Abstract
Data consistently demonstrate comorbidity between pathological gambling and psychiatric disorders. This study compares severity of gambling and psychosocial problems and gambling treatment outcomes in treatment-seeking pathological gamblers (N = 231) based on their self-reported mental health treatment utilization. As expected, participants currently receiving mental health treatment demonstrated the most psychiatric problems, and those with no mental health treatment the least. Although preferred gambling activity differed according to mental health treatment status, severity of gambling problems and gambling treatment outcomes did not. Individual cognitive-behavioral therapy was efficacious in reducing gambling problems irrespective of mental health treatment utilization.
Pathological gambling is as an impulse control disorder characterized as the excessive risking of money and other valuables on games of chance by the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV).1 Lifetime prevalence rates of pathological gambling range from 0.4% to 1.9% in the general U.S. population.2–5 This disorder is associated with significant financial, social, medical, and psychiatric problems.2,5–7
Epidemiological studies find comorbidity between pathological gambling and substance use disorders. In a national sample of over 43,000 respondents, Petry et al.4 found that 73.2% of pathological gamblers (PGs) had a lifetime alcohol use disorder and 38.1% had a lifetime drug use disorder. In another study of 9,282 randomly selected household residents, Kessler et al.3 reported that 76.3% of respondents identified as PGs met criteria for a lifetime substance use disorder. In two smaller nationally-based surveys of about 2,000 respondents each, Gerstein et al.2 found that 9.9% of PGs had lifetime alcohol or drug dependence in comparison to 1.1% of non-gamblers, and Welte et al.5 also noted a strong association between pathological gambling and alcohol dependence. PGs were 23 times more likely to be currently alcohol dependent than non-PGs. In a Canadian study of 7,214 respondents, Bland et al.8 found that 63.3% of PGs met lifetime criteria for substance use disorders in comparison to 19.0% of non-gamblers.
Epidemiological studies also demonstrate co-occurring pathological gambling and other psychiatric disorders. For example, Bland et al.8 reported that 33.3% of PGs met lifetime criteria for an affective disorder, 26.7% for an anxiety or somatoform disorder, and 40.0% for antisocial personality disorder in comparison to 14.2%, 9.2%, and 3.1% of non-PGs, respectively. Petry et al.4 found that 49.6% of PGs met criteria for a lifetime mood disorder, 41.3% for an anxiety disorder, and 60.8% for a personality disorder, with all of these rates significantly greater among PGs than controls. Kessler et al.3 reported that 96.3% of PGs met criteria for at least one other psychiatric disorder during their lifetime, including mood disorders, anxiety disorders, and impulse-control disorders.
Consistent findings of high rates of comorbidity with psychiatric disorders are also noted in PG treatment-seeking populations. Kerber et al.9 found high levels of lifetime major depression (82.5%), anxiety disorders (47.5%), obsessive compulsive disorder (37.5%), panic disorder (27.5%), and avoidant personality disorder (27.5%) in their sample of treatment-seeking PGs. Ibáñez et al.10 noted that 62.3% of PGs met lifetime criteria for a comorbid psychiatric disorder, with the most common psychiatric diagnosis being personality disorders (42.0%). Pietrzak and Petry11 also found that 16.5% of PGs met diagnostic criteria for antisocial personality disorder. With respect to substance use disorders, Maccallum and Blaszczynski12 found that 16% of individuals who were receiving gambling treatment met current criteria for alcohol abuse and 8% met criteria for alcohol dependence. Stinchfield and Winters13 reported that 35% of treatment-seeking PGs had received alcohol or drug treatment services in the past, and 16% met diagnostic criteria for a current substance use disorder.
