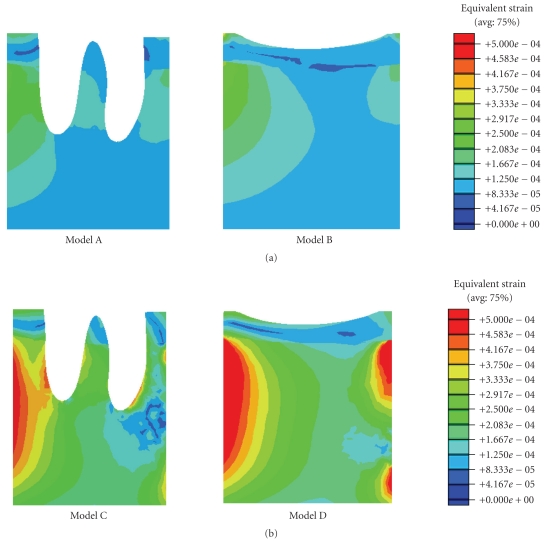
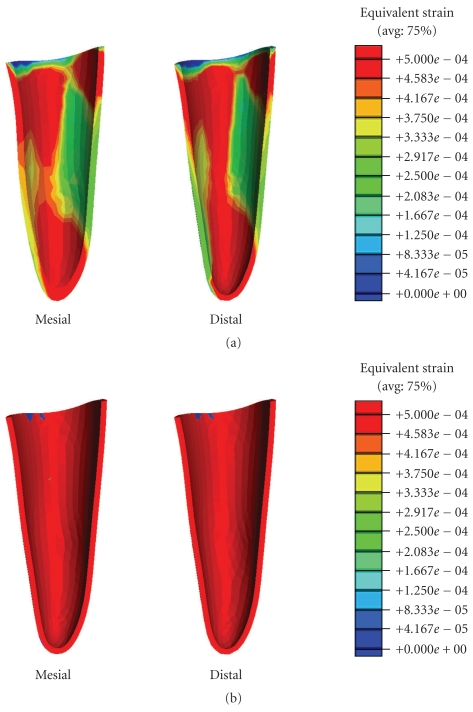
Tooth extraction significantly altered the equivalent strain concentrations around the first molar (Figure 3). The average lingual strains in Models A, B, C, and D were 0.0002ε, 0.0005ε, 0.0002ε, and 0.0004ε, while the average buccal strains were 0.0001ε, 0.0002ε, 0.0002ε, and 0.001ε, respectively.
Figure 3.
Equivalent strain cross-sectional contours about the first molar.
4. Discussion
In order to gain understanding of the consequences of FPD treatment, it is essential to establish a sound knowledge of the physiological characteristics of all the supporting tissues within such an oral environment. A fundamental design criterion for an FPD is to institute compatibility with its surrounding living tissues. The vitality of bone about an FPD is of primary importance as the condition of bone can in turn affect the stability of the FPD considerably [40]. From the clinician's point of view, it is imperative that the selected abutment teeth for the FPD are supported by adequately healthy alveolar bone [41, 42]. However, it has remained unclear how the alteration of local oral condition induced by extraction of natural tooth and construction of FPD could affect the alveolar bone. Therefore there is a need to quantify the mechanical responses of alveolar bone due to construction of FPD. In this study the stress and strain distributions were examined in the pre-FPD and post-FPD cases within the mandible.
Certain levels of mechanical masticatory stimulation is vital in maintaining sufficient underlying bone health [8]. Tooth extraction leads to immediate changes in local bone morphology and loadings, which consequently alter the biomechanical responses in the surrounding bone bed. Frost's mechanostat theory suggests that the minimum effective strain (MES) in the range of 0.0008–0.002 enables the dynamics of bone turnover to reach equilibrium [10].
