Abstract
Ascertaining the symptom experience of chronically critically ill (CCI) patients is difficult due to communication impairment and fluctuations in patient cognition and physiological conditions. The use of checklist self report ratings is hampered by the inability of most CCI patients to respond verbally to symptom queries. In addition to the communication problems caused by mechanical ventilation, the apparently diverse idioms of symptom expression add to the potential for miscommunication regarding symptom experience. Although patient communication impairment is a major barrier to symptom identification, symptom assessment and treatment are fundamental components of nursing care for CCI. This paper reviews and describes the unique constellation of symptoms experienced by many critically ill patients. We report our observations of symptom communication among CCI patients and nurses and discuss inconsistency in the language of symptom expression among nurses and patients. Clinically applicable strategies to improve nurse-patient symptom communication and suggestions for refinement of symptom assessment in chronic critical illness are provided.
Keywords: Symptom assessment, chronic critical illness, nonverbal communication
Introduction and Background
A symptom is defined as a “subjective experience reflecting changes in the biopsychosocial functioning, sensations or cognition of an individual.” 1 (p.669) Symptom amelioration comprises an essential aspect of nursing care during prolonged critical illness, as nurses intervene to minimize the psychological and physiological effects of noxious symptoms such as pain, dyspnea, and worry. Indeed, Doran and colleagues2 proposed that symptom frequency and severity are nurse-sensitive patient outcomes. For the chronically critically ill (CCI) patient, who is typically mechanically ventilated and thus, nonspeaking, nurses' interpretation of the patient's entire symptom experience (both physical and psycho-emotional aspects) becomes key to symptom relief.
More than a protracted period of acute critical illness, chronic critical illness is a distinct syndrome of multisystem alterations that includes metabolic, neuroendocrine, neuropsychiatric, and immunologic dysfunction. The only hallmark of this syndrome is the need for prolonged mechanical ventilation at some point during its trajectory. The CCI may be cared for in a variety of settings, including inpatient respiratory care units, long term acute care hospitals, and nursing homes. Despite receiving technologically advanced care, outcomes are poor in the CCI. This population exhibits high rates of mortality, poor functional status, and reduced quality of life. In essence, the CCI are those patients who survive an acute, life threatening episode but progress to a chronic and prolonged state of multi-organ compromise with recurring complications, prolonged dependence on medical and nursing care, high symptom burden, and poor outcomes.
Because of the prolonged, symptom-laden nature of chronic critical illness,3-5 it is incumbent on nurses to fully evaluate these patients' symptom experience. Although the perception of the individual experiencing the symptom is considered to be the “gold standard” for identifying and studying symptoms,1 obtaining data on symptom experience during chronic critical illness is difficult. Symptom assessment is impeded by communication impairments secondary to respiratory tract intubation and mechanical ventilation. In addition, recall biases and fluctuations in patient cognitive and physiological status hamper accurate retrospective recall of symptoms experienced.6 In one sample of CCI patients, 75% exhibited cognitive impairment at study enrollment, and nearly 40% exhibited cognitive impairment at the end of their RCU (respiratory care unit) stay.4 Such difficulty with symptom assessment may lead to inadequately treated symptoms and high levels of untreated pain or misinterpretation of nonverbal cues.7 For example, when he had finally regained the ability to speak, a CCI patient reported to the Speech-Language Pathologist (SLP) that the nurses misinterpreted his mouthed word as “pain” when he was actually requesting a pair of pants! (Brooke Paull, SLP, personal communication July 15, 2009). In a classic study, Baer and colleagues8 found that professional caregivers (nurses, physicians, and social workers) attributed higher pain levels to patients able to verbalize their pain than to their nonverbal counterparts. The authors speculated that professionals may believe that patients experiencing pain are responsible to verbalize their symptoms to the health care team to receive treatment. In contrast, in a retrospective record review of 52 mechanically ventilated patients, investigators reported that both physicians and nurses documented observable indicators of pain such as cardiorespiratory signs, body movements, and ventilator compliance more frequently than patient self reports of pain, indicating that physicians' and nurses' interpretation of symptom experience is an important aspect of providing care to CCI patients.9 Clinicians interprete physiological and behavioral signs as indicators of pain, however, dyspnea, anxiety, or fear, are also competing explanations for the meaning of these physiological and behavioral signs. Thus, we need to better understand the process of symptom assessment and symptom identification in the care of CCI patients.
Symptom Identification
Symptom assessments often employ checklist self report ratings. Many symptom surveys, such as the Memorial Symptom Assessment Scale, were originally designed for use in outpatient cancer care and require retrospective recall about symptom presence and intensity during the preceding days or weeks.10, 11 These tools have also been applied to other chronic health conditions such as chronic obstructive pulmonary disease and AIDS.12 Use of assessment techniques designed for the setting and type of population is crucial, as various symptoms may occur as a result of disease process or treatments experienced during the illness trajectory.13 The symptom experience of the CCI is likely to be quite different than that of cancer patients in an outpatient or community setting.
Nelson and colleagues3 applied the Condensed Memorial Symptom Assessment Scale (C-MSAS)14 to CCI patients in an RCU. Using the C-MSAS, a self-report numerical rating scale, CCI patients were asked to rate symptom distress and frequency for each of 15 symptoms, using word descriptor scales (e.g., “Never” to “Almost constantly”). Seventy-two percent of queried patients in Nelson's study were able to respond to symptom questions at least once during their period of mechanical ventilation (“responders”). The number of times patients were unable to respond to queries was not reported. Symptom assessments were performed twice a week, for an average of 3-4 weeks, yet the mean number of responses to the twice-weekly symptom queries among the participating patients was 3.6 out of the potential 6 - 8 total opportunities. Patients were unable to respond to symptom queries for a variety of reasons, including “lacking capacity,” on a number of occasions. Patients unable to communicate by verbalizing, writing, or pointing to a card, were excluded from the study.3
Nelson's study3 was the first to focus on the symptom experience of CCI patients receiving mechanical ventilation in the post-intensive care unit (ICU) phase of illness. Importantly, the use of prospective methods in this study avoided the recall bias and exclusion of non-survivors inherent in retrospective symptom experience studies, and recognized the necessity of symptom assessment on a ‘real-time’ basis. The exclusion of patients with complex communication difficulties, and the potentially high number of nonresponses in this study, highlight the need for improving symptom assessment methods for the most seriously ill and the CCI, typically the most debilitated nonverbal and cognitively impaired patients in ICU and post-ICU settings.
