Abstract
Human immunodeficiency virus type 1 (HIV-1) isolates from 20 chronically infected patients who participated in a structured treatment interruption (STI) trial were studied to determine whether viral fitness influences reestablishment of viremia. Viruses derived from individuals who spontaneously controlled viremia had significantly lower in vitro replication capacities than viruses derived from individuals that did not control viremia after interruption of antiretroviral therapy (ART), and replication capacities correlated with pre-ART and post-STI viral set points. Of note, no clinically relevant improvement of viral loads upon STI occurred. Virus isolates from controlling and noncontrolling patients were indistinguishable in terms of coreceptor usage, genetic subtype, and sensitivity to neutralizing antibodies. In contrast, viruses from controlling patients exhibited increased sensitivity to inhibition by chemokines. Sensitivity to inhibition by RANTES correlated strongly with slower replication kinetics of the virus isolates, suggesting a marked dependency of these virus isolates on high coreceptor densities on the target cells. In summary, our data indicate that viral fitness is a driving factor in determining the magnitude of viral rebound and viral set point in chronic HIV-1 infection, and thus fitness should be considered as a parameter influencing the outcome of therapeutic intervention in chronic infection.
The level of human immunodeficiency virus type 1 (HIV-1) viremia that patients reach and maintain after the acute infection phase predicts disease progression (26). This steady-state level of plasma viral load (VL) is referred to as viral set point and can vary more than 1,000-fold between individuals (35). Viral set points are a consequence of the interplay of viral, immunological, and host genetic factors (8, 36), including maintenance and specificity of anti-HIV CD4 and CD8 T-cell responses (2), neutralizing antibodies (33), target cell availability (13), genetic polymorphisms of the viral coreceptors, and the HLA type (38).
Likewise, biological properties of HIV-1, namely, tropism, cytopathicity, and replication rate, are relevant parameters in AIDS pathogenesis. The switch in coreceptor usage from CCR5 to CXCR4, which occurs in approximately 50% of patients, is associated with more-vigorous viral replication and rapid disease progression (5, 6, 12, 20, 40). In recent years, investigations of viral features have shifted to evaluation of overall viral fitness (36). Viral fitness reflects the aptitude of a viral isolate to replicate in a given host system and is a consequence of the capacity of the virus to efficiently enter and infect target cells and to establish and spread the infection (8, 36). The efficacy of this process is further influenced by the availability of target cells, adaptive and innate immune responses, genetic host factors, and antivirals. Estimation of viral fitness has gained particular interest in the investigation of viral strains with drug resistance mutations, since these mutations are frequently accompanied by a loss of replicative capacity (7, 14, 24, 36). The outcome of the Swiss-Spanish intermittent treatment trial (SSITT) with 133 chronically infected patients was previously reported(15, 29-31). No clinically relevant impact of structured treatment interruption (STI) on improvement of viremia control was found. A boost of cytotoxic T lymphocyte and T helper responses occurred in most patients but did not correlate with viremia control (15, 31). In total, 17% of the SSITT patients potently suppressed VLs to levels below 5,000 RNA copies/ml without treatment after completion of the trial. However, as observed in similar studies (18), these patients had significantly lower viral set points before the initial onset of antiretroviral therapy (ART). No further decrease in their VLs upon STI was found (15). This result indicates strongly that preexisting viral and immune properties determined the outcome of this STI trial. Here we investigate the impact of fitness and intrinsic biological properties of the patient viruses on the extent of viremia rebound and the manifestation of viral set point during STI in a subgroup of 20 patients participating in the SSITT.
MATERIALS AND METHODS
Patients.
Twenty chronically infected patients (Table 1) participating in the SSITT (15) at the University Hospital Zurich, Zurich, Switzerland, were studied. Patients underwent four consecutive STI cycles (2 weeks off and 8 weeks on treatment) followed by a fifth long treatment interruption (a minimum of 12 weeks off treatment if no adverse effects occurred). Patients had never experienced drug failure and had undetectable VLs (<50 RNA copies/ml) for ≥6 months. Detailed descriptions of the respective clinical trial and patient characteristics have been reported elsewhere (15, 30). Written informed consent was obtained from all patients according to the guidelines of the University Hospital Zurich.
TABLE 1.
Patient and virus characteristics
| Patient | Age (yrs) | Gendera | Characteristics before ART
|
Baseline data for STI trial
|
Post-STI characteristics
|
Autologous virus characteristics
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amt of time (mos) HIV-1 positive | Clinical stage | No. of RNA copies/ml | ARTb | Mos at VL of <50 copies/ml | No. of CD4 cells/mm3 | No. of RNA copies/ml | No. of CD4 cells/mm3 | Coreceptorc
|
HIV subtype | ||||
| First cycle | Fifth cycle | ||||||||||||
| Controlling group | |||||||||||||
| 106 | 39 | M | >24 | A | 402 | AZT, 3TC | 36 | 878 | 5,128 | 650 | ND | R5 | B |
| 107 | 44 | F | >24 | A | 5,216 | AZT, 3TC, NFV | 25 | 544 | 2,551 | 537 | ND | R5 | B |
| 112 | 46 | M | 6-12 | A | 32,140 | AZT, 3TC, IDV | 25 | 347 | 6,866 | 431 | ND | R5 | B |
| 117 | 33 | F | 12-24 | A | 29,344 | AZT, 3TC, RTV | 36 | 489 | 13,007 | 341 | ND | R5 | B |
| 118 | 33 | M | 12-24 | A | 16,927 | AZT, 3TC, IDV | 30 | 832 | 3,099 | 785 | R5 | R5 | B |
| 125 | 35 | F | >24 | A | 11,298 | ddI, d4T, NFV | 23 | 777 | 4,873 | 882 | R5 | R5 | E/CRF1 |
| 130 | 66 | M | 6-12 | A | 537 | AZT, 3TC, NFV | 30 | 829 | 107 | 729 | ND | R5 | A |
| Noncontrolling group | |||||||||||||
| 102 | 40 | M | >24 | C | 561,831 | AZT, 3TC, IDV | 32 | 723 | 76,805 | 491 | R5 | R5 | B |
| 109 | 38 | M | >24 | B | 34,752 | AZT, 3TC, RTV | 31 | 1115 | 148,191 | 806 | R5 | R5 | B |
| 111 | 38 | M | >24 | A | 122,729 | ddI, d4T, NFV | 11 | 422 | 22,030 | 362 | R5 | R5 | B |
| 113 | 59 | M | 12-24 | A | 107,303 | AZT, 3TC, RTV | 20 | 995 | 34,110 | 792 | ND | R5 | B |
| 114 | 32 | M | >24 | A | 9,276 | AZT, 3TC, RTV | 29 | 907 | 28,478 | 784 | ND | R5 | B |
| 116 | 53 | M | >24 | C | 467,593 | AZT, 3TC, IDV | 32 | 350 | 31,500 | 202 | R5×4 | R5×4 | B |
| 119 | 35 | M | 12-24 | A | 113,052 | d4T, 3TC, SQV, RTV | 12 | 440 | 99,274 | 394 | ND | R5 | B |
| 120 | 55 | M | 12-24 | A | 150,390 | AZT, 3TC, IDV | 28 | 766 | 38,252 | 511 | R5 | R5 | B |
| 121 | 38 | M | 3-6 | A | 164,772 | d4T, 3TC, NFV | 12 | 591 | 67,321 | 380 | R5 | R5 | B |
| 122 | 40 | M | >24 | A | 13,317 | AZT, 3TC, IDV | 30 | 669 | 24,982 | 481 | ND | R5 | B |
| 126 | 49 | M | >24 | A | 63,698 | AZT, 3TC, RTV | 34 | 842 | 19,782 | 441 | ND | R5 | B |
| 127 | 52 | F | >24 | A | 25,417 | d4T, 3TC, NFV | 22 | 839 | 106,923 | 614 | R5 | R5 | B |
| 128 | 43 | F | >24 | A | 9,404 | AZT, ddI, NFV | 25 | 749 | 20,236 | 949 | R5 | R5 | B |
M, male; F, female.
