Abstract
We compared the effects of DQ-113, a new quinolone, to those of vancomycin (VCM) and teicoplanin (TEIC) in murine models of hematogenous pulmonary infections caused by methicillin-resistant Staphylococcus aureus (MRSA) and VCM-insensitive S. aureus (VISA). The MICs of DQ-113, VCM, and TEIC for MRSA were 0.125, 1.0, and 0.5 μg/ml, respectively; and those for VISA were 0.25, 8.0, and 8.0 μg/ml, respectively. Treatment with DQ-113 resulted in a significant decrease in the number of viable bacteria in the lungs of the mice used in the MRSA infection model (counts in mice treated with DQ-113, VCM, and TEIC and control mice, 6.33 ± 0.22, 7.99 ± 0.14, 7.36 ± 0.20, and 8.47 ± 0.22 log10 CFU/lung [mean ± standard error of the mean], respectively [P < 0.01 for the group treated with DQ-113 compared with the group treated with VCM or TEIC or the untreated group]). Mice infected with VISA were pretreated with cyclophosphamide, and the survival rate was recorded daily for 10 days. At the end of this period, 90% of the DQ-113-treated mice were still alive, whereas only 45 to 55% of the mice in the other three groups were still alive (P < 0.05 for the group treated with DQ-113 compared with the group treated with VCM or TEIC or the untreated group]). DQ-113 also significantly (P < 0.05) reduced the number of viable bacteria in the lungs compared with those in the lungs of the other three groups (counts in mice treated with DQ-113, VCM, and TEIC and control mice, 5.76 ± 0.39, 7.33 ± 0.07, 6.90 ± 0.21, and 7.44 ± 0.17 log10 CFU/lung, respectively). Histopathological examination revealed milder inflammatory changes in DQ-113-treated mice than in the mice in the other groups. Of the antibiotics analyzed, the parameters of area under the concentration-time from 0 to 6 h (AUC0-6)/MIC and the time that the AUC0-6 exceeded the MIC were the highest for DQ-113. Our results suggest that DQ-113 is potent and effective for the treatment of hematogenous pulmonary infections caused by MRSA and VISA strains.
Methicillin-resistant Staphylococcus aureus (MRSA) was first identified in the 1960s and was reported to colonize the upper respiratory tract and to cause severe infections, such as pneumonia, pulmonary abscesses, and septicemia. MRSA infection develops mainly in inpatients with risk factors related to health care (5), although it has also recently been described in the general population (1). Glycopeptides, such as vancomycin (VCM) and teicoplanin (TEIC), are the most reliable therapeutic agents against infections caused by MRSA. However, the first report of a Japanese patient harboring an MRSA strain resistant to VCM appeared in 1996 (3). Subsequent isolation of several VCM-resistant S. aureus (or VCM-insensitive S. aureus [VISA]) strains from the United States, France, Korea, South Africa, and Brazil confirmed that the emergence of VCM resistance in S. aureus is a global issue (9). Thus, some new agents with activities against MRSA and VISA, such as linezolid, daptomycin, and quinupristin-dalfopristin, have been developed (6). Tanaka et al. (10) reported that DQ-113, a new quinolone-type antibacterial agent, showed potent in vitro activities against various bacteria, including multiple-resistant strains, such as MRSA, VISA, and penicillin-resistant Streptococcus pneumoniae. It is expected that DQ-113 will be effective against severe staphylococcal infections, such as pneumonia, septicemia, and pulmonary abscesses.
A murine model of pulmonary infection with S. aureus by intravenous injection of bacteria enmeshed in agar beads was previously established (8) to evaluate the efficacies of antibiotics and the pathogenesis of blood-borne staphylococcal pneumonia. In the present study, we used the model to evaluate the antibacterial and histopathological effects of DQ-113 against MRSA and VISA by comparing these effects with those of VCM and TEIC.
MATERIALS AND METHODS
Laboratory animals.