Given the high rates of psychiatric disorders among PGs, many may have received treatment for these conditions. Ladd and Petry14 found that 31.0% of treatment-seeking PGs had sought treatment for a substance use disorder, with 54.5% of them reporting treatment for alcohol use disorder, 8.4% for cocaine, and 28.3% for other drugs. Pathological gamblers with substance abuse treatment histories demonstrated more severe gambling, substance abuse, psychiatric, and employment problems than gamblers without treatment histories. Stinchfield et al.15 reported that 33.5% of treatment-seeking gamblers previously sought substance abuse treatment. In comparison to those without substance abuse treatment histories, those who had sought substance abuse treatment had higher rates of alcohol and drug use at the time of study participation and evidenced more psychosocial and marital problems. Although participants as a whole showed reductions in gambling over time, those with a substance abuse treatment history and who frequently drank alcohol showed greater improvement than participants with no substance abuse treatment history and who drank alcohol less frequently.
While treatment-seeking PGs with a history of substance abuse treatment demonstrate more severe gambling and psychosocial problems than those without a history of substance abuse treatment, little research has reported on PGs with and without treatment histories for other psychiatric conditions. In their epidemiological study, Kessler et al.3 found that 49.0% of individuals identified as PGs had sought treatment for an emotional or substance use disorder. Stinchfield et al.15 also reported that 45.5% of treatment-seeking PGs previously sought mental health treatment. However, no known studies have evaluated how mental health treatment status impacts gambling and other psychosocial problems in treatment-seeking gamblers.
Several studies have examined how the severity and presence of psychiatric symptoms may affect gambling treatment outcomes among PGs. This research generates mixed findings. For example, Echeburúa et al.16 found that PGs with high levels of anxiety were at an increased risk of dropping out of gambling treatment or relapsing in comparison to less anxious PGs. In contrast, Leblond et al.17 reported that the presence of depression and anxiety did not impact gambling treatment outcomes.
The purpose of this study is to examine the relationship between mental health treatment utilization and psychosocial functioning and gambling treatment outcomes among treatment-seeking PGs. We compared demographic characteristics and baseline severity of gambling and other psychosocial problems among PGs classified by mental health treatment utilization status. We hypothesized that PGs reporting current or past mental health treatment would demonstrate a greater severity of gambling and psychosocial problems in comparison to PGs reporting no mental health treatment. We also examined gambling treatment outcomes to ascertain whether mental health treatment status impacted response to gambling treatment.
METHODS
Participants
Two-hundred thirty-one participants meeting past-year DSM-IV1 criteria for PG were recruited through media announcements in Connecticut for a treatment study between 1998 and 2002. Participants were at least 18 years old, had gambled in the past two months, and had at least a fifth-grade reading level. Individuals currently experiencing suicidal intentions or psychotic symptoms, or who were already receiving gambling treatment, were excluded from the study.
The present study is a retrospective analysis using data from the original report.18 We categorized participants in the following three groups according to their self- reported utilization of mental health treatment services at intake: those who had never received mental health treatment (“no mental health treatment”), those with a history of mental health treatment (“past mental health treatment”), and those currently receiving mental health treatment (“current mental health treatment”). Mental health treatment was defined as treatment for any emotional or psychological problem, ranging from marital concerns to depression, anxiety, or schizophrenia, but did not include prior or current gambling or substance abuse treatment.
Instruments
An adapted version of The Structured Clinical Interview for the DSM-IV was used to evaluate whether participants met criteria for pathological gambling.19 This measure has established reliability and validity in diagnosing pathological gambling.
The South Oaks Gambling Screen (SOGS)20 is a reliable and valid screen for problem gambling.21,22 Scores ranged from 0 to 20, with higher scores indicating more severe gambling problems.
The Addiction Severity Index (ASI)23 measured the severity of participants’ medical, employment, gambling, drug and alcohol abuse, legal, family/social, and psychiatric problems in the last 30 days. Composite scores ranged from 0 to 1.0, with higher scores indicating more severe problems. This instrument has established psychometric properties in substance abusers24 and PGs.21,25,26 It was administered before treatment and 8 weeks later (post-treatment), and ASI-Gambling scores were the principal outcome measure in the primary study.18 One hundred and eighty-five participants (80.1%) completed the post-treatment evaluation. No differences in follow-up rates occurred across treatment groups or demographic characteristics, p’s > .14.