AZT, zidovudine; 3TC, lamivudine; NFV, nelfinavir; IDV, indinavir; RTV, ritonavir; ddI, dideoxyinosine; d4T, stavudine; SQV, saquinavir.
ND, not determined.
Quantification of plasma VL.
Plasma HIV RNA was quantified by using the Amplicor HIV-1 Monitor test, version 1.5 (Roche Diagnostics, Rotkreuz, Switzerland) with a detection limit of <50 copies/ml (30).
Genotypic analysis.
Peripheral blood mononuclear cell (PBMC) DNA from participants was genotyped at CCR5 G-2455A, CCR5 delta 32, RANTES G-403A, RANTES C-28G, macrophage inflammatory protein 1α (MIP-1α), T113C, and SDF-1 3′A genes by using TaqMan allelic discrimination techniques (Applied Biosystems). The contribution of the various alleles to HIV-1 susceptibility has been described elsewhere (41). Determination of HLA genotypes was performed as described previously (9).
Stimulated primary CD4+ T cells.
Buffy coats obtained from three healthy blood donors were depleted of CD8+ T cells by using Rosette Sep cocktail (StemCell Technologies Inc.), and PBMCs were isolated by Ficoll-Hypaque centrifugation. Cell concentrations were adjusted to 4 × 106 per ml in culture medium (RPMI 1640, 10% fetal calf serum, 100 U of interleukin-2/ml, glutamine, and antibiotics), and cell samples were divided into three parts and stimulated with either 5 μg of phytohemagglutinin/ml, 0.5 μg of phytohemagglutinin/ml, or anti-CD3 monoclonal antibody (MAb) OKT3. After 72 h, cells from all three stimulations were combined and used as the source of stimulated CD4+ T cells for infection and virus isolation experiments.
Autologous patient viruses.
Autologous virus was isolated from patient PBMCs during the first interruption cycle (week 2 of the trial) and the beginning of the fifth interruption cycle (weeks 42 to 50) by coculturing patient CD4+ T cells with stimulated PBMCs (49). The 50% tissue culture infectious dose and coreceptor usage of the obtained virus stocks were determined as described previously (4, 43, 44).
In vitro replicative capacity.
Virus inoculum (100 50% tissue culture infectious doses in 50 μl) was added to 12 replicate wells of a 96-well culture plate containing 2 × 105 stimulated PBMCs in 150 μl of culture medium. Culture supernatant was assayed for p24 antigen on days 4, 6, 10, and 14 postinfection (p.i.) by using an in-house p24 antigen enzyme-linked immunosorbent assay as described previously (27, 46). As the virus inoculum was not washed out at any stage of the experiment, the residual input p24 concentration was measured and subtracted from all test results. Cultures were fed 100 μl of medium on days 6 and 10 p.i.
Inhibition by chemokines.
Inhibition of infection by chemokines was assessed on stimulated CD8-depleted PBMCs (45). The calculated inhibitory doses refer to the final concentrations of chemokines in the cultures on day 0. Virus production in the absence of chemokines was designated as 100%, and the ratios of p24 antigen production in chemokine-containing cultures were calculated relative to this value. The chemokine concentrations (in nanograms per milliliter) causing 50, 70, and 90% reduction in p24 antigen production (50, 70, and 90% inhibitory doses) were determined by linear regression analysis. If the appropriate degree of inhibition was not achieved at the highest or lowest chemokine concentration, a value of more than or less than was recorded and these upper or lower limits were used for statistical analysis.
Neutralization assay.
Neutralization activity was evaluated as described previously (4, 44). MAbs 2F5 (28) and 2G12 (47) were gifts from H. Katinger, MAb IgG1b12 (3) was from D. Burton, and the CD4-immunoglobulin CD4-IgG2 molecule was from P. Maddon (1). Briefly, virus inoculum was incubated with serial dilutions of antibodies for 1 h at 37°C. Then stimulated PBMCs were infected with aliquots of this preincubation mixture. Three days postinfection, cultures were washed three times and supplemented with fresh medium and fresh stimulated PBMCs. Cultures were incubated for 6 to10 days and assayed for p24 antigen. Calculation of inhibitory doses was as described above.
Data analysis.
For each patient, the following viral life history parameters were calculated.
(i) Pre-ART VL.
The pretreatment VL corresponds to the last plasma HIV RNA value recorded before ART or, if two measurements within 6 months before initiation of ART were available, to the geometric mean of those levels.
(ii) Post-STI VL.
The post-STI VL value reflects the viral set point, i.e., the plateau of viremia post-STI, and was determined as the geometric mean of plasma HIV RNA levels measured after week 40, when a steady state was reached (usually between weeks 46 and 64). Three patients (patients 102, 109, and 116) had plateau VLs calculated from the two or three time points just prior to the restart of therapy. For two patients (patients 107 and 130), the week 46 data point was part of a peak and was therefore omitted from the estimation of the plateau. For the 17 patients who remained off therapy for extended periods, an average of 9.06 data points (range, 6 to 12) was used to calculate the plateau VLs.
(iii) Control of viremia.
Patients were classified into a controlling group and a noncontrolling group according to their abilities to control viremia in the absence of ART between weeks 40 and 76. Control of viremia was defined as maintenance of a VL of <5,000 RNA copies/ml for at least 8 weeks during this time period. The cutoff of 5,000 RNA copies/ml was set in the SSITT trial as a value above which patients had to reinitiate ART (15).
(iv) Improvement of viral set point.
For differences between pre-ART VLs and post-STI VLs, positive values indicate decreases (improvement) in VLs and negative values indicate increases. A decrease in VL of 0.5 logs is considered to be a significant change.
(v) Cumulative VL.
The total amount of virus produced during the individual cycles was estimated by calculating the area under the curve (AUC). The AUC between successive time points was calculated using the following formula: AUC = (VL2 − VL1) × (T2 − T1)/ln(VL2/VL1), where 1 and 2 indicate values at first and second time points and time T is measured in days after start of therapy. The total AUC is determined by adding the AUCs between successive time points. Since for some patients RNA levels at weeks 10, 20, 30, and 40 were not available, AUC values for all patients from these time points were derived from RNA levels at weeks 2, 9, 12, 19, 22, 29, 32, and 39 by extrapolation: e.g., VL at week 10 (VLwk10) = VLwk9 × exp{[ln(VLwk9) − ln(VLwk2)]/[(T at week 9) − (T at week 2)] × 7}. When a given VL was undetectable, the limit of detection was used as the anchor for the extrapolation.
(vi) In vitro replication capacity (slope between values from days 0 and 6).
Slopes were calculated by performing linear regression analysis using the natural logarithm of p24 antigen values obtained on days 0, 4, and 6 p.i.
Statistical analyses.
Statistical analyses were performed using GraphPad Prism version 4.0 (GraphPad Software Inc., San Diego, Calif.). Patient groups were compared by using nonparametric (Mann-Whitney) tests unless stated otherwise.
RESULTS
Phenotypic and genotypic evaluation of autologous patient isolates.
Twenty patients participating in the SSITT were studied to determine the impact of intrinsic patient virus characteristics and overall viral fitness on the level of viremia rebound and manifestation of viral set point upon STI. Patients were classified into controlling and noncontrolling groups according to their abilities to control viremia in the absence of drugs after STI (Table 1). The controlling and noncontrolling groups differed significantly in their pretreatment VLs (P = 0.016) and their post-STI VL plateaus (P = 0.0004), but no difference in the abilities to improve VLs upon STI was observed (see also reference 15). Thus, potent control of viremia upon STI was not a consequence of treatment interruptions but correlated strongly with pre-ART VLs.
