Abstract
Gene expression profiling (GEP) of 8 stage 0/I untreated Chronic Lymphocytic Leukemia (CLL) patients showed over-expression of Frizzled 3 (FZD3)/ROR-1 receptor tyrosine kinase (RTK), FLT-3 RTK and CXCR3 G-protein coupled receptor (GPCR). RT-PCR of 24 genes in 21 patients of the WNT pathway corroborated the GEP. Transforming growth factorβ, fibromodulin, TGFβRIII and SMAD2 are also over-expressed by GEP. Serum cytokine profiling of 26 low stage patients showed elevation of IFNγ, CSF3, Flt-3L and insulin-like growth factor binding protein 4. In order to ascertain why CLL cells grow poorly in culture, a GEP of 4 CLL patients cells at 0 hr and 24 hr in culture demonstrated over expression of CXCL5, CCL2 and CXCL3, that may recruit immune cells for survival. Treatment with thalidomide, an immunomodulatory agent, showed elevation of CCL5 by GEP but was not cytotoxic to CLL cells. Our data suggest an interplay of several oncogenic pathways, cytokines and immune cells that promote a survival program in CLL.
1. Introduction
B-cell chronic lymphocytic leukemia (CLL) is the most common adult leukemia in the Western world. CLL cells express 1 or more B cell associated antigens, generally CD19, CD20 and CD23 with coexpression of CD5, a T cell marker [1, 2]. Fluorescent in Situ Hybridization (FISH) for specific karyotypic markers [3] and polymerase chain reaction (PCR) for immunoglobulin heavy chain variable region (IgVH) gene mutations [4, 5] provide prognostic information. An association between IgVH gene mutation and CD38 expression has been observed [6]. Increased CD38 expression has been correlated with the unmutated state [6]. The 70 kDa zeta-associated protein (ZAP-70) a cytoplasmic tyrosine kinase measured by flow cytometry [7, 8] or by RT-PCR and immunohistochemistry (IHC) [9], appears to improve the prognostic significance of cytogenetics and IgVH mutational status. CLL patients who are ZAP-70 positive irrespective of their clinical stage, cytogenetics and IgVH mutational status have a shorter progression free survival [10].
Several groups have performed gene expression profiling (GEP) on CLL [11–16] to establish a gene expression signature, prognostic groups, cell of origin, correlation with genomic defects and diagnostic markers. These studies provide evidence that the CLL GEP is related to memory B-cells. Further, there appears to be a correlation between GEP and genomic loss or gain suggesting that gene dosage may be important to CLL pathogenesis [11, 17]. More recently microRNA (miRNA) expression profiles have been utilized to distinguish normal B-cells from CLL cells and provide a signature that is associated with prognosis and progression [18]. The WNT/FZD canonical pathway has been proposed as a possible mechanism of oncogenesis in CLL [19–21]. ROR-2, a close member of ROR-1, has been shown to bind Wnt-5A via the cysteine rich domain (CRD) and to activate the JNK signaling pathway [22].
Current treatments cannot cure CLL and more effective therapies based on abrogating key oncogenic signaling pathways are needed. Here, we pose several key objectives and goals to address this statement by utilizing gene expression and cytokine profiling of Rai stage 0/I CLL patients which include, (A) What are the differentially expressed genes in CLL? Previous studies used a microarray platform containing fewer genes, and therefore the current study with >10,000 novel genes would likely yield novel differentially expressed genes, (B) What oncogenic signaling pathway(s) are likely to drive CLL progression?, as they may help identify parallel cross-talking pathways, (C) What serum cytokines are associated with immune evasion and survival?, that may activate CLL and/or stromal cells , (D) What are the six hallmarks of cancer for CLL and can they be targeted rationally?, (E) What is the status of p53 and ZAP-70 in low stage CLL?, since both are associated with a poor prognosis, (F) Does GE change when CLL cells are cultured for a given time? This would address the important question of why it is difficult to grow CLL cells in culture and help identify differentially expressed genes after treatment with drugs (e.g., thalidomide, an immunomodulatory agent). Based on GEP studies we identified over-expression of members of the non-canonical WNT/PCP-ROR-1 signaling pathway genes that were validated by RT-PCR. Two other pathways (CXCL9/CXCR3 and Flt3L-Flt-3 RTK) were identified where both ligand serum levels and cognate receptors, on CLL cells, were elevated. We show that the majority of the patients differentially over-expressed ZAP-70 while p53 was down regulated. The GEP of CLL cells at 0 hours and 24 hours in culture showed differential over-expression of the cytokine CXCL5. Treatment of CLL cells with thalidomide, a potent anti-angiogenic and immunomodulatory drug, had no effect on cell viability but led to the over-expression of cytokine CCL5. Together, these results provide novel biological insights and potential therapeutic targets for low-stage CLL patients.
2. Materials and Methods
2.1. Reagents
Isolated and purified CLL cells from patients were cultured in 10% human serum albumin (Gemini BioProducts, Woodland, CA) in RPMI-1640 media. Polyclonal antibodies to FZD3 (R&D Systems, MN), ROR-1 (R&D Systems, MN) and Flt-3 (Santa Cruz, CA) were obtained. Secondary antibody at a 1 : 5000 dilution (IRDye™ 800 donkey anti-rabbit, Rockland Immunochemicals) was used to visualize bands with a LI-COR Odyssey Infrared Imaging System. Thalidomide powder (Sigma) was freshly dissolved in dimethyl sulphoxide (DMSO) at a 5mM stock solution and diluted into RPMI-1640 media with 10% human serum immediately prior to use. CD19+ normal PB B-cell RNA from 4 normal volunteers was purchased from AllCells, CA.
2.2. Patient Samples and Preparation
All patients studied had a diagnosis of CLL stage 0 or I. Patient blood samples (N = 26) were collected after obtaining informed consent on an Institutional Review Board approved protocol. Whole blood was collected for cells and serum. Mononuclear cells were separated and either stored frozen at −80°C or maintained in RPMI-1640 medium with 10% human serum (Gemini BioProducts, CA) at 37°C in 5% CO2. Separated serum was stored in 0.5 mL aliquots at −80°C until further studies were performed. Mononuclear cells were separated from peripheral blood samples by Ficoll-Hypaque density centrifugation [12] and phenotype was determined by immunofluorescent flow cytometry analysis [13]. The CLL cells were then maintained in culture in RPMI-1640 at 37°C for further studies.