The Brief Symptom Inventory (BSI)27 assessed how much discomfort participants experienced with respect to psychiatric symptoms in the past week. Using a scale from 0 to 4, participants indicated how much they were distressed (“not at all” to “extremely”) by 53 items ranging from poor appetite to feelings of hopelessness and guilt. Higher scores indicated a greater level of distress. This instrument demonstrates reliability and validity in assessing the severity of psychiatric and emotional symptoms.28
Random assignment to treatment condition
Participants were randomized to one of three conditions as described in Petry et al.18 Briefly, all participants were referred to Gamblers Anonymous (GA). GA referral was the only intervention for 63 participants, 84 also received a manual containing cognitive-behavioral therapy (CBT) exercises designed to reduce gambling, and 84 received the same CBT but via individual weekly meetings with a therapist; see Petry29 for therapy description. Rates of GA participation did not differ across the three treatment conditions, with 37.3%, 44.0% and 32.5% of those assigned to the GA alone, CBT workbook, and CBT individual therapy conditions, respectively, attending any GA meetings during the 8-week treatment period, X2(2)=2.37, p=.31.
Data analysis
Analysis of variance (ANOVA), Kruskal-Wallis, and chi-square tests evaluated baseline differences among the three groups based upon mental health service utilization. For ASI scores, a multivariate analysis of variance examined group differences in composite scores, controlling for gender. To evaluate the effects of mental health treatment status on gambling outcomes, a repeated measures ANOVA investigated changes over time from baseline to post-treatment on ASI-Gambling scores. Mental health treatment group, treatment condition, and gender were entered as dummy-coded independent variables and ASI-Gambling scores as the dependent variable. The alpha level was 0.05, and all analyses were performed using SPSS.
RESULTS
Table 1 presents demographic characteristics and baseline gambling variables across the three mental health treatment groups. Participants with no, prior, and current mental health treatment were equally likely to be assigned to the three treatment conditions, and no statistically significant differences were noted among the groups in age, race, education, income, or marital status. However, gender and employment status differed significantly across the groups. The no mental health treatment group contained more males than the other two groups. The current mental health treatment group contained fewer full-time employees, and more unemployed and non-labor force participants, in comparison to the other two groups.
TABLE 1.
Demographic Characteristics and Gambling Variables
| No Mental Health Treatment | Past Mental Health Treatment | Current Mental Health Treatment | Test Results | p-Value | |
|---|---|---|---|---|---|
| N | 79 | 81 | 71 | ||
| Age | 42.7±11.9 | 46.3±10.3 | 45.6±9.9 | F(2, 228) = 2.37 | 0.10 |
| Male (%) | 67.1% (53)a | 50.6% (41)b | 46.5% (33)b | X2(2, N = 231) = 7.38 | p < 0.05 |
| Race (%) | |||||
| Caucasian | 86.1% (68) | 84.0% (68) | 83.1% (59) | X2(6, N = 231) = 2.69 | 0.85 |
| African-American | 8.9% (7) | 8.6% (7) | 8.5% (6) | ||
| Hispanic | 2.5% (2) | 3.7% (3) | 7.0% (5) | ||
| Other | 2.5% (2) | 3.7% (3) | 1.4% (1) | ||
| Education completed | 11.9±0.5 | 11.8±0.7 | 11.6±1.0 | F(2, 228) = 2.55 | 0.08 |
| Income (median and interquartile range) | $40,000 (32,000) | $40,000 (41,000) | $30,000 (40,000) | F(2, 228) = 0.92 | 0.40 |
| Marital status (%) | |||||
| Married | 50.6% (40) | 44.4% (36) | 31.0% (22) | X2(6, N = 231) = 10.46 | 0.11 |
| Never married | 29.1% (23) | 22.2% (18) | 29.6% (21) | ||
| Divorced/separated | 15.2% (12) | 29.6% (24) | 33.8% (24) | ||