Virus isolates from patient PBMCs were collected during the first interruption cycle (week 2 of the trial) and the fifth interruption cycle (weeks 42 to 50). Isolation of virus during the first cycle was not possible in all cases because some patients had no or extremely low viral rebound during this cycle. Altogether, 10 first-cycle and 20 fifth-cycle virus isolates were obtained (Table 1). With one exception (patient 116), all patients were infected with R5 virus isolates both during the first STI and after completion of the STI (Table 1). The isolate from patient 116 utilized CCR5 and CXCR4 before and after the STI. Thus, viremia control in these patients was not determined by a specific viral tropism nor did we find evidence that STI provoked changes in coreceptor utilization patterns. Equally, the distribution of HIV subtypes among patients does not suggest that spontaneous control of plasma viremia was influenced by the genetic subtype (Table 1).
In vitro replicative capacity.
To compare the efficacies of patient isolates in infection of target cells, we evaluated their in vitro replication capacities on stimulated primary CD4+ T cells. In order to allow interisolate comparisons, infection experiments for all isolates were performed on the same day by using the same target cells from healthy donors, which eliminates possible distortion of the results by donor cell variability. For the assessment of the viral replication capacity, the absolute amount of viral antigen generated was taken as a measure of viral productiveness. Therefore, this analysis relies on the assumption that the p24 antigens from all isolates are detected equally well by the p24 antigen detection system used. In fact, all virus isolates were readily detectable by our p24 antigen enzyme-linked immunosorbent assay, irrespective of their genetic subtypes (data not shown). A range of methods have been developed with the aim of evaluating viral fitness or the contribution of specific viral genes to the overall replicative capacities of viral variants (36). The strength but also the limitations of the assay used in our studies lie in the use of replication-competent patient isolates and primary cells as target cells. This allowed us to investigate the influences of all viral genes on replication in the natural target cells in order to get an initial estimate of the relative fitness levels of the diverse patient isolates. Although useful for the analysis described here, exact measurements of the relative contributions of specific viral genes are not possible with this method.
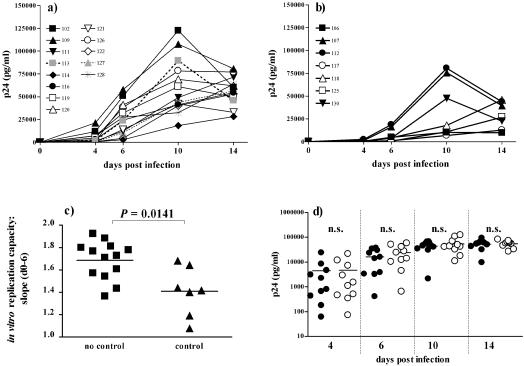
We observed a striking difference between the cultures infected with virus isolates from the controlling and noncontrolling groups in both the amount of p24 antigen produced and the timing of production (Fig. 1a and b). The levels of p24 antigen generated by days 4 and 6 p.i. were significantly lower in the controlling group (P = 0.0216 and 0.0175, respectively). In the majority of cultures in both groups, the peak of infection was reached by day 10 p.i. and virus production decreased thereafter.
FIG. 1.
In vitro replication kinetics of patient isolates. (a and b) Profile of p24 antigen production in cultures of CD8-depleted PBMCs infected with isolates derived during the fifth cycle from patients in the noncontrolling group (a) and the controlling group (b). (c) In vitro replication capacities. Slopes of viral antigen production between days 0 and 6 [slope (d0-6)] were calculated by performing linear regression analysis using the natural logarithm of p24 antigen values obtained on days 0, 4, and 6 p.i. Slopes for viruses from controlling (triangles) and noncontrolling (squares) patients were compared using the Mann-Whitney test. Data are means of results from two independent experiments. (d) The extent of viral replication of first-cycle and fifth-cycle virus pairs from eight patients of the noncontrolling group and two patients of the controlling group on CD8-depleted PBMCs is depicted as p24 antigen production on days 4, 6, 10, and 14 p.i. Antigen production levels of first-cycle (closed circles) and fifth-cycle (open circles) virus pairs were compared using the Wilcoxon signed-rank test. n.s., not significant. Bars indicate means.
To obtain a numerical measure of the in vitro replicative capacities, we calculated the slopes of viral antigen production between days 0 and 6. During this early phase before replication peaks, both groups of viruses have the same growth conditions in terms of supply of target cells and nutrition and thus a logarithmic growth phase can be safely assumed. Again, a significant difference between the controlling and noncontrolling groups was found using these slopes as a measure of the in vitro replicative capacities (Fig. 1c).
The in vitro replicative capacity does not change during short-term STI.
It cannot be excluded that isolates derived during the fifth cycle evolved as a consequence of immune escape and viral evolution during STI (23). Specimens for virus isolation at pre-ART time points were not available, but it was recently shown that virus evolving early in STI represents pre-ART quasipecies (B. Joos, M. Fischer, A. Trkola, J. Böni, H. Kuster, A. Oxenius, J. Wong, B. Hirschel, R. Weber, and H. Günthard, 9th Conf. Retrovir. Opportunistic Infect., abstr. 531-M, 2002). We therefore probed whether or not STI induced changes in the replication potencies of individual strains by comparing the growth characteristics of first-cycle and fifth-cycle virus pairs from 10 patients (8 noncontrolling and 2 controlling patients) (Table 1 and Fig. 1d). We observed no tendency towards the evolution of more rapidly replicating or more slowly replicating strains. No significant differences between total levels of viral antigen produced by early and late isolate pairs were detected (Wilcoxon signed-rank test) (Fig. 1d), nor was a difference in replication slopes detectable (data not shown). This excludes the possibility that short-term STI induced changes in virulence and indicates a preexisting infection with these slow-replicating isolates before initiation of ART.
Relationship between viral replicative capacities and viremia levels.
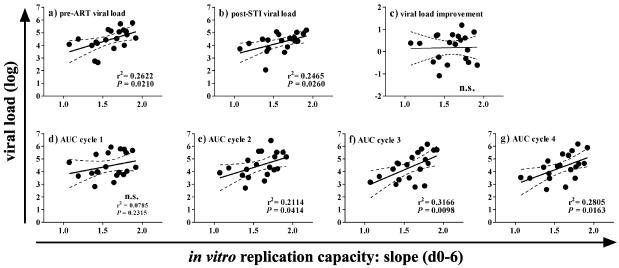
A central point of our investigation was to determine whether viral replication capacity in vitro substantially impacts viral replication in vivo. We observed that low replication capacities of the patient isolates correlated with both low pre-ART and low post-STI plateaus but not with the patients' abilities to improve viral set points upon STI (Fig. 2a to c).
FIG. 2.
In vitro replication kinetics correlate with in vivo VLs. Results of the correlation analysis of in vitro replication capacities {slopes of viral antigen production between days 0 and 6 [slope (d0-6)]} and pre-ART VLs (a), post-STI VLs (b), levels of VL improvement (c), and cumulative levels of viral replication (AUC) during cycles 1 (d), 2 (e), 3 (f), and 4 (g) are shown. n.s., not significant.
Our data provide further evidence that the in vitro replication capacity of a viral isolate influences the total amount of virus replication during the short-term treatment interruption. The in vitro replication capacities of patient virus isolates correlated with the cumulative viral production levels (AUC) during cycles 2, 3, and 4 but did not reach statistical significance for the first cycle (Fig. 2d to g). This suggests that viral rebound may be driven at least in part by viral properties.
Sensitivity to inhibition by chemokines.
