Abstract
BACKGROUND
Midurethral slings are increasingly used for the treatment of stress incontinence, but there are limited data comparing types of slings and associated complications.
METHODS
We performed a multicenter, randomized equivalence trial comparing outcomes with retropubic and transobturator midurethral slings in women with stress incontinence. The primary outcome was treatment success at 12 months according to both objective criteria (a negative stress test, a negative pad test, and no retreatment) and subjective criteria (self-reported absence of symptoms, no leakage episodes recorded, and no retreatment). The predetermined equivalence margin was ±12 percentage points.
RESULTS
A total of 597 women were randomly assigned to a study group; 565 (94.6%) completed the 12-month assessment. The rates of objectively assessed treatment success were 80.8% in the retropubic-sling group and 77.7% in the transobturator-sling group (3.0 percentage-point difference; 95% confidence interval [CI], −3.6 to 9.6). The rates of subjectively assessed success were 62.2% and 55.8%, respectively (6.4 percentage-point difference; 95% CI, −1.6 to 14.3). The rates of voiding dysfunction requiring surgery were 2.7% in those who received retropubic slings and 0% in those who received transobturator slings (P = 0.004), and the respective rates of neurologic symptoms were 4.0% and 9.4% (P = 0.01). There were no significant differences between groups in postoperative urge incontinence, satisfaction with the results of the procedure, or quality of life.
CONCLUSIONS
The 12-month rates of objectively assessed success of treatment for stress incontinence with the retropubic and transobturator approaches met the prespecified criteria for equivalence; the rates of subjectively assessed success were similar between groups but did not meet the criteria for equivalence. Differences in the complications associated with the two procedures should be discussed with patients who are considering surgical treatment for incontinence. (ClinicalTrials.gov number, NCT00325039.)
Urinary incontinence affects up to 50% of women, resulting in substantial medical, social, and economic burdens.1,2 Among U.S. women with urinary incontinence, 15 to 80% have a component of stress incontinence,3 which results in leakage of urine during physical exertion, sneezing, and coughing.4 Of these women, 4 to 10% undergo surgery.5
In 1996, Ulmsten et al.6 introduced a procedure that involved the placement of a retropubic midurethral mesh sling for the treatment of stress incontinence; this procedure was less invasive than the Burch colposuspension and the autologous rectus fascial sling procedures that were the reference standards at the time. With the retropubic-sling procedure, a synthetic tape is passed transvaginally at the midurethral level through the retropubic space (Fig. 1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). The success rates of this procedure that have been reported in trials range from 86% to 99%,7,8 and a large, multi-center, randomized trial showed no significant differences in efficacy and safety between this approach and the Burch colposuspension.9 Recognized complications of the retropubic midurethral sling include postoperative voiding difficulties and new symptoms of urgency and urge incontinence, as well as the potential for bladder, bowel, and vascular injury.10,11 Surgeons have performed more than 1 million retropubic-sling procedures,11 and this procedure is increasingly considered to be the standard of care for women who undergo surgical treatment for stress incontinence.
The transobturator approach was developed to minimize the potential for bladder and bowel injuries associated with the retropubic sling, since the sling is passed through the obturator foramen, avoiding the pelvic organs in the retro-pubic space12 (Fig. 1 in the Supplementary Appendix). Meta-analyses of small superiority studies comparing various retropubic and transobturator approaches have suggested that the approaches have similar efficacy; however, the studies were not designed and powered to make robust conclusions about efficacy equivalence and safety.7,8,13 We report the results of a large, multicenter equivalence trial comparing the 12-month efficacy and safety of the transobturator and retro-pubic midurethral slings.
METHODS
STUDY DESIGN AND OVERSIGHT
This was a multicenter, randomized equivalence trial comparing the retropubic midurethral sling with the transobturator midurethral sling for the treatment of stress incontinence. The study methods have been described previously.14 Women 21 years of age or older who were planning to undergo surgery for the treatment of stress incontinence were invited to participate. Eligibility requirements included at least a 3-month history of symptoms of urinary incontinence that were predominantly or solely associated with stress incontinence (as compared with urge incontinence) and a positive urinary stress test at a bladder volume of 300 ml or less (urodynamic stress leakage was not required). Randomization was performed after anesthesia was administered. Women were randomly assigned with the use of a permuted-block randomization schedule, with stratification according to clinical site. After the surgery, information regarding the treatment assignment was not kept from the patient. An institutional review board at each of the nine clinical sites and the coordinating center approved the study protocol. Written informed consent was obtained from all participants. An independent data and safety monitoring board reviewed the progress, interim results, and safety of the study.