| Widowed | 5.1% (4) | 3.7% (3) | 5.6% (4) | ||
| Employment status (%) | |||||
| Full-time | 68.4% (54)a | 60.5% (49)a | 39.4% (28)b | X2 (6, N = 231) = 25.37 | p < 0.001 |
| Part-time | 12.7% (10) | 21.0% (17) | 11.3% (8) | ||
| Unemployed | 13.9% (11) | 14.8% (12) | 35.2% (25) | ||
| Not in labor force | 5.1% (4) | 3.7% (3) | 14.1% (10) | ||
| Age when first gambled | 19.9±10.0 | 22.2±12.6 | 19.3±10.3 | F(2, 228) = 1.48 | 0.23 |
| Days gambled in last 30 days (median and interquartile range) | 9.0 (16.0) | 8.0 (10.0) | 9.0 (21.0) | X2(2, N = 231) = 0.87 | 0.65 |
| Amount gambled in last 30 days (median and interquartile range) | $1,500 (3,350) | $1,760 (2,385) | $950 (2,878) | X2(2, N = 231) = 5.40 | 0.07 |
| South Oaks Gambling Screen scores | 12.3±3.2 | 12.9±3.9 | 12.8±3.4 | F(2, 228) = 0.60 | 0.55 |
| Preferred form of gambling (%) | |||||
| Slot machines | 26.6% (21)a | 51.9% (42)b | 46.5% (33)a,b | X2(12, N = 231) = 20.90 | p < 0.05 |
| Cards | 22.8% (18) | 14.8% (12) | 12.7% (9) | ||
| Scratch tickets | 13.9% (11) | 9.9% (8) | 16.9% (12) | ||
| Sports | 15.2% (12) | 3.7% (3) | 7.0% (5) | ||
| Horses/track | 8.9% (7) | 8.6% (7) | 2.8% (2) | ||
| Other | 6.3% (5) | 7.4% (6) | 9.9% (7) | ||
| Craps | 6.3% (5) | 3.7% (3) | 4.2% (3) | ||
| Treatment Condition | |||||
| Gamblers Anonymous | 24.1% (19) | 28.4% (23) | 29.6% (21) | X2(4, N = 231) = 5.25 | 0.26 |
| Gamblers Anonymous and cognitive-behavioral manual | 31.6% (25) | 34.6% (28) | 43.7% (31) | ||
| Gamblers Anonymous and cognitive-behavioral therapy | 44.3% (35) | 37.0% (30) | 26.8% (19) | ||
Values represent means ± standard deviations, unless otherwise noted.
Different superscripts (i.e., a,b) denote groups that differ significantly (p < 0.05) from one another according to post hoc tests. Similar superscripts denote groups that do not differ significantly from one another.
As shown in Table 1, the groups did not differ significantly for the following gambling-related variables: age when first gambled, days and amount gambled in the last 30 days, and SOGS scores. The three groups differed significantly in their preferred forms of gambling, with past mental health treatment participants more likely to report slot machine gambling in comparison to the no mental health treatment participants.
Table 2 presents ASI composite scores across the three groups, which differed significantly, F(16, 438) = 3.56, p < 0.001. Medical, employment, and psychiatric problems differed across the three groups. Current mental health treatment participants demonstrated significantly more severe medical problems than no mental health treatment participants, and they had more severe employment and psychiatric problems than no and past mental health treatment participants. Past mental health treatment participants also had significantly higher ASI psychiatric scores than the no mental health treatment participants.
TABLE 2.
Addiction Severity Index Composite Scores
| No Mental Health Treatment | Past Mental Health Treatment | Current Mental Health Treatment | Test Results | p-Value | |
|---|---|---|---|---|---|
| Medical | 0.25 (0.04)a | 0.33 (0.04)a,b | 0.42 (0.04)b | F(2, 228) = 5.22 | p < 0.01 |
| Employment | 0.21 (0.03)a | 0.20 (0.03)a | 0.36 (0.03)b | F(2, 228) = 9.93 | p < 0.001 |
| Gambling | 0.69 (0.02) | 0.73 (0.02) | 0.71 (0.03) | F(2, 228) = 1.01 | 0.37 |
| Alcohol | 0.09 (0.02) | 0.07 (0.02) | 0.07 (0.02) | F(2, 228) = 0.36 | 0.70 |
| Drug | 0.01 (0.01) | 0.02 (0.01) | 0.02 (0.01) | F(2, 228) = 0.90 | 0.41 |
| Legal | 0.06 (0.02) | 0.07 (0.02) | 0.04 (0.02) | F(2, 228) = 0.59 | 0.56 |
| Family | 0.24 (0.03) | 0.25 (0.03) | 0.31 (0.03) | F(2, 228) = 1.79 | 0.17 |
| Psychiatric | 0.24 (0.02)a | 0.32 (0.02)b | 0.39 (0.02)c | F(2, 228) = 9.98 | p < 0.001 |
Values represent adjusted means and standard errors (in parenthesis).