Puntillo's seminal program of research elucidated the importance of assessing, documenting, and treating pain among acutely critically ill patients, including procedural pain15-17 as well as the generalized symptom experience during acute critical illness.18 Critically ill, mechanically ventilated patients may, however, experience a wide range of other symptoms beyond pain and dyspnea that are difficult but important to assess. In three separate studies of CCI, symptoms were prevalent in over 90% of subjects; pain was predominant in a list of symptoms that also included dyspnea, distress related to communication, fatigue, and anxiety.3-5
Our research team is currently studying symptom communication between nonspeaking mechanically ventilated patients and their nurses to investigate relationships between communication performance, symptom management, and clinical outcomes in the ICU (K24- NR010244, M. Happ). Most patients in our study qualify as CCI, with the average time on mechanical ventilation 23 days at the beginning of study observations. Thus, we are gaining unique insight into the symptom experience and communication about symptoms, treatments offered and enacted in the care of CCI patients.
Conceptual Model
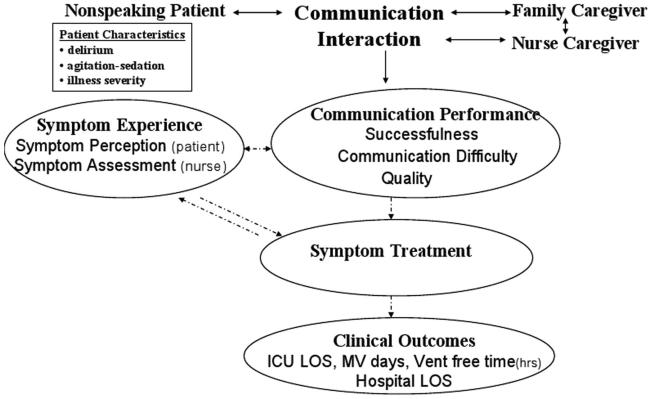
The conceptual model informing the work upon which this article is based is an adaptation of the Revised Symptom Management Model,1 in which symptom experience and treatment are proposed to be mediated by nurse-patient communication [Figure 1]. Difficulty, quality, and success of nurse-patient communication may impact symptom identification and treatment, in turn potentially affecting clinical outcomes such as days of mechanical ventilation, ICU length of stay, hospital length of stay, and comfort over what is usually a very protracted course in acute care settings. Further, the relationship between nurse-patient communication and symptom experience is likely bi-directional. That is, while the communication process impacts symptom interpretation and treatment, the nurse's interpretation of the CCI patient's symptom experience may also affect subsequent nurse-patient communication. Appropriate symptom treatment is crucial, as it may impact clinical outcomes including length of ICU stay and weaning from mechanical ventilation.
Figure 1.
Symptom Communication, Management and Outcomes Model. (based on Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nur 2001; 33(5):668-676.)
Key to abbreviations: ICU = Intensive Care Unit; LOS = length of stay; MV = mechanical ventilation
When direct patient-nurse communication is difficult or impossible, symptoms experienced by nonverbal CCI patients must be interpreted by proxies (for example, family or members of the clinical teams) for treatment to occur. Research, however, has suggested that proxy symptom reports show low to moderate concordance with patient symptom self reports.5, 18 Learning more about patient-nurse communication (both verbal and nonverbal) is crucial, then, to improving the accuracy of symptom assessment and treatment with CCI patients.
The remainder of this paper will discuss symptoms commonly experienced by CCI and/or mechanically ventilated patients. We include insights gleaned thus far during our study of nurse-patient symptom communication and the clinical implications for critical care nurses.
Symptom Assessment and Symptom Communication in CCI
Nelson3 pioneered the identification of a unique set of symptoms experienced by CCI patients, which has been further expanded upon by Wiencek.5 Li19 conducted similar work with mechanically ventilated ICU patients. Although studies of outpatient cancer patients identified pain, nausea, depression, and fatigue as the most commonly reported distressful symptoms,13 studies of CCI patients identify a constellation of symptoms that seem related to respiratory failure and respiratory tract intubation. The critical care studies suggest that CCI patients experience a different set of symptoms than other populations, and that this symptom set may require unique assessment and management techniques.
The most frequently noted symptoms among CCI patients in the Nelson et al. study included pain, lack of energy, difficulty communicating, thirst, dyspnea, and psychological symptoms such as sadness, nervousness, and worry.3 Over 50% of patients reported experiencing these common physical symptoms at levels termed “quite a bit” or “very” distressing. Moreover, psychological symptoms were more prevalent in the CCI than physical symptoms. Nelson and colleagues found that 70% of the sample experienced worry on a “frequent” or “almost constant” basis, and over 60% reported a similar frequency of both sadness and nervousness. These results are congruent with a review of several studies of symptom assessment in ICU previously performed by Nelson's group in 2001,20 in which they concluded that, in addition to pain, ICU patients frequently experience high levels of dyspnea, anxiety, and fear while being mechanically ventilated.
Li19 noted a similar symptom constellation in a pilot study of coexisting symptoms of mechanically ventilated ICU patients in which all study patients reported some degree of dyspnea. Forty percent of the sample experienced severe thirst and moderate to severe pain, while moderately intense tiredness, hunger, generalized discomfort, and depressed feelings were experienced by more than 30% of participants. In addition, Wiencek5 performed a secondary analysis of a CCI database in which both patients and proxies responded to the question, “What symptoms are most bothersome at this time?” Congruent with other studies' findings,3, 19 patients were most bothered by pain, fatigue, and respiratory distress. Further, proxy respondents thought that patients were most bothered by pain, loss of independence, communication difficulty, and impaired cognition.5
Puntillo's18 qualitative exploration of how nurses assess and treat symptoms among nonverbal critically ill patients provides further insight into the symptom experience of acute and chronic critical illness. This study focused on the nurse's assessment process and subsequent choice of treatments for patients unable to self report. Using a series of open-ended questions, interviewers queried nurses about the approaches they used to identify symptoms and to select treatments to alleviate those symptoms. Based on these interviews, Puntillo18 surmised that when confronted with patient inability to self report symptoms, nurses rely on physiologic signs (e.g., heart rate, blood pressure), behavioral signs (e.g., tearfulness, restlessness), or a combination of both to identify that symptoms are present. However, similar changes in vital signs or behaviors may be associated with many different symptoms. For example, elevated heart rate, blood pressure, and respiratory rate could be signs of pain, anxiety, dyspnea, or fear. How, then, do nurses identify the specific symptom and provide appropriate treatment? One possible explanation is that nurses may use their own personal or professional experiences to find potential meaning in their observations of the patient, and provide treatment based on these personal interpretations.18 Puntillo's study further illustrates the key role that nurses play in the assessment and interpretation of symptom manifestations in understanding and treating symptoms of the nonspeaking CCI patient. These studies demonstrate that ICU patients experience a range of symptoms that are difficult to accurately identify. The logical implication of these findings is that this range of patient symptoms continues to be under-assessed and undertreated in the ICU.