2.3. RNA Isolation and Affymetrix Microarrays
Total RNA was extracted using the RNeasy Mini Kit (Qiagen, CA) from 8 patient CLL cells at collection. Further, RNA was extracted from 4 patient CLL cells in culture for 24 hours and after treatment with thalidomide (1 μM) for 24 hours. The amount of total RNA isolated from the cells was quantified using spectrophotometric OD260 measurements with yields≥25 μg/sample. Control RNA was obtained from normal peripheral (PB) B-cells from 4 volunteers (AllCells, CA). 5 μg of mRNA was used to generate first-strand cDNA by using a T7-linked oligo(dT) primer. After second-strand synthesis, in vitro transcription (Ambion) was performed with biotinylated UTP and CTP (Enzo Diagnostics), resulting in 40- to 80-fold linear amplification of RNA. 40 μg of biotinylated RNA was fragmented to 50- to 150-nt size before overnight hybridization at 45°C to HG-U133A 2.0 Affymetrix array comprising ~18,400 transcripts and 22,000 probe sets (Santa Clara, CA). After washing, arrays were stained with streptavidin—phycoerythrin (Molecular Probes) and scanned on a Hewlett-Packard scanner. Intensity for each feature of the array was captured by using GENECHIP SOFTWARE (Affymetrix, CA), and a single raw expression level for each gene was derived from the 10-20 probe pairs representing each gene by using a trimmed mean algorithm. Intensity values were scaled such that overall intensity for each chip of the same type was equivalent. After hybridization, the quality of the data was tested with several methods. The arrays were first inspected visually for artifacts and B2 Oligo performance per manufacturer's instructions (Affymetrix, Inc. “Gene Chip© Expression Analysis Technical Manual”, November 2004). Chip CEL files were then imported into R-BioConductor (v. 1.7) (http://genomebiology.com/2004/5/10/R80). MAS5 Present/Absent calls were generated with the simpleaffy (http://bioinformatics.picr.man.ac.uk/simpleaffy/) package using a target scaling factor of 100. The scale factors were within 3-fold of each other as recommended in the guidelines provided in the Affymetrix Gene Chip© Expression Analysis: Data Analysis Fundamentals manual. The quality control metrics were generated using the “qc” function provided in the simpleaffy package. All chips performed as follows: the average backgrounds fell between 20 and 100, hybridization controls (bioB, bioC, bioD and cre) were all called present with increasing signal intensities and the 3′/5′ ratios for the internal controls (GAPDH and β-actin) were less than 1.25 and 3 respectively. Further quality control was performed using the affy PLM package provided in the BioConductor suite. The microarray data were normalized by robust multi-chip analysis (RMA) using the “fitPLM” function (default values). Chip pseudo-images of the weights and residuals, normalized unscaled standard error (NUSE) and relative log expression (RLE) values were used for chip-level quality assessment. Chip pseudo-images displayed no apparent artifacts that warranted excluding a chip from further analysis. NUSE and RLE plotting revealed the chips used in the experiments to be consistent. Next, chips were normalized by RMA using the simpleaffy package. Log-fold changes were calculated from the normalized log2 expression values.
2.4. Gene Expression Data Analysis and Visualization
For each CLL sample at collection, in culture for 24 hours or treated with thalidomide for 24 hours a comparison to the control samples (normal B-cells) and lists of ‘robust increasers' or ‘robust decreasers' was generated utilizing the Affymetrix Data Analysis Program (Affymetrix MAS 5.0). Fundamentals' guide was used to import these lists into GeneSpring (version 5.0) and obtain the intersection of robust increasers or decreasers across all patients. Increasers or decreasers common to CLL patients were compared to normal PB B-cells. In order to assess quality and reproducibility of our data, we leveraged published independent global GEP studies of CLL for robust increasers and decreasers. GEP for each patient was further classified according to the hallmarks of cancer [23], to determine CLL specific ‘tumor profile signatures'. Intersection of the gene lists for each target with the commonly up-regulated and down-regulated genes across patient samples was obtained. This was also performed on the intersects of the up- and down-regulated gene lists with the GeneSpring “Simplified GO Ontology” as another method of classifying genes.
2.5. Real Time Quantitative RT-PCR
One hundred nanograms of total RNA were used for reverse transcriptase (RT) reactions (20 ml total volume) carried out using SuperScript™ III Platinum® Reverse Transcriptase (Invitrogen, Carlsbad, CA). Reactions were incubated at 42°C for 50 minutes followed by incubation at 37°C with RNase H for 20 minutes. An Opticon DNA Engine (MJ Research, Reno, NV) was used to perform real-time fluorescence detection PCR. 1 μl cDNA was added to 12.5 μl of Platinum® SYBR® Green qPCR SuperMix-UDG (Invitrogen, Carlsbad, CA), 1 μl of gene-specific or β-actin specific primer pair (see primer design), and 10.5 μl of dH2O (final volume of 25 μl). Amplification (95°C for 15 s, 55°C for 30 s, and 72°C for 30 s) was repeated for 44 cycles. Threshold cycle value (Ct) for each sample indicated the cycle at which a statistically significant increase in fluorescence was first detected. These data were then normalized to β-actin, which served as an unaffected control gene, for each data point and compared to a normal B-cell control to determine relative expression ratios. Each measurement was performed in triplicate.
2.6. Primer Design
PCR primers were designed using MacVector® (Accelrys, San Diego, CA) to produce amplicons with lengths ranging from 80-250 bp to optimize the efficiency of qPCR. β-actin primers from QuantumRNA™β-Actin Internal Standards (Ambion, Austin, TX) were used to normalize the qPCR data. The following genes were analyzed by real time quantitative RT-PCR: AXIN1, BLK, CSN1A1, CTNNB1, DVL1, FRAT1, FZD3, FZD6, FLT-3, GSK3 β, ITK, JAK2, JUN, LEF-1, MAPK10, MAPK8, MAPK9, PRKCB1, ROR-1, ROR-2, SYK, TCF4, P53, WNT-3A, WNT-5A and ZAP70.
2.7. Serum Cytokine Profiling
Stored (−80°C) or fresh patient serum samples were utilized (N = 26 patients). Array slides were thawed at room temperature as serum was diluted 3.5-fold with 1x blocking buffer (Cytokine Array Protocol, RayBiotech, Inc #AAH-CYT-G1000). Slides were blocked with blocking buffer and 50 μL of each sample was hybridized with the slide for 2 hours; 1 μL internal controls were also added. After washing, provided biotin-conjugated anti-cytokine antibodies were diluted with 300 μL of blocking buffer, added to the slide, and incubated for 2 hours at room temperature. Washing steps were repeated, followed by addition of a 1:1500 dilution of Alexa Flour 555-conjugated streptavidin and incubated overnight at 4°C. Slides were washed multiple times and read on the Axon GenePix using the cy3 channel. Analysis was conducted using the RayBiotech analysis tool.
2.8. Immunoprecipitation and Immunoblotting
CLL cells were lysed with 1% Nonidet P-40 lysis buffer. 500 μg clarified lysate per sample was incubated at 4°C overnight with anti-ROR-1 polyclonal antibodies followed by the addition of protein A agarose (Upstate Biotechnology) for a further 2 hours. After PAGE and transfer to Immobilon membranes (Millipore, MA), immunoblotting was performed using the anti-ROR-1 antibody. Alternatively, 50–100 μg of protein from cell extracts was separated by PAGE and immunoblotted with protein-specific antibodies. Protein bands were visualized utilizing the secondary antibody at a 1:5000 dilution (IRDye™ 800 donkey anti-rabbit, Rockland Immunochemicals) with a LI-COR Odyssey Infrared Imaging System.
3. Results
3.1. Gene Expression Profile of Stage 0/I CLL
The purity of the CLL samples estimated from the percentage of CD19 cells was at a mean of 89% (range 80–95%) (Supplementary Figure 1) which is very similar to that described by Stratowa et al. [13]. A GEP was conducted on 8 low stage CLL patients, 4 normal volunteers without age-matched CD19+ B-cells (AllCells, CA) utilizing the Affymetrix platform (22,000 genes) with >10,000 genes than previously published GEP studies. We compared the most significantly over-expressed and down-regulated genes of CLL versus normal B-cells in our GEP to that of Klein et al. 2001 [12] (U95A Affymetrix microarray) and Jelinek et al. 2003 [17] (U95Av2 Affymetrix microarray). Ten distinct genes represented by 15 probe sets were differentially expressed in all three studies (Table 1). Moreover, 46 [12] and 55 genes [17] also matched our data set. Hence, our data validate and add to the current knowledge on CLL GEP studies. An analysis of differentially expressed genes by fold change between CLL versus normal PB B-cells was performed in a gene-by-gene analysis for differences between the 2 groups. Genes that are “robustly” highly over-expressed or down regulated that are common to all 8 CLL patients were compared to normal PB B-cells. For brevity only the 20 top over-expressed (Table 2(a)) or down regulated (Table 2(b)) genes are shown. Of the over-expressed genes (Table 2(a)), 5 are listed in Table 1 (ABCA6, fibromodulin, LEF-1, IGFBP4, RASGRF1) confirming the data from Klein et al., 2001[12] and Jelinek et al., 2003 [17]. Novel over-expressed genes from this study are HBA, HBB, PDGF-DD, ROR-1, FRY, SELP, HLA-DQA1 and VIPR1 all of which are implicated in human malignancies including leukemia, lymphoma and solid tumors. It appears that the comparison of CLL patients to normal PB B-cells demonstrates that several of the differentially genes are represented within the 6 hallmarks of cancer [23]. For CLL they are tumor invasion (COL9A2, RAPGEF3, SPOCK2, WNT3, CORO1B, CCL5, IL2RB, MAP2K6), anti-apoptosis and survival (LEF1, IGFBP4, ROR-1, MYBL1, PIM-1, LCK, FLT-3), cell cycle deregulation (PFTK1, PLK3) and angiogenesis (PDGF-DD, FGF2). Consistent with CLL several of the Ig gene family members (light chain variable and heavy chain constant) are the most highly down regulated. Other highly down regulated genes of significance to tumor biology include CCR6, BCL7A, MYC, MAFB, CASP2 and HSP70B.
