Abstract
Objective:
This study aimed at exploring the psychosocial and clinical correlates of substance use disorder in an adolescent inpatient psychiatric population.
Method:
During the period from 2006–2007, all subjects were systematically screened for substance use disorder (SUD) and were assessed for SUD characteristics by an independent support team using the RECAP (Joint Report on Drug Addiction and Treatment). Each SUD case was matched for age, gender, unit, and admission week, so as to compare a consumer sample (cases) with a non-consumer sample (controls). We retrospectively extracted data (socio-demographic and clinical characteristics) from charts to realize a case-control comparison. To assess Axis II borderline psychopathology, the child retro-DIB (Diagnosis Interview for Borderline) was used.
Results:
The sample included 30 cases and 30 controls between 14 and 17 years of age. SUD was significantly associated with maltreatment (p=0.038), loss of a first-degree relative (p=0.039), school absenteeism (p=0.035) and suicide attempts (p=0.02). Regarding psychopathology, significant co-occurrence was observed between SUD and conduct disorder (p=0.019), all personality disorders (p=0.003) and borderline personality disorder specifically (p=0.021).
Conclusion:
Adolescent inpatients with SUD possess differential psychosocial and clinical characteristics and particular correlates that justify adopting a specific multidisciplinary approach to this high-risk clinical subgroup.
Keywords: substance use disorder, psychiatric disorder, personality disorder, adolescent, inpatients
Résumé
Objectif:
Explorer les corrélats psychosociaux et cliniques de la consommation de substances dans une population d’adolescents hospitalisés en psychiatrie.
Méthodologie:
De 2006 à 2007, une équipe de soutien indépendante a utilisé le programme RECAP pour procéder à un dépistage systématique des troubles liés à la consommation de substances et pour évaluer les caractéristiques de ce trouble. Les sujets ont été appariés par âge, sexe, unité et semaine d’admission, puis comparés à un échantillon témoin. Nous avons comparé les sujets de l’étude aux sujets témoins en utilisant les données sociodémographiques et cliniques extraites des dossiers: The Diagnostic Interview for Borderline Patients (Interview diagnostique pour patient souffrant d’un trouble de personnalité limite) a servi à évaluer la psychopathologie de l’axe II.
Résultats:
L’échantillon était composé de 30 sujets et de 30 témoins âgés de 14 à 17 ans. La consommation de substances était en forte corrélation avec les mauvais traitements (p = 0,038), la perte d’un parent au premier degré (p = 0,039), l’absentéisme scolaire (p = 0,035) et les tentatives de suicide (p = 0,02). Au niveau psychopathologique, on a constaté une corrélation significative entre les troubles liés à la consommation de substances et les troubles de conduite (p = 0,019), les troubles de personnalité (p = 0,003) et le trouble de la personnalité limite (p = 0,021).
Conclusion:
Les caractéristiques psychosociales et cliniques des patients d’une unité interne qui affichent des troubles liés à la consommation de substances sont différentes de celles des autres patients; les corrélations particulières présentées par ce sous-groupe à risque élevé justifient une approche multidisciplinaire spécifique.
Keywords: trouble lié à la consommation de substances, trouble psychiatrique, trouble de la personnalité, adolescent, patient hospitalisé
Introduction
Adolescence is a particularly challenging period in the course of development. It is also a critical time for the development of psychiatric disorders, as many adolescents are at great risk for developing substance use related disorders (Burke et al., 1990). Substance use and abuse among adolescents are viewed as major public health problems. The adolescent psychiatric inpatient population is at an even higher risk of use, abuse, and dependence on legal and illegal psychotropic substances. Niethammer (2007) examined the prevalence of use, abuse, and dependence on psychoactive substances in an adolescent inpatient psychiatric population and found a high prevalence of use and substance use disorder (SUD). Around 76% of subjects reported regular use of tobacco, 44% reported regular alcohol use, and 40% reported regular use of illegal substances. Diagnosis (abuse or dependence) was made in 50% of cases for nicotine, 29% for alcohol, and 26% for illegal substances (Niethammer et al., 2007). In France, the OFDT (French Monitoring Centre for Drugs and Drug Addictions) carries out a national statistical survey among 17-year-old teenagers (ESCAPAD) every 4 years. This survey is carried out during the Journée d’Appel et Préparation à la Défense (JAPD, [Army Prepartion Day]). It focuses on health, drug use and lifestyles. Around 28.9% of adolescents reported regular use of tobacco, 8.9% reported regular alcohol use and 7.3% reported regular use of cannabis. Diagnoses of abuse or dependence was made in 7.7% of cases for nicotine, 8.8% for alcohol and 3.2% for cannabis. Such findings make it clear that SUD is a major issue in adolescent psychiatric patients. It is important to diagnose these disorders and to install preventive and therapeutic programs in clinical therapeutic settings.
Adolescent SUDs are associated with most psychiatric disorders, but systematic studies on coexisting psychiatric disorders among adolescent SUDs are sparse. The published literature on comorbidity shows huge variations in methodology (e.g., retrospective vs. prospective, parent report vs. self-report), population (e.g., inpatient vs. outpatient) and focus (e.g., general psychiatry vs. drug use treatment programs). It is therefore very hard to make comparisons between the results of previous studies. Research with adolescents has documented that psychiatric problems frequently co-occur with substance use problems, most notably mood disorders, conduct disorders, attention-deficit hyperactivity disorder, and anxiety disorders. (Baker et al., 2007; Bukstein et al., 1989; Deas et al., 2006; Demilio et al., 1989; Godstein et al., 2008; Grilo et al., 1996; Hovens et al., 1994; Stowell et al., 1992; Swadi et al., 2003;). Few studies, however, have examined comorbidity in an inpatient adolescent population (Bukstein et al., 1992; Grilo et al., 1995; Hovens et al., 1994; Stowell et al., 1994). SUD in adolescents has been associated with family or parenting problems in several studies of nonclinical populations (McKay et al., 1991). Some of the factors that have been most consistently implicated as having etiological significance include parental drug use and school failure. Ethnic differences in the predictors of drug and alcohol abuse have also been observed (Becker et al., 2007). One risk factor for early onset of substance abuse that has received only a modicum of attention from clinicians is child maltreatment (Van Hasselt et al., 1992). Descriptive reports suggest an association between both physical and sexual abuse and subsequent use of alcohol or drugs.