We recently conducted an extensive literature review to identify definitions of the symptoms likely to be experienced by CCI, mechanically ventilated patients. These definitions were used to identify symptoms from 356 videorecorded observations of nurse-patient communication among 89 nurse-patient dyads. These patients had been intubated an average of 23 days before enrollment in the study. Overall, the group's median length of time on mechanical ventilation was 35 days during lengthy hospital stays, ranging from 7- 297 days (median = 50 days). When applying literature-derived definitions to actual communication between nurses and CCI patients, we noted the use of inconsistent and overlapping terminology for naming and describing symptoms as well as some differences between patients and nurses in language used. Such discrepancies may contribute to a lack of congruence noted in some studies between patients and surrogates (nurses or family caregivers) when identifying symptoms.5 Some of the differences between literature and nurse-patient terminology are shown in Table 1.21-34 We concentrate here specifically on the set of symptoms most common among CCI patients.
Table 1.
Definitional Terms for Common Symptoms in Chronic Critical Illness.
| Symptom and references |
Literature-Derived Definition | Nurse-Patient Terminology |
|---|---|---|
| Lack of Energy21-23 |
|
|
| Thirst 24 |
|
|
| Dry Mouth25, 26 |
|
|
| Dyspnea27 |
|
|
| Anxiety28, 29 |
|
|
| Worry30-32 |
|
|
| Communication Difficulty30, 33, 34 |
|
|
Pain
Visual analog scales (VAS) or verbally administered numerical rating scales (NRS) have been used to assess pain. As with other types of self report instruments, impaired cognitive, physical, and communicative abilities may prevent adequate patient expression of symptom distress. Several published pain assessment scales have been designed for use with nonverbal patients, including the Behavioral Pain Rating Scale,35 the PAIN Algorithm,36 the Behavioral Pain Scale,37 the Nonverbal Pain Scale (NPS),38 the Pain Behavior Assessment Tool,17 and the Critical Care Pain Observation Tool.39 (See Table 2 for a synopsis of these instruments. For an in-depth discussion of these instruments, there are several reviews of interest.40-43) Some of these scales combine physiological and behavioral signs of pain with technology interface (i.e., ventilator asynchrony).44
Table 2.
Pain Assessment Tools for Nonverbal Patients
| Assessment Tool | Features | Score Range | Advantages and Disadvantages40 |
|---|---|---|---|
| Behavioral Pain Rating Scale 35 |
|
|
|
| PAIN Algorithm36 |
|
|
|
| Behavioral Pain Scale 37 |
|
|
|
| Nonverbal Pain Scale 38 |
|
|
|
| Pain Behavior Assessment Tool 17 |
|
|
|
| Critical Care Pain Observation Tool 39 |
|
|
|
Despite increasing awareness of the prevalence of pain in the CCI since early work highlighting this issue,7 high rates of unrelieved pain remain in critical illness.3, 5, 20 In our review of video recorded care episodes, we have noted that nurses often query patients regarding presence of pain, which patients may deny. Despite patients' denial of pain, the focus of conversation during the remainder of the care episode frequently involved identifying and resolving various noxious stimuli such as nasogastric or endotracheal tubes, positioning issues, room temperature, or even wrinkled linens, all of which cause great patient discomfort, if not pain. Perhaps pain represents to nurses a set of conditions related to various aspects of physical discomfort. By using a broad conceptualization of pain assessment to include various sources of discomfort, nurses may seek to decrease the perception of pain among the CCI.
Lack of Energy and Fatigue
Although lack of energy is a distinct symptom on assessment checklists such as the C-MSAS, this symptom label is not widely used in the literature, appearing in only one article.21 Most authors refer to fatigue,22, 23, 45, 46 and may equate fatigue with lack of energy.45 Fatigue is defined as a “subjective, unpleasant symptom…ranging from tiredness to exhaustion” interfering with the “ability to function.”23 (p.527) Inherent in these definitions is the implication that fatigue affects one's ability to perform mental and/or physical work. Some authors note that ‘tiredness’ implies a temporary situation of energy depletion, while ‘fatigue’ connotes a chronic condition.22 This level of discrimination is difficult, and perhaps unnecessary, in sedentary, bed-ridden critically ill and CCI patients.
We found, during observations of video recorded care episodes, that several terms are used interchangeably by patients and nurses. Symptom terminology and descriptors that were not included in formal definitions of lack of energy, tiredness, and fatigue, were often used by patients and nurses to seemingly describe tiredness and lack of energy. For example, while patients do not commonly complain of lethargy, nurses frequently described patients' as “lethargic” in clinical documentation and in conversations with other team members, such as physicians and respiratory therapists. Likewise, although considered distinct in academic symptom definitions, nurses and patients often used the terms ‘sleepy’ or ‘drowsy’ when discussing patients' tiredness and lack of energy. Finally, ‘weakness’ is defined as objective measures of muscle strength, 21 yet patients and nurses also use the term, ‘weakness,’ when discussing the subjective experience of fatigue and lack of energy. In our video examples and review of nurses' clinical record documentation, nurses and patients appear to equate ‘weakness’ with the subjective sensation of inability to perform physical activities rather than an objective assessment of muscle strength. These findings illuminate the need for nurses caring for the CCI to be aware of the various types of fatigue or lack of energy that this population may experience. Ameliorative interventions for muscle weakness or deconditioning are different than those appropriate for sleepiness. The few extra minutes needed to delve more deeply into patients' individual experiences of lack of energy could result in greatly improved symptom management. The nurse may wish to query patients for the presence of sleepiness, muscle fatigue or weakness, and ability to participate in functional activities (such as turning, getting out of bed) in order to fully assess fatigue and determine appropriate interventions.