Different superscripts (i.e., a,b,c) denote groups that differ significantly (p < 0.05) from one another according to post hoc tests. Similar superscripts denote groups that do not differ significantly from one another.
Table 3 presents psychiatric variables drawn from the BSI and ASI. BSI scores differed significantly among the groups, with the no mental health treatment group showing a lower mean BSI score in comparison to the other two groups. As expected, a significantly greater percentage of participants who were currently receiving mental health treatment reported that they were receiving a pension for a psychiatric disability and that they took psychiatric medication in the last 30 days and during their lifetime in comparison to participants in the other two groups. A significantly greater percentage of participants in this group also reported difficulty understanding, concentrating, or remembering in the last 30 days and during their lifetime in comparison to participants in the other two groups. A significantly lower percentage of those in the no mental health treatment group reported serious depression, anxiety, suicidal ideation, and attempted suicide during their lifetime compared to those in the other two groups. However, there were no differences among the three groups with respect to the proportions experiencing significant depression or anxiety in the month before initiating gambling treatment.
TABLE 3.
Psychological Variables
| No Mental Health Treatment | Past Mental Health Treatment | Current Mental Health Treatment | Test Results | p-Value | |
|---|---|---|---|---|---|
| Brief Symptom Inventory scores (mean ± standard deviation) | 0.91±0.68a | 1.17±0.75b | 1.32±0.75b | F(2, 228) = 6.10 | p < 0.01 |
| Currently receiving pension for psychiatric disability | 0.0% (0)a | 3.7% (3)a | 15.5% (11)b | X2(2, N = 231) = 16.98 | p < 0.001 |
| In last 30 days, experienced: | |||||
| Serious depression | 45.6% (36) | 58.0% (47) | 49.3% (35) | X2(2, N = 231) = 2.61 | 0.27 |
| Serious anxiety | 62.0% (49) | 67.9% (55) | 60.6% (43) | X2(2, N = 231) = 1.02 | 0.60 |
| Difficulty understanding, concentrating, or remembering | 26.6% (21)a | 39.5% (32)a | 56.3% (40)b | X2(2, N = 231) = 13.80 | p < 0.001 |
| During lifetime, experienced: | |||||
| Serious depression | 44.3% (35)a | 74.1% (60)b | 85.9% (61)b | X2(2, N = 231) = 31.96 | p < 0.001 |
| Serious anxiety | 54.4% (43)a | 77.8% (63)b | 85.9% (61)b | X2(2, N = 231) = 20.38 | p < 0.001 |
| Difficulty understanding, concentrating, or remembering | 29.1% (23)a | 42.0% (34)a | 64.8% (46)b | X2(2, N = 231) = 19.61 | p < 0.001 |
| Serious suicidal ideation | 19.0% (15)a | 38.3% (31)b | 53.5% (38)b | X2(2, N = 231) = 19.47 | p < 0.001 |
| Suicidal attempt | 6.3% (5)a | 23.5% (19)b | 33.8% (24)b | X2(2, N = 231) = 17.69 | p < 0.001 |
| Took psychiatric medication in the last 30 days | 7.6% (6)a | 21.0% (17)b | 76.1% (54)c | X2(2, N = 231) = 87.42 | p < 0.001 |
| Took psychiatric medication during lifetime | 10.1% (8)a | 63.0% (51)b | 90.1% (64)c | X2(2, N = 231) = 100.90 | p < 0.001 |
Values represent mean percentages and total numbers (N), unless otherwise noted.