STUDY PROCEDURES
The definitions of clinical terms, the methods of evaluation, and key surgical elements, including cystoscopic evaluation, were standardized across centers.4,15 Urodynamic testing, according to standardized protocols, was performed before and 12 months after surgery in accordance with International Continence Society guidelines. Preoperative urodynamic test results were interpreted by an investigator other than the study surgeon; the study surgeon remained unaware of the results throughout the study unless unblinding of the results was necessary for the management of postoperative care. The retropubic sling used was the Tension-free Vaginal Tape (Gynecare); one of two transobturator slings was used: the Tension-free Vaginal Tape Obturator (Gynecare), which is placed starting inside the vagina and coming out through the obturator foramen (“in-to-out”), or the Monarc (American Medical System), which is placed starting in the groin area, passing through the obturator foramen, and then into the vagina (“out-to-in”). The manufacturers of the slings did not provide products for this trial and had no involvement in the design of the trial, the collection or analysis of the data, or the writing of the manuscript. Before the start of the study, the surgeons declared which transobturator sling they would use. Concomitant vaginal surgery was permitted.
OUTCOMES
The composite primary outcome was assessed at 12 months after randomization and included treatment success according to objective criteria and treatment success according to subjective criteria. The objective criteria were a negative provocative stress test, a negative 24-hour pad test, and no retreatment (behavioral, pharmacologic, or surgical) for stress incontinence; the subjective criteria were the absence of self-reported symptoms of stress-type urinary incontinence, as assessed with the use of the Medical, Epidemiological and Social Aspects of Aging (MESA)16 questionnaire, no leakage recorded in a 3-day voiding diary, and no retreatment for stress incontinence. A woman could not be classified as having met the criteria for the primary outcome if she had had a documented treatment failure. Data were collected before surgery and 2 weeks, 6 weeks, and 6 and 12 months after surgery by means of interviews and clinical examinations. The urodynamic measures that were assessed are listed in Table 1. Patient satisfaction was assessed at 12 months with the question, “How satisfied or dissatisfied are you with the result of bladder surgery related to urine leakage?” Possible responses were completely satisfied, mostly satisfied, neutral, mostly dissatisfied, and completely dissatisfied. Completely and mostly satisfied were reported as “satisfied,” and neutral, mostly dissatisfied, and completely dissatisfied as “not satisfied.” The reporting of adverse events and the classification of the severity of events were standardized across sites with the use of specific pre-specified definitions of events and a modified version of the classification system of Dindo et al.17
Table 1.
Demographic, Anthropometric, Clinical, and Urodynamic Characteristics of the Study Population.*
| Characteristic | Retropubic Sling (N = 298) | Transobturator Sling (N = 299) |
|---|---|---|
|
Demographic characteristics† | ||
| Age — yr | 52.7±10.5 | 53.1±11.5 |
|
Race or ethnic group — no. (%)‡ | ||
| Hispanic | 33 (11.1) | 38 (12.7) |
| Non-Hispanic white | 240 (80.5) | 233 (77.9) |
| Non-Hispanic black | 8 (2.7) | 9 (3.0) |
| Non-Hispanic other | 17 (5.7) | 19 (6.4) |
| Married or living as married — no. (%) | 203 (68.1) | 209 (69.9) |
| Body-mass index§ | 30.6±7.0 | 30.0±6.5 |
|
No. of vaginal deliveries — no. (%) | ||
| 0 | 35 (11.7) | 35 (11.7) |
| 1 or 2 | 146 (49.0) | 145 (48.5) |
| ≥3 | 117 (39.3) | 119 (39.8) |
| Previous surgery for urinary incontinence — no./total no. (%) | 38/297 (13) | 41/298 (14) |
| Previous surgery for prolapse — no./total no. (%) | 13/297 (4) | 10/298 (3) |
| Postmenopausal — no./total no. (%) | 209/297 (70) | 206/298 (69) |
| Current hormone-replacement therapy — no./total no. (%) | 81/297 (27) | 90/298 (30) |
|
Quality-of-life measures | ||
| Urogenital Distress Inventory score¶ | 132.4±48.2 | 136.8±42.5 |
| Incontinence Impact Questionnaire score|| | 150.0±97.5 | 153.1±97.4 |
|
Pad-test weight — g | ||
| Median | 11.5 | 13.7 |
| 10th–90th percentile | 3.8–89.1 | 3.3–84.5 |
|
Incontinence episodes — no./day | ||
| Median | 2.7 | 2.7 |
| 10th–90th percentile | 0.7–6.7 | 0.7–6.7 |
|
Urinary-incontinence symptom score** | ||
| Stress score | 19.2±4.6 | 19.5±4.6 |
| Urge score | 5.9±4.0 | 6.6±4.0 |
|
Urodynamic measures | ||
| Urodynamic stress incontinence — no./total no. (%) | 246/291 (85) | 259/298 (87) |
| Valsalva leak-point pressure — cm of water†† | 114.4±43.1 | 124.2±41.4 |
| Maximum urethral closure pressure — cm of water‡‡ | 66.6±34.0 | 69.3±31.1 |
| Detrusor overactivity — no./total no. (%) | 38/292 (13) | 32/297 (11) |
Plus–minus values are means ±SD. Percentages may not total 100 because of rounding. Data on pad-test weight were available for 594 women; data on incontinence episodes per day for 593 women; data on Valsalva leak-point pressure for 372 women, and data on maximum urethral closure pressure for 539 women.