Thirst and Dry Mouth
Nelson's work exploring the symptoms experienced by CCI patients showed that thirst is a distinct symptom experienced at high rates among critically ill patients, and this symptom was added to the modified C-MSAS.3 The symptom literature uses patient self-report regarding degree of distress related to dry mouth rather than describing or defining thirst. Thirst is presented as the result of a dry mouth, implying that the two often occur concomitantly and is described simply as a desire to drink fluids.24 No conceptual work has been published to differentiate between thirst and dry mouth. Nurses and patients in our video recorded care episodes certainly used these terms interchangeably. Treatment for these two symptoms was often the same, consisting mostly of offering mouth swabs and lip moisturizer, and when appropriate, ice chips.
In contrast to CCI, the oncologic symptom literature contains numerous references to dry mouth(xerostomia), a common side effect of many cancer treatment regimens.47 Dry mouth is also common in other populations such as renal dialysis patients48 as well as among healthy elderly people, in addition to those with chronic illnesses.47 Subjective “thirst,” however, receives little attention in the chronic illness literature. CCI patients have the added “drying” insult of oral or tracheal intubation and may be unable to safely swallow oral fluids, causing thirst and dry mouth to be particularly distressing. Thus, thirst and dry mouth are overlapping, interdependent symptoms among ventilator-dependent CCI patients that require frequent nursing assessment and treatment. Nurses can ask about both dry mouth and thirst in order to determine the most appropriate interventions for the patient's particular symptom experience.
Dyspnea
Most nurses are extensively trained in assessment of breathing difficulties. Objective measures of breathing effectiveness such as noting respiratory rate and character, observing for cyanosis, auscultating for adventitious breath sounds, and measuring oxygen saturation, are basic aspects of physical assessment for most patients. However, the patient's experience surrounding breathing difficulties may encompass much more than can be gleaned by observation of physiologic signs. The subjective experience of dyspnea is comprised of 3 dimensions: physiologic, functional, and psychological.27 Physiologic aspects reflect measurable parameters such as respiratory rate and oxygenation levels. Functional aspects of dyspnea are expressions of the affect breathlessness has on the patient's ability to complete various activities of daily living. When patients discuss psychological aspects of dyspnea, they refer to emotional state(s) associated with difficulty breathing, such as feelings of suffocation, fear, or anxiety. Thus, nurses and CCI patients address various aspects of shortness of breath when communicating about their symptoms. In nonverbal patients, it is difficult to ensure that patient and nurse are discussing the same aspects of the symptom. For example, when patients in our study reported shortness of breath or feelings of difficulty breathing, especially during ventilator weaning trials, nurses would often respond: “Yes, you're tired from breathing on your own. We'll put you back on the vent now so that you can rest,” implying a functional focus. Nurses also addressed the physiologic aspects of dyspnea, for example, informing a patient who complains of shortness of breath that her “numbers” (pulse oximetry) are below the desired level, and that the weaning trial will be discontinued.
Less commonly were nurses and patients observed discussing possible feelings of fear when patients reported breathing difficulty. This may be due to the difficulty in communicating abstract emotional constructs in the presence of respiratory tract intubation. To ensure that all aspects of the experience of dyspnea are addressed, nurses could ask patients whether they are afraid when they experience breathing difficulties. When patients exhibit signs of possible anxiety, nurses should remember that, even in the absence of physiologic data indicating poor oxygenation, patients may feel a sense of dyspnea and react with anxiety or fear; asking patients whether they feel short of breath may provide an opportunity for reassurance and education and reduce the need to administer anxiolytic medications. Further, because of the multiple meanings and labels used for tiredness by both patients and nurses, it is important for nurses to fully validate patients' symptom experience through clarification whenever possible. For example, a nurse might ask, “I want to make sure I understand, are you feeling sleepy or tired from the breathing work?”
Psychological Symptoms
Emotional or psychological symptoms are often experienced by the CCI and critically ill individuals. 3, 19 Sadness and depression, fear, worry, anxiety or nervousness are terms that nurses in our study used when naming these abstract constructs. As with other symptoms, we observed that clinicians and patients used terms interchangeably that the definitional literature treats as distinct constructs. For example, anxiety is defined as a somatic response characterized by a vague, generalized feeling of uneasiness or increasing tension. It may be accompanied by objective signs such as trembling, cardiovascular excitation, and motor agitation.28, 29 In contrast to generalized anxiety manifested by somatic responses, worry is described as a purely cognitive symptom in which the negative feelings have some specific object.30, 32 That is, while anxiety is generalized, worry is about something specific. In our observations, nurses and patients do not seem to make these distinctions regarding generalized versus specific origins for the subjective feelings. Rather, worry and anxiety are used interchangeably with “nervous,” and even colloquial terms. One patient reported feeling “jumpy” in several videorecorded sessions, without clear identification of cause. Nurses offered various treatments including reassurance, anxiolytic medications, and analgesia.
Communication Difficulty
Communication difficulty ranks as one of the most common, distressing symptoms of CCI. Although it is a “condition” caused by respiratory tract intubation, communication difficulty certainly meets the definition of symptom as a “subjective experience reflecting changes in the biopsychosocial functioning…of an individual.” 1(p.669) Nurses may not regularly assess or document this condition; yet, it remains a frequent source of distress among ICU patients.49 Nelson's group, the first to designate difficulty communicating as a “symptom” in chronic critical illness, found that difficulty communicating was one of the most distressing symptoms experienced by two separate samples of the mechanically ventilated, comprising 50 CCI patients3 and 100 critically ill cancer patients,20 respectively. This finding is corroborated by studies of perceived stressors during critical illness,50-53 and studies of the experience of mechanical ventilation and of nurse-patient communication in the ICU.34, 54, 55
Other psychological symptoms such as anxiety, panic, frustration, anger, and sleeplessness are associated with the inability to communicate during mechanical ventilation treatment.30,49-51 These psychobehavioral symptoms are often treated with sedating medications which can prolong treatment with mechanical ventilation and may cause or potentiate delirium, further isolating the critically ill patient from nurses and family visitors and placing them at risk for adverse sequelae of critical illness. Moreover, hospitalized patients who have a communication impairment are more likely to experience a preventable adverse event than patients without communication impairments.56 These studies have clearly established the problem and potential consequences of communication impairment during critical illness. Yet, we have noted infrequent explicit assessment of this symptom by nurses. The literature on communication difficulty documents few nurse-initiated ameliorative interventions.57 Nurses should maintain heightened awareness of the prevalence and serious consequences of communication difficulty among those with CCI, and should include assessment of communication difficulty in their plan of care.