Different superscripts (i.e., a,b,c) denote groups that differ significantly (p < 0.05) from one another according to post hoc tests. Similar superscripts denote groups that do not differ significantly from one another.
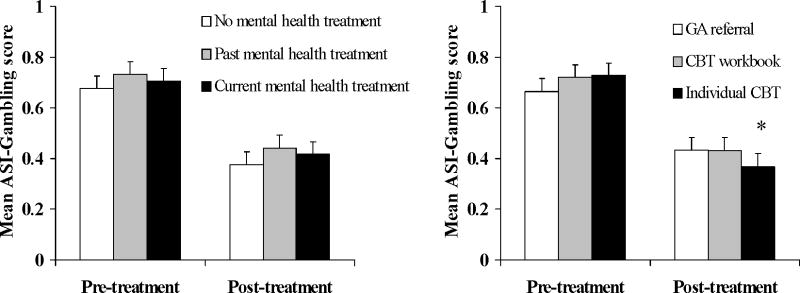
Figure 1 (left panel) shows changes in ASI-Gambling scores over time among participants with no, prior, and current mental health treatment. The mental health treatment status groups did not differ with respect to changes in ASI-Gambling scores over time, F(2, 171) = 0.02, p = 0.98. Consistent with the main study,18 the treatment condition by time effect was significant, F(2, 171) = 3.04, p < 0.05, with individual CBT resulting in the greatest reductions in ASI-Gambling scores over time (Figure 1 right panel). The interaction between treatment condition and mental health status was not significant, F(4, 171) = 0.24, p = 0.91 (data not shown).
FIGURE 1.
Addiction Severity Index-Gambling composite scores pre and post-treatment. The left panel represents data from participants with no (white bars), past (grey bars) or current (black bars) mental health treatment, collapsed across treatment group assignment. The right panel represents data from participants assigned to Gamblers Anonymous (GA) referral alone (white bars), GA referral plus Cognitive-behavioral therapy (CBT) workbook (grey bars), and GA referral plus individual delivered CBT (black bars), collapsed across mental health treatment groups. Values represent means and standard errors. The asterisks indicates a statistically significant treatment condition by time effect, p < .05.
DISCUSSION
In this study, about two-thirds of PGs reported receiving treatment for mental health conditions other than gambling or substance use. Mental health treatment status was associated with other indices of psychiatric distress in the expected manner. Participants with no history of mental health treatment demonstrated the least psychiatric problems, and those reporting current mental health treatment evidenced the most psychiatric problems.
This study also found that mental health treatment status was associated with preferred form of gambling. Past mental health treatment participants were more likely to report slot machine gambling than participants in the other two groups. In a sample of 347 treatment-seeking PGs, Petry30 reported that severity of gambling and psychosocial problems varied by preferred gambling activity, and primary slot machine gamblers were significantly more likely than sports gamblers and card players to evidence psychiatric distress. Although preferred gambling activity was associated with mental health treatment status in this study, severity of gambling problems as assessed by the SOGS, ASI, and gambling frequency and intensity measures did not differ across groups. Thus, treatment-seeking PGs appear to have similar severities of gambling problems regardless of their mental health treatment status.
Consistent with the primary paper,18 individual CBT was efficacious in reducing gambling problems. Furthermore, individual CBT was equally effective across all three mental health status groups. These results suggest PGs are equally likely to benefit from individual CBT, regardless of whether or not they are, or have been, engaged in treatments for other psychiatric disorders. Prior literature has reported inconsistent findings regarding the association of psychiatric problems and response to gambling treatment. Studies have found poorer outcomes16 or no changes17 in outcomes among patients with greater psychiatric problems compared to those with fewer psychiatric concerns. The data from the present study are consistent with the latter study,17 in that patients with greater psychopathology as defined histories of psychiatric treatment or by depression or anxiety symptoms are equally likely to benefit from treatment for their gambling disorder.