Six-week-old male specific-pathogen-free ddY mice (body weight, 25 to 30 g) were purchased from Shizuoka Agricultural Cooperative Association Laboratory Animals (Shizuoka, Japan). All animals were housed in a pathogen-free environment and received sterile food and water ad libitum in the Laboratory Animal Centre for Biomedical Science at Nagasaki University. The Ethics Review Committee for Animal Experimentation at our institution approved in advance all experimental protocols described in this study.
Bacterial strain.
Two strains of S. aureus were examined. Strain NUMR101 was isolated clinically at Nagasaki University Hospital from blood samples of infected patients. Mu50, a VCM-insensitive strain, was kindly provided by K. Hiramatsu (Juntendo University, Tokyo, Japan) (3). The bacteria were stored at −70°C in brain heart infusion broth (BBL Microbiology System, Cockeysville, Md.) supplemented with 10% (vol/vol) glycerol and 5% (wt/vol) skim milk (Yukijirushi Co., Tokyo, Japan) until use.
MIC determinations.
DQ-113 (Daiichi Pharmaceutical Co., Tokyo, Japan) was dissolved in 0.01 N NaOH-2% glucose-1 mM phosphate-buffered saline. VCM (Shionogi Pharmaceutical Co., Tokyo, Japan) and TEIC (Aventis Pharmaceutical Co., Tokyo, Japan) were dissolved in sterile water immediately before use. The MIC of each agent was determined by the microplate dilution technique with Mueller-Hinton medium and an inoculum of 5 × 105 CFU/ml. The MIC was defined as the lowest concentration of the test drug that inhibited visible growth of the bacteria after 18 h of incubation at 37°C.
Inoculum.
The method of inoculation was described previously (8). S. aureus was cultured on a Trypticase soy agar (BBL Microbiology Systems)-based sheep blood agar plate for 24 h at 37°C. The bacteria were suspended in endotoxin-free sterile saline and harvested by centrifugation (3,000 × g, 4°C, 10 min). The microorganisms were resuspended in cold sterile saline and diluted to 2 × 109 to 4 × 109 CFU/ml, as estimated by turbidimetry. The suspension was warmed to 45°C, and then 10 ml of the suspension was mixed with 10 ml of 4% (wt/vol) molten Noble agar (Difco Laboratories, Detroit, Mich.) at 45°C. The agar-bacterium suspension (1.0 ml) was placed in a 1.0-ml syringe, and the suspension was rapidly injected with a 26-gauge needle into 49 ml of rapidly stirred ice-cooled sterile saline. This resulted in solidification of the agar droplets into beads of approximately 200 μm in diameter. The final concentration of agar was 0.04% (wt/vol), and the final number of bacteria was 2 × 107 to 4 × 107 CFU/ml.
Because of the low level of pathogenicity of Mu50, mice infected with VISA were pretreated with cyclophosphamide (100 mg/kg) at 1 and 3 days before inoculation, and the survival rate was recorded daily over a period of 10 days (12).
Experimental model.
We injected 0.20 to 0.25 ml of the agar beads that contained the bacteria and that were suspended in saline into the tail vein of each mouse (10 ml/g of body weight). Before the bacteria were enmeshed in the agar beads, we verified their numbers by inoculating duplicates of serial dilutions onto blood agar plates and counting the number of CFU after 48 h of incubation at 37°C. The method used to induce infection has previously been described in detail (8). Treatment commenced a day after inoculation by intraperitoneal administration of antibiotics. For the study with MRSA, 45 animals received one of the following eight treatments: DQ-113 (40 mg/kg of body weight/day; n = 6), VCM (40, 80, or 160 mg/kg/day; n = 6 each), TEIC (40, 80, or 160 mg/kg/day; n = 6, 5, and 5, respectively), or no treatment (controls; n = 5). Each drug was administered twice daily (every 12 h) for 7 days. We also conducted a survival study and a bacteriological study with VISA. Mice infected with VISA were pretreated with cyclophosphamide. In the survival study, the mice were treated every 12 h with 40 mg/kg/day for 10 days (n = 20). In the bacteriological study, 24 animals received one of the following four treatments: DQ-113 (40 mg/kg/day; n = 6), VCM (40 mg/kg/day; n = 6), TEIC (40 mg/kg/day; n = 6), or no treatment (controls; n = 6). We investigated the number of viable bacteria in the lungs after 7 days of treatment.