Viral fitness in vivo will not only be a consequence of the efficacy of virus-target cell interaction but will also be steered by the presence of and susceptibility to antiviral agents. Since the virus isolates investigated here were fully suppressed by the antiretroviral drugs prescribed, we focused our investigation on naturally occurring antiviral agents, namely chemokines and neutralizing antibodies. Differential susceptibilities to one or both of these classes of inhibitors could potentially affect viral replication in vivo.
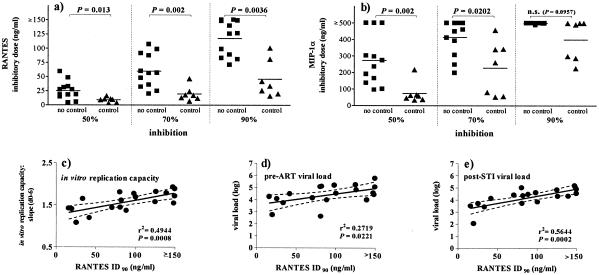
We assessed the inhibitory effects of the chemokines RANTES/CCL5 and MIP-1α/CCL3 on viral replication in stimulated healthy donor CD4+ T cells. To rule out distortion of the results by donor cell influences, all isolates were analyzed on cells from the same donors. The R5X4 isolate from patient 116 was excluded from this analysis.
We observed in both the controlling and the noncontrolling patient groups chemokine-sensitive and -insensitive isolates. In agreement with previous observations (45), we found that isolates were overall more susceptible to inhibition by RANTES than by MIP-1α (median 70% inhibitory doses were 36 and 393 ng/ml, respectively). Isolates from the controlling group showed an increased sensitivity to inhibition by chemokines compared to isolates from the noncontrolling group (Table 2; Fig. 3a and b). The median inhibitory doses of RANTES differed significantly between the two patient groups. A difference in susceptibilities to inhibition by MIP-1α was also observed but was less pronounced. This is probably due to the lower intrinsic inhibitory activity of MIP-1α. Only 6 of the 19 isolates were inhibited to 90% at the highest concentration tested (500 ng/ml).
TABLE 2.
Inhibitory doses (ID)a of chemokines, neutralizing antibodies, and tetrameric CD4-IgG2
| Patient | RANTES
|
MIP-1α
|
2F5 ID90 (mg/ml) | 2G12 ID90 (mg/ml) | IgG1 b12 ID90 (mg/ml) | CD4-IgG2 ID90 (mg/ml) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| ID50 (ng/ml) | ID70 (ng/ml) | ID90 (ng/ml) | ID50 (ng/ml) | ID70 (ng/ml) | ID90 (ng/ml) | |||||
| Control group | ||||||||||
| 106 | 16 | 46 | 81 | 218 | >343 | 491 | 13.9 | >25 | 5.4 | 19.2 |
| 107 | <3 | 13 | 34 | 58 | >458 | >500 | 16.2 | 0.8 | >10 | 24.3 |
| 112 | 9 | 24 | 101 | 65 | 341 | >500 | 12.7 | >25 | 7.9 | 14.1 |
| 117 | 11 | 17 | 42 | 62 | 262 | >500 | 3.7 | 2.3 | 4.4 | >25 |
| 118 | <10 | 12 | 16 | 37 | 53 | 288 | 19.3 | >25 | >10 | 24.3 |
| 125 | 11 | 18 | 26 | 33 | 56 | 225 | 22.9 | >25 | >10 | >25 |
| 130 | 4 | 7 | 20 | 45 | 81 | 300 | 17.7 | >25 | 9.6 | 22.4 |
| Noncontrol group | ||||||||||
| 102 | 14 | >98 | >150 | >500 | >500 | >500 | 20.5 | 1.4 | 8.5 | 22.3 |
| 109 | 27 | 91 | >148 | >500 | >500 | >500 | 21.3 | >25 | >10 | 9.5 |
| 111 | 30 | 57 | 83 | 164 | >393 | >500 | 17.4 | 16.9 | 9.5 | 15.4 |
| 113 | 48 | 107 | >150 | >273 | >500 | >500 | >25 | 4.7 | >10 | 24.1 |
| 114 | 32 | 60 | 89 | 95 | >461 | >500 | >25 | 24.8 | >10 | 17.5 |
| 116 | ND | ND | ND | ND | ND | ND | 21.3 | 7.0 | 5.9 | 18.1 |
| 119 | 18 | 25 | 81 | 235 | >412 | >500 | 19.8 | >25 | >10 | >25 |
| 120 | 27 | 56 | 99 | 136 | 247 | >500 | 7.9 | 22.4 | >10 | 13.1 |
| 121 | 4 | 20 | >125 | >296 | >500 | >500 | 3.6 | 0.6 | 6.9 | 9.4 |
| 122 | 5 | 32 | 71 | 100 | 197 | >488 | 11.8 | 8.1 | 5.2 | 7.4 |
| 126 | 19 | 36 | >126 | 190 | >307 | >498 | 22.1 | >25 | >10 | 23.1 |
| 127 | 18 | 47 | >149 | 303 | >450 | >500 | 19.8 | 17.0 | 9.6 | 10.3 |
| 128 | 59 | 87 | >140 | >500 | >500 | >500 | 16.3 | 10.0 | 9.5 | 11.1 |
ID50, ID70, and ID90 are 50, 70, and 90% inhibitory doses, respectively. ND, not determined.
FIG. 3.
Sensitivity to inhibition by chemokines. The 50, 70, and 90% inhibitory doses of RANTES (a) and MIP-1α (b) in CD8-depleted PBMC cultures are shown. Inhibitory doses for viruses from controlling (triangles) and noncontrolling (squares) patients were compared using the Mann-Whitney test. Data are means of results from two independent experiments. Results of the correlation analysis of the 90% inhibitory doses (ID90) of RANTES with in vitro replication capacities {slopes of viral antigen production between days 0 and 6 [slope (d0-6)]} (c), pre-ART VLs (d), and post-STI VLs (e) are displayed. n.s., not significant. Bars indicate means.
Most strikingly, a strong correlation between low replication capacities of viral isolates in vitro and high sensitivities to RANTES was found (Fig. 3c). In addition, sensitivities to inhibition by RANTES correlated with pre-ART VLs and post-STI viral set points (Fig. 3d and e). Increased sensitivity of low-replicating isolates to inhibition by CCR5-targeting chemokines could indicate that these viruses require high coreceptor densities on target cells for entry. A low availability of cells expressing high levels of CCR5 together with the increased sensitivity to inhibition by endogenous chemokines could therefore contribute to reduced fitness and consequently lower replication of these viruses in vivo. Of note, no influence of genetic polymorphisms in the genes for CCR5, RANTES, and MIP-1α on viremia control was observed in our subset of patients (Table 3).
TABLE 3.
Genotypic analysisa
| Patient | Characterization of genes for:
|
||||||
|---|---|---|---|---|---|---|---|
| CCR5 G-2455A | CCR5 delta 32 | CCR2 V64I | RANTES G-403A | RANTES C-28G | MIP-1α T113C | SDF-1 3′A | |
| Controlling group | |||||||
| 106 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| 107 | 3 | 2 | 1 | 1 | 1 | 1 | 1 |
| 112 | 3 | 2 | 1 | 1 | 1 | 2 | 1 |
| 117 | 1 | 1 | 1 | 2 | 1 | 2 | 1 |
| 118 | 3 | 1 | 2 | 1 | 1 | 1 | 1 |
| 125 | 2 | 1 | 1 | 2 | 1 | 2 | 3 |
| 130 | 2 | 1 | 1 | 1 | 1 | 2 | 2 |
| Noncontrolling group | |||||||
| 102 | 2 | 1 | 1 | 1 | 1 | 2 | 1 |
| 109 | 2 | 2 | 1 | 1 | 1 | 2 | 1 |
| 111 | 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| 113 | 3 | 1 | 2 | 1 | 1 | 2 | 1 |
| 114 | 2 | 1 | 1 | 1 | 1 | 2 | 1 |
| 116 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 119 | 2 | 2 | 1 | 1 | 1 | 1 | 3 |
| 120 | 2 | 2 | 1 | 1 | 1 | 2 | 3 |
| 121 | 2 | 2 | 1 | 1 | 1 | 2 | 1 |
| 122 | 2 | 1 | 1 | 1 | 1 | 2 | 1 |
| 126 | 2 | 1 | 1 | 1 | 1 | 1 | 2 |
| 127 | 2 | 1 | 1 | 1 | 1 | 2 | 1 |
| 128 | 3 | 1 | 2 | 1 | 1 | 1 | 2 |
1 indicates wild-type genes, and 2 and 3 indicate heterozygosity and homozygosity, respectively, for the mutant gene.