Strengths of this study include its large sample size, reasonable follow-up rates, and limited exclusion criteria, increasing the generalizability of findings. As noted in the primary report,18 collaterals (e.g., participants’ friends, family members, etc.) were also contacted to verify self-reported information, and patient and collateral reports of patients’ gambling were highly concordant.
A weakness of the study was that diagnoses for other psychiatric conditions were not systematically conducted. Thus, we cannot distinguish the sample based on other psychiatric diagnoses or reasons for other mental health treatment, or what proportion had diagnoses but never received other mental health treatment. Men, in particular, are less likely to receive psychiatric treatment than women.31 Furthermore, it is unclear whether mental health problems preceded gambling problems among participants, or vice-versa, a temporal sequence that may have impacted treatment-seeking behaviors for other conditions. Findings from this study might also not be generalizable to treatment-seeking PGs in other geographic locations, where access to gambling and/or mental health services may vary and impact treatment-seeking as well as short-and long-term outcomes.
In summary, these data suggest that treatment-seeking PGs who have sought other mental health treatment are more likely to demonstrate psychosocial problems and engage in slot machine gambling than their counterparts who are not seeking mental health treatment. Despite these differences among groups, mental health treatment status does not appear to be associated with gambling treatment outcomes. These findings suggest that individual CBT is effective for PGs with a range of psychiatric problems and treatment histories.
Acknowledgments
Funding for this study and preparation of this report was provided by grants R01-MH60417, R01-DA021567, P30-DA023918, R01-DA016855, R01-DA13444, R01-DA018883, R01-DA022739, R01-DA024667, R01-DA027615, P50-DA09241, and P60-AA03510 from the National Institutes of Health, Bethesda, MD (Dr. Petry).
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Gerstein DR, Volberg RA, Toce MT, et al. Gambling Impact and Behavior Study: Report to the National Gambling Impact Study Commission. Chicago, IL: National Opinion Research Center; 1999. [Google Scholar]
- 3.Kessler RC, Hwang I, LaBrie R, et al. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychol Med. 2008;38:1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- 5.Welte J, Barnes G, Wieczorek W, Tidwell MC, Parker J. Alcohol and gambling pathology among U.S. adults: prevalence, demographic patterns and comorbidity. J Stud Alcohol. 2001;62:706–712. doi: 10.15288/jsa.2001.62.706. [DOI] [PubMed] [Google Scholar]
- 6.Morasco BJ, Pietrzak RH, Blanco C, Grant BF, Hasin D, Petry NM. Health problems and medical utilization associated with gambling disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2006;68:976–984. doi: 10.1097/01.psy.0000238466.76172.cd. [DOI] [PubMed] [Google Scholar]
- 7.Shaffer HJ, Korn DA. Gambling and related mental disorders: a public health analysis. Annu Rev Public Health. 2002;23:171–212. doi: 10.1146/annurev.publhealth.23.100901.140532. [DOI] [PubMed] [Google Scholar]
- 8.Bland RC, Newman SC, Orn H, Stebelsky G. Epidemiology of pathological gambling in Edmonton. Can J Psychiatry. 1993;38:108–112. doi: 10.1177/070674379303800207. [DOI] [PubMed] [Google Scholar]
- 9.Kerber CS, Black DW, Buckwalter K. Comorbid psychiatric disorders among older adult recovering pathological gamblers. Issues Ment Health Nurs. 2008;29:1018–1028. doi: 10.1080/01612840802274933. [DOI] [PubMed] [Google Scholar]
- 10.Ibáñez A, Blanco C, Donahue E, et al. Psychiatric comorbidity in pathological gamblers seeking treatment. Am J Psychiatry. 2001;158:1733–1735. doi: 10.1176/ajp.158.10.1733. [DOI] [PubMed] [Google Scholar]