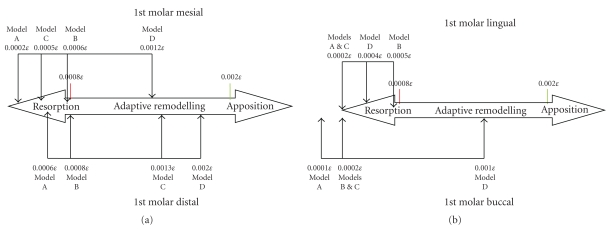
In this study, the equivalent strains in the different scenarios yielded the strains within, above, and below Frost's bone adaptive MES remodelling range. The FE analyses showed that the equivalent strains in the cortical ridge of the first molar in the mesial, distal, and buccal regions in Model D (healed with FPD) were within the equilibrium range (Figures 4 and 5). This is a realistic indication that an FPD treatment could better maintain an appropriate bone remodelling equilibrium, thereby preserving a healthy status of bone.
Figure 4.
(a) Mesial/distal strains and (b) lingual/buccal strains within in the cortical ridge of the 1st molar in all three cases evaluated with Frost's bone mechanostat (not to scale).
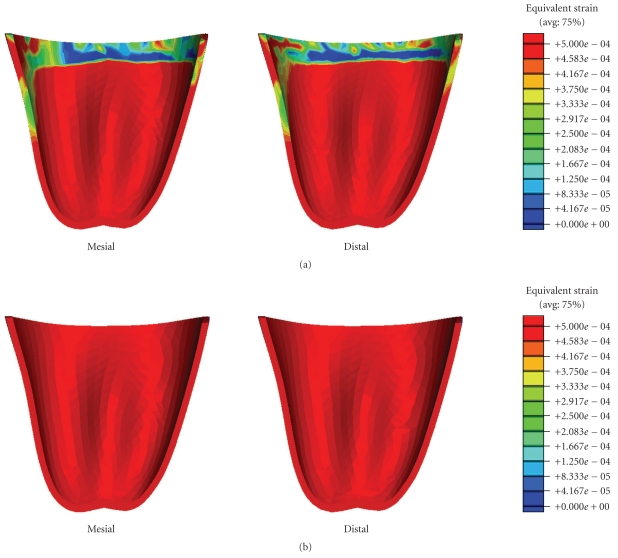
Figure 5.
Equivalent strain contours in mandibular bone (a) prebridgework models and (b) FPD models indicating mandibular bone apposition (red), resorption (blue), and equilibrium (green).
It is also seen that Models C and D incorporating the FPD undergo overall higher equivalent strain than Models A and B (Figure 2). The higher magnitude of equivalent strains is evident and logical as the two abutment teeth are supporting a mastication load suitable for three native teeth. Thus the strains within the abutments will be significantly greater than its prebridgework counterparts as the loading condition has substantially increased. From Figure 2, the cortical strains in the freshly extracted tooth Models A and C are observed to be much lower than their native counterparts [25] due to removal of part of mastication load, suggesting that resorption may occur around the cortical ridge. The resorption is an expected outcome as upon extraction a reduction in ridge height subsequently follows [8]. Figure 5 also displays a considerable increase in strains around the apical third tooth root and root apex of the extracted tooth in Models A and C. This higher strain concentration suggests that it would be a site of bone apposition. This is a probable scenario as clinically upon extraction the process of bone healing involves the formation of bone within the extraction socket. It can also be noted that with the presence of bridgework, the strains within the mandibular bone are noticeably higher due to restoration of normal masticatory function (Figure 2).
Figure 4 relates the equivalent strains to the MES remodelling range suggested by Frost [10], where significant difference can be observed between the counterparts with or without the FPD construction. Model A suggests that resorption may occur in the mesial/distal/lingual/buccal areas of the cortical ridge, but apposition in root apex and about the root surface within the apical third. Model B indicates that resorption may appear in the mesial/lingual/buccal regions, making the buccal-lingual ridge thinner and lower. Model C (FPD) implies resorption in the mesial/lingual/buccal sites and remodelling equilibrium around distal region. Model D appears to perform best in terms of the effective strain level and shows possible occurrence of resorption on the lingual side only.