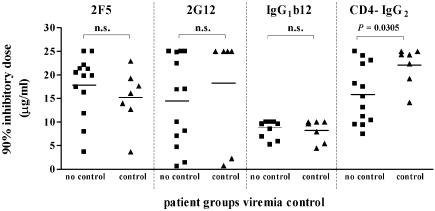
Sensitivity to inhibition by neutralizing antibodies.
Given that high sensitivity to inhibition by chemokines was strongly associated with low in vitro replication capacity of a virus isolate, one could reason that the observed effect of chemokines may be simply a consequence of the decreased infectivity in vitro. This may potentially be the case, since efficacy of inhibition was assessed over multiple rounds of infection and, therefore, over time inhibitory agents will have to counter vastly different amounts of virus. In order to probe whether viruses with low replication capacities are in general more susceptible to antivirals, we investigated their sensitivities to inhibition by the potent neutralizing anti-gp41 MAb 2F5 and the anti-gp120 MAbs 2G12 and IgG1b12 as well as the tetrameric CD4 molecule, CD4-IgG2. In contrast to results for inhibition by chemokines, we found no significant differences in sensitivities to these antibodies. Of note, virus isolates from the controlling group proved to be slightly more resistant to CD4-IgG2 (Table 2; Fig. 4). Therefore, the increased sensitivities of virus isolates with slow replication capacities to inhibition by chemokines is a distinct feature of these virus strains and does not reflect a general sensitivity to entry inhibitors.
FIG. 4.
Sensitivity to inhibition by neutralizing antibodies and CD4-IgG2. The 90% inhibitory doses for the neutralizing anti-gp41 MAb 2F5, the anti-gp120 MAbs 2G12 and IgG1b12, and the tetrameric CD4 molecule, CD4-IgG2, are shown. Inhibitory doses for viruses from controlling (triangles) and noncontrolling (squares) patients were compared using the Mann-Whitney test. Data are means of results from two to four independent experiments. n.s., not significant. Bars indicate means.
HLA genotypes and viremia control.
Our analysis of virus isolates from chronically HIV-1-infected individuals thus far leaves open the question of whether virus isolates with low replication capacities were transmitted or emerged over time as a result of an active immune defense. In order to resolve the issue of whether low viral fitness is more a consequence of selection during transmission or a reflection of the impact of immune pressure, an extensive, longitudinal monitoring of patients from acute to chronic disease stages will be necessary. While this type of analysis could not be performed since natural history samples from the acute infection stage were not available for our patient cohort, we further investigated the potential influence of host genetic factors on viral replication and control. This is of particular interest since both transmission and emergence of viral isolates with low fitness will be influenced by genetic host factors, either directly as in the case of the chemokine and chemokine receptor polymorphisms described above or indirectly through control of immune responses. Several HLA genotypes been shown to influence disease progression and viremia control and are considered to drive immune defense and thus viral replication (10, 22, 42). We therefore determined HLA genotypes in our cohort (Table 4) and explored whether the distribution of HLA genotypes which are described to be associated with susceptibility (HLA-B*08, HLA-B*3501, HLA-B*45, HLA-B*53, and HLA-Cw*04) or protection (HLA-A2/*6802, HLA-A*11, HLA-B*27, HLA-B*51, HLA-B*57, HLA-B*58, HLA-Cw*08, and HLA DRB*01) may indicate why viral variants with low or high replication capacities were selected in our patient cohort. We found that neither genes considered to confer protection nor genes associated with increased viral replication and disease progression were present at higher frequencies in either the controlling or the noncontrolling group. However, it has to be taken into consideration that our cohort of patients is small, and given the vast polymorphism of HLA genes, it is not too surprising that no such associations were found. Although it does not appear that HLA genotypes were a driving force in the establishment of viral fitness in our patients, it nevertheless cannot be ruled out that these genes in concert with other immune and genetic parameters contributed to the selection of viral variants.
TABLE 4.
HLA genotypesa
| Patient | Genotype of HLA-I
|
Genotype of HLA-II
|
|||||
|---|---|---|---|---|---|---|---|
| A | B | Cw | DRB1 | DRB3 | DRB4 | DRB5 | |
| Controlling group | |||||||
| 106 | *31, *2601/02/08 | *14, *40 | *0304/06/08/05, *0802/04 | *04, *1101/04 | *02 | *01 | |
| 107 | *02, *− | *44, *5201 | *0303, *0501 | *1301/02, *− | *0101, *0301 | ||
| 112 | *02, *03 | *07, *51 | *0702, *1203 | *0101/03/04, *1301/02 | *0301 | ||
| 117 | *02, *68 | *4901, *57 | *0602/03, *07 | *1101/04, *07 | *02 | *01 | |
| 118 | *0101-05N | *08, *57 | *0602, *07 | *1501/03, *03011/05 | *0101 | *0101 | |
| 125 | *11, *33 | *5801, *15 | *1203, *0302/05 | *12, *1301/02 | *0301, *0301 | ||
| 130 | *02, *03 | *15, *35 | *0304/06/08/09, *0401/04/05 | *0101/04, *04 | *01 | ||
| Noncontrolling group | |||||||
| 102 | *2301, *32 | *35, *38 | *0401/04/05, *1203 | *1101/04, *1303 | *0101 | ||
| 109 | *11, *25 | *18, *− | *02022/024, *0701/05/06 | *1101/04, *0701 | *02 | *01 | |
| 111 | *02, *03 | *07, *− | *07, *− | *1501*03, *− | *0101 | ||
| 113 | *03, *− | *15, *57 | *0304/06/08/09, *0602/03 | *04, *07 | *01, *01 | ||
| 114 | *02, *31012/3102 | *27, *51 | *0102/03, *1502/05/06 | *0101/04, *1101/04 | *02 | ||
| 116 | *02, *03 | *44, *4901 | *02, *07 | *1101/04, *04 | *02 | *01 | |
| 119 | *24, *68 | *15, *44 | *0303, *0704 | *04, *1101/04 | *02 | *01 | |
| 120 | *02, *24 | *27, *44 | *0102/03, *1601 | *0103, *07 | *01 | ||
| 121 | *01, *− | *07, *27 | *0702, *02 | *1501/03, *0901 | *01 | *0101 | |
| 122 | *03, *24 | *57, *15 | *0303, *0602/03 | *07, *1301/02 | *02 | *01 | |
| 126 | *03, *33 | *14, *18 | *0701/05/06, *0802/04 | *11, *13 | *02, *0101 | ||
| 127 | *01, *11 | *08, *15 | *0701/05/06, *0102/03 | *04, *1102/03 | *02 | *01 | |
| 128 | *03, *24 | *35, *57 | *0602/03, *0401/02/04/05 | *0101/04, *07 | *01 | ||
Dashes indicate homozygosity.
DISCUSSION
In this study, we investigated the generic fitness of virus isolates derived from patients participating in the SSITT (15, 32). A fraction of patients (17%) participating in this trial potently suppressed viremia upon final cessation of ART. However, this control of viremia was not induced by STI but reflected pre-ART viral set points (15, 32). Thus far no parameter could be identified that provided insight into how and why these patients maintained low VLs in the absence of treatment (15, 29-32).