Table 1.
The most significantly over-expressed and down regulated genes representative in CLL versus normal PB B-cells in our GEP (HG-U133A Affymetrix array) compared to that of Klein et al. (12; U95A Affymetrix array) and Jelinek et al. (15; U95Av2 Affymetrix array). The 10 distinct genes represented by 15 probe sets differentially expressed in all three CLL GEP studies with fold change.
| Gene | Name | Fold Change |
|---|---|---|
| ABCA6 | ATP-binding cassette, subfamily A(ABC1), member 6 | 151 |
| COL9A3 | Collagen, type IX, alpha 3 | 9 |
| FMOD | Fibromodulin | 142 |
| IGFBP4 | Insulin-like growth factor binding protein 4 | 63 |
| LEF1 | Lymphoid enhancer-binding factor 1 | 92 |
| RASGRF1 | Ras protein-specific guanine nucleotide-releasing factor 1 | 25 |
| TGFbR3 | Transforming growth factor, beta receptor III (beta glycan, 300kDa) | 3 |
| MYC | v-Myc myelocytomatosis viral oncogene homolog (avian) | −12 |
| SORL1 | Sortilin-related receptor, L(DLR class) A repeats- containing | −8 |
| TKT | Transketolase (Wernicke-Korsakoff Syndrome) | −3 |
Table 2.
(A). The top 20 over-expressed genes; (B). The top 20 down regulated genes.
| ID | Symbol | Name | Fold Change |
|---|---|---|---|
| A 217232_x_at | HBB | hemoglobin, beta | 188.0 |
| 217414_x_at | HBA2 | hemoglobin, alpha 2 | 178.6 |
| 214414_x_at | HBA1 | hemoglobin, alpha 1 | 163.3 |
| 217504_at | ABCA6 | ATP-binding cassette, sub-family A (ABC1), member 6 | 150.6 |
| 202709_at | FMOD | fibromodulin | 142.4 |
| 221558_s_at | LEF1 | lymphoid enhancer-binding factor 1 | 92.1 |
| 221078_s_at | KIAA1212 | KIAA1212 | 76.4 |
| 204135_at | DOC1 | NA | 70.1 |
| 201508_at | IGFBP4 | insulin-like growth factor binding protein 4 | 63.4 |
| 222154_s_at | DNAPTP6 | NA | 47.1 |
| 205414_s_at | KIAA0672 | NA | 45.4 |
| 219304_s_at | PDGFD | platelet derived growth factor D | 36.2 |
| 205805_s_at | ROR1 | receptor tyrosine kinase-like orphan receptor 1 | 34.8 |
| 219387_at | KIAA1212 | KIAA1212 | 34.8 |
| 204072_s_at | FRY | furry homolog (Drosophila) | 34.0 |
| 206049_at | SELP | selectin P (granule membrane protein 140kDa, antigen CD62) | 33.7 |
| 213831_at | HLA-DQA1 | major histocompatibility complex, class II, DQ alpha 1 | 33.4 |
| 205019_s_at | VIPR1 | vasoactive intestinal peptide receptor 1 | 32.3 |
| 210550_s_at | RASGRF1 | Ras protein-specific guanine nucleotide-releasing factor 1 | 24.7 |
| B 221530_s_at | BHLHB3 | basic helix-loop-helix domain containing, class B, 3 | −52.6 |
| 211635_x_at | IGHV1-69 | immunoglobulin heavy variable 1-69 | −52.9 |
| 219049_at | ChGn | NA | −60.2 |
| 211639_x_at | NA | NA | −68.3 |
| 211798_x_at | IGLJ3 | Immunoglobulin lambda joining 3 | −74.2 |
| 214973_x_at | IGHD | Immunoglobulin heavy constant delta | −90.9 |
| 211637_x_at | NA | NA | −93.7 |
| 203038_at | PTPRK | Protein tyrosine phosphate, receptor type, K | −93.9 |
| 211645_x_at | NA | NA | −97.7 |
| 200606_at | DSP | Desmoplakin | −98.9 |
| 217227_x_at | NA | NA | −109.0 |
| 211644_x_at | IGKC | Immunoglobulin kappa constant | −119.3 |
| 211650_x_at | NA | NA | −126.9 |
| 216491_x_at | IGHM | Immunoglobulin heavy constant mu | −133.0 |
| 210432_s_at | SCN3A | Sodium channel, voltage-gated, type III, alpha | −153.6 |
| 214777_at | NA | NA | −192.3 |
| 216984_x_at | IGLC2 | Immunoglobulin lambda constant 2(kem-Oz-marker) | −194.3 |
| 214768_x_at | IGKV1-5 | Immunoglobulin kappa variable 1-5 | −247.1 |
| 216510_x_at | IGHA1 | Immunoglobulin heavy constant alpha 1 | −288.4 |
| 217148_x_at | IGLV3-25 | Immunoglobulin lambda variable 3-25 | −433.5 |
3.2. Serum Cytokine Profile (SCP) of CLL Patients
Serum samples from 26 CLL patients and 4 normal volunteers were analyzed utilizing the cytokine array G-1000 platform consisting of 120 cytokines/chemokines/growth factors (RayBio, GA). Fold change was calculated for each patient, corrected for absolute lymphocyte count and a mean ± SD obtained for each cytokine for all patients. The mean fold change of ≥6-fold are shown in Table 3(a). Our cytokine profile identified all of the published elevated cytokines associated with CLL cell survival (IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, TNF〈, IFNγ or 〈, G-CSF or GM-CSF) or inhibition (IL-5, TGFβ) [24]. In our cytokine profile the 1st ranked is IFNγ (14.46 fold) which is well known to prevent apoptosis of CLL cells. The 2nd ranked is IGFBP-4 (14.22 fold) and of significance is that it is also over-expressed in the GEP indicating that serum levels reflect CLL production of this cytokine. The function(s) IGFBP-4 are not well characterized except for binding IGF-I and IGF-II. In most human malignancies IGFBP-4 is expressed at levels which appear to correlate with their state of differentiation [25]. The 3rd ranked is G-CSF (10.89 fold) which is known to decreases CLL cell apoptosis. The 4th ranked is IL-3 (8.45 fold) which provides a proliferative signal to CLL cells especially during the lymphoblastoid phase [26]. Other significantly increased serum cytokines are Flt-3 ligand (7.82 fold), SCF (6.76 fold) and SDF-1 (6.54 fold).
Table 3.