In addition to involving other members of the interdisciplinary team, particularly the speech-language pathologist, to assist with evaluation of communication difficulties and initiation of appropriate interventions, the nurse can advocate with the entire care team to facilitate consistent use of recommended adaptive communication strategies during all care interactions, potentially resulting in improved symptom identification and management by all disciplines.
Clinical Implications for Critical Care Nurses
The CCI symptom research literature reviewed in this paper highlights the unique symptom burden experienced by this population. Symptoms commonly experienced include pain, lack of energy, thirst, dry mouth, psychological symptoms such as anxiety and worry, and communication difficulty. Complicating symptom identification is a lack of universally agreed-upon definitions for these distressing symptoms. Literature-based definitions, a foundation of symptom management research, may differ from the language of symptom expression used in daily practice by nurses and patients. Improving nurses' appreciation for language or naming differences and their understanding of the importance of validating the interpretation of symptom messages with nonspeaking CCI patients is essential to improving symptom management in this patient population.
The central role of communication difficulty as both symptom, and as context in which symptoms are interpreted, is critical to understanding and improving the symptom experience for CCI patients. The research literature has clearly established the problem and potential consequences of communication impairment during prolonged critical illness. Addressing communication impairments and preventing the detrimental effects of communication difficulty is a safety and quality of care concern for critical care nurses. There is a growing recognition that improved communication is essential to improve the quality and safety of healthcare in America;58, 59 however, patient communication impairment has received little to no attention in critical care quality and safety research. Nonvocal critically ill and CCI patients are at risk for suboptimal management and high distress over a protracted course of illness. In addition to improving the patient's critical care experience, improved communication performance between the patient and nurse may reduce misunderstanding, misinterpretation, and missed communication that can be potential sources of error.
Interventions to improve patient communication in the ICU have been described and pilot tested with mixed, but promising, results.57, 60-67 Recently, there are multiple resources for structuring patient communication interventions and improving nurse communication skills.63, 68, 69 The speech-language pathologist can be a key member of the interdisciplinary team for CCI patients, recommending assisted communication strategies based on an assessment of the patient's motor and cognitive abilities, and providing a resource for staff, patients, and family/significant others.
Communication difficulty with nonvocal patients may discourage critical care nurses from directly asking about many symptoms, especially psychological symptoms such as sadness or worry. When patients are nonvocal, whether due to intubation or to physical or cognitive deficits, nurses essentially ‘control’ the conversation and are responsible for naming the symptoms being experienced. Treatments are based on the symptom labels assigned by the nurse. However, as Puntillo18 noted, nurses may provide “treatments” based on observation of objective signs such as vital sign changes, without fully ascertaining patient perceptions about current symptoms. Yet these objective signs could indicate a number of potential subjective sources of distress. Symptom assessment is incomplete without explicit validation of the patient's subjectively experienced symptoms, and symptoms that are not fully assessed cannot be adequately treated. In addition, if nurses attempt to elicit self-report information about the symptom from the patient, but the communication difficulty is too great, the patient may acknowledge symptoms such as pain or dyspnea, because communicating about more subtle symptoms is simply too exhausting or too frustrating.
Nurses combine observation of signs with context and empathic interpretation of how they might feel in a similar situation18 to identify potential symptoms. Identification, clarification, and validation of the subjective symptom(s) being manifested through the signs observed by the nurse should be accomplished using as many communication techniques as possible, including communication boards, tagged yes/no questions, or computer technologies designed to permit patient self expression.63 While these augmentative communication techniques are not appropriate for heavily sedated or comatose patients, they can provide useful adjuncts to care for many conscious patients struggling for a way to communicate with healthcare providers and their loved ones.
Critical care nurses can further positively impact the care of the chronically critically ill by maintaining familiarity with the symptoms most commonly experienced including pain, lack of energy, thirst, dry mouth, dyspnea, psychological symptoms such as anxiety and worry, and communication difficulty. Providing appropriate treatment still depends upon accurate symptom identification by the nurse. Nurse awareness of the most frequently occurring symptoms, combined with use of easily learned communication techniques, permit healthcare providers of all disciplines to obtain patient reports of symptoms and enabling targeted treatment of those symptoms.
Simple Techniques to Improve Symptom Communication
Commercially available communication boards or “printed” communication boards developed by nurses or SLPs can facilitate communication about symptom location (body part), intensity (visual analogue or numerical rating scales), and quality (descriptor word list). Communication board examples are available at http://www.pitt.edu/~speacs and from the CD-ROM accompanying the Beukelman, Garrett, and Yorkston text64 or from commercial sources (see http://www.vidatak.com/).66 Nurses can encourage the consistent use of gesture and pointing to indicate symptom location and intensity.70 Topic communication lists for symptom identification can help narrow the focus of symptom queries.63 Establishing a clear and consistent YES – NO response with patients facilitates accurate confirmation and validation of the patient's message.34, 68, 71 For patients who are sedated or have difficulties with attention and focus, tagging the end of a YES-NO question (Example: “Are you having pain – Yes (slight pause) or No?”) can provide the focus necessary for the patient to complete a response.72 At minimum, nurses should gain the CCI patient's attention before speaking, speak clearly, slowly and provide adequate time for the patient to respond 73 (For additional communication tips, go to http://hartfordign.org/uploads/File/nursing_counts/AJNFinal5_06.pdf).
Because most CCI patients have tracheostomies, they can be encouraged to mouth words in a slow, exaggerated manner while pointing to the first letter of each word as it is mouthed. This technique, “first letter spelling,” can increase accuracy of lip reading when patients are cognitively intact, fairly literate, and able to point74, 75 Patients who are cognitively intact and have good arm and hand coordination can be assisted with writing using clipboards, pen grips, and other adaptive writing supports.64 Involve occupational therapy to obtain the adaptive equipment best suited to patients' abilities and consult speech language pathology for patients with complex communication needs such as those with limited upper extremity movement (e.g., spinal cord injury, Guillian Barre, myasthenia gravis, cerebral vascular accident).
Future research
Finally, further clinically-based research is needed, with collaboration between bedside nurses and researchers, to further illuminate the language of symptom experience most commonly used by the chronically critically ill. Patricia Benner76 describes how nurses learn from patients, developing the learned information into sets of “common meanings” that “evolve over time and are shared among nurses.” 76(p.6) Researchers and nurses caring for the CCI can further the development of these shared common meanings, with the goal of better understanding the symptom experience in the CCI to facilitate improved management and improved patient outcomes.