Observations made in long-term nonprogressing patients and analysis of drug-resistant strains of HIV-1 strongly suggest that low viral replication capacity in vitro may be directly associated with a decreased viral burden in vivo and predicts slower disease progression (5, 14, 16, 17, 19, 20, 36, 37, 40, 48). In agreement with the results of previous studies, we found a significant correlation between viral replication capacities in vitro and viral set points in our group of 20 chronically infected patients.
Previous reports have by and large focused on cross-sectional analyses of patients. The advantage of the present study lies in the nature of the STI, in which a coherent group of patients, fully sensitive to antiretroviral drugs, underwent several controlled viremic episodes. The close longitudinal monitoring of these patients provided the empirical data to probe whether viral fitness steers the magnitude of the rebounding viremia. We were able to demonstrate that the difference in replication capacities as measured in vitro remains proportional to the replication rate in vivo over several short-term intervals of viral replication. Collectively, although the investigated group of patients is small, these data support the hypothesis that viral rebound in chronic HIV-1 infection is in part driven by viral fitness.
Of note is that the determination of the replicative capacity in vitro excludes several potential factors affecting viral replication in vivo. Thus, in vivo viral fitness will not be driven only by the virus's access to target cells and its aptitude to efficiently enter these cells and establish productive infection but also by its sensitivity to inhibitory agents such as drugs, neutralizing antibodies, and antiviral chemokines.
With one exception, all virus isolates tested utilized solely R5 for entry and should thus in principle be able to infect the same pool of target cells. HIV-1 isolates are known to differ greatly in their susceptibilities to inhibition by chemokines (45). Whether or not the antiviral potency of chemokines substantially contributes to viremia control in vivo has not yet been conclusively determined (11, 21, 25, 34). The efficacy of chemokine inhibition will be governed by the sensitivity of the individual virus strain to inhibition, by the magnitude of chemokine secretion, and also by the genetically and cell type-dependent density of chemokine receptor expression.
A key finding of the present study was the observation that viruses from patients who control viremia at low levels are more susceptible to inhibition by CCR5-targeting chemokines. This correlation argues for a low affinity of the respective viral envelope proteins in the interaction with the receptor and/or a particular need of these viruses for high levels of CCR5 expression on their target cells. The restriction in replication could be to some extent due to the lack of appropriate target cells expressing the required high density of receptors. Taken together, our data suggest that the low replication capacities of these viruses are at least in part due to a limitation in viral entry. We are currently cloning the envelopes of these viruses to investigate whether the ensuing low replication capacity is mainly the result of a less efficient entry process or whether additional viral genes participate in manifesting the low-replication phenotype.
Due to their reduced virulence, viruses with low replication capacities will cause less destruction to the immune system and thus might be more successful in inducing and maintaining immune responses (5, 17, 39). Likewise, at a reduced replication rate, mechanisms of escape from immune responses and antiretroviral drugs will appear less rapidly (8, 36). Whether or not low viral fitness was a cause or an effect of an improved anti-HIV immune response could not be determined conclusively in this cohort of patients. Despite significant increases in HIV-specific cytotoxic T-cell responses and T helper responses, no correlation between these cellular immune responses and control of viremia was found (32). However, autologous neutralization responses pre-STI were found to be higher among patients who suppressed viremia (A. Trkola and H. F. Günthard, unpublished data). Determining when and why these viruses with low replicating capacities evolved will require further investigations. At present it remains unclear whether viruses with decreased replication capacities were already present at the stage of transmission or were selected over time as a consequence of an active immune defense and/or genetic host factors. To fully unravel the dependencies of virus and immune responses, a longitudinal analysis of a larger set of patients from acute to chronic disease stages will be required.
Our data provide substantial evidence that viral fitness was a determining factor of low viral set points detected in a fraction of patients participating in the SSITT. Furthermore, our observations strongly suggest that low-replicating viruses were present before ART was initiated and therefore are not a consequence of STI. Thus, to fully understand the prospects of therapeutic interventions in chronic infection, it is pivotal to consider viral fitness and its consequences for activation and maintenance of immune responses or emergence of drug resistance.
Acknowledgments
This study was financed within the framework of the Swiss HIV Cohort Study, supported by the Swiss National Science Foundation (grant no. 3345-062041). Support was provided by the Swiss National Science Foundation (grant no. 3345-65168 to H. F. Günthard and A. Trkola and Swiss grant no. 3100-62030 to A. Trkola), the Swiss HIV Cohort Study project 290, and a subcontract to A. Trkola from NIH grant R37 AI36082 to J. P. Moore.
We thank J. P. Moore for helpful discussions, our patients for their commitment, Christine Schneider and Roland Hafner for excellent patient care, Jean-Marie Tiercy for HLA typing, and Friedericke Burgener and Erika Schlaepfer for laboratory support.
Members of the Swiss HIV Cohort Study are M. Battegay, E. Bernasconi, H. Bucher, P. Bürgisser, M. Egger, P. Erb, W. Fierz, M. Fischer, M. Flepp (chairman of the clinical and laboratory committee), P. Francioli (president of the Swiss HIV Cohort Study, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland), H. J. Furrer, M. Gorgievski, H. Günthard, P. Grob, B. Hirschel, L. Kaiser, C. Kind, T. Klimkait, B. Ledergerber, U. Lauper, M. Opravil, F. Paccaud, G. Pantaleo, L. Perrin, J.-C. Piffaretti, M. Rickenbach (head of data center), C. Rudin (chairman of the mother and child substudy), J. Schupbach, R. Speck, A. Telenti, A. Trkola, P. Vernazza (chairman of the scientific board), T. Wagels, R. Weber, and S. Yerly.