- 11.Pietrzak RH, Petry NM. Antisocial personality disorder is associated with increased severity of gambling, medical, drug, and psychiatric problems among treatment-seeking pathological gamblers. Addiction. 2005;100:1183–1193. doi: 10.1111/j.1360-0443.2005.01151.x. [DOI] [PubMed] [Google Scholar]
- 12.Maccallum F, Blaszczynski A. Pathological gambling and comorbid substance use. Aust N Z J Psychiatry. 2002;36:411–415. doi: 10.1046/j.1440-1614.2001.01005.x. [DOI] [PubMed] [Google Scholar]
- 13.Stinchfield R, Winters KC. Outcome of Minnesota’s gambling treatment programs. J Gambl Stud. 2001;17:217–245. doi: 10.1023/a:1012268322509. [DOI] [PubMed] [Google Scholar]
- 14.Ladd GT, Petry NM. A comparison of pathological gamblers with and without substance abuse treatment histories. Exp Clin Psychopharmacol. 2003;11:202–209. doi: 10.1037/1064-1297.11.3.202. [DOI] [PubMed] [Google Scholar]
- 15.Stinchfield R, Kushner MG, Winters KC. Alcohol use and prior substance abuse treatment in relation to gambling problem severity and gambling treatment outcome. J Gambl Stud. 2005;21:273–297. doi: 10.1007/s10899-005-3100-1. [DOI] [PubMed] [Google Scholar]
- 16.Echeburúa E, Fernández-Montalvo J, Báez C. Predictors of therapeutic failure in slot-machine pathological gamblers following behavioural treatment. Behav Cogn Psychother. 2001;29:379–383. [Google Scholar]
- 17.Leblond J, Ladouceur R, Blaszczynski A. Which pathological gamblers will complete treatment? Br J Clin Psychol. 2003;42:205–209. doi: 10.1348/014466503321903607. [DOI] [PubMed] [Google Scholar]
- 18.Petry NM, Ammerman Y, Bohl J, et al. Cognitive-behavioral therapy for pathological gamblers. J Consult Clin Psychol. 2006;74:555–567. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- 19.Grant JE, Steinberg MA, Kim SW, Rounsaville BJ, Potenza MN. Preliminary validity and reliability testing of a structured clinical interview for pathological gambling. Psychiatry Res. 2004;128:78–88. doi: 10.1016/j.psychres.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): a new instrument for the identification of pathological gamblers. Am J Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- 21.Petry NM. Concurrent and predictive validity of the Addiction Severity Index in pathological gamblers. Am J Addict. 2007;16:272–282. doi: 10.1080/10550490701389849. [DOI] [PubMed] [Google Scholar]
- 22.Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks Gambling Screen (SOGS) Addict Behav. 2002;27:1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- 23.McLellan AT, Luborsky L, Cacciola J, et al. New data from the Addiction Severity Index: reliability and validity in three centers. J Nerv Ment Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 24.McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The Addiction Severity Index at 25: origins, contributions and transitions. Am J Addict. 2006;15:113–124. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 25.Lesieur HR, Blume SB. Modifying the Addiction Severity Index for use with pathological gamblers. Am J Addict. 1992;1:240–247. [Google Scholar]
- 26.Petry NM. Validity of a gambling scale for the Addiction Severity Index. J Nerv Ment Dis. 2003;191:399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- 27.Derogatis LR. Brief Symptom Inventory. Baltimore, MD: Clinical Psychometric Research; 1993. [Google Scholar]
- 28.Morlan KK, Tan SY. Comparison of the Brief Psychiatric Rating Scale and the Brief Symptom Inventory. J Clin Psychol. 1998;54:885–894. doi: 10.1002/(sici)1097-4679(199811)54:7<885::aid-jclp3>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 29.Petry NM. Gamblers anonymous and cognitive-behavioral therapies for pathological gamblers. J Gambl Stud. 2005;21:27–33. doi: 10.1007/s10899-004-1919-5. [DOI] [PubMed] [Google Scholar]
- 30.Petry NM. A comparison of treatment-seeking pathological gamblers based on preferred gambling activity. Addiction. 2003;98:645–655. doi: 10.1046/j.1360-0443.2003.00336.x. [DOI] [PubMed] [Google Scholar]
- 31.Wang PS, Lane M, Olfson M, et al. Twelve month use of mental health services in the United States. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]