Bacteriological, survival, and histopathological examinations.
Each group of animals was killed by cervical dislocation at specific time intervals. After exsanguination, the lungs were dissected and removed under aseptic conditions. The organs used for bacteriological analyses were homogenized and cultured quantitatively by serial dilution on blood agar plates. Lung tissue for histological examination was fixed in 10% buffered formalin and stained with hematoxylin-eosin.
Lung and serum drug concentrations in mice.
The animals were killed by cervical dislocation at 0.25, 0.5, 1, 2, 4, and 6 h after treatment. Serum was separated after the blood had clotted. Four animals were used for each group. The lungs were removed, washed briefly, and cryohomogenized with saline. These samples were immediately frozen and stored at −80°C for a few days until the assay was performed. The concentration of DQ-113 was measured by the paper disk (bioassay) method (4). The test organism was Bacillus subtilis ATCC 6633. The concentrations of VCM and TEIC were measured by fluorescence polarization immunoassay (7). Pharmacokinetic parameters were calculated from the arithmetic mean concentrations in serum and lung tissue.
Statistical analysis.
Bacteriological data were expressed as means ± standard errors of the means (SEMs). Survival data were compared by plotting Kaplan-Meier curves. Differences between groups were examined for statistical significance by the unpaired t test for MRSA and the log-rank test for VISA. A P value less than 0.05 denoted the presence of a statistically significant difference.
RESULTS
Therapeutic effects of antibiotics.
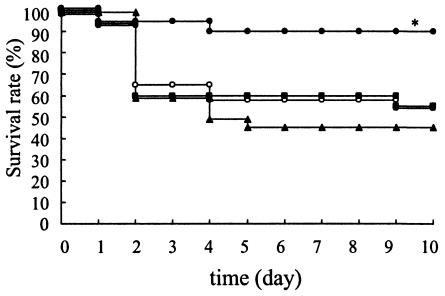
Treatment with VCM (40 or 80 mg/kg/day) did not reduce the number of viable bacteria in the lungs relative to the number in the lungs of the controls (VCM at 40 mg/kg/day, 7.99 ± 0.14 log10 CFU/lung; VCM at 80 mg/kg/day, 8.15 ± 0.18 log10 CFU/lung; controls, 8.47 ± 0.22 log10 CFU/lung [n = 6, 6, and 5, respectively]). Treatment with VCM (160 mg/kg/day) or TEIC (40, 80, or 160 mg/kg/day) reduced the number of viable bacteria in the lungs relative to the number in the lungs of the controls (VCM at 160 mg/kg/day, 7.15 ± 018 log10 CFU/lung; TEIC at 40 mg/kg/day, 7.36 ± 0.20 log10 CFU/lung; TEIC at 80 mg/kg/day, 7.66 ± 0.18 log10 CFU/lung; TEIC at 160 mg/kg/day, 6.95 ± 0.27 log10 CFU/lung [n = 6, 6, 5, and 5, respectively]). In contrast, administration of DQ-113 at 40 mg/kg/day resulted in a significant decrease in the number of viable bacteria compared with the number in the other groups (6.33 ± 0.22 log10 CFU/lung [n = 6] [P < 0.05 versus the counts for the other groups]). The data are representative of those from three independent experiments. In the VISA study, 90% of mice treated with DQ-113 were still alive at the end of the study, while the survival rates were only 45 to 55% for the other three groups (Fig. 1). The differences in survival rates between the group treated with DQ-113 and the other three groups were significant (P < 0.05 for each comparison). The data are representative of those from two independent experiments. DQ-113 also significantly (P < 0.05) reduced the number of viable bacteria in the lungs compared with the number in the lungs of the other three groups (for DQ-113, VCM, TEIC, and the controls, 5.76 ± 0.39, 7.33 ± 0.07, 6.90 ± 0.21, and 7.44 ± 0.17 log10 CFU/lung, respectively [n = 6 for each group]).
FIG. 1.
