Abstract
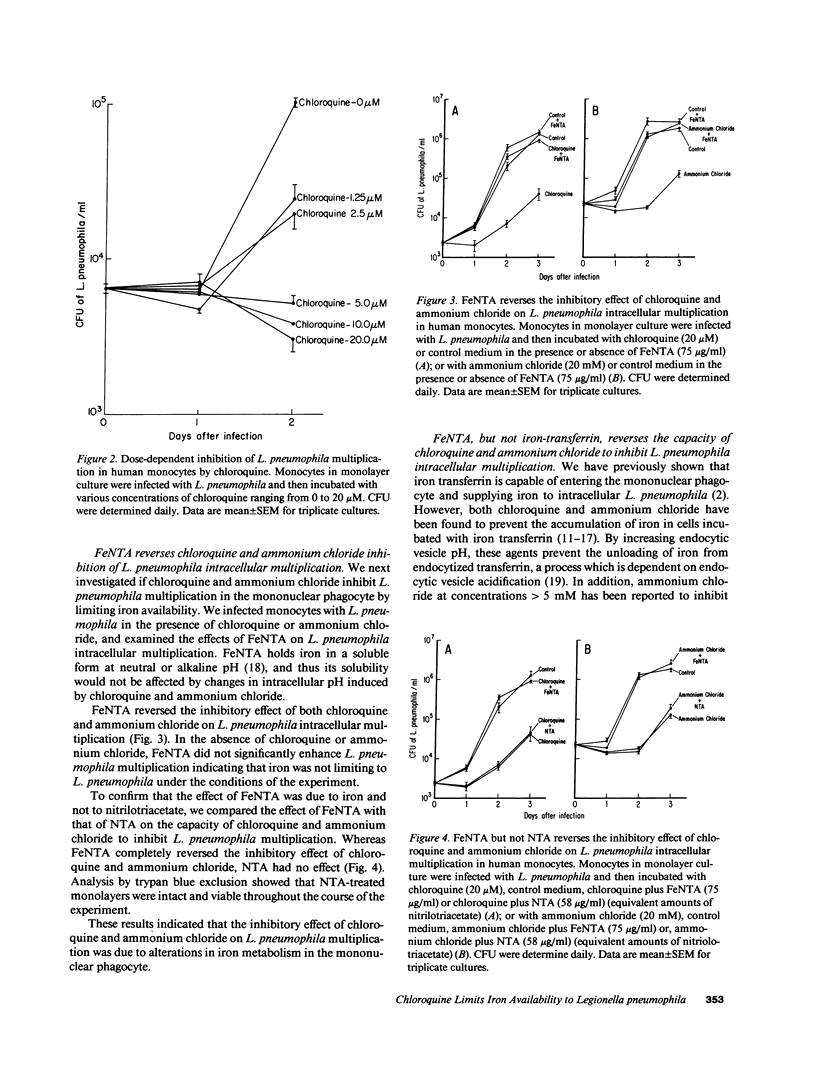
Chloroquine and ammonium chloride, by virtue of their basic properties, have been shown to raise endocytic and lysosomal pH and thereby interfere with normal iron metabolism in a variety of cell types, including mononuclear phagocytes. Cellular iron metabolism is of critical importance to Legionella pneumophila, an intracellular bacterial pathogen whose capacity to multiply in human mononuclear phagocytes is dependent upon the availability of intracellular iron. In view of this, we have studied the effects of chloroquine and ammonium chloride on L. pneumophila intracellular multiplication in human monocytes. Chloroquine, at a concentration of 20 microM, and ammonium chloride, at a concentration of 20 mM, inhibited L. pneumophila intracellular multiplication by 1.4 +/- 0.2 (SEM) logs and 1.5 +/- 0.2 logs, respectively. Chloroquine- and ammonium chloride-induced inhibition of L. pneumophila intracellular multiplication was completely reversed by iron nitrilotriacetate, an iron compound which is soluble in the neutral to alkaline pH range, but not by iron transferrin, which depends upon acidic intracellular conditions to release iron. Chloroquine had no major direct effect on L. pneumophila multiplication in artificial media except at extremely high concentrations (15,000-fold that which inhibited L. pneumophila multiplication in mononuclear phagocytes), and inhibition at such concentrations was not reversed by iron nitrilotriacetate. This study demonstrates that chloroquine and ammonium chloride inhibit the intracellular multiplication of L. pneumophila by limiting the availability of iron to the bacterium. It is possible that such a mechanism of action underlies chloroquine's antimicrobial effect against other intracellular pathogens, such as the agents of malaria and tuberculosis.