Serum cytokine profile of 26 CLL patients with ≥6-fold change compared to 4 normal volunteers and SCF identified several ligand-receptor (L-R) pairs of the chemokine, cytokine, and growth factor receptor pathways. In parenthesis are the fold changes for each of the L-R pairs and known function(s) of the pathway.
(a)
| Cytokine | Fold Change | Function(s) |
|---|---|---|
| IFNg | 14.463 | Antiviral; activates macrophages |
| IGFBP-4 | 14.217 | Alters IGF interaction with receptors |
| G-CSF | 10.894 | Control white cell population |
| IL-3 | 8.446 | Growth & differentiation; histamine release |
| PIG-F | 8.361 | GPI-anchor biosynthesis |
| TNFb | 8.074 | Phagocytosis and cell death |
| IL-6 | 8.052 | B-cell differentiation |
| IGF-I | 7.543 | Regulates somatic growth and proliferation |
| IL-13 | 7.509 | Inhibits inflammatory cytokine production |
| MCP-1 | 7.220 | Monocyte recruitment and attraction |
| Flt-3L | 7.021 | Stimulates hematopoietic cell production |
| SCF | 6.764 | Stimulates mast cell production |
| SDF-1 | 6.538 | Chemoattractant for monocytes & T-cells |
| FGF-6 | 6.484 | Stimulates mitogenesis and angiogenesis |
| BMP-6 | 6.206 | Induces bone & cartilage formation |
(b)
| Ligand (Fold D) | Receptor (Fold D) | Function(s) |
|---|---|---|
| CXCL9 (5-fold) | CXCR3 (2.5-fold) | Chemotaxis (24) |
| WNT-3 (8-fold) | FDZ3 (3-fold) | Cell Survival (18) |
| WNT-16 (2-fold) | ROR-1 (35-fold) | |
| Flt-3L (7-fold) | FLT-3 (7-fold) | Cell Survival & Proliferation |
| IL-2 (5.3-fold) | IL-2RA (3.3-fold) | Proliferation (48) |
| IL-15 (5.4-fold) | IL-2RB (6-fold) | |
| IL-7 (4.6-fold) | IL-7R (6.7-fold) | Immunological Dysregulation (49) |
| IL-10 (6-fold) | IL-10RA (2.7-fold) | Growth Factor (50) |
| TNF (8-fold) | SF1A (3-fold) | Apoptosis & NF-kappa-B |
| LTA (4.6-fold) | signaling |
3.3. Identification of a G-Protein Coupled Receptor and Receptor Tyrosine Kinase Pathways in CLL
Utilizing both the GEP and SCP, an analysis of ligand-receptor (L-R) pairs of the cytokine-cytokine receptor or growth factor-growth factor receptor (PDGF, TNF, TGFβ, WNT) that are simultaneously elevated in our cohort of CLL patients were analyzed utilizing the KEGG database (http://www.genome.jp/kegg/). Several L-R pairs were identified as significantly over-expressed. Table 3B highlights several of these L-R pairs with their respective fold changes and known function(s). We identified 3 major oncogenic signaling pathways: GPCR CXCL9/CXCR3 pathway; and the RTK pathways of WNT/FDZ3-ROR-1 PCP and Flt-3L/FLT-3. Previously, it has been shown that CXCR3 is expressed on CLL cells [27] and may play a role in chemotaxis. Moreover, the CXCR3 ligand, CXCL9, is coexpressed in CLL cells [28] implicating an autocrine mechanism of activation. Our data confirm these individual observations, extend the finding that low stage CLL patients express both CXCL9 and CXCR3 that may promote immune mediated cell homing in addition to chemotaxis.
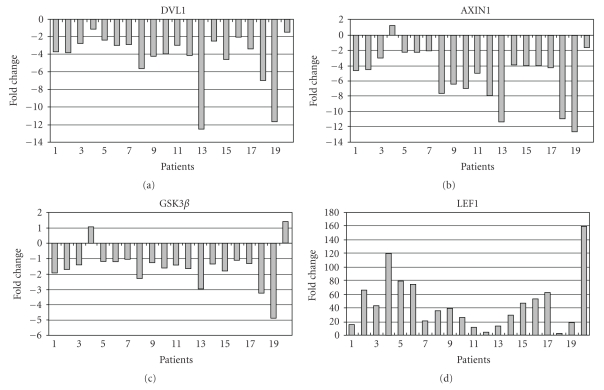
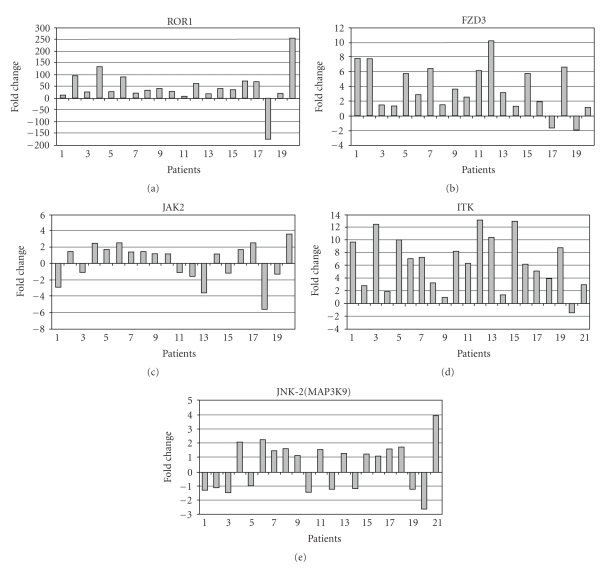
The expression and activation of the classical WNT/FZD signaling cascade has been implicated in CLL. Lu et al., 2004 [19], quantified the GEP of the WNT family and their cognate FZD receptors in CLL cells, and determined the role of WNT signaling in promoting CLL cell survival. Our GEP identified ROR-1 RTK to be over-expressed, which is a member of the non-canonical WNT/PCP pathway. The coreceptor of ROR-1, FZD3 and FZD6 are also over-expressed implicating the activation of the WNT non-canonical pathway in CLL (Table 3(b)). Hence, we analyzed 20 representative members of the canonical and non-canonical pathway from the cell membrane to the nucleus by quantitative real time RT-PCR to ascertain which pathway was active in CLL. The members of the canonical pathway are down regulated (DVL1, AXIN, GSK-3β, TCF-1) except for LEF-1 (Figure 1), while members of the non-canonical pathway are over-expressed (ROR-1, FZD3, JAK2, JNK2, ITK) (Figure 2). GEP identified over-expression of several members of the non-canonical pathway: WNT3 (8-fold), WNT16 (2-fold), FZD3 (3-fold), FZD6 (2-fold) and PCKε (7-fold) to be over-expressed. Western blotting analyses performed on 4 representative CLL patient cells for Ror-1 confirmed expression at the protein level (Supplementary Figure 2). These studies provide evidence for importance of the WNT-ROR-1 non-canonical pathway in CLL.
Figure 1.
Quantitative real time RT-PCR on 21 low stage CLL patients for selected genes of the WNT/FDZ canonical pathway where key members are down regulated except for LEF-1.
Figure 2.
Quantitative real time RT-PCR on 21 low stage CLL patients for selected genes of the WNT/PCP non-canonical pathway where key members are over-expressed.
The SCP and GEP identified Flt-3L to be elevated (serum) and FLT-3 to be over-expressed (microarray) in all 8 CLL patients. RT-PCR of 20 CLL patients for FLT-3 showed that 8 (40%) had over-expression while 12 (60%) had no change in expression (Supplementary Figure 3) Please see in supplementary materials avilable online at doi:10.1155/2007/453634. We next searched for downstream signaling molecules associated with Flt-3 activation and identified over-expression of PIM-1 (8-fold) (proviral insertional mutagenesis-1 serine/threonine kinase) and c-MYB (4-fold) proto-oncogenes. This novel finding implicates activation of the FLT-3 RTK pathway in a subset of CLL that may contribute to cell survival. In acute myeloid leukemia (AML), FLT-3 signaling up-regulates PIM-1 expression and activation [29] but such a role has not been previously described for CLL. Hence, our finding of coexpression of Flt-3L and FLT-3 L-R pair is novel and requires further investigation.