This study sought to retrospectively examine psychosocial and clinical correlates of SUD in an adolescent inpatient psychiatric population belonging to a large catchment area.
Methods
Sample
Participants were adolescents diagnosed with SUD who had been hospitalized in the department of child and adolescent psychiatry at Pitié-Salpêtrière University Teaching Hospital (Paris) between January 2006 and December 2007. The department runs 1/3 of the acute inpatient facilities offered for a catchment area of 8 millions. It is organized with three separate inpatient adolescent units according to age (11–14 vs. 15–18) and severity (intensive care vs. acute inpatient care). In the department, drug consumption is systematically and prospectively screened using a nurse interview on admission. The interview is repeated after one week of stay. Inclusion criteria were:
SUD, including abuse and dependence, that were reported to ECIMUD (coordination and medical care team for drug addicts); and
inpatient admission.
Exclusion criteria were as follows:
exclusive tobacco consumers (who are not systematically reported to ECIMUD);
outpatients;
SUD adolescents admitted or transferred to another department for somatic disease; and (4) those discharged against medical advice.
Over the study period, 410 adolescents were admitted into the service. Among them, 30 (7.3%) adolescents were referred to ECIMUD and were consequently included in the SUDs group. Each case was matched with a non-SUD hospitalized adolescent for age, gender, inpatient unit, and time of admission, so as to compare a SUDs group (cases, N=30) with a non-SUD group (controls, N=30). Of the 60 subjects, 32 (53.3%) were male and 28 (46.7%) were female. The mean age was 15.82 (± 0.98) years. Age ranged between 14 and 17 at the time of admission. Forty patients (66.6%) were Caucasian, 9 (15%) were African, 7 (11.7%) were Asian, and 4 (6.7%) were of other ethnicities. Twenty-nine patients (48.3%) were from immigrant families. Reason for referral and DSM-IV diagnoses are detailed in Table 2 and 3.
Table 2.
Sociodemographic and characteristics, and history of adolescent inpatients with substance use disorder (N=30) versus non abuser adolescent inpatients (N=30) matched for age, sex and in-patient unit
| Case (N = 30) | Control (N = 30) | P | |
|---|---|---|---|
| Sociodemographics | |||
| Age, mean (±SD) [range], years | 15.82 (± 0.98) [14–17] Caucasian 40 (66.6%), Other 20 (33.4%) |
||
| Origin | |||
| Psychosocial background: N (%) | |||
| Unstable family | 7 (23.3%) | 4 (13.3%) | 0.51 |
| Unstable institutional care | 6 (20%) | 5 (16.7%) | 1 |
| Parental separation | 16 (53.3%) | 17 (56.7%) | 1 |
| First degree loss | 12 (40%) | 4 (13.3%) | 0.039 |
| School absenteeism | 22 (73.3%) | 13 (43.3%) | 0.035 |
| Maltreatment | 19 (63.3%) | 10 (33.3%) | 0.038 |
| Orphan or adopted child | 4 (13.3%) | 4 (13.3%) | 1 |
| Educational support | 17 (56.7%) | 12 (40%) | 0.30 |
| History: N (%) | |||
| Personal psychiatric history | 23 (76.7%) | 23 (76.7%) | 1 |
| Prior hospitalization | 16 (53.3%) | 13 (43.3%) | 0.61 |
| N of hospitalization ≥2 | 16 (53.3%) | 10 (33.3%) | 0.19 |
| N of suicide attempts ≥1 | 19 (63.3%) | 10 (33.3%) | 0.02 |
| Family psychiatric history | 24 (80%) | 19 (63.3%) | 0.23 |
| Family history of substance use | 10 (33.3%) | 4 (13.3%) | 0.12 |
| Reason for referral | |||
| Acute psychiatric state | 27 (90%) | 30 (100%) | 0.24 |
| Substance withdrawal | 5 (16.7%) | 0 | 0.05 |
| Hospitalization characteristics | |||
| In-patient duration, mean (±SD), weeks | 9.24 (± 9.1) | 10.8 (± 11) | |
| Cumulated duration of hospitalization | 17.5 (± 23.9) | 14.6 (± 14.2) | |
| GAF at admission, mean (±SD) | 32.0 (± 8.5) | 28.1 (±10.5) | |
| Ä Global Assessment Functioning* | 24.8 (± 13.9) | 27.5 (± 10) | 0.38 |
[Global Assessment Functioning at admission - Global Assessment Functioning at discharge]
Table 3.