Full text
PDF





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armstrong N. J., Morgan E. H. The effect of lysosomotrophic bases and inhibitors of transglutaminase on iron uptake by immature erythroid cells. Biochim Biophys Acta. 1983 Apr 5;762(2):175–186. doi: 10.1016/0167-4889(83)90069-1. [DOI] [PubMed] [Google Scholar]
- Bates G. W., Wernicke J. The kinetics and mechanism of iron(3) exchange between chelates and transferrin. IV. The reaction of transferrin with iron(3) nitrilotriacetate. J Biol Chem. 1971 Jun 10;246(11):3679–3685. [PubMed] [Google Scholar]
- Baynes R., Bukofzer G., Bothwell T., Bezwoda W., Macfarlane B. Transferrin receptors and transferrin iron uptake by cultured human blood monocytes. Eur J Cell Biol. 1987 Jun;43(3):372–376. [PubMed] [Google Scholar]
- Byrd T. F., Horwitz M. A. Interferon gamma-activated human monocytes downregulate transferrin receptors and inhibit the intracellular multiplication of Legionella pneumophila by limiting the availability of iron. J Clin Invest. 1989 May;83(5):1457–1465. doi: 10.1172/JCI114038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciak J., Hahn F. E. Chloroquine: mode of action. Science. 1966 Jan 21;151(3708):347–349. doi: 10.1126/science.151.3708.347. [DOI] [PubMed] [Google Scholar]
- Dautry-Varsat A., Ciechanover A., Lodish H. F. pH and the recycling of transferrin during receptor-mediated endocytosis. Proc Natl Acad Sci U S A. 1983 Apr;80(8):2258–2262. doi: 10.1073/pnas.80.8.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haldar K., Henderson C. L., Cross G. A. Identification of the parasite transferrin receptor of Plasmodium falciparum-infected erythrocytes and its acylation via 1,2-diacyl-sn-glycerol. Proc Natl Acad Sci U S A. 1986 Nov;83(22):8565–8569. doi: 10.1073/pnas.83.22.8565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershko C., Peto T. E. Deferoxamine inhibition of malaria is independent of host iron status. J Exp Med. 1988 Jul 1;168(1):375–387. doi: 10.1084/jem.168.1.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz M. A., Silverstein S. C. Legionnaires' disease bacterium (Legionella pneumophila) multiples intracellularly in human monocytes. J Clin Invest. 1980 Sep;66(3):441–450. doi: 10.1172/JCI109874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacopetta B. J., Morgan E. H. The kinetics of transferrin endocytosis and iron uptake from transferrin in rabbit reticulocytes. J Biol Chem. 1983 Aug 10;258(15):9108–9115. [PubMed] [Google Scholar]
- Jacobs A. Low molecular weight intracellular iron transport compounds. Blood. 1977 Sep;50(3):433–439. [PubMed] [Google Scholar]
- Karin M., Mintz B. Receptor-mediated endocytosis of transferrin in developmentally totipotent mouse teratocarcinoma stem cells. J Biol Chem. 1981 Apr 10;256(7):3245–3252. [PubMed] [Google Scholar]
- Krogstad D. J., Schlesinger P. H. A perspective on antimalarial action: effects of weak bases on Plasmodium falciparum. Biochem Pharmacol. 1986 Feb 15;35(4):547–552. doi: 10.1016/0006-2952(86)90345-x. [DOI] [PubMed] [Google Scholar]
- Krogstad D. J., Schlesinger P. H. Acid-vesicle function, intracellular pathogens, and the action of chloroquine against Plasmodium falciparum. N Engl J Med. 1987 Aug 27;317(9):542–549. doi: 10.1056/NEJM198708273170905. [DOI] [PubMed] [Google Scholar]
- Krogstad D. J., Schlesinger P. H., Gluzman I. Y. Antimalarials increase vesicle pH in Plasmodium falciparum. J Cell Biol. 1985 Dec;101(6):2302–2309. doi: 10.1083/jcb.101.6.2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krogstad D. J., Schlesinger P. H. The basis of antimalarial action: non-weak base effects of chloroquine on acid vesicle pH. Am J Trop Med Hyg. 1987 Mar;36(2):213–220. doi: 10.4269/ajtmh.1987.36.213. [DOI] [PubMed] [Google Scholar]