Effects of DQ-113, VCM, and TEIC on survival rates of animals with hematogenous pulmonary infections caused by VISA. The mice were treated with one of the antibiotics after infection with VISA or were left untreated (controls). The survival rate was determined daily for 10 days. At 10 days, 90% of the mice in the DQ-113-treated group and 45 to 55% of mice in the other three groups (VCM- and TEIC-treated mice and untreated mice) were still alive. DQ-113 significantly improved the survival rate (*, P < 0.05). •, DQ-113; ▴, VCM; ▪, TEIC; □, control.
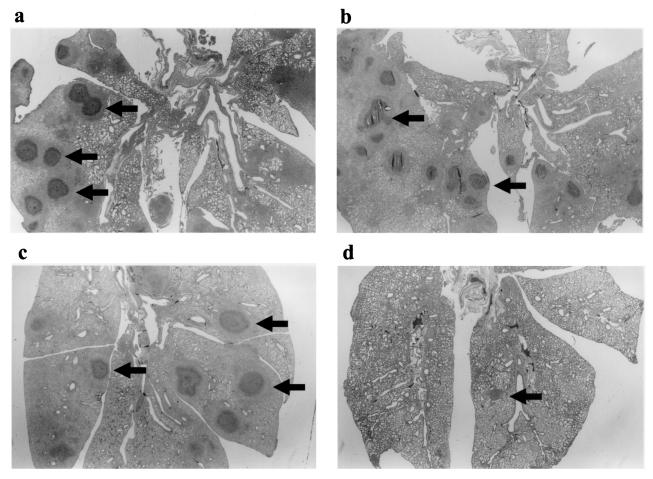
Histopathological examination.
At 7 days after treatment, microscopic examination of lung tissue specimens of mice infected with VISA Mu50 showed lung abscesses consisting of a central zone comprising a bacterial colony with infiltration of acute inflammatory cells (Fig. 2). Findings for the mice treated with VCM (Fig. 2c) and TEIC (Fig. 2b) were similar to those for the control mice (Fig. 2a). DQ-113-treated mice (Fig. 2d) exhibited fewer abscesses and milder inflammatory processes relative to those for the other groups.
FIG. 2.
Histopathological examination of lung specimens from mice killed 10 days after treatment. Each specimen exhibited typical features of lung abscesses consisting of a central zone comprising a bacterial colony with infiltration of acute inflammatory cells (hematoxylin and eosin stain). Arrows show the lung abscesses. (a) control; (b) TEIC-treated group; (c) VCM-treated group; (d) DQ-113-treated group. Note that the severity of the inflammatory process is less in DQ-113-treated mice than in the mice in the other groups. Magnifications, ×5.
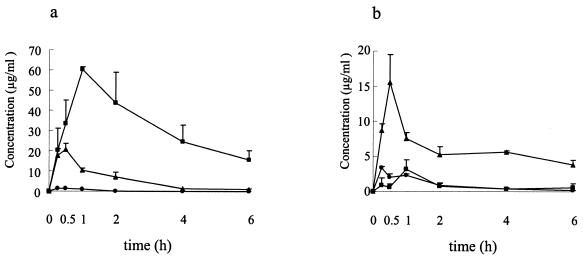
Serum and lung DQ-113, VCM, and TEIC concentrations in mice.
Figure 3a and b shows the mean concentrations of DQ-113, VCM, and TEIC in the sera and lungs of the mice 0.25, 0.5, 1, 2, 4, and 6 h after administration. These data are for MRSA-infected mice, and each drug was administered at 20 mg/kg once a day after inoculation. The peak concentrations of DQ-113, VCM, and TEIC in serum were 1.30 ± 0.23, 20.46 ± 2.98, and 60.40 ± 1.47 μg/ml, respectively (mean ± SEM; n = 4). The peak concentrations of DQ-113, VCM and TEIC in lung tissue were 3.38 ± 0.19, 15.51 ± 4.04, and 3.18 ± 1.34 μg/ml, respectively (mean ± SEM; n = 4). Table 1 shows the pharmacodynamic and pharmacokinetic parameters in the lung tissues of mice with MRSA and VISA infections. The MICs of DQ-113, VCM, and TEIC for NUMR101 were 0.125, 1.0, and 0.5 μg/ml, respectively; and those for Mu50 were 0.25, 8.0, and 8.0 μg/ml, respectively. Of the antibiotics analyzed, the parameters of the area under the concentration-time curve from 0 to 6 h (AUC0-6)/MIC and the time that the AUC0-6 exceeded the MIC (AUC0-6 > MIC)/MIC (AUIC0-6) were the highest for DQ-113.