Psychopathological characteristics of adolescent in-patients with substance use disorder (N=30) versus controls matched for age, sex and in-patient unit (N=30)
| Case (N=30) | Control (N=30) | p | |
|---|---|---|---|
| Current DSM-IV Axis I diagnosis: N (%)a | |||
| All psychotic disorders | 9 (30%) | 9 (30%) | 1 |
| Including brief psychotic episode | 5 (16.7%) | 2 (6.7%) | 0.4 |
| pharmaco-psychosis | 3 (10%) | 0 | 0.24 |
| All mood disorders | 12 (40%) | 14 (46.7%) | 0.79 |
| Including major depressive episode | 8 (26.7%) | 7 (23.3%) | 1 |
| bipolar I | 2 (6.7%) | 5 (16.7%) | 0.42 |
| with psychotic features | 3 (10%) | 7 (23.3%) | 0.3 |
| All anxiety disorders | 3 (10%) | 2 (6.7%) | 1 |
| Including post traumatic stress disorder | 2 (6.7%) | 1 (3.3%) | 1 |
| Conversion | 0 | 1 (3.3%) | 1 |
| Eating disorder | 2 (6.7%) | 0 | 0.49 |
| Organic condition | 3 (10%) | 2 (6.7%) | 1 |
| Intellectual disability | 0 | 9 (30%) | 0.24 |
| Pervasive developmental disorder | 0 | 3 (10%) | 0.24 |
| Conduct disorder | 21 (70%) | 3 (10%) | 0.019 |
| Current DSM-IV Axis II diagnosis: N (%) | |||
| All personality disorders | 18 (60%) | 6 (20%) | 0.003 |
| Including borderline personality disorderb | 10 (33.3%) | 2 (6.7%) | 0.021 |
| narcissistic personality disorder | 5 (16.7%) | 3 (10%) | 0.71 |
| C-Retro-DIB scores | |||
| Social adaptation | 4.8 (± 1.3) | 3.5 (± 1.9) | 0.005 |
| Impulsivity | 5.6 (± 2.3) | 2.6 (± 1.9) | <0.001 |
| Affects | 2.6 (± 1.9) | 1.4 (± 1.7) | 0.018 |
| Psychosis | 3.1 (± 2.9) | 4.3 (± 2.9) | 0.13 |
| Interpersonal relationship | 2.3 (± 2.3) | 0.8 (± 1.2) | 0.01 |
| Total score | 5.8 (± 2.3) | 4 (± 1.9) | <0.001 |
More than one diagnosis was given to many subject. Therefore, the percentage total is greater than 100.
Validated by the C-DIB-R.
Procedure
At Pitié-Salpétrière Hospital (GHPS), inpatients positively screened for substance use who were admitted to the department of child and adolescent psychiatry were reported to ECIMUD (the hospital coordination and medical care team for drug addiction) for proper diagnostic assignment. Final diagnoses were made by the ECIMUD senior psychiatrist. ECIMUD is a mobile transverse hospital unit that intervenes with drug-addicted patients. Systematic evaluation of the substance use and habits was conducted via a semi-structured interview which allowed for scoring the RECAP index (joint report on drug addiction and drug treatment). Criteria used to diagnose the SUDs were DSM-IV-TR criteria for substance abuse and substance dependence.
Following the hospital’s research ethics procedure, we were granted access to the ECIMUD and RECAP medical files of the SUD adolescents hospitalized in the department of child and adolescent psychiatry between January 2006 and December 2007. Two co-authors independently reviewed the charts (clinician and nurse notes) over the hospitalization period. Contradictory data were checked for errors or consensus. When detailed information was insufficient, data were marked as absent. All information pertaining to the identity of the subjects was removed.
Variables and instruments
The variables examined in the medical charts retrospectively were grouped under four headings. The first consisted of socio-demographic data: age, gender, and geographic origin (classified into ethnic origin and immigrant origin).
Hospitalization characteristics were reviewed, including reason for referral, hospitalization unit, admission week, duration of the hospitalization in weeks, and cumulated duration of hospitalization.
Recorded data also included a detailed personal and family psychiatric history. These data consisted of personal psychiatric history, prior hospitalization, number of hospitalizations, number of suicide attempts, family psychiatric history, and family history of substance use.
We documented psychosocial background, including living arrangements (classified into four groups: stable family, unstable family, stable institutional care, unstable institutional care), school absenteeism (partial or complete), orphan or adopted child, first-degree loss, family dysfunction (e.g., parental conflict, parental separation, divorce), maltreatment (e.g., neglect, intrafamilial violence, physical maltreatment, sexual abuse), and educational support.
The overall functioning was prospectively measured with the Children’s Global Assessment Scale, or C-GAS (Shaffer et al., 1983), which is systematically used in the department at admission and discharge (prospective evaluation). It is one of the most widely used measures of the overall severity of disturbance in children and adolescents. It is a unidimensional (global) measure of social and psychiatric functioning for children aged 4 to 16 years. In this study, it had been extended to 17-year-old adolescents. The C-GAS is based on an adaptation of the Global Assessment Scale (GAS) for adults and can be used as an indicator of need for clinical services, a marker for the impact of treatment, or a single index of impairment in epidemiological studies.
SUD was prospectively measured using the RECAP index (joint report on drug addiction and drug treatment) recommended by the EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) and adapted by the OFDT (French monitoring centre for drugs and drug addiction). Records of treatment requests at drug addiction treatment centers kept by RECAP give an idea of the principal characteristics of people undergoing specialized treatment for problems linked to drug use. Data were collected on substances used in the last month, including alcohol, cannabis, opioids, cocaine, crack, amphets, MDMA (3,4-methylenedioxymethamphetamine, also known as ecstasy), other stimulants, LSD, other hallucinogens, solvents, psychotropics, and tobacco. Type of use (no use, abuse, dependence), age at which consumption began, standard number of drinks and frequency of drunkenness during last month (daily alcohol consumption), number of cigarettes smoked per day (tobacco consumption), and history of substance use (first substance other than tobacco and alcohol, age when beginning substance consumption, age when beginning tobacco consumption, age of first drunkenness, and first year of treatment for substance use) were also assessed.