Conclusion
Accurate assessment and appropriate treatment of identified symptoms is a vital nursing role when caring for the CCI, with their high incidence of cognitive impairment and communication barriers such as sedating medications, artificial airways, prolonged mechanical ventilation, and protracted stays in acute care settings. Effective symptom management is associated with improved patient outcomes such as more ventilator-free days and shorter lengths of stay.
Mechanically ventilated critically ill adults may manifest symptoms via various behavioral and physiological signs that could be associated with a variety of symptoms. Evidence has shown that the CCI most frequently experience pain, lack of energy and fatigue, thirst and dry mouth, dyspnea, anxiety and worry, and communication difficulty. It is imperative that nurses caring for CCI patients understand the unique symptoms likely to be experienced by their patients, and allow sufficient time for adequate assessment of these symptoms. Nurses need to educate the CCI and their families that emotional and psychological symptoms such as anxiety, fear, and worry are common, and permit patients to acknowledge these feelings. It is also incumbent upon nurses to work with the interdisciplinary team to implement appropriate communication strategies to facilitate patient communication of their symptom experience and to allow patient participation in selecting effective, timely treatment of those symptoms.
Acknowledgements
We thank Jill Radtke and Judith Tate, University of Pittsburgh School of Nursing doctoral students, for their insights regarding symptom language between nurses and ICU patients.
Funding Source: National Institute for Nursing Research, Grant # K24- NR010244; Symptom Management, Patient-Caregiver Communication, and Outcomes in ICU. M. Happ, P.I.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Grace B. Campbell, John A. Hartford Foundation “Building Academic Geriatric Nursing Capacity” Predoctoral Scholar, University of Pittsburgh School of Nursing 336 Victoria Building 3500 Victoria Street Pittsburgh, PA 15261.
Mary Beth Happ, University of Pittsburgh School of Nursing 336 Victoria Building 3500 Victoria Street Pittsburgh, PA 15261.
References
- 1.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. Journal of Advanced Nursing. 2001;33(5):668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 2.Doran DM, Harrison MB, Laschinger HS, et al. Nursing-sensitive outcomes data collection in acute care and long-term-care settings. Nurs Res. 2006;55(2 suppl):S75–81. doi: 10.1097/00006199-200603001-00012. [DOI] [PubMed] [Google Scholar]
- 3.Nelson J, Meier DE, Litke A, Natale DA, Siegel RE, Morrison SR. The symptom burden of chronic critical illness. Crit Care Med. 2004;32:1527–1534. doi: 10.1097/01.ccm.0000129485.08835.5a. [DOI] [PubMed] [Google Scholar]
- 4.Nelson JE, Tandon N, Mercado AF, Camhi SL, Ely EW, Morrison RS. Brain dysfunction: another burden for the chronically critically ill. Arch Int Med. 2006;166(18):1993–1999. doi: 10.1001/archinte.166.18.1993. [DOI] [PubMed] [Google Scholar]
- 5.Wiencek C. Symptom burden and its relationship to functional status in the chronically critically ill [Dissertation] School of Nursing, Case Western Reserve University; Cleveland, OH: 2008. [Google Scholar]
- 6.van de Leur JP, van der Schans CP, Loef BG, Deelman BG, Geertzen JHB, Zwaveling JH. Discomfort and factual recollection in intensive care unit patients. Crit Care. 2004;8:R467–R473. doi: 10.1186/cc2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puntillo KA. Pain experiences of intensive care unit patients. Heart Lung. 1990;19(5 Pt 1):526–533. [PubMed] [Google Scholar]
- 8.Baer E, Davitz LJ, Lieb R. Inferences of physical pain and psychological distress in relation to verbal and nonverbal patient communication. Nurs Res. 1970;19(5):388–392. [PubMed] [Google Scholar]
- 9.Gelinas C, Fortier M, Viens C, Fillion L, Puntillo K. Pain assessment and management in critically ill intubated patients: a retrospective study. Am J Crit Care. 2004;13(2):126–135. [PubMed] [Google Scholar]
- 10.Chang VT, Hwang SS, Geuerman M, Kaismis BS, Thaler HT. The Memorial Symptom Assessment Scale short form (MSAS-SF) validity and reliability. Cancer. 2000;89(5):1162–1171. doi: 10.1002/1097-0142(20000901)89:5<1162::aid-cncr26>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 11.Portenoy RK, Thaler HT, Kornblith AB, et al. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics, and distress. Eur J Cancer Care. 1994;30A(9):1326–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 12.Kris AE, Dodd MJ. Symptom experience of adult hospitalized medical-surgical patients. Pain Symptom Manage. 2004;28(5):451–459. doi: 10.1016/j.jpainsymman.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Barsevick AM, Whitmer K, Nail LM, Beck SL, Dudley WN. Symptom cluster research: conceptual, design, measurement, and analysis issues. Pain Symptom Managet. 2006;31(1):85–95. doi: 10.1016/j.jpainsymman.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 14.Chang VT, Hwang SS, Kaismis BS, Thaler HT. Shorter symptom assessment instruments: The Condensed Memorial Symptom Assessment Scale (CMSAS) Cancer Invest. 2004;22(4):526–536. doi: 10.1081/cnv-200026487. [DOI] [PubMed] [Google Scholar]
- 15.Puntillo K, Wild LR, Morris AB, Stanik-Hutt J, Thompson CL, White C. Practices and predictors of analgesic interventions for adults undergoing painful procedures. Am J Crit Care. 2002;11(5):415–429. [PubMed] [Google Scholar]
- 16.Puntillo KA. Dimensions of procedural pain and its analgesic management in critically ill surgical patients. Am J Crit Care. 1994;3(2):116–122. [PubMed] [Google Scholar]
- 17.Puntillo KA, White C, Morris AB, et al. Patients' perceptions and responses to procedural pain: results from Thunder Project II. Am J Crit Care. 2001;10(4):238–251. [PubMed] [Google Scholar]
- 18.Puntillo K, Smith D, Arai S, Stotts N. Critical care nurses provide their perspectives of patients' symptoms in intensive care units. Heart Lung. 2008;37(6):466–475. doi: 10.1016/j.hrtlng.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Li DT, Puntillo K. A pilot study on coexisting symptoms in intensive care patients. Appl Nurs Res. 2006;19:216–219. doi: 10.1016/j.apnr.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Nelson JE, Meier DE, Oei EJ, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29(2):277–282. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Molassiotis A. A correlational evaluation of tiredness and lack of energy in survivors of haematological malignancies. Eur J Cancer Care. 1999;8:19–25. doi: 10.1046/j.1365-2354.1999.00109.x. [DOI] [PubMed] [Google Scholar]
- 22.National Cancer Care Network Guidelines in oncology: cancer-related fatigue. http://www.nccn.org/professionals/physician_gls/PDF/fatigue.pdf. Accessed September 29, 2009.