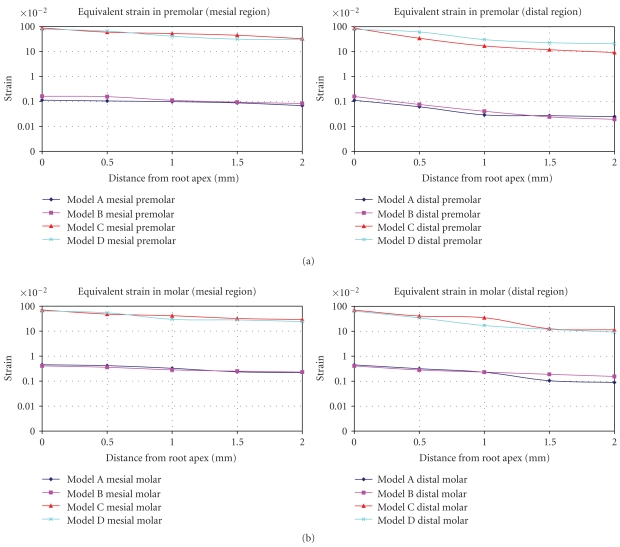
Since PDLs are of special importance to bone remodelling [43], Figures 6 and 7 provide the equivalent strain values observed within the PDLs of the premolar and molar in all the models. It is seen that the regions of bone resorption and apposition can correlate to those strains developed in the PDL. Nevertheless, the equivalent strains within the PDL are higher than those observed within the mandibular bone due to its much lower Young's modulus.
Figure 6.
Equivalent strain contours in the premolar PDL (a) prebridgework models and (b) FPD models.
Figure 7.
Equivalent strain contours in the molar PDL (a) prebridgework models and (b) FPD models.
To better observe the strain distribution in PDL, Figure 8 plots the equivalent strains in the different regions versus the distance from the root apex. It is shown that in all dentitions, the highest equivalent strains are at the root apex. In addition, the equivalent strains in the prebridgework models are considerably lower than those in the FPD-models. This is a realistic outcome as the two abutments are supporting a masticatory load of three dentitions after the FPD treatments. Quantifying the response within the PDL can provide the indicators as to whether the appropriate mechanical signals are indicative to bone remodelling.
Figure 8.
Equivalent strain contours in the PDL (a) premolar and (b) molar.
Furthermore, the anticipation of bone resorption in the extracted Models A and C can be seen as a step in the healing process of extraction as alveolar bone atrophy posttooth extraction is a well-known phenomenon [44, 45]. From Figure 3, it is noted that the FPD treatment results in the fresh extraction site experiencing a considerably higher equivalent strain, thereby somewhat better preserving the ridge height and reducing bone loss. As summarized in Table 3, considerable better apposition volumes (in percentage) can be anticipated in the bridgework Models C and D. Much greater bone volumes, 45.93% and 40.57%, respectively, in the freshly-extracted FPD and healed FPD models, reach the equilibrium of bone turn-over, compared with much higher resorption volumes of 86.20% and 86.97% in the corresponding non-FPD models. This clearly indicates the primary importance of timely FPD treatment, not only for restoring the normal masticatory function but also for maintaining bone quantity and quality.
Table 3.
Percentage bone volume fraction due to mastication.
| Model A | Model B | Model C | Model D | |
|---|---|---|---|---|
| Resorption volume fraction (%)(εe < 0.0008) | 86.20 | 86.97 | 53.62 | 59.14 |
| Equilibrium volume (%) fraction (%)(0.0008 < εe < 0.002) | 13.80 | 13.02 | 45.93 | 40.57 |
| Appositive volume fraction (%)(εe > 0.002) | 0 | 0 | 0.46 | 0.29 |
The present study defines the initial biomechanical responses and possible adaptive changes within surrounding bone with or without construction of FPD. This method can supplement existing experience-based clinical predicative procedures. It is revealed that the application of an FPD leads to a noticeable alteration in normal stress/strain patterns undergone within the alveolar bone. As a consequence, the supporting bone adapts itself to such a changed functional environment. This paper suggested that the response of the bone-FPD interface (PDL and adjoining bone) to functional load is crucial to the long-term success of the prosthetic treatment. This initial status of biomechanics can be associated with specific biological cellular reactions as a consequence of biomechanical stimuli. The results provide supportive evidence that an FPD treatment in a healed extraction site would help maintain a proper equilibrium of bone turnover. Enumerating the adaptive ability of bone to multiple respective loading situations attained by using remodelling processes and bone remodelling algorithms will be our future work.