Other psychiatric diagnoses were made using DSM-IV-TR criteria. Axis II diagnoses were investigated with respect to the DSM-IV-TR statement that in order “to diagnose a personality disorder in an individual under 18 years of age, the features must have been present for at least one year” (1, p. 687). Team consensus best-estimate diagnostic method was used. The team included four senior psychiatrists trained for DSM scoring (DC, AC, JMG, ED). Diagnoses were based on all available information, including direct interviews, family history data, and treatment records, and explicit guidelines were developed to resolve discrepancies between data sources (Klein et al., 1994).
In addition, borderline psychopathology was retrospectively rated using the Child and Adolescent Version of the Retrospective Diagnostic Instrument for Borderlines, or C-retro-DIB (Greenman et al., 1986; Ludolph et al., 1990). The retro-DIB parallels the Diagnostic Interview for Borderlines (DIB). Adaptations to children and to adolescents have been made by Greenman and Ludolph (1991) respectively, to allow for retrospective (DIB-R) diagnoses of borderline personality disorder. This specific and sensitive semi-structured instrument is widely used for reviewing charts with regard to borderline psychopathology, covering the following five domains: I) social adaptation; II) impulsivity; III) affective disturbances; IV) psychotic features, and V) relationship impairments (e.g. Jaunay et al., 2006; Guzder et al., 1996). The internal consistency was evaluated with Cronbach alpha coefficients and section-total correlations. Alpha coefficients were as follows: .24, .75, .39, .93, .55 and .63 for I, II, III, IV, V sections and the total respectively. Section-total correlations ranged from .11 to .62, the psychosis section’s correlation being the lowest and the relationship section being the highest. A good interrater reliability was established for this instrument (kappa: 0.72).Using a cut-off score of 7, the DIB-R had a sensitivity of 0.88, and a specificity of 0.55 when compared with clinically-derived psychiatric diagnoses (Zanarini et al, 1989).
Statistical analysis
Statistical analyses were performed using R Software Version 2.7 (The R Foundation for Statistical Computing). First, the distribution of the continuous variables was assessed using the Shapiro-Wilk test and the F-test test with regard to the assumption of normality and the assumption of equal variances, respectively. The variables’ frequencies and means were compared between the SUD group and the control group using Chi2 and student t tests. Non-parametric tests were used in case of non-normal distribution, such as Mann-Whitney test for C-DIB-R scores. Secondly, the strength of association between variables was assessed using Pearson correlations. Strength of association was also assessed between groups and variables using Fisher’s exact test. A two-tailed p value <.05 was considered significant for all analyses.
Results
Profile of substance use
Profile of substance use is listed in Table 1. The psychoactive substances predominantly used were tobacco (93.3%), cannabis (70%), alcohol (60%), and MDMA (23.3%). Forty-one cases of dependence were identified: tobacco (70%), cannabis (33.3%), alcohol (16.7 %), opioid (10%, all in intravenous), and MDMA (6.7%). The mean age at onset was 11.6 years (range: 6–14) for tobacco consumption, 13 years (range: 9–15) for cocaine, 13.2 years (range: 9–15) for alcohol and 13.3 years (range: 11–15) for cannabis.
Table 1.
Profile of substance use by adolescent inpatients (N=30)
| N (%)a | Substance abuse N (%)a | Dependence N (%)a | Age at beginning of consumption mean [range], years | |
|---|---|---|---|---|
| Tabacco | 28 (93.3) | 7 (23.3) | 21 (70) | 11.6 [6–14] |
| Cannabis | 21 (70) | 11 (36.7) | 10 (33.3) | 13.3 [11–15] |
| Alcohol | 18 (60) | 13 (43.3) | 5 (16.7) | 13.2 [9–15] |
| MDMA | 7 (23.3) | 5 (16.7) | 2 (6.7) | 14.3 [14–15] |
| Cocaine | 5 (16.7) | 5 (16.7) | 0 | 13 [9–15] |
| Opioid | 3 (10) | 0 | 3 (10) | 14.7 [13–16] |
| LSD | 3 (10) | 3 (10) | 0 | 14.7 [14–16] |
| Amphets | 2 (6.7) | 2 (6.7) | 0 | 14.5 [14–15] |
| Solvents | 1 (3.3) | 1 (3.3) | 0 | 15 |
More than one diagnosis was given to many subject. Therefore, the percentage total is greater than 100.
Socio-demographic, personal and family history, and hospitalization characteristics (Table 2)
Both groups showed severely affected lifetime psychosocial backgrounds. Subjects in the non-SUD group more often lived in stable families (63.3%) or in stable institutional care (6.7%) than did SUDs inpatients (56.7% in stable families and 0% in stable institutional care). Subjects in the SUDs group more often lived in unstable families (23.3%) or in unstable institutional care (20%) than did non-SUD inpatients (13.3% in unstable families and 16.7% in unstable institutional care), but these differences did not reach statistical significance. In addition, 53.3% of the SUDs inpatients and 56.7% of the non-SUD group had experienced at least one parental separation.
Of the SUDs group, 63.3% had been victims of maltreatment (neglect: 46.7 %, intrafamilial violence: 46.7 %, physical maltreatment: 23.3 %, sexual abuse: 13.3%), compared with 33.3% of the non-SUD group (neglect: 23.3%, intrafamilial violence: 26.7%, physical maltreatment: 20%, sexual abuse: 13.3%); the difference was significant (p<0.038). Of the SUDs group, 40% lost a first-degree relative, compared with 13.3% of the non-SUD group (p<0.039). In addition, 73.3% of the SUDs group dropped out of the school system (partial: 33.3% and total: 40%), compared with 43.3% (partial: 13.3% and total: 30%) of the non-SUD group (p<0.035). These results should be regarded as exploratory since they did not remain significant after Bonferroni correction.