- 23.Ream E, Richardson A. Fatigue: a concept analysis. Int J Nurs Stud. 1996;33(5):519–529. doi: 10.1016/0020-7489(96)00004-1. [DOI] [PubMed] [Google Scholar]
- 24.Bots CP, Brand HS, Veerman ECI, et al. Interdialytic weight gain in patients on hemodialysis is associated with dry mouth and thirst. Kidney Int. 2004;66:1662–1668. doi: 10.1111/j.1523-1755.2004.00933.x. [DOI] [PubMed] [Google Scholar]
- 25.Nagler RM. Salivary glands and the aging process: mechanistic aspects, health-status and medicinal-efficacy monitoring. Biogerontology. 2004;5:223–233. doi: 10.1023/B:BGEN.0000038023.36727.50. [DOI] [PubMed] [Google Scholar]
- 26.Thomson WM. Measuring change in dry-mouth symptoms over time using the Xerostomia Inventory. Gerodontology. 2007;24:30–35. doi: 10.1111/j.1741-2358.2007.00137.x. [DOI] [PubMed] [Google Scholar]
- 27.MacDonald S, Yates J, Lance R, Giganti N, Chepurko D. Are you asking the right admission questions when assessing dyspnea? Heart Lung. 2005;34:260–269. doi: 10.1016/j.hrtlng.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Bay EJ, Algase DL. Fear and anxiety: a simultaneous concept analysis. Nur Diagnosis. 1999;10(3):103–111. doi: 10.1111/j.1744-618x.1999.tb00036.x. [DOI] [PubMed] [Google Scholar]
- 29.Grossman S, Labedzki D, Butcher R, Dellea L. Definition and management of anxiety, agitation, and confusion in ICUs. Nurs Connect. 1996;9(2 (Summer)):49–55. [PubMed] [Google Scholar]
- 30.Menzel LK. Factors related to the emotional responses of intubated patients being unable to speak. Heart Lung. 1998;27(4):245–252. doi: 10.1016/s0147-9563(98)90036-x. [DOI] [PubMed] [Google Scholar]
- 31.Price RB, Mohlman J. Inhibitory control and symptom severity in late life generalized anxiety disorder. Behav Res Therapy. 2007;45:2628–2639. doi: 10.1016/j.brat.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Zebb BJ, Beck GJ. Worry versus anxiety: is there really a difference? BehavMod. 1998;22:45–61. doi: 10.1177/01454455980221003. [DOI] [PubMed] [Google Scholar]
- 33.Ebert DA. Communication disabilities among medical inpatients. New Engl J Med. 1998;339(4):272–273. doi: 10.1056/NEJM199807233390416. [DOI] [PubMed] [Google Scholar]
- 34.Happ MB. Interpretation of nonvocal behavior and the meaning of voicelessness in critical care. Soc Sci Med. 2000;50(9):1247–1255. doi: 10.1016/s0277-9536(99)00367-6. [DOI] [PubMed] [Google Scholar]
- 35.Mateo O, Krenzischek D. A pilot study to assess the relationship between behavioral manifestations and self-report of pain in postanesthesia care unit patients. J Post Anesth Nurs. 1992;7:15–21. [PubMed] [Google Scholar]
- 36.Puntillo K, Miaskowski C, Kehrle K, Stannard D, Gleeson S, Nye P. Relationship between behavioral and physiological indicators of pain, critical care patients' self-reports of pain, and opioid administration. Crit Care Med. 1997;25:1159–1166. doi: 10.1097/00003246-199707000-00017. [DOI] [PubMed] [Google Scholar]
- 37.Payen J, Bru O, Bosson J, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med. 2001;29:2258–2263. doi: 10.1097/00003246-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Odhner M, Wegman D, Freeland N, Steinmetz A, Ingersoll G. Assessing pain control in nonverbal critically ill adults. Dimens Crit Care Nurs. 2003;22(22):260–267. doi: 10.1097/00003465-200311000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Gelinas C, Fillion L, Puntillo K, Viens C, Fortier M. Validation of the critical care pain observation tool in adult patients. Am J Crit Care. 2006;15(4):420–427. [PubMed] [Google Scholar]
- 40.Li DT, Puntillo K, Miaskowski C. A review of objective pain measures for use with critical care adult patients unable to self-report. J Pain. 2008;9(1):2–10. doi: 10.1016/j.jpain.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 41.Jensen M, Karoly P, O'Riordan E, Bland F, Burns R. The subjective experience of acute pain: an assessment of the utility of 10 indices. Clin J Pain. 1989;5:153–159. doi: 10.1097/00002508-198906000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Paice J, Cohen F. Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs. 1997;20(2):88–93. doi: 10.1097/00002820-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Reading AE. A comparison of pain rating scales. J Psychosom Res. 1980;24(3-4):119–124. doi: 10.1016/0022-3999(80)90032-x. [DOI] [PubMed] [Google Scholar]
- 44.Kabes AM, Graves JK, Norris J. Further validation of the Nonverbal Pain Scale in intensive care patients. Crit Care Nurse. 2009;29(1):59–66. doi: 10.4037/ccn2009992. [DOI] [PubMed] [Google Scholar]
- 45.Gift AG, Shepard CE. Fatigue and other symptoms in patients with Chronic Obstructive Pulmonary Disease: do women and men differ? JOGN Nursing. 1999;28(2):201–208. doi: 10.1111/j.1552-6909.1999.tb01985.x. [DOI] [PubMed] [Google Scholar]
- 46.Trendall J. Concept analysis: chronic fatigue. J Adv Nurs. 2000;32(5):1126–1131. doi: 10.1046/j.1365-2648.2000.01583.x. [DOI] [PubMed] [Google Scholar]
- 47.Barasch A, Peterson DE. Risk factors for ulcerative oral mucositis in cancer patients: unanswered questions. Oral Oncol. 2003;39:91–100. doi: 10.1016/s1368-8375(02)00033-7. [DOI] [PubMed] [Google Scholar]
- 48.Bots CP, Brand HS, Veerman ECI, et al. Chewing gum as a saliva substitute alleviate thirst and xerostomia in patients on haemodialysis. Nephrol Dial Transplant. 2005;20:578–584. doi: 10.1093/ndt/gfh675. [DOI] [PubMed] [Google Scholar]