REFERENCES
- 1.Allaway, G. P., K. L. Davis-Bruno, G. A. Beaudry, E. B. Garcia, E. L. Wong, A. M. Ryder, K. W. Hasel, M. C. Gauduin, R. A. Koup, J. S. McDougal, et al. 1995. Expression and characterization of CD4-IgG2, a novel heterotetramer that neutralizes primary HIV type 1 isolates. AIDS Res. Hum. Retrovir. 11:533-539. [DOI] [PubMed] [Google Scholar]
- 2.Allen, T. M., and D. I. Watkins. 2001. New insights into evaluating effective T-cell responses to HIV. AIDS 15(Suppl. 5):S117-S126. [DOI] [PubMed] [Google Scholar]
- 3.Barbas, C. F., III, D. Hu, N. Dunlop, L. Sawyer, D. Cababa, R. M. Hendry, P. L. Nara, and D. R. Burton. 1994. In vitro evolution of a neutralizing human antibody to human immunodeficiency virus type 1 to enhance affinity and broaden strain cross-reactivity. Proc. Natl. Acad. Sci. USA 91:3809-3813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Binley, J. M., A. Trkola, T. Ketas, D. Schiller, B. Clas, S. Little, D. Richman, A. Hurley, M. Markowitz, and J. P. Moore. 2000. The effect of highly active antiretroviral therapy on binding and neutralizing antibody responses to human immunodeficiency virus type 1 infection. J. Infect. Dis. 182:945-949. [DOI] [PubMed] [Google Scholar]
- 5.Blaak, H., M. Brouwer, L. J. Ran, F. de Wolf, and H. Schuitemaker. 1998. In vitro replication kinetics of human immunodeficiency virus type 1 (HIV-1) variants in relation to virus load in long-term survivors of HIV-1 infection. J. Infect. Dis. 177:600-610. [DOI] [PubMed] [Google Scholar]
- 6.Blaak, H., A. B. van't Wout, M. Brouwer, B. Hooibrink, E. Hovenkamp, and H. Schuitemaker. 2000. In vivo HIV-1 infection of CD45RA(+)CD4(+) T cells is established primarily by syncytium-inducing variants and correlates with the rate of CD4(+) T cell decline. Proc. Natl. Acad. Sci. USA 97:1269-1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bleiber, G., M. Munoz, A. Ciuffi, P. Meylan, and A. Telenti. 2001. Individual contributions of mutant protease and reverse transcriptase to viral infectivity, replication, and protein maturation of antiretroviral drug-resistant human immunodeficiency virus type 1. J. Virol. 75:3291-3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonhoeffer, S., A. D. Barbour, and R. J. De Boer. 2002. Procedures for reliable estimation of viral fitness from time-series data. Proc. R. Soc. Lond. B 269:1887-1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bunce, M., C. M. O'Neill, M. C. Barnardo, P. Krausa, M. J. Browning, P. J. Morris, and K. I. Welsh. 1995. Phototyping: comprehensive DNA typing for HLA-A, B, C, DRB1, DRB3, DRB4, DRB5 & DQB1 by PCR with 144 primer mixes utilizing sequence-specific primers (PCR-SSP). Tissue Antigens 46:355-367. [DOI] [PubMed] [Google Scholar]
- 10.Carrington, M., and S. J. O'Brien. 2003. The influence of HLA genotype on AIDS. Annu. Rev. Med. 54:535-551. [DOI] [PubMed] [Google Scholar]
- 11.Cocchi, F., A. L. DeVico, A. Garzino-Derno, S. K. Arya, R. C. Gallo, and P. Lusso. 1995. Identification of RANTES, MIP-1 alpha and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science 270:1811-1815. [DOI] [PubMed] [Google Scholar]
- 12.Connor, R. I., K. E. Sheridan, D. Ceradini, S. Choe, and N. R. Landau. 1997. Change in coreceptor use correlates with disease progression in HIV-1-infected individuals. J. Exp. Med. 185:621-628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Boer, R. J., and A. S. Perelson. 1998. Target cell limited and immune control models of HIV infection: a comparison. J. Theor. Biol. 190:201-214. [DOI] [PubMed] [Google Scholar]
- 14.Deeks, S. G., R. M. Grant, T. Wrin, E. E. Paxinos, T. Liegler, R. Hoh, J. N. Martin, and C. J. Petropoulos. 2003. Persistence of drug-resistant HIV-1 after a structured treatment interruption and its impact on treatment response. AIDS 17:361-370. [DOI] [PubMed] [Google Scholar]
- 15.Fagard, C., A. Oxenius, H. Günthard, F. Garcia, M. Le Braz, G. Mestre, M. Battegay, H. Furrer, P. Vernazza, E. Bernasconi, A. Telenti, R. Weber, D. Leduc, S. Yerly, D. Price, S. J. Dawson, T. Klimkait, T. V. Perneger, A. McLean, B. Clotet, J. M. Gatell, L. Perrin, M. Plana, R. Phillips, and B. Hirschel. 2003. A prospective trial of structured treatment interruptions in human immunodeficiency virus infection. Arch. Intern. Med. 163:1220-1226. [DOI] [PubMed] [Google Scholar]
- 16.Fenyo, E. M., L. Morfeldt-Manson, F. Chiodi, B. Lind, A. von Gegerfelt, J. Albert, E. Olausson, and B. Asjo. 1988. Distinct replicative and cytopathic characteristics of human immunodeficiency virus isolates. J. Virol. 62:4414-4419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grovit-Ferbas, K., J. Ferbas, V. Gudeman, S. Sadeghi, M. B. Goetz, J. V. Giorgi, I. S. Chen, and W. A. O'Brien. 1998. Potential contributions of viral envelope and host genetic factors in a human immunodeficiency virus type 1-infected long-term survivor. J. Virol. 72:8650-8658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatano, H., S. Vogel, C. Yoder, J. A. Metcalf, R. Dewar, R. T. Davey, Jr., and M. A. Polis. 2000. Pre-HAART HIV burden approximates post-HAART viral levels following interruption of therapy in patients with sustained viral suppression. AIDS 14:1357-1363. [DOI] [PubMed] [Google Scholar]
- 19.Kaufmann, D., M. Munoz, G. Bleiber, S. Fleury, B. Lotti, R. Martinez, W. Pichler, P. Meylan, and A. Telenti. 2000. Virological and immunological characteristics of HIV treatment failure. AIDS 14:1767-1774. [DOI] [PubMed] [Google Scholar]
- 20.Kwa, D., J. Vingerhoed, B. Boeser, and H. Schuitemaker. 2003. Increased in vitro cytopathicity of CC chemokine receptor 5-restricted human immunodeficiency virus type 1 primary isolates correlates with a progressive clinical course of infection. J. Infect. Dis. 187:1397-1403. [DOI] [PubMed] [Google Scholar]
- 21.Liu, H., D. Chao, E. E. Nakayama, H. Taguchi, M. Goto, X. Xin, J. K. Takamatsu, H. Saito, Y. Ishikawa, T. Akaza, T. Juji, Y. Takebe, T. Ohishi, K. Fukutake, Y. Maruyama, S. Yashiki, S. Sonoda, T. Nakamura, Y. Nagai, A. Iwamoto, and T. Shioda. 1999. Polymorphism in RANTES chemokine promoter affects HIV-1 disease progression. Proc. Natl. Acad. Sci. USA 96:4581-4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MacDonald, K. S., K. R. Fowke, J. Kimani, V. A. Dunand, N. J. Nagelkerke, T. B. Ball, J. Oyugi, E. Njagi, L. K. Gaur, R. C. Brunham, J. Wade, M. A. Luscher, P. Krausa, S. Rowland-Jones, E. Ngugi, J. J. Bwayo, and F. A. Plummer. 2000. Influence of HLA supertypes on susceptibility and resistance to human immunodeficiency virus type 1 infection. J. Infect. Dis. 181:1581-1589. [DOI] [PubMed] [Google Scholar]
- 23.Martinez-Picado, J., K. Morales-Lopetegi, T. Wrin, J. G. Prado, S. D. Frost, C. J. Petropoulos, B. Clotet, and L. Ruiz. 2002. Selection of drug-resistant HIV-1 mutants in response to repeated structured treatment interruptions. AIDS 16:895-899. [DOI] [PubMed] [Google Scholar]
- 24.Martinez-Picado, J., A. V. Savara, L. Sutton, and R. T. D'Aquila. 1999. Replicative fitness of protease inhibitor-resistant mutants of human immunodeficiency virus type 1. J. Virol. 73:3744-3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDermott, D. H., M. J. Beecroft, C. A. Kleeberger, F. M. Al-Sharif, W. E. R. Ollier, P. E. Zimmerman, B. A. Boatin, S. F. Leitman, R. Detels, A. H. Hajeer, and P. M. Murphy. 2000. Chemokine RANTES promotor polymorphism affects risk of both HIV infection and disease progression in the Multicenter AIDS Cohort Study. AIDS 14:2671-2678. [DOI] [PubMed] [Google Scholar]