Before admission, 53.3% of the SUDs group and 43.3% of the non-SUD group had received inpatient psychiatric treatment (not a significant difference). The number of subjects who attempted suicide more than once was significantly higher in the SUDs group when compared to the non-SUD group (63.3% vs. 33.3%, respectively, p<0.05).
Eighty percent of the SUDs group had a family psychiatric history, and 33.3% had a family history of substance use. In contrast, 63.3% and 13.3% of the non-SUD group had a family psychiatric history and a family history of substance use, respectively (not significant). Although there were no significant differences between SUD and non-SUD inpatients, it is nonetheless important to note the extremely high prevalence of family psychiatric history in both groups.
The mean inpatient duration was 9.24 (±9.1) weeks among SUDs inpatients versus 10.8 (±11) weeks among non-SUD inpatients. Cumulated duration of hospitalization was 17.5 (±23.9) weeks among cases versus 14.6 (±14.2) among controls. The inpatients with and without SUD did not differ with regard to global assessment of functioning, and both groups were in a severe range of psychopathology. Mean GAF scores at admission (± SD) were 32.0 (± 8.5) and 28.1 (± 10.5), respectively.
Psychopathological characteristics
Psychopathology coexisting with substance abuse in adolescents is often encountered in a variety of clinical settings. Table 3 summarizes the distributions of the major DSM-IV-TR Axis I and II diagnoses in both groups. Each patient could be given more than one diagnosis.
Conduct disorder was significantly more frequently reported in the SUD group than in the non-SUD group (70 % and 10 %, respectively, p=0.019). The next most frequently reported Axis I diagnosis was mood disorder, which was present in 40% of SUDs inpatients and 46.7% of non-SUD inpatients. The next most frequent diagnoses were psychotic disorders, which were present in 30% of SUDs inpatients and 30% of non-SUD inpatients. Sixty percent of SUDs inpatients displayed prominent features of personality disorders. In particular, 33.3% of these patients fulfilled the criteria for borderline personality disorder.
As shown in Table 3, the rates of conduct disorder, personality disorders, and borderline personality disorder were significantly higher in the SUDs group when compared to the non-SUD group. Significant co-occurrence was observed between SUD and conduct disorder (p<0.019), all personality disorders (p<0.003), and borderline personality disorder (p<0.021).
In comparison with the non-SUD group, higher scores for the C-R-DIB were found in the SUDs group: social adaptation (p<0.005), impulsivity (p<0.001), affect (p<0.018), and interpersonal relations (p<0.01). Total scores differed significantly, thereby confirming the diagnostic evaluations of the treating psychiatrists (p<0.001). The social adaptation, impulsivity and the overall borderline scores remain significant after Bonferroni adjustments.
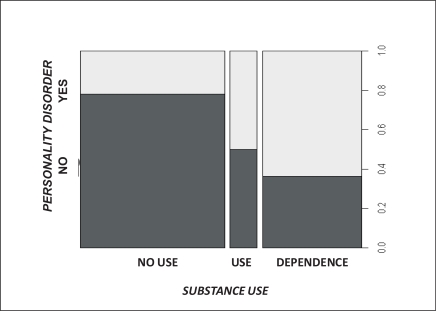
To see if the identified drug of choice correlated with any psychiatric disorder, we compared the rate of the major diagnoses in the adolescents grouped by their drug of choice (Table 4). Personality disorders (more specifically, borderline personality disorder) significantly increased the risk of consuming alcohol. Personality disorders, borderline personality disorder, and conduct disorder significantly augmented the risk of consuming tobacco. Figure 1 shows an association between personality disorders and the degree of substance use (no use, abuse, or dependence). Furthermore, correlations between retro-DIB total score and age at the start of consumption for tobacco, cannabis, and alcohol (the most frequently consumed substance) were calculated with the Pearson correlation coefficient (designated by the letter r.) A significant correlation coefficient was found for tobacco consumption (r=–0.49, t=–2.515, p=0.021) and for alcohol consumption (r=–0.55, t=–2.370, p=0.034). Thus, it appears as though the younger the consumer is at first use, the higher his or her retro-DIB score.
Table 4.
Association between diagnosis and substance use in adolescents in-patients (N=30)
| Odd | 95%CI | p* | Odd | 95%CI | p* | Odd | 95%CI | p* | |
|---|---|---|---|---|---|---|---|---|---|
| CD | 3.1 | 0.8–13.1 | .09 | 3.2 | 0.9–12.2 | .06 | 3.0 | 1.6–20.2 | .04 |
| Borderline | 4.6 | 1.0–22.3 | .03 | 1.4 | 0.3–6.2 | .74 | 4.5 | 1.0–28.9 | .05 |
| All PD | 3.4 | 1.0–13.1 | .04 | 2.2 | 0.7–7.5 | .17 | 5.4 | 1.0–10.3 | .003 |
PD = personality disorder; CD = conduct disorder; 95%CI = 95%Confidence Interval
Fisher’s test
Figure 1.
Presence of personality disorders (yes or no) according to the degree of substance use (no use, abuse or dependence) in adolescent inpatients (N=30)
Discussion
The current study provided a detailed clinical picture of a sample of substance use adolescents hospitalized in a psychiatric setting (a university teaching hospital serving a large catchment area). The aim of this exploratory study was to determine the rate and nature of SUD comorbidity among inpatient youth with severe psychiatric disorders. SUDs in young people differ from those in adults in many ways. This study documented substance use, sociodemographic and hospitalization characteristics, and the history of adolescents. In addition, it examined the possible relationship between substance abuse and certain specific psychiatric disorders and psychosocial correlates in adolescents. Screening is essential to identify those patients who need a further detailed specialist assessment for SUD.