FIG. 3.
Pharmacokinetics of DQ-113 (20 mg/kg), VCM (20 mg/kg), and TEIC (20 mg/kg) in the sera (a) and lungs (b) of MRSA-infected mice. Each drug was administered intraperitoneally after infection. The results are presented as means ± SEMs. •, DQ-113; ▴, VCM; ▪, TEIC.
TABLE 1.
Selected pharmacokinetic parameter estimates for antibiotics in lung tissues in MRSA and VISA studya
| Antibiotic | Strain | MIC (μg/ml) | AUC0-6 (μg · h/ml) | Cmax (μg/ml) | t1/2 (h) | AUC0-6/MIC (h) | AUC0-6 > MIC (μg · h/ml) | AUIC0-6 (h) |
|---|---|---|---|---|---|---|---|---|
| DQ-113 | MR101 | 0.125 | 5.52 | 3.38 | 1.62 | 44.14 | 5.52 | 44.14 |
| Mu50 | 0.25 | 22.07 | 5.31 | 21.25 | ||||
| VCM | MR101 | 1 | 36.36 | 15.51 | 6.26 | 36.36 | 36.34 | 36.34 |
| Mu50 | 8 | 4.54 | 8.68 | 1.08 | ||||
| TEIC | MR101 | 0.5 | 5.32 | 3.18 | 2.25 | 10.65 | 4.08 | 8.15 |
| Mu50 | 8 | 0.67 | 0 | 0 |
The pharmacokinetic data are for MRSA-infected mice. Each drug was administered at 20 mg/kg once a day after inoculation. Pharmacokinetic parameters were calculated from the arithmetic means of the concentrations in lung tissue (mean values for four animals). Cmax, maximum concentration; t1/2, half-life.
DISCUSSION
In the present study, we were successful in inducing severe pneumonia and lung abscesses in VISA Mu50-infected immunocompromised mice, resulting in the death of 60% of the mice at 10 days after infection. While VCM and TEIC had no effect on the survival rate, DQ-113 protected the mice against fatal pneumonia and resulted in a significant reduction in the mortality rate. VCM and TEIC had insufficient effects in the model because they poorly penetrated lung tissue. VCM and TEIC were effective in a dose-dependent manner in the MRSA study.
In our model of hematogenous pulmonary infection, the new oxazolidinone antimicrobial linezolid significantly reduced the number of MRSA organisms and improved the survival rates of mice infected with VISA compared to the effects of VCM and TEIC (12). Our present data suggest that DQ-113 is a potent antimicrobial agent against VISA infection as well as MRSA, similar to linezolid.
VCM-resistant S. aureus was recently isolated in the United States. In a study published by the Centers for Disease Control and Prevention (2), the MICs of VCM, TEIC, and oxacillin for VISA were >128, 32, and 16 mg/ml, respectively. The isolate contained the vanA VCM resistance gene from enterococci, which is consistent with the glycopeptide MIC profiles (2).
The new oxazolidinone antimicrobial linezolid has been approved for use for the treatment of infections caused by various gram-positive bacteria, including MRSA and VCM-resistant enterococci. However, one MRSA strain resistant to linezolid has already been isolated from a patient treated with this agent for dialysis-associated peritonitis (11). These reports emphasize the need to develop antimicrobial agents potent against VISA. The available in vitro data (10) and the present results suggest that DQ-113 is a promising and potent candidate. In the pharmacokinetic study, the AUC/MIC and AUIC values for DQ-113 were the highest of those for the antibiotics analyzed. A recent brief report showed that DQ-113 accumulates at higher concentrations than other quinolones, suggesting that both its high intracellular concentrations and its inhibitory activities against target enzymes contribute to its potent antibacterial activity (M. Tanaka, T. Akasaka, Y. Onodera, M. Yoshihara, T. Takemura, and K. Sato, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. 552, 2001).