3.4. Status of P53 and Zap70 in Low Stage CLL Patients
Both ZAP-70 and P53 have been demonstrated to be important prognostic factors in CLL. In a subset of CLL patients with 17p deletion where p53 is lost an aggressive chemo-resistant clinical course ensues. ZAP-70 expression apparently identifies a CLL subtype with an inferior clinical outcome. We conducted quantitative real time RT-PCR on 21 low stage CLL patients for ZAP-70 and P53 expression (Supplementary Figure 4). The results show that P53 is down-regulated in almost all patients, while ZAP-70 is over-expressed in 18 of 21 patients. It is possible that a small fraction of contaminating normal T-cells in the purified CLL samples may affect the ZAP-70 RT-PCR data, however the differential expression observed by GEP suggests this is minimal. The down regulation of p53 expression in low stage CLL appears to be an early event in the oncogenic program.
3.5. Differential Gene Expression of CLL Cells at 24 Hours in Culture
It is an enigma as to why CLL cells purified from patients are not amenable to medium and long term cell culture. These predominantly mature malignant B-cells are resistant to apoptosis but once in cell culture lose viability. A key goal of the study was to identify factor(s) that may contribute to loss of viability and differential gene expression by GEP was utilized to investigate this phenomenon. A GEP study of 4 CLL patients at 0 hours and at 24 hours in culture showed several genes to be differentially expressed at 24 hours (Supplementary Table 1). The chemokine CXCL5 was ~120 fold over-expressed followed by several other chemokines, CCL (2, 3 and 23) and CXCL (1, 2 and 3) subtypes. Interleukins-1 (α and β), IL-6 and IL-8 were also over-expressed.
3.6. Thalidomide is not cytotoxic and induces modest GEP changes
The iMiDs thalidomide and lenalidomide are currently under evaluation as potential novel agents in Phase I trials in CLL (24). We investigated the effect of thalidomide on the differential gene expression of 4 CLL patient cells treated in culture for 24 hours. Since there were gene expression changes at 24 hours in culture without thalidomide therapy, these changes were taken into account when analyzing the effects of thalidomide on changes in gene expression. Cell viability studies indicated thalidomide was not cytotoxic to CLL cells (data not shown). Thalidomide induced modest differential gene expression changes (Supplementary Table 2), with CCL5 ~2.5 fold over-expressed.
3.7. Discovery of New Therapeutic Targets
Our study also analyzed potential therapeutic targets that may be amenable to targeting either with small molecular inhibitors and/or monoclonal antibodies. For patients with CLL the following are novel targets: small molecular inhibitors to protein kinases (ROR-1, Flt-3, ZAP-70, PIM-1, LCK PFTK1, PLK-3), monoclonal antibodies to circulating ligands (CXCL9, IGFBP4, Flt-3 ligand, PDGF-DD, FGF2) and monoclonal antibodies to cell surface receptor (FZD3, Flt-3, ROR-1, CXCR3).
4. Discussion
We undertook a gene expression and serum cytokine profile study of low stage CLL patients to glean biological insights into disease pathogenesis. First, our data confirmed the key GEP findings of Klein et al., 2001[12] and Jelinek et al., 2003 [17] and significantly adds to current knowledge of CLL biology. Second, we identified several significantly over-expressed novel genes that enhance further differentiation of CLL from normal circulating PB B-cells. This has allowed an extension of the molecular signature profile based on the six hallmarks of cancer [23] for CLL. Third, a serum cytokine profile of 26 CLL patients show several elevated cytokines/growth factors that are novel and help identify ligand-receptor pairs that may be pertinent to CLL biology. Finally, quantitative real time RT-PCR and Western blotting analyses of key genes and proteins respectively were utilized to validate and confirm the GEP.
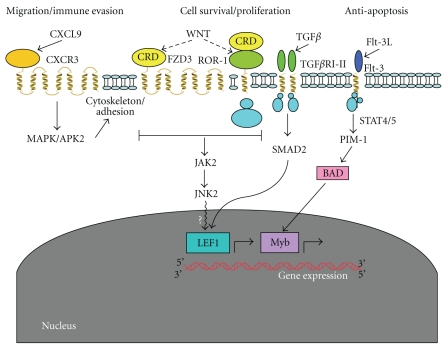
The WNT/FDZ3-ROR-1 PCP non-canonical pathway is over-expressed in CLL cells. The PCP signaling pathway controls tissue polarity and cell movement through activation of RhoA, c-Jun N-terminal kinase (JNK), and nemo-like kinase (NLK). Human Wnt5A, Wnt5B, and Wnt11 are non-canonical Wnt ligands that transduce PCP signals through FZD3 or FZD6 receptors, and coreceptors ROR-1, ROR-2 or PTK7. The aberrant activation of WNT/PCP signaling pathway leads to a malignant phenotype with associated abnormal tissue polarity, invasion, and metastasis [30]. Previously, Lu et al., 2004 [19], provided evidence for the WNT/FZD canonical pathway as a possible mechanism of oncogenesis and cell survival in CLL. RT-PCR of both the canonical and non-canonical pathway members, confirmed down regulation of the WNT/FDZ canonical pathway (DLV1, AXIN, FRAT-1, GSK-3β, β-CATENIN, TCF) except for LEF-1 which was over-expressed in all patients (Figure 1). Over-expression of LEF-1 in CLL cells has been described [12, 17, 19] and appears to play a role in pro-B cell development but not in mature B-cells [31]. In contrast, we found that FZD3 to be over-expressed and FZD6 to be down-regulated, while their coreceptor Ror-1 and JNK-2 of the WNT/PCP pathway are over-expressed (Figure 2). ROR-1 is a neural developmental kinase (937 amino acids) [32] but its cellular role has not been fully characterized. A truncated ROR-1 is found to be expressed in human leukemia and lymphoma cell lines and in several human neuroectodermal malignancies [33]. A mechanism is proposed for activation of the FZD3-ROR-1 PCP pathway (Figure 3) via Wnt binding to the Ror-1 CRD [34]. Thus a switch from WNT/FZD canonical to WNT/PCP non-canonical signaling in CLL is proposed.
Figure 3.
Schematic representation of four novel signaling pathways that may contribute to the malignant phenotype observed in early stage CLL.
Although key members of the WNT/FZD canonical pathway are down regulated in CLL, LEF-1 is over-expressed. This discrepancy may be due to expression and activation of LEF-1 via an alternative signaling pathway(s). Evidence points to the TGFβ pathway, where TGF-β1 and -β3 are elevated in the serum cytokine profile while TGF-β receptor III (TGF-β RIII, β-glycan) and SMAD2 are over-expressed in the GEP. The TGFβ pathway is known to cross-talk with the WNT signaling pathway via Smads [35, 36]. TGFβ can also induce novel LEF-1 splice variants through a Smad-independent signaling pathway [37]. Therefore, in CLL the expression and activation of LEF-1 may occur through TGF β-Smad dependent or independent mechanisms (Figure 3). Moreover, CLL cells respond abnormally to TGFβ stimulation [38] and over-expression of TGF-βRIII has been linked to over-expression of mutant K-ras [39]. Hence, it is conceivable that over-expression of RASGRF1 in CLL (Table 1) [40] may activate the MAP kinase pathway leading to LEF-1 activation. Mikels and Nusse (2006) have shown that when Ror-2 is expressed, Wnt5A [41] and more recently IGFBP-4 [42] have been shown to inhibit canonical signaling downstream of β-catenin stabilization at the level of TCF driven transcription. A similar mechanism may operate in CLL where Ror-1 is expressed and an alternative pathway activates LEF-1.