The main limitations of this study are:
the retrospective design;
the limited size of the total population and subgroups; and
the severity of the sample that limits possible generalization to other youth populations.
Our findings would not be generalizable to outpatient or community populations in which base rates of disorders were lower. The strengths of the study are: (a) the multidisciplinary approach, including ECIMUD (coordination and medical care team for drug addicts) and adolescent psychiatrists; and (b) the use of several clinical instruments (C-GAS, C-DIB-R, RECAP index, best-estimate diagnostic method).
Among the psychosocial characteristics, maltreatment appeared as the most striking correlate. Our finding supported the necessity to further investigate the prevalence of maltreatment in psychiatrically hospitalized, dually-diagnosed adolescent substance abusers. Several descriptive reports suggest an association between both physical and sexual abuse and subsequent use of alcohol or drugs (Alfaro, 1981; Dembo et al., 1987; Edwall et al., 1989; Van Hasselt et al., 1992). For example, Van Hasselt (1992) examined the medical charts of 150 consecutive admissions of dually-diagnosed substance abusing adolescents admitted to a psychiatric hospital in order to determine the extent and characteristics of maltreatment. In our study we found that 63% of our sample experienced maltreatment. In previous study, results indicated the same prevalence of maltreatment: 61% of the sample reported a history that warranted suspicion of past and/or current maltreatment. Physical abuse was the most frequent form for maltreatment, followed by sexual abuse and neglect. Furthermore, 37% of patients experienced multiple forms of maltreatment. School absenteeism, which is one of the treatment targets, was also significantly higher among substance consumers. Our results are consistent with a study by Perera (2009), which showed that school absenteeism and substance use are associated with physical and emotional abuse in a population of late adolescents.
Number of suicide attempts was also identified as a psychosocial correlate by substance abusers. Rush (2008) examined the prevalence and profile of inpatients with co-occurring mental and substance use disorders. Having a co-occurring disorder was strongly associated with the risk of suicide or self-harm. The risk of self-harm was also higher in younger people, as well as in those with diagnoses of personality disorders and substance misuse (Gunnell et al., 2008). Multiple attempters were more likely to be diagnosed with at least one externalizing disorder, particularly substance use disorders (D’Eramo et al., 2004). Riala (2009) investigated the degree of nicotine dependence and suicidality among underage adolescents and found that the risk for suicide attempts was increased by a high level of nicotine dependence.
The age at the start of tobacco and alcohol consumption was correlated with retro-DIB total scores. Ribeiro et al. (2008) found an association between conduct disorder and attention-deficit/hyperactivity disorder and an early initiation of tobacco and alcohol use. Early initiation and elevated rates of nicotine and alcohol use were particular risks for adolescents with conduct disorder and attention-deficit/hyperactivity disorder. Early problems with psychoactive substances in adolescence may undermine subsequent personality development (Cohen et al., 2008).
Personality disorders, especially borderline personality disorder (BPD), were diagnosed more frequently in the substance use disorder group. In our study the SUD group presented with a higher rate of borderline traits as evaluated with the C-retro-DIB (p<.001). The co-occurrence of BPD and SUD is a common and clinically relevant phenomenon in need of further empirical investigation. There are numerous ways to explain why BPD would be associated with increased rates of SUDs. First, Gratz (2008) identified the factors associated with co-occurring BPD among substance users, examining the relationships between childhood maltreatment (in the form of sexual, physical, and emotional abuse, and emotional and physical neglect), negative affect intensity/reactivity, emotion dysregulation, and BPD pathology. Results indicated that the presence of a BPD diagnosis was associated with higher levels of both childhood maltreatment and negative affect intensity/reactivity (Gratz et al., 2008). Second, the deficits in affect regulation and impulse control that characterize BPD may also predispose individuals to SUD. In our study, impulsivity scores on the C-DIB-R differed significantly between substance users and non-users. Third, individuals with BPD can be very sensitive to any cue (real or perceived) indicating that they are being rejected or abandoned. This could explain the first-degree loss identified by substance abusers as a psychosocial correlate. Finally, Cohen (2008) documented associations between BPD and SUDs in general adolescent populations and examined how early manifestations of personality disorders might influence the developmental course of SUDs from adolescence to adulthood. These personality disorders in adolescence clearly warrant clinical attention when assessing early risk for SUDs and implementing interventions to prevent and treat those disorders.
Our study highlighted the relationship between SUD and maltreatment and significant losses on the one hand, and SUD and BPD on the other hand. Maltreatment and losses are well-documented childhood risk factors for later BPD (Zelkowitz et al., 2004). Interestingly, adolescent alcohol use disorder has been shown to be a mediating factor in the process leading from childhood maltreatment to adult BPD (Thatcher et al., 2005). In keeping with our results, one could question the role adolescent SUD might play in the development of adult BPD. Further confirmatory studies are needed in order to investigate such a hypothesis.
Conclusion
A major implication of our findings is the need for the simultaneous evaluation of both substance abuse and psychiatric disorders in the adolescent population. These findings can have important therapeutic implications. A multidisciplinary approach (psychiatric, addictive, social, and scholastic) provides the most up-to-date and comprehensive aspects of evaluation and therapy for adolescents. Our results highlight the need to focus on specific subpopulations and sectors in pursuit of more integrated treatment and support for their mental health and addictions problems.
Acknowledgements/Conflict of Interest
The authors have no financial relationships or conflicts to disclose.