Acknowledgment
This study was supported by the Australian Research Council Discovery Project.
References
- 1.Yamashita J, Wang Q, Dechow PC. Biomechanical effects of fixed partial denture therapy on strain patterns of the mandible. The Journal of Prosthetic Dentistry. 2006;95(1):55–62. doi: 10.1016/j.prosdent.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Creugers NH, van ’t Hof MA. An analysis of clinical studies on resin-bonded bridges. Journal of Dental Research. 1991;70(2):146–149. doi: 10.1177/00220345910700021001. [DOI] [PubMed] [Google Scholar]
- 3.Kerschbaum T, Haastert B, Marinello CP. Risk of debonding in three-unit resin-bonded fixed partial dentures. The Journal of Prosthetic Dentistry. 1996;75(3):248–253. doi: 10.1016/s0022-3913(96)90480-1. [DOI] [PubMed] [Google Scholar]
- 4.Carter DR. Mechanical loading history and skeletal biology. Journal of Biomechanics. 1987;20(11-12):1095–1109. doi: 10.1016/0021-9290(87)90027-3. [DOI] [PubMed] [Google Scholar]
- 5.Beaupre GS, Orr TE, Carter DR. An approach for time-dependent bone modeling and remodeling—theoretical development. Journal of Orthopaedic Research. 1990;8(5):651–661. doi: 10.1002/jor.1100080506. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs CR. Numerical Simulational of Bone Adaptation to Mechanical Loading. Stanford, Calif, USA: Stanford University; 1994. [Google Scholar]
- 7.Mathews MF, Breeding LC, Dixon DL, Aquilino SA. The effect of connector design on cement retention in an implant and natural tooth-supported fixed partial denture. The Journal of Prosthetic Dentistry. 1991;65(6):822–827. doi: 10.1016/s0022-3913(05)80021-6. [DOI] [PubMed] [Google Scholar]
- 8.Bodic F, Hamel L, Lerouxel E, Baslé MF, Chappard D. Bone loss and teeth. Joint Bone Spine. 2005;72(3):215–221. doi: 10.1016/j.jbspin.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Lin D, Li W, Swain M. Dental implant induced bone remodeling and associated algorithms. Journal of the Mechanical Behavior of Biomedical Materials. 2009;2(5):410–432. doi: 10.1016/j.jmbbm.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Frost HM. A determinant of bone architecture: the minimum effective strain. Clinical Orthopaedics and Related Research. 1983;(175):286–292. [PubMed] [Google Scholar]
- 11.Melsen B, Lang NP. Biological reactions of alveolar bone to orthodontic loading of oral implants. Clinical Oral Implants Research. 2001;12(2):144–152. doi: 10.1034/j.1600-0501.2001.012002144.x. [DOI] [PubMed] [Google Scholar]
- 12.Lin C-L, Chang S-H, Chang W-J, Kuo Y-C. Factorial analysis of variables influencing mechanical characteristics of a single tooth implant placed in the maxilla using finite element analysis and the statistics-based Taguchi method. European Journal of Oral Sciences. 2007;115(5):408–416. doi: 10.1111/j.1600-0722.2007.00473.x. [DOI] [PubMed] [Google Scholar]
- 13.Brehm TW, Abadi BJ. Patient response to variations in complete denture technique—part IV: residual ridge resorption–cast evaluation. The Journal of Prosthetic Dentistry. 1980;44(5):491–494. doi: 10.1016/0022-3913(80)90065-7. [DOI] [PubMed] [Google Scholar]
- 14.Sennerby L, Carlsson GE, Bergman B, Warfvinge J. Mandibular bone resorption in patients treated with tissue-integrated prostheses and in complete-denture wearers. Acta Odontologica Scandinavica. 1988;46(3):135–140. doi: 10.3109/00016358809004759. [DOI] [PubMed] [Google Scholar]
- 15.Oh W, Gotzen N, Anusavice KJ. Influence of connector design on fracture probability of ceramic fixed-partial dentures. Journal of Dental Research. 2002;81(9):623–627. doi: 10.1177/154405910208100909. [DOI] [PubMed] [Google Scholar]