- 26.Mellors, J. W., C. R. Rinaldo, Jr., P. Gupta, R. M. White, J. A. Todd, and L. A. Kingsley. 1996. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science 272:1167-1170. [DOI] [PubMed] [Google Scholar]
- 27.Moore, J. P., Y. Cao, D. D. Ho, and R. A. Koup. 1994. Development of the anti-gp120 antibody response during seroconversion to human immunodeficiency virus type 1. J. Virol. 68:5142-5155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muster, T., F. Steindl, M. Purtscher, A. Trkola, A. Klima, G. Himmler, F. Ruker, and H. Katinger. 1993. A conserved neutralizing epitope on gp41 of human immunodeficiency virus type 1. J. Virol. 67:6642-6647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oxenius, A., H. F. Günthard, B. Hirschel, S. Fidler, J. N. Weber, P. J. Easterbrook, J. I. Bell, R. E. Phillips, and D. A. Price. 2001. Direct ex vivo analysis reveals distinct phenotypic patterns of HIV-specific CD8(+) T lymphocyte activation in response to therapeutic manipulation of virus load. Eur. J. Immunol. 31:1115-1121. [DOI] [PubMed] [Google Scholar]
- 30.Oxenius, A., A. R. McLean, M. Fischer, D. A. Price, S. J. Dawson, R. Hafner, C. Schneider, H. Joller, B. Hirschel, R. E. Phillips, R. Weber, and H. F. Günthard. 2002. Human immunodeficiency virus-specific CD8(+) T-cell responses do not predict viral growth and clearance rates during structured intermittent antiretroviral therapy. J. Virol. 76:10169-10176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oxenius, A., D. A. Price, S. J. Dawson, H. F. Günthard, M. Fischer, L. Perrin, E. Ramirez, C. Fagard, B. Hirschel, G. Scullard, J. N. Weber, A. R. McLean, and R. E. Phillips. 2002. Residual HIV-specific CD4 and CD8 T cell frequencies after prolonged antiretroviral therapy reflect pretreatment plasma virus load. AIDS 16:2317-2322. [DOI] [PubMed] [Google Scholar]
- 32.Oxenius, A., D. A. Price, H. F. Günthard, S. J. Dawson, C. Fagard, L. Perrin, M. Fischer, R. Weber, M. Plana, F. Garcia, B. Hirschel, A. McLean, and R. E. Phillips. 2002. Stimulation of HIV-specific cellular immunity by structured treatment interruption fails to enhance viral control in chronic HIV infection. Proc. Natl. Acad. Sci. USA 99:13747-13752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parren, P. W., J. P. Moore, D. R. Burton, and Q. J. Sattentau. 1999. The neutralizing antibody response to HIV-1: viral evasion and escape from humoral immunity. AIDS 13(Suppl. A):S137-S162. [PubMed] [Google Scholar]
- 34.Paxton, W. A., A. U. Neumann, S. Kang, L. Deutch, R. C. Brown, R. A. Koup, and S. M. Wolinsky. 2001. RANTES production from CD4+ lymphocytes correlates with host genotype and rates of human immunodeficiency virus type 1 disease progression. J. Infect. Dis. 183:1678-1681. [DOI] [PubMed] [Google Scholar]
- 35.Piatak, M., Jr., M. S. Saag, L. C. Yang, S. J. Clark, J. C. Kappes, K. C. Luk, B. H. Hahn, G. M. Shaw, and J. D. Lifson. 1993. High levels of HIV-1 in plasma during all stages of infection determined by competitive PCR. Science 259:1749-1754. [DOI] [PubMed] [Google Scholar]
- 36.Quinones-Mateu, M. E., and E. J. Arts. 2001. HIV-1 fitness: implications for drug resistance, disease progression, and global epidemic evolution, p. 134-170. In C. Kuiken, B. Foley, B. Hahn, P. Marx, F. McCutchan, J. Mellors, S. Wolinsky, and B. Korber (ed.), HIV sequence compendium 2001. Theoretical Biology and Biophysics Group, Los Alamos National Laboratory, Los Alamos, N.Mex.
- 37.Quinones-Mateu, M. E., S. C. Ball, A. J. Marozsan, V. S. Torre, J. L. Albright, G. Vanham, G. van der Groen, R. L. Colebunders, and E. J. Arts. 2000. A dual infection/competition assay shows a correlation between ex vivo human immunodeficiency virus type 1 fitness and disease progression. J. Virol. 74:9222-9233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rowland-Jones, S., S. Pinheiro, and R. Kaul. 2001. New insights into host factors in HIV-1 pathogenesis. Cell 104:473-476. [DOI] [PubMed] [Google Scholar]
- 39.Scarlatti, G., T. Leitner, V. Hodara, M. Jansson, A. Karlsson, J. Wahlberg, P. Rossi, M. Uhlen, E. M. Fenyo, and J. Albert. 1996. Interplay of HIV-1 phenotype and neutralizing antibody response in pathogenesis of AIDS. Immunol Lett. 51:23-28. [DOI] [PubMed] [Google Scholar]
- 40.Schuitemaker, H., M. Koot, N. A. Kootstra, M. W. Dercksen, R. E. de Goede, R. P. van Steenwijk, J. M. Lange, J. K. Schattenkerk, F. Miedema, and M. Tersmette. 1992. Biological phenotype of human immunodeficiency virus type 1 clones at different stages of infection: progression of disease is associated with a shift from monocytotropic to T-cell-tropic virus population. J. Virol. 66:1354-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Telenti, A., V. Aubert, and F. Spertini. 2002. Individualising HIV treatment—pharmacogenetics and immunogenetics. Lancet 359:722-723. [DOI] [PubMed] [Google Scholar]
- 42.Trachtenberg, E., B. Korber, C. Sollars, T. B. Kepler, P. T. Hraber, E. Hayes, R. Funkhouser, M. Fugate, J. Theiler, Y. S. Hsu, K. Kunstman, S. Wu, J. Phair, H. Erlich, and S. Wolinsky. 2003. Advantage of rare HLA supertype in HIV disease progression. Nat. Med. 9:928-935. [DOI] [PubMed] [Google Scholar]
- 43.Trkola, A., T. Ketas, V. N. Kewalramani, F. Endorf, J. M. Binley, H. Katinger, J. Robinson, D. R. Littman, and J. P. Moore. 1998. Neutralization sensitivity of human immunodeficiency virus type 1 primary isolates to antibodies and CD4-based reagents is independent of coreceptor usage. J. Virol. 72:1876-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trkola, A., J. Matthews, C. Gordon, T. Ketas, and J. P. Moore. 1999. A cell line-based neutralization assay for primary human immunodeficiency virus type 1 isolates that use either the CCR5 or the CXCR4 coreceptor. J. Virol. 73:8966-8974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trkola, A., W. A. Paxton, S. P. Monard, J. A. Hoxie, M. A. Siani, D. A. Thompson, L. Wu, C. R. Mackay, R. Horuk, and J. P. Moore. 1998. Genetic subtype-independent inhibition of human immunodeficiency virus type 1 replication by CC and CXC chemokines. J. Virol. 72:396-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Trkola, A., A. B. Pomales, H. Yuan, B. Korber, P. J. Maddon, G. P. Allaway, H. Katinger, C. F. Barbas III, D. R. Burton, D. D. Ho, and J. P. Moore. 1995. Cross-clade neutralization of primary isolates of human immunodeficiency virus type 1 by human monoclonal antibodies and tetrameric CD4-IgG. J. Virol. 69:6609-6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Trkola, A., M. Purtscher, T. Muster, C. Ballaun, A. Buchacher, N. Sullivan, K. Srinivasan, J. Sodroski, J. P. Moore, and H. Katinger. 1996. Human monoclonal antibody 2G12 defines a distinctive neutralization epitope on the gp120 glycoprotein of human immunodeficiency virus type 1. J. Virol. 70:1100-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van't Wout, A. B., H. Blaak, L. J. Ran, M. Brouwer, C. Kuiken, and H. Schuitemaker. 1998. Evolution of syncytium-inducing and non-syncytium-inducing biological virus clones in relation to replication kinetics during the course of human immunodeficiency virus type 1 infection. J. Virol. 72:5099-5107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wong, J. K., M. Hezareh, H. F. Günthard, D. V. Havlir, C. C. Ignacio, C. A. Spina, and D. D. Richman. 1997. Recovery of replication-competent HIV despite prolonged suppression of plasma viremia. Science 278:1291-1295. [DOI] [PubMed] [Google Scholar]