References
- Alfaro JD. Report on the relationship between child abuse and neglect and later socially deviant behaviour. In: Hunter RJ, Walker YE, editors. Exploring the relationship between child abuse and delinquency. Montclair, N.J.: Allanheld, Osmun; 1981. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. revised. [Google Scholar]
- Baker KD, Lubman DI, Cosgrave EM, Killackey EJ, Yuen HP, Hides L, Baksheev GN, Buckby JA, Yung AR. Impact of co-occuring substance use on 6 months outcomes for young people seeking mental health treatment. Australian and New Zealand Journal of Psychiatry. 2007;41(11):896–902. doi: 10.1080/00048670701634986. [DOI] [PubMed] [Google Scholar]
- Becker DF, Grilo CM. Prediction of drug and alcohol abuse in hospitalized adolescents: comparisons by gender and substance type. Behaviour Research and Therapy. 2006;44(10):1431–40. doi: 10.1016/j.brat.2005.10.009. [DOI] [PubMed] [Google Scholar]
- Becker DF, Grilo CM. Ethnic differences in the predictors of drug and alcohol abuse in hospitalized patients. American Journal on Addictions. 2007;16(5):389–96. doi: 10.1080/10550490701525343. [DOI] [PubMed] [Google Scholar]
- Bukstein OG, Brent D, Kaminer Y. Comorbidity of substance abuse and other psychiatric disorders in adolescence. American Journal of Psychiatry. 1989;146(9):1131–41. doi: 10.1176/ajp.146.9.1131. [DOI] [PubMed] [Google Scholar]
- Bukstein OG, Glancy LJ, Kaminer Y. Patterns of affective comorbidity in a clinical population of dually diagnosed adolescent substance abusers. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(6):1041–5. doi: 10.1097/00004583-199211000-00007. [DOI] [PubMed] [Google Scholar]
- Children’s Global Assessment Scale (CGAS) Shaffer D, Gould MS, Bird H, Fisher P. APA; Washington, D.C: 2000. Modified From: Rush, J, et al: Psychiatric Measures, [DOI] [PubMed] [Google Scholar]
- Cohen P, Chen H, Crawford TN, Brooks JS, Gordon K. Personality disorders in early adolescence and the development of later substance use disorders in the general population. Drug and Alcohol Dependence. 2007;88(Suppl 1):S71–84. doi: 10.1016/j.drugalcdep.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deas D. Adolescent substance abuse and psychiatric comorbidities. Journal of Clinical Psychiatry. 2006;(Suppl 7):18–13. [PubMed] [Google Scholar]
- Dembo R, Dertke M, La Voie L, Borders S, Washburn M, Schmeider J. Physical abuse, sexual victimization and illicite drug use: a structural analysis among high risk adolescents. Journal of Adolescence. 1987;10:13–33. doi: 10.1016/s0140-1971(87)80030-1. [DOI] [PubMed] [Google Scholar]
- Demilio L. Psychiatric syndromes in adolescent substance abusers. American Journal of Psychiatry. 1989;146(9):1212–4. doi: 10.1176/ajp.146.9.1212. [DOI] [PubMed] [Google Scholar]
- D’Eramo KS, Prinstein MJ, Freeman J, Grapentine WL, Spirito A. Psychiatric diagnoses and comorbidity in relation to suicidal behavior among psychiatrically hospitalized adolescents. Child Psychiatry and Human Development. 2004;35(1):21–35. doi: 10.1023/b:chud.0000039318.72868.a2. [DOI] [PubMed] [Google Scholar]
- Edwall GE, Hoffman NG, Harrison PA. Psychological correlates of sexual abuse in adolescent girls in chemical dependency treatment. Adolescence. 1989;24:279–288. [PubMed] [Google Scholar]
- EMCDDA 2000. Treatment demand indicator, Standard protocol 2.0.
- Goldstein BI, Strober MA, Birmaher B, Axelson DA, Esposito-Smythers C, Goldstein TR, Leonard H, Hunt J, Gill MK, Iyengar S, Grimm C, Yang M, Ryan ND, Keller MB. Substance use disorders among adolescents with bipolar spectrum disorders. Bipolar Disorders. 2008;10(4):469–78. doi: 10.1111/j.1399-5618.2008.00584.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Baruch DE, Bornovalova MA, Lejuez CW. Factors associated with co-occurring borderline personality disorder among inner-city substance users: the roles of childhood maltreatment, negative affect intensity/reactivity, and emotion dysregulation. Comprehensive Psychiatry. 2008;49(6):603–15. doi: 10.1016/j.comppsych.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Greenman DA, Gunderson JG, Cane M, Saltzman PR. An examination of the borderline diagnosis in children. American Journal of Psychiatry. 1986;143(8):998–1003. doi: 10.1176/ajp.143.8.998. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Becker DF, Fehon D, Edell W, McGlashan T. Conduct disorder, substance use disorders, and coexisting conduct and substance use disorders in adolescent inpatients. American Journal of Psychiatry. 1996;153(7):914–920. doi: 10.1176/ajp.153.7.914. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Becker DF, Walker BA, Levy MA, Edell WS, McGlashan TH. Psychiatric comorbidity in adolescent inpatients with substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(8):1085–91. doi: 10.1097/00004583-199508000-00019. [DOI] [PubMed] [Google Scholar]
- Gunnell D, Hawton K, Ho D, Evans J, O’Connor S, Potokar J, Donovan J, Kapur N. Hospital admissions for self harm after discharge from psychiatric inpatient care: cohort study. British Medical Journal. 2008;337:a 2278. doi: 10.1136/bmj.a2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzder J, Paris J, Zelkowitz P, Marchessault K. Risk factors for borderline pathology in children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(1):26–33. doi: 10.1097/00004583-199601000-00009. [DOI] [PubMed] [Google Scholar]
- Harris SK, Kurland M, Knight JR. Substance use problems and associated psychiatric symptoms among adolescents in primary care. Pediatrics. 2003;111:699–705. doi: 10.1542/peds.111.6.e699. [DOI] [PubMed] [Google Scholar]
- Hovens J, Cantwell D, Kiriakos R. Psychiatric comorbidity in hospitalized adolescent substance abusers. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(4):476–83. doi: 10.1097/00004583-199405000-00005. [DOI] [PubMed] [Google Scholar]
- Jaunay E, Consoli A, Greenfield B, Guilé J-M, Mazet P, Cohen D. Treatment refusal in adolescents with severe chronic illness and borderline personality disorder. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2006;15(3):135–42. [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Ouimette PC, Kelly HS, Ferro T, Riso LP. Test-retest reliability of team consensus best-estimate diagnoses of axis I and II disorders in a family study. American Journal of Psychiatry. 1994;151(7):1043–7. doi: 10.1176/ajp.151.7.1043. [DOI] [PubMed] [Google Scholar]
- Legleye S, Spilka S, Le Nézet O, Laffiteau C. Drug use among 17-year-olds. 2009. Results of the 2008 ESCAPAD survey. French Monitoring Centre for Drugs and Drug Addictions. Tendances, 66.