- 16.Taskonak B, Mecholsky JJ, Jr., Anusavice KJ. Fracture surface analysis of clinically failed fixed partial dentures. Journal of Dental Research. 2006;85(3):277–281. doi: 10.1177/154405910608500314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin C-L, Chang S-H, Wang J-C, Chang W-J. Mechanical interactions of an implant/tooth-supported system under different periodontal supports and number of splinted teeth with rigid and non-rigid connections. Journal of Dentistry. 2006;34(9):682–691. doi: 10.1016/j.jdent.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Magne P, Perakis N, Belser UC, Krejci I. Stress distribution of inlay-anchored adhesive fixed partial dentures: a finite element analysis of the influence of restorative materials and abutment preparation design. The Journal of Prosthetic Dentistry. 2002;87(5):516–528. doi: 10.1067/mpr.2002.124367. [DOI] [PubMed] [Google Scholar]
- 19.Misch CM, Ismail YH. Finite element stress analysis of tooth-to-implant fixed partial denture designs. Journal of Prosthodontics. 1993;2(2):83–92. doi: 10.1111/j.1532-849x.1993.tb00388.x. [DOI] [PubMed] [Google Scholar]
- 20.Glantz PJ, Nilner K, Jendresen MD, Sundberg H. Quality of fixed prosthodontics after twenty-two years. Acta Odontologica Scandinavica. 2002;60(4):213–218. doi: 10.1080/000163502760147972. [DOI] [PubMed] [Google Scholar]
- 21.Kern M, Douglas WH, Fechtig T, Strub JR, DeLong R. Fracture strength of all-porcelain, resinbonded bridges after testing in an artificial oral environment. Journal of Dentistry. 1993;21(2):117–121. doi: 10.1016/0300-5712(93)90160-r. [DOI] [PubMed] [Google Scholar]
- 22.Koutayas SO, Kern M, Ferraresso F, Strub JR. Influence of design and mode of loading on the fracture strength of all-ceramic resin-bonded fixed partial dentures: an in vitro study in a dual-axis chewing simulator. The Journal of Prosthetic Dentistry. 2000;83(5):540–547. doi: 10.1016/s0022-3913(00)70012-6. [DOI] [PubMed] [Google Scholar]
- 23.Ichim I, Swain M, Kieser JA. Mandibular biomechanics and development of the human chin. Journal of Dental Research. 2006;85(7):638–642. doi: 10.1177/154405910608500711. [DOI] [PubMed] [Google Scholar]
- 24.Li W, Swain MV, Li Q, Steven GP. Towards automated 3D finite modeling of direct fiber reinforced composite dental bridge. Journal of Biomedical Materials Research Part B. 2005;74(1):520–528. doi: 10.1002/jbm.b.30233. [DOI] [PubMed] [Google Scholar]
- 25.Field C, Li Q, Li W, Swain M. Influence of tooth removal on mandibular bone response to mastication. Archives of Oral Biology. 2008;53(12):1129–1137. doi: 10.1016/j.archoralbio.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 26.Johnson K. A study of the dimensional changes occurring in the maxilla following tooth extraction. Australian Dental Journal. 1969;14(4):241–244. doi: 10.1111/j.1834-7819.1969.tb06001.x. [DOI] [PubMed] [Google Scholar]
- 27.Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. International Journal of Periodontics & Restorative Dentistry. 2003;23(4):313–323. [PubMed] [Google Scholar]
- 28.Vaillancourt H, Pilliar RM, McCammond D. Finite element analysis of crestal bone loss around porous-coated dental implants. Journal of Applied Biomaterials. 1995;6(4):267–282. doi: 10.1002/jab.770060408. [DOI] [PubMed] [Google Scholar]
- 29.Schwarz MS. Mechanical complications of dental implants. Clinical Oral Implants Research. 2000;11(supplement 1):156–158. doi: 10.1034/j.1600-0501.2000.011s1156.x. [DOI] [PubMed] [Google Scholar]