The study identified CXCL9-CXCR3 L-R pair where CXCL9 levels are elevated in the serum and CXCR3 was over-expressed in the GEP (Table 3(b)). CXCR3, a G-protein coupled chemokine receptor is normally expressed on Th1 cells and its expression is associated with peripheral inflammation. Th1 cells express CXCR3 during activation and differentiation implying effector functions in both central and peripheral lymphoid tissue [43]. CLL cells highly express CXCR3, which promotes efficient migration in response to CXCL9 in comparison to normal PB B-cells [27]. CXCL9 is coexpressed with CXCR3 in CLL [28] implicating an autocrine mechanism of malignant B-cell activation and promotion of migration (Figure 3). Interferon-γ (IFNγ) the 1st ranked elevated cytokine (Table 3(a)) in the cytokine profile is known to induce CXCL9 required for T-cell recruitment and effector functions [44]. A similar mechanism may operate in CLL cells.
Flt-3L is elevated in the serum cytokine profile and FLT-3 is over-expressed by GEP. RT-PCR analysis of 20 CLL patients confirmed over-expression of FLT-3 (6-40 fold) in a subset of cases (40%) (Supplementary Figure 3). Flt-3 is constitutively activated due to internal tandem duplication (ITD) mutations in the juxta-membrane domain in a majority of patients with acute myeloid leukemia (AML) and acute B-cell leukemia (ALL) [29]. Kim K-T et al., 2005 [45], demonstrated that PIM-1, a proto-oncogene with serine/threonine kinase activity is significantly down-regulated when Flt-3 is inhibited with CEP-701, an Flt-3 tyrosine kinase inhibitor. A similar inhibitory effect with CEP-701 was also shown for BAD (Bcl-2 antagonist of cell death) phosphorylation [45]. In our GEP, PIM-1 is over-expressed while its substrates c-MYB, BCL11B, STAT4 and CDC25B are also over-expressed. Pim-1 is known to be up-regulated by stat 5, which is also a downstream target of Flt-3 signaling. We propose that activated Flt-3 up-regulates and activates Pim-1 kinase providing proliferative and anti-apoptotic signals to some CLL cells.
Hemoglobin (HB) A and B are over-expressed in CLL patients (Table 2(a)). Alpha and beta-globin RNA have been detected in erythroid cells (fetal liver and reticulocytes) and non-erythroid tissues (adult brain and liver, and cultured lymphoma, untransformed, and transformed fibroblast cell lines) [46]. Reactive oxygen species (ROS) at physiological concentrations are required for normal cell function but excessive production of ROS is detrimental to cells. It has been shown that treatment of HT-29 colon cancer cells with HB enhanced proliferation via reactive oxygen species (ROS) production and significantly blunts the cytotoxic effects of 5-FU and 5-DFUR [47]. Papillary thyroid carcinomas (PTC) express HBB at similar levels to normal thyroid gland but over-expression of HBB in KTA2 cells (anaplastic thyroid cancer cell line), significantly suppressed their growth [48]. In CLL, there is progressive accumulation of well differentiated malignant cells that are arrested in G0/G1 and generation of excessive ROS in this setting would be detrimental. Therefore, over-expression of HBA and HBB may counter excessive ROS production and be protective to CLL cells.
P53 and ZAP-70 are important markers of CLL pathogenesis. We show that P53 expression is down regulated and ZAP-70 is over-expressed in low stage CLL (Supplementary Figure 4). When the white cell count or the absolute lymphocyte count (ALC) was plotted against P53 or ZAP-70 level of expression, there is no significant correlation. Hence, the loss of P53 or gain of ZAP-70 function is independent of disease burden, but may be related to initiation and progression of the abnormal CLL clone.
CLL cells are resistant to apoptosis but once in cell culture appear to lose viability. Several different approaches to maintain CLL cells in culture have been investigated but none has been successfully implemented [49]. We hypothesize that a major reason for inability to grow these cells is due to the removal of a factor or factors from their natural (plasma or serum) environment. We demonstrate that CLL cells elaborate a chemokine-cytokine response to being in culture at 24 hours. It is known that CLL cells regulate the microenvironment through modulation of the cytokine milieu that recruit and activate immune cells (T-cells). Since standard culture conditions do not have access to accessory survival mechanisms, these cells undergo apoptosis over a period of 1-2 weeks.
Targeting of the tumor microenvironment with immunomodulatory (iMiD) agents such as thalidomide and lenalidomide has been evaluated in CLL [24] with promising clinical activity [50]. Thalidomide therapy in CLL cells showed no cytotoxicity, and a similar result has been reported for lenalidomide in in vitro tumor models of CLL [24]. We also evaluated differential gene expression between thalidomide untreated and treated CLL cells in culture for 24 hours and showed very modest gene expression changes. This is consistent with its proposed mechanism of action on the stroma and activation of the immune system rather than a direct effect on malignant cells. The lack of a direct effect of thalidomide on CLL cells in culture and activity in patients implies a role for iMiDs in modulating the stromal microenvironment for their therapeutic efficacy.
5. Conclusion
Our study identified 3 novel differentially expressed oncogenic pathways pertinent to low stage CLL patients. These pathways are implicated aberrant regulation of cell proliferation, survival and migration of CLL cells. Further, in most of the patients p53 is down-regulated while ZAP70 is up-regulated suggesting a common mechanism of pathogenesis. Interferonγ, Flt-3L and IGFBP4 are the most prominent serum cytokines in low stage CLL with the latter implicated in modulating the Wnt signaling pathway [51]. The 6 essential alterations in cell physiology that collectively dictate malignant growth (CLL) are represented by 25–30 up-regulated over-expressed cancer genes and down-regulated tumor suppressors which appear to determine a slow proliferator phenotype. This CLL phenotype has gained the ability to avoid immune attack by NK and T-cells by secreting factors that inhibit effector activity and appears to subvert the bone marrow stromal environment for survival. Our data provide a platform to extend these studies to high stage (Rai III/IV) CLL patients. A recent GEP study of Waldenstrom macroglobulinemia (WM) showed a phenotype similar to CLL and PB B-cells than multiple myeloma [52] implicating a small set of differentially expressed genes which may distinguish between these lymphoproliferative diseases.
Supplementary Material
Supplementary Material is divided into figures and tables presented as follows.
Supplementary Figure 1 shows an analysis of a representative Ficoll-density purified CLL blood sample. Using 4 color flow cytometry, the majority of cells, 85%, show dual staining for both CD5 and CD20. Supplementary Figure 2 shows Western blotting analyses of 4 representative CLL patient cells for ROR-1 expression. Supplementary Figure 3 shows a Real time RT-PCR analysis of 20 CLL patients cells for FLT-3 expression. Finally, Supplementary Figure 4 presents a Quantitative real time RT-PCR on 21 low stage CLL patients for ZAP-70 and p53. ZAP70 is over-expressed and p53 is down regulated in low stage CLL.
Supplementary Table 1 shows Differential GEP of low stage CLL cells at 0-Hr Vs 24-Hr in Culture, and Supplementary Table 2 shows Differential GEP of low stage CLL cells treated with thalidomide at 24-Hr in culture.
Acknowledgments
The authors wish to thank Sunni Beeck for technical help and Drs. Thomas P. Miller and Lee D. Cranmer for identifying CLL patients for this study. This research was made possible through Preceptorship funds and patient gifts.