In conclusion, we have demonstrated in the present study that DQ-113, a novel antibacterial quinolone, effectively reduced the number of bacteria in MRSA and VISA hematogenous infection models and significantly improved the rates of survival of immunocompromised mice infected with VISA compared with the rates achieved with VCM and TEIC.
Acknowledgments
We thank F. G. Issa for assistance with editing the manuscript.
REFERENCES
- 1.Centers for Disease Control and Prevention. 1999. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus: Minnesota and North Dakota, 1997-1999. Morb. Mortal. Wkly. Rep. 48:707-710. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2002. Staphylococcus aureus resistant to vancomycin—United States, 2002. Morb. Mortal. Wkly. Rep. 51:565-567. [PubMed] [Google Scholar]
- 3.Hiramatsu, K., H. Hanaki, T. Ino, K. Yabuta, T. Oguri, and F. C. Tenover. 1997. A methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J. Antimicrob. Chemother. 40:135-146. [DOI] [PubMed] [Google Scholar]
- 4.Kohno, S., H. Koga, K. Yamaguchi, M. Masaki, Y. Inoue, Y. Dotsu, Y. Masuyama, T. Hayashi, M. Hirota, A. Saito, and K. Hara. 1989. A new macrolide, TE-031 (A-56268), in treatment of experimental Legionnaire's disease. J. Antimicrob. Chemother. 24:397-405. [DOI] [PubMed] [Google Scholar]
- 5.Lowy, F. D. 1998. Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532. [DOI] [PubMed] [Google Scholar]
- 6.Rybak, M. J., E. Hershberger, T. Moldvan, and R. G. Grucz. 2000. In vitro activities of daptomycin, vancomycin, linezolid, and quinupristin-dalfopristin against staphylococci and enterococci, including vancomycin-intermediate and -resistant strains. Antimicrob. Agents Chemother. 44:1062-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rybak, M. J., E. M. Bailey, and V. N. Reddy. 1991. Clinical evaluation of teicoplanin fluorescence polarization immunoassay. Antimicrob. Agents Chemother. 35:1586-1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sawai, T., K. Tomono, K. Yanagihara, Y. Yamamoto, M. Kaku, Y. Hirakata, H. Koga, T. Tashiro, and S. Kohno. 1997. Role of coagulase in a murine model of hematogenous pulmonary infection by intravenous injection of Staphylococcus aureus enmeshed in agar beads. Infect. Immun. 65:466-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith, T. L., M. L. Pearson, K. R. Wilcox, C. Cruz, M. V. Lancaster, B. Robinson-Dunn, F. C. Tenover, M. J. Zervos, J. D. Band, E. White, and W. R. Jarvis. 1999. Emergence of vancomycin resistance in Staphylococcus aureus. N. Engl. J. Med. 340:493-501. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka, M., E. Yamazaki, M. Chiba, K. Yoshihara, T. Akasaka, M. Takemura, and K. Sato. 2002. In vitro antibacterial activities of DQ-113, a potent quinolone, against clinical isolates. Antimicrob. Agents Chemother. 46:904-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsiodras S., H. S. Gold, G. Sakoulas, G. M. Eliopoulos, C. Wennersten, L. Venkataraman, R. C. Moellering, and M. J. Ferraro. 2001. Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet 358:207-208. [DOI] [PubMed] [Google Scholar]
- 12.Yanagihara K., Y. Kaneko, T. Sawai, Y. Miyazaki, K. Tsukamoto, Y. Hirakata, K. Tomono, J. Kadota, T. Tashiro, I. Murata, and S. Kohno. 2002. Efficacy of linezolid against methicillin-resistant or vancomycin-insensitive Staphylococcus aureus in a model of hematogenous pulmonary infection. Antimicrob. Agents Chemother. 46:3288-3291. [DOI] [PMC free article] [PubMed] [Google Scholar]