- Laub R., Schneider Y. J., Octave J. N., Trouet A., Crichton R. R. Cellular pharmacology of deferrioxamine B and derivatives in cultured rat hepatocytes in relation to iron mobilization. Biochem Pharmacol. 1985 Apr 15;34(8):1175–1183. doi: 10.1016/0006-2952(85)90492-7. [DOI] [PubMed] [Google Scholar]
- Lestas A. N. The effect of pH upon human transferrin: selective labelling of the two iron-binding sites. Br J Haematol. 1976 Mar;32(3):341–350. doi: 10.1111/j.1365-2141.1976.tb00937.x. [DOI] [PubMed] [Google Scholar]
- Mackenzie A. H. Pharmacologic actions of 4-aminoquinoline compounds. Am J Med. 1983 Jul 18;75(1A):5–10. doi: 10.1016/0002-9343(83)91264-0. [DOI] [PubMed] [Google Scholar]
- Maxfield F. R. Weak bases and ionophores rapidly and reversibly raise the pH of endocytic vesicles in cultured mouse fibroblasts. J Cell Biol. 1982 Nov;95(2 Pt 1):676–681. doi: 10.1083/jcb.95.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Octave J. N., Schneider Y. J., Hoffmann P., Trouet A., Crichton R. R. Transferrin protein and iron uptake by cultured rat fibroblasts. FEBS Lett. 1979 Dec 1;108(1):127–130. doi: 10.1016/0014-5793(79)81193-x. [DOI] [PubMed] [Google Scholar]
- Peto T. E., Thompson J. L. A reappraisal of the effects of iron and desferrioxamine on the growth of Plasmodium falciparum 'in vitro': the unimportance of serum iron. Br J Haematol. 1986 Jun;63(2):273–280. doi: 10.1111/j.1365-2141.1986.tb05550.x. [DOI] [PubMed] [Google Scholar]
- Pollack S., Fleming J. Plasmodium falciparum takes up iron from transferrin. Br J Haematol. 1984 Oct;58(2):289–293. doi: 10.1111/j.1365-2141.1984.tb06087.x. [DOI] [PubMed] [Google Scholar]
- Poole B., Ohkuma S. Effect of weak bases on the intralysosomal pH in mouse peritoneal macrophages. J Cell Biol. 1981 Sep;90(3):665–669. doi: 10.1083/jcb.90.3.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Princiotto J. V., Zapolski E. J. Difference between the two iron-binding sites of transferrin. Nature. 1975 May 1;255(5503):87–88. doi: 10.1038/255087a0. [DOI] [PubMed] [Google Scholar]
- Raventos-Suarez C., Pollack S., Nagel R. L. Plasmodium falciparum: inhibition of in vitro growth by desferrioxamine. Am J Trop Med Hyg. 1982 Sep;31(5):919–922. doi: 10.4269/ajtmh.1982.31.919. [DOI] [PubMed] [Google Scholar]
- Rodriguez M. H., Jungery M. A protein on Plasmodium falciparum-infected erythrocytes functions as a transferrin receptor. 1986 Nov 27-Dec 3Nature. 324(6095):388–391. doi: 10.1038/324388a0. [DOI] [PubMed] [Google Scholar]
- Sibille J. C., Kondo H., Aisen P. Uptake of ferritin and iron bound to ferritin by rat hepatocytes: modulation by apotransferrin, iron chelators and chloroquine. Biochim Biophys Acta. 1989 Feb 9;1010(2):204–209. doi: 10.1016/0167-4889(89)90162-6. [DOI] [PubMed] [Google Scholar]
- Starke P. E., Gilbertson J. D., Farber J. L. Lysosomal origin of the ferric iron required for cell killing by hydrogen peroxide. Biochem Biophys Res Commun. 1985 Dec 17;133(2):371–379. doi: 10.1016/0006-291x(85)90916-7. [DOI] [PubMed] [Google Scholar]
- Swaiman K. F., Machen V. L. Chloroquine reduces neuronal and glial iron uptake. J Neurochem. 1986 Feb;46(2):652–654. doi: 10.1111/j.1471-4159.1986.tb13017.x. [DOI] [PubMed] [Google Scholar]
- Wollheim F. A., Hanson A., Laurell C. B. Chloroquine treatment in rheumatoid arthritis. Correlation of clinical response to plasma protein changes and chloroquine levels. Scand J Rheumatol. 1978;7(3):171–176. doi: 10.3109/03009747809095649. [DOI] [PubMed] [Google Scholar]
- Zhang Y. Inhibition of hemoglobin degradation in Plasmodium falciparum by chloroquine and ammonium chloride. Exp Parasitol. 1987 Dec;64(3):322–327. doi: 10.1016/0014-4894(87)90042-7. [DOI] [PubMed] [Google Scholar]