References
- 1.Cheson BD, Bennett JM, Grever M, et al. National Cancer Institute-sponsored Working Group guidelines for chronic lymphocytic leukemia: revised guidelines for diagnosis and treatment. Blood. 1996;87(12):4990–4997. [PubMed] [Google Scholar]
- 2.Mahadevan D, Garewal H. Advances in the diagnosis and treatment of Chronic Lymphocytic Leukemia. American College of Physicians-American Board of Internal Medicine. PIER Module ACP-ASIM, October 2003.
- 3.Döhner H, Stilgenbauer S, Benner A, et al. Genomic aberrations and survival in chronic lymphocytic leukemia. The New England Journal of Medicine. 2000;343(26):1910–1916. doi: 10.1056/NEJM200012283432602. [DOI] [PubMed] [Google Scholar]
- 4.Hamblin TJ, Davis Z, Gardiner A, Oscier DG, Stevenson FK. Unmutated Ig VH genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood. 1999;94(6):1848–1854. [PubMed] [Google Scholar]
- 5.Fais F, Ghiotto F, Hashimoto S, et al. Chronic lymphocytic leukemia B cells express restricted sets of mutated and unmutated antigen receptors. Journal of Clinical Investigation. 1998;102(8):1515–1525. doi: 10.1172/JCI3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Damle RN, Wasil T, Fais F, et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood. 1999;94(6):1840–1847. [PubMed] [Google Scholar]
- 7.Orchard JA, Ibbotson RE, Davis Z, et al. ZAP-70 expression and prognosis in chronic lymphocytic leukaemia. The Lancet. 2004;363(9403):105–111. doi: 10.1016/S0140-6736(03)15260-9. [DOI] [PubMed] [Google Scholar]
- 8.Rassenti LZ, Huynh L, Toy TL, et al. ZAP-70 compared with immunoglobulin heavy-chain gene mutation status as a predictor of disease progression in chronic lymphocytic leukemia. The New England Journal of Medicine. 2004;351(9):893–901. doi: 10.1056/NEJMoa040857. [DOI] [PubMed] [Google Scholar]
- 9.Wiestner A, Rosenwald A, Barry TS, et al. ZAP-70 expression identifies a chronic lymphocytic leukemia subtype with unmutated immunoglobulin genes, inferior clinical outcome, and distinct gene expression profile. Blood. 2003;101(12):4944–4951. doi: 10.1182/blood-2002-10-3306. [DOI] [PubMed] [Google Scholar]
- 10.Del Principe MI, Del Poeta G, Buccisano F, et al. Clinical significance of ZAP-70 protein expression in B-cell chronic lymphocytic leukemia. Blood. 2006;108(3):853–861. doi: 10.1182/blood-2005-12-4986. [DOI] [PubMed] [Google Scholar]
- 11.Haslinger C, Schweifer N, Stilgenbauer S, et al. Microarray gene expression profiling of B-cell chronic lymphocytic leukemia subgroups defined by genomic aberrations and VH mutation status. Journal of Clinical Oncology. 2004;22(19):3937–3949. doi: 10.1200/JCO.2004.12.133. [DOI] [PubMed] [Google Scholar]
- 12.Klein U, Tu Y, Stolovitzky GA, et al. Gene expression profiling of B cell chronic lymphocytic leukemia reveals a homogeneous phenotype related to memory B cells. Journal of Experimental Medicine. 2001;194(11):1625–1638. doi: 10.1084/jem.194.11.1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stratowa C, Löffler G, Lichter P, et al. CDNA microarray gene expression analysis of B-cell chronic lymphocytic leukemia proposes potential new prognostic markers involved in lymphocyte trafficking. International Journal of Cancer. 2001;91(4):474–480. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1078>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 14.Rosenwald A, Alizadeh AA, Widhopf G, et al. Relation of gene expression phenotype to immunoglobulin mutation genotype in B cell chronic lymphocytic leukemia. Journal of Experimental Medicine. 2001;194(11):1639–1647. doi: 10.1084/jem.194.11.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haferlach T, Kohlmann A, Schnittger S, et al. Global approach to the diagnosis of leukemia using gene expression profiling. Blood. 2005;106(4):1189–1198. doi: 10.1182/blood-2004-12-4938. [DOI] [PubMed] [Google Scholar]
- 16.Kienle DL, Korz C, Hosch B, et al. Evidence for distinct pathomechanisms in genetic subgroups of chronic lymphocytic leukemia revealed by quantitative expression analysis of cell cycle, activation, and apoptosis-associated genes. Journal of Clinical Oncology. 2005;23(16):3780–3792. doi: 10.1200/JCO.2005.02.568. [DOI] [PubMed] [Google Scholar]
- 17.Jelinek DF, Tschumper RC, Stolovitzky GA, et al. Identification of a global gene expression signature of B-chronic lymphocytic leukemia. Molecular Cancer Research. 2003;1(5):346–361. [PubMed] [Google Scholar]
- 18.Calin GA, Ferracin M, Cimmino A, et al. A microRNA signature associated with prognosis and progression in chronic lymphocytic leukemia. The New England Journal of Medicine. 2005;353(17):1793–1801. doi: 10.1056/NEJMoa050995. [DOI] [PubMed] [Google Scholar]
- 19.Lu D, Zhao Y, Tawatao R, et al. Activation of the Wnt signaling pathway in chronic lymphocytic leukemia. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(9):3118–3123. doi: 10.1073/pnas.0308648100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DaneshManesh AH, Mikaelsson E, Jeddi-Tehrani M, et al. Ror1, a cell surface receptor tyrosine kinase is expressed in chronic lymphocytic leukemia and may serve as a putative target for therapy. International Journal of Cancer. 2008;123(5):1190–1195. doi: 10.1002/ijc.23587. [DOI] [PubMed] [Google Scholar]
- 21.Green JL, Kuntz SG, Sternberg PW. Ror receptor tyrosine kinases: orphans no more. Trends in Cell Biology. 2008;18(11):536–544. doi: 10.1016/j.tcb.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oishi I, Suzuki H, Onishi N, et al. The receptor tyrosine kinase Ror2 is involved in non-canonical Wnt5a/JNK signalling pathway. Genes to Cells. 2003;8(7):645–654. doi: 10.1046/j.1365-2443.2003.00662.x. [DOI] [PubMed] [Google Scholar]
- 23.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70. doi: 10.1016/s0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 24.Chanan-Khan A, Porter CW. Immunomodulating drugs for chronic lymphocytic leukaemia. The Lancet Oncology. 2006;7(6):480–488. doi: 10.1016/S1470-2045(06)70723-9. [DOI] [PubMed] [Google Scholar]
- 25.Durai R, Davies M, Yang W, et al. Biology of insulin-like growth factor binding protein-4 and its role in cancer. International Journal of Oncology. 2006;28(6):1317–1325. [PubMed] [Google Scholar]
- 26.Tohda S, Nara N, Murohashi I, Aoki N. Establishment of an interleukin-3-dependent leukemic cell line from a patient with chronic lymphocytic leukemia in the acute phase. Blood. 1991;78(7):1789–1794. [PubMed] [Google Scholar]
- 27.Trentin L, Agostini C, Facco M, et al. The chemokine receptor CXCR3 is expressed on malignant B cells and mediates chemotaxis. Journal of Clinical Investigation. 1999;104(1):115–121. doi: 10.1172/JCI7335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones D, Benjamin RJ, Shahsafaei A, Dorfman DM. The chemokine receptor CXCR3 is expressed in a subset of B-cell lymphomas and is a marker of B-cell chronic lymphocytic leukemia. Blood. 2000;95(2):627–632. [PubMed] [Google Scholar]