- Ludolph PS, Westen D, Misle B, Jackson A, Wixom J, Wiss FC. The borderline diagnosis in adolescents: symptoms and developmental history. American Journal of Psychiatry. 1990;147(4):470–6. doi: 10.1176/ajp.147.4.470. [DOI] [PubMed] [Google Scholar]
- Niethammer O, Frank R. Prevalence of use, abuse and dependence on legal and illegal psychotropic substances in an adolescent inpatient psychiatric population. European Child and Adolescent Psychiatry. 2007;16(4):254–9. doi: 10.1007/s00787-006-0597-5. [DOI] [PubMed] [Google Scholar]
- McKay JR, Murphy RT, Rivinus TR, Maisto SA. Family dysfunction and alcohol and drug use in adolescent psychiatric inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30(6):967–72. doi: 10.1097/00004583-199111000-00015. [DOI] [PubMed] [Google Scholar]
- OFDT/IDI Rapport de synthèse des travaux du groupe de travail sur le recueil de données auprès des consommateurs de substances psychoactives pris en charge dans les structures de soins. Juillet. 2002.
- Perera B, Ostbye T, Ariyananda PL, Lelwala E. Prevalence and correlates of physical and emotional abuse among late adolescents. Ceylon Medical Journal. 2009;54(1):10–5. doi: 10.4038/cmj.v54i1.466. [DOI] [PubMed] [Google Scholar]
- Perneger TV. What’s wrong with Bonferroni adjustments. British Medical Journal. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riala K, Hakko H, Räsänen P. Study-70 Workgroup. Nicotine dependence is associated with suicide attempts and self-mutilation among adolescent females. Comprehensive Psychiatry. 2009;50(4):293–8. doi: 10.1016/j.comppsych.2008.08.012. [DOI] [PubMed] [Google Scholar]
- Robeiro SN, Jennen-Steinmetz C, Schmidt MH, Becker K. Nicotine and alcohol use in adolescent psychiatric inpatients: associations with diagnoses, psychosocial factors, gender and age. Nordic Journal of Psychiatry. 2008;62(4):315–21. doi: 10.1080/08039480801984073. [DOI] [PubMed] [Google Scholar]
- Rush G, Koegl CJ. Prevalence and profile of people with co-occurring mental and substance use disorders within a comprehensive mental health system. Canadian Journal of Psychiatry. 2008;53(12):810–21. doi: 10.1177/070674370805301207. [DOI] [PubMed] [Google Scholar]
- Stowell R, Estroff T. Psychiatric disorders in substance-abusing adolescent inpatients: a pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(6):1036–40. doi: 10.1097/00004583-199211000-00006. [DOI] [PubMed] [Google Scholar]
- Swadi H, Bobier C. Substance use disorder comorbidity among inpatients youths with psychiatric disorder. Australian and New Zealand Journal of Psychiatry. 2003;37(3):294–8. doi: 10.1046/j.1440-1614.2003.01180.x. [DOI] [PubMed] [Google Scholar]
- Thatcher DL, Cornelius JR, Clark DB. Adolescent alcohol use disorders predict adult borderline personality. Addictive Behaviors. 2005;30(9):1709–24. doi: 10.1016/j.addbeh.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Van Hasselt V, Ammerman R, Glancy L, Bukstein O. Maltreatment in psychiatrically hospitalized dually diagnosed adolescent substance abusers. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(5):868–74. doi: 10.1097/00004583-199209000-00014. [DOI] [PubMed] [Google Scholar]
- Weaver MF, Dupre MA, Cropsey KL, Koch JR, Sood BA, Wiley JL, Balster RL. Addiction epidemiology in adolescents receiving inpatient psychiatric treatment. Addictive Behaviors. 2007;32(12):3107–13. doi: 10.1016/j.addbeh.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The revised diagnostic interview for borderlines: discriminating BPD from other axis II disorders. Journal of Personality Disorders. 1989;3:10–18. [Google Scholar]
- Zelkowitz P, Guzder J, Paris J, Feldman R, Roy C, Schiavetto A. Borderline Pathology of Childhood: Implications of Early Axis II Diagnoses. Canadian Child and Adolescent Psychiatry Review. 2004;13(3):58–61. [PMC free article] [PubMed] [Google Scholar]