- 49.Nelson JE, Danis M. End-of-life care in the intensive care unit: where are we now? Crit Care Med. 2001;29(2 suppl.):N2–N9. doi: 10.1097/00003246-200102001-00002. [DOI] [PubMed] [Google Scholar]
- 50.Bergbom-Engberg I, Haljamae H. Assessment of patients' experience of discomforts during respirator therapy. Crit Care Med. 1989;17(10):1068–1072. doi: 10.1097/00003246-198910000-00021. [DOI] [PubMed] [Google Scholar]
- 51.Pennock BE, Crawshaw L, Maher T, Price T, Kaplan PD. Distressful events in the ICU as perceived by patients recovering from coronary artery bypass surgery. Heart Lung. 1994;23(4):323–327. [PubMed] [Google Scholar]
- 52.Rotondi AJ, Chelluri L, Sirio C, et al. Patients' recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 53.Wunderlich RJ, Perry A, Lavin MA, Katz B. Patients' perceptions of uncertainty and stress during weaning from mechanical ventilation. Dimens Crit Care Nurs. 1999;18(1):8–12. [PubMed] [Google Scholar]
- 54.Carroll SM. Silent, slow lifeworld: the communication experience of nonverbal patients. Qual Health Res. 2007;17(9):1165–1177. doi: 10.1177/1049732307307334. [DOI] [PubMed] [Google Scholar]
- 55.Wojnicki-Johansson G. Communication between nurse and patient during ventilator treatment: patient reports and RN evaluations. Int Crit Care Nurs. 2001;17(1):29–39. doi: 10.1054/iccn.2000.1547. [DOI] [PubMed] [Google Scholar]
- 56.Bartlett G, Blais R, Tamblyn R, et al. Impact of patient communication problems on the risk of preventable adverse events in the acute care settings. CAMJ. 2008;178:1555–1562. doi: 10.1503/cmaj.070690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Happ MB. Communicating with mechanically ventilated patients: State of the science. AACN Clin Issues. 2001;12(2):247–258. doi: 10.1097/00044067-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 58.Despins LA. Patient safety and collaboration of the intensive care unit team. Crit Care Nurse. 2009;29:85–92. doi: 10.4037/ccn2009281. [DOI] [PubMed] [Google Scholar]
- 59.Rothschild JM, Landrigan CP, Cronin JW, et al. The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. Critical Care Med. 2005;33:1694–1700. doi: 10.1097/01.ccm.0000171609.91035.bd. [DOI] [PubMed] [Google Scholar]
- 60.Dowden P, Beukelman DR, Lossing C. Serving nonspeaking patients in acute care settings: intervention outcomes. Augment Altern Commun. 1986;2(2):38–44. [Google Scholar]
- 61.Etchels MC, MacAulay F, Judson A, et al. ICU-Talk: the development of a computerised communication aid for patients in ICU. Care Crit Ill. 2003;19(1):4–9. [Google Scholar]
- 62.Fried-Oken M, Howard JM, Stewart SR. Feedback on AAC intervention from adults who are temporarily unable to speak. Augment Altern Commun. 1991;7(1):43–50. [Google Scholar]
- 63.Garrett KL, Happ MB, Costello JR, Fried-Oken MB. AAC in the Intensive Care Unit. In: Bukelman DR, Garrett KL, Yorkston KM, editors. Augmentative Communication Strategies for Adults with Acute or Chronic Medical Conditions. Paul H. Brookes Publishing C.; Baltimore, MD: 2007. [Google Scholar]
- 64.Happ MB, Roesch TK, Garrett K. Electronic voice-output communication aids for temporarily nonspeaking patients in a medical intensive care unit: a feasibility study. Heart Lung. 2004;33(2):92–101. doi: 10.1016/j.hrtlng.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 65.Miglietta MA, Bochicchio G, Scalea TM. Computer-assisted communication for critically ill patients: a pilot study. J Trauma. 2004;57(3):488–493. doi: 10.1097/01.ta.0000141025.67192.d9. [DOI] [PubMed] [Google Scholar]
- 66.Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients' reports of health care practitioner interventions that are related to communication during mechanical ventilation. Heart Lung. 2004;33:323–327. doi: 10.1016/j.hrtlng.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 67.Stovsky B, Rudy E, Dragonette P. Comparison of two types of communication methods used after cardiac surgery with patients with endotracheal tubes. Heart Lung. 1988;17(3):281–289. [PubMed] [Google Scholar]
- 68.Costello JM. AAC intervention in the intensive care unit: The Children's Hospital Boston model. Augment Altern Commun. 2000;16(3):137–153. [Google Scholar]
- 69.Happ MB, Paull B. Silence is not golden. Geriatr Nurs. 2008;29(3):166–168. doi: 10.1016/j.gerinurse.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Connolly MA. Communicating with temporarily nonvocal patients. Perspect Respir Nurs. 1995;6:7–9. [PubMed] [Google Scholar]
- 71.Hemsley B, Sigafoos J, Balandin S, et al. Nursing the patient with severe communication impairment. J Adv Nurs. 2001;35(6):827–835. doi: 10.1046/j.1365-2648.2001.01920.x. [DOI] [PubMed] [Google Scholar]
- 72.Beukelman DR, Mirenda P. Augmentative and Alternative Communication Supporting Children & Adults with Complex Communication Needs. 3rd ed. Paul H. Brookes Publishing Co.; Baltimore: 2005. [Google Scholar]
- 73.Happ MB, Tate J, Garrett K. Nonspeaking older adults in the ICU. Am J Nurs. 2006;106(5):37. [Google Scholar]
- 74.Beukelman DR, Yorkston KM. A communication system for severely dysarthric speakers with intact language system. J Speech Hear Disord. 1977;42:265–270. doi: 10.1044/jshd.4202.265. [DOI] [PubMed] [Google Scholar]
- 75.Yorkston KM, MIller R, Strand E. Management of Speech and Swallowing Diseases. 2nd ed. PRO-ED; Austin, TX: 2004. [Google Scholar]
- 76.Benner P. From Novice to Expert. Excellence and Power in Clinical Nursing Practice. Addison-Wesley Publishing Co.; Menlo Park, CA: 1984. [Google Scholar]