- 30.Howell A, Brudevold F. Vertical Forces used during chewing of food. Journal of Dental Research. 1950;29(2):133–136. doi: 10.1177/00220345500290020401. [DOI] [PubMed] [Google Scholar]
- 31.Okesson J. Management of Temporomandibular Disorders and Occlusion. 4th edition. St Louis, Mo, USA: Mosby; 1998. [Google Scholar]
- 32.Zheng J, Zhou ZR. Effect of age on the friction and wear behaviors of human teeth. Tribology International. 2006;39(3):266–273. [Google Scholar]
- 33.Dalkiz M, Zor M, Aykul H, Toparli M, Aksoy S. The three-dimensional finite element analysis of fixed bridge restoration supported by the combination of teeth and osseointegrated implants. Implant Dentistry. 2002;11(3):293–300. doi: 10.1097/00008505-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Eraslan O, Sevimay M, Usumez A, Eskitascioglu G. Effects of cantilever design and material on stress distribution in fixed partial dentures: a finite element analysis. Journal of Oral Rehabilitation. 2005;32(4):273–278. doi: 10.1111/j.1365-2842.2004.01429.x. [DOI] [PubMed] [Google Scholar]
- 35.Pini M, Wiskott HWA, Scherrer SS, Botsis J, Belser UC. Mechanical characterization of bovine periodontal ligament. Journal of Periodontal Research. 2002;37(4):237–244. doi: 10.1034/j.1600-0765.2002.00344.x. [DOI] [PubMed] [Google Scholar]
- 36.Daegling DJ, Hylander WL. Biomechanics of torsion in the human mandible. American Journal of Physical Anthropology. 1998;105(1):73–87. doi: 10.1002/(SICI)1096-8644(199801)105:1<73::AID-AJPA7>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 37.Lekholm U, Zarb G. Patient selection and preparation. In: Branemark PI, Zarb G, Albrektsson T, editors. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago, Ill, USA: Quintessence; 1985. pp. 199–209. [Google Scholar]
- 38.Mellal A, Wiskott HWA, Botsis J, Scherrer SS, Belser UC. Stimulating effect of implant loading on surrounding bone. Comparison of three numerical models and validation by in vivo data. Clinical Oral Implants Research. 2004;15(2):239–248. doi: 10.1111/j.1600-0501.2004.01000.x. [DOI] [PubMed] [Google Scholar]
- 39.Frost HM. Bone’s mechanostat: a 2003 update. The Anatomical Record Part A. 2003;275(2):1081–1101. doi: 10.1002/ar.a.10119. [DOI] [PubMed] [Google Scholar]
- 40.Olsson M, Gunne J, Astrand P, Borg K. Bridges supported by free-standing implants versus bridges supported by tooth and implant: a five-year prospective study. Clinical Oral Implants Research. 1995;6(2):114–121. doi: 10.1034/j.1600-0501.1995.060207.x. [DOI] [PubMed] [Google Scholar]
- 41.Himmel R, Pilo R, Assif D, Aviv I. The cantilever fixed partial denture—a literature review. The Journal of Prosthetic Dentistry. 1992;67(4):484–487. doi: 10.1016/0022-3913(92)90077-n. [DOI] [PubMed] [Google Scholar]
- 42.Yang H-S, Chung H-J, Park Y-J. Stress analysis of a cantilevered fixed partial denture with normal and reduced bone support. The Journal of Prosthetic Dentistry. 1996;76(4):424–430. doi: 10.1016/s0022-3913(96)90549-1. [DOI] [PubMed] [Google Scholar]
- 43.Lee Y-H, Nahm D-S, Jung Y-K, et al. Differential gene expression of periodontal ligament cells after loading of static compressive force. Journal of Periodontology. 2007;78(3):446–452. doi: 10.1902/jop.2007.060240. [DOI] [PubMed] [Google Scholar]
- 44.Atwood DA. Reduction of residual ridges: a major oral disease entity. The Journal of Prosthetic Dentistry. 1971;26(3):266–279. doi: 10.1016/0022-3913(71)90069-2. [DOI] [PubMed] [Google Scholar]
- 45.Atwood DA, Coy WA. Clinical, cephalometric, and densitometric study of reduction of residual ridges. The Journal of Prosthetic Dentistry. 1971;26(3):280–295. doi: 10.1016/0022-3913(71)90070-9. [DOI] [PubMed] [Google Scholar]