- 29.Kim K-T, Baird K, Ahn J-Y, et al. Pim-1 is up-regulated by constitutively activated FLT3 and plays a role in FLT3-mediated cell survival. Blood. 2005;105(4):1759–1767. doi: 10.1182/blood-2004-05-2006. [DOI] [PubMed] [Google Scholar]
- 30.Katoh M. WNT/PCP signaling pathway and human cancer. Oncology Reports. 2005;14(6):1583–1588. [PubMed] [Google Scholar]
- 31.Reya T, O’Riordan M, Okamura R, et al. Wnt signaling regulates B lymphocyte proliferation through a LEF-1 dependent mechanism. Immunity. 2000;13(1):15–24. doi: 10.1016/s1074-7613(00)00004-2. [DOI] [PubMed] [Google Scholar]
- 32.Masiakowski P, Carroll RD. A novel family of cell surface receptors with tyrosine kinase-like domain. The Journal of Biological Chemistry. 1992;267(36):26181–26190. [PubMed] [Google Scholar]
- 33.Reddy UR, Phatak S, Pleasure D. Human neural tissues express a truncated Ror1 receptor tyrosine kinase, lacking both extracellular and transmembrane domains. Oncogene. 1996;13(7):1555–1559. [PubMed] [Google Scholar]
- 34.Saldanha J, Singh J, Mahadevan D. Identification of a Frizzled-like cysteine rich domain in the extracellular region of developmental receptor tyrosine kinases. Protein Science. 1998;7(8):1632–1635. [PMC free article] [PubMed] [Google Scholar]
- 35.Edlund S, Lee SY, Grimsby S, et al. Interaction between Smad7 and β-catenin: importance for transforming growth factor β-induced apoptosis. Molecular and Cellular Biology. 2005;25(4):1475–1488. doi: 10.1128/MCB.25.4.1475-1488.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Medici D, Hay ED, Goodenough DA. Cooperation between snail and LEF-1 transcription factors is essential for TGF-β1-induced epithelial-mesenchymal transition. Molecular Biology of the Cell. 2006;17(4):1871–1879. doi: 10.1091/mbc.E05-08-0767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cordray P, Satterwhite DJ. TGF-β induces novel Lef-1 splice variants through a Smad-independent signaling pathway. Developmental Dynamics. 2005;232(4):969–978. doi: 10.1002/dvdy.20275. [DOI] [PubMed] [Google Scholar]
- 38.Lagneaux L, Delforge A, Bernier M, Stryckmans P, Bron D. TGF-β activity and expression of its receptors in B-cell chronic lymphocytic leukemia. Leukemia and Lymphoma. 1998;31(1-2):99–106. doi: 10.3109/10428199809057589. [DOI] [PubMed] [Google Scholar]
- 39.Yan Z, Deng X, Friedman E. Oncogenic Ki-ras confers a more aggressive colon cancer phenotype through modification of transforming growth factor-β receptor III. The Journal of Biological Chemistry. 2001;276(2):1555–1563. doi: 10.1074/jbc.M004553200. [DOI] [PubMed] [Google Scholar]
- 40.Zippel R, Balestrini M, Lomazzi M, Sturani E. Calcium and calmodulin are essential for Ras-GRF1-mediated activation of the Ras pathway by lysophosphatidic acid. Experimental Cell Research. 2000;258(2):403–408. doi: 10.1006/excr.2000.4937. [DOI] [PubMed] [Google Scholar]
- 41.Zhu W, Shiojima I, Ito Y, et al. IGFBP-4 is an inhibitor of canonical Wnt signalling required for cardiogenesis. Nature. 2008;454(7202):345–349. doi: 10.1038/nature07027. [DOI] [PubMed] [Google Scholar]
- 42.Mikels AJ, Nusse R. Purified Wnt5a protein activates or inhibits beta-catenin-TCF signaling depending on receptor context. PLoS Biology. 2006;4(4, article e115):1–13. doi: 10.1371/journal.pbio.0040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rabin RL, Alston MA, Sircus JC, et al. CXCR3 is induced early on the pathway of CD4+ T cell differentiation and bridges central and peripheral functions. The Journal of Immunology. 2003;171(6):2812–2824. doi: 10.4049/jimmunol.171.6.2812. [DOI] [PubMed] [Google Scholar]
- 44.Whiting D, Hsieh G, Yun JJ, et al. Chemokine monokine induced by IFN-γ/CXC chemokine ligand 9 stimulates T lymphocyte proliferation and effector cytokine production. The Journal of Immunology. 2004;172(12):7417–7424. doi: 10.4049/jimmunol.172.12.7417. [DOI] [PubMed] [Google Scholar]
- 45.Kim K-T, Levis M, Small D. Constitutively activated FLT3 phosphorylates BAD partially through Pim-1. British Journal of Haematology. 2006;134(5):500–509. doi: 10.1111/j.1365-2141.2006.06225.x. [DOI] [PubMed] [Google Scholar]
- 46.Humphries S, Windass J, Williamson R. Mouse globin gene expression in erythroid and non erythroid tissues. Cell. 1976;7(2):267–277. doi: 10.1016/0092-8674(76)90026-x. [DOI] [PubMed] [Google Scholar]
- 47.Lee R-A, Kim H-A, Kang B-Y, Kim K-H. Hemoglobin induces colon cancer cell proliferation by release of reactive oxygen species. World Journal of Gastroenterology. 2006;12(35):5644–5650. doi: 10.3748/wjg.v12.i35.5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Onda M, Akaishi J, Asaka S, et al. Decreased expression of haemoglobin beta (HBB) gene in anaplastic thyroid cancer and recovery of its expression inhibits cell growth. British Journal of Cancer. 2005;92(12):2216–2224. doi: 10.1038/sj.bjc.6602634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ghia P, Circosta P, Scielzo C, et al. Differential effects on CLL cell survival exerted by different microenvironmental elements. Current Topics in Microbiology and Immunology. 2005;294:135–145. doi: 10.1007/3-540-29933-5_8. [DOI] [PubMed] [Google Scholar]
- 50.Chanan-Khan A, Miller KC, Musial L, et al. Clinical efficacy of lenalidomide in patients with relapsed or refractory chronic lymphocytic leukemia: results of a phase II study. Journal of Clinical Oncology. 2006;24(34):5343–5349. doi: 10.1200/JCO.2005.05.0401. [DOI] [PubMed] [Google Scholar]
- 51.Zhu W, Shiojima I, Ito Y, et al. IGFBP-4 is an inhibitor of canonical Wnt signalling required for cardiogenesis. Nature. 2008;454(7202):345–349. doi: 10.1038/nature07027. [DOI] [PubMed] [Google Scholar]
- 52.Chng WJ, Schop RF, Price-Troska T, et al. Gene-expression profiling of Waldenström macroglobulinemia reveals a phenotype more similar to chronic lymphocytic leukemia than multiple myeloma. Blood. 2006;108(8):2755–2763. doi: 10.1182/blood-2006-02-005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material is divided into figures and tables presented as follows.
Supplementary Figure 1 shows an analysis of a representative Ficoll-density purified CLL blood sample. Using 4 color flow cytometry, the majority of cells, 85%, show dual staining for both CD5 and CD20. Supplementary Figure 2 shows Western blotting analyses of 4 representative CLL patient cells for ROR-1 expression. Supplementary Figure 3 shows a Real time RT-PCR analysis of 20 CLL patients cells for FLT-3 expression. Finally, Supplementary Figure 4 presents a Quantitative real time RT-PCR on 21 low stage CLL patients for ZAP-70 and p53. ZAP70 is over-expressed and p53 is down regulated in low stage CLL.
Supplementary Table 1 shows Differential GEP of low stage CLL cells at 0-Hr Vs 24-Hr in Culture, and Supplementary Table 2 shows Differential GEP of low stage CLL cells treated with thalidomide at 24-Hr in culture.