Other demographic characteristics are listed in Table 1 in the Supplementary Appendix.
Race or ethnic group was self-reported.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Scores on the Urogenital Distress Inventory range from 0 to 300, with higher scores indicating greater distress.
Scores on the Incontinence Impact Questionnaire range from 0 to 400, with higher scores indicating more negative effect on quality of life.20
Symptom scores are the sum of responses from nine questions regarding stress symptoms (with scores ranging from 0 to 27 and higher scores indicating greater severity) and six questions regarding urge symptoms (with scores ranging from 0 to 18 and higher scores indicating greater severity), adapted from the Medical, Epidemiological, and Social Aspects of Aging questionnaire.16
Valsalva leak-point pressure refers to the vesical pressure at the time of leakage. There was a significant difference between the two groups in baseline Valsalva leak-point pressure (P = 0.03).
Maximum urethral closure pressure is the maximum difference between the urethral pressure and the intravesical pressure measured from a profile obtained during a motorized constant catheter withdrawal from the urethra.
STATISTICAL ANALYSIS
With the use of a power analysis, we estimated that with 294 women in each group, the study would have 80% power to show equivalence between the two sling procedures, with an equivalence margin of ±12 percentage points, at a two-sided significance level of 5%. The margin of ±12 was chosen on the basis of clinical considerations and a calculation of the number of patients it was feasible to enroll in the trial. Generalized linear modeling, assuming a logit link and binomial distribution, was used for calculating the rates of treatment success. Standard errors of rates of treatment success were obtained by application of the delta method.18 A determination of equivalence required the entire 95% confidence interval for the difference between the two surgical treatments to be within the equivalence margin.
To minimize bias toward determining equivalence, data from women who were treated per protocol (i.e., were eligible and had received the assigned surgery) were included in the primary analysis.19 A secondary analysis of the primary outcome was performed on the intention-to-treat population. Analyses of secondary outcomes were also performed on the intention-to-treat population. A planned subgroup analysis was performed according to whether the women received or did not receive concomitant surgery. Models for the composite primary outcome were adjusted for site. Models were also adjusted for the Valsalva leak-point pressure (for which values were not balanced between the groups after randomization) and for maximal urethral closure pressure (a related measure of urethral function). Interactions between treatment and measures of urethral function were also assessed. The rates of treatment success were calculated with the assumption that women who were lost to follow-up had treatment success, and sensitivity analyses were performed in which these women were excluded and in which they were considered not to have had treatment success. Fisher’s exact test was used to compare the proportions of patients in each group who had one or more adverse events. Continuous outcomes were analyzed with the use of least-squares modeling methods. Generalized linear modeling was also used for the unplanned sub-analysis comparing outcomes between the two transobturator approaches. No formal adjustment for multiple comparisons has been made.
A planned time-to-event interim analysis of the primary outcome of treatment success according to objective criteria was conducted when 33% of the anticipated treatment failures occurred. We adjusted the primary outcome analysis for this interim data analysis by assigning nominal alpha values of 0.049 to the 95% confidence intervals. Analyses were performed with the use of SAS statistical software, version 9.2 (SAS Institute).
RESULTS
STUDY POPULATION AND ASSIGNED TREATMENT
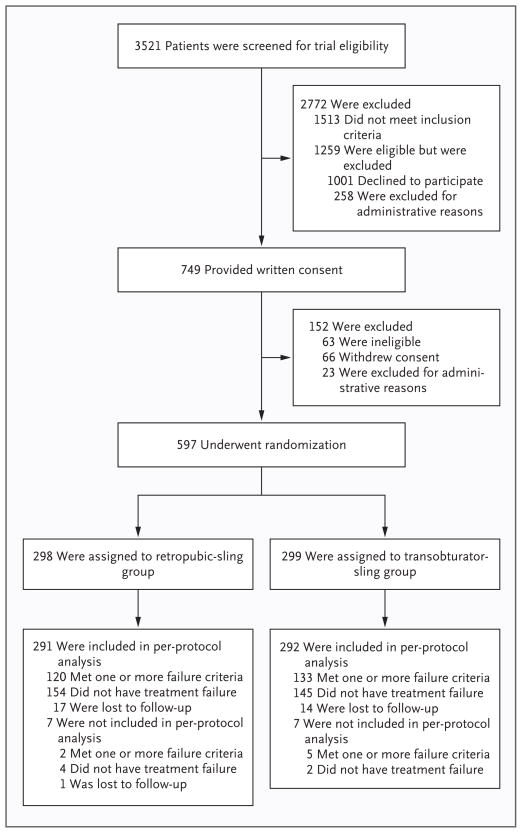
Between April 2006 and June 2008, a total of 3521 women were screened for eligibility; 1259 were considered to be eligible for inclusion in the study, and 597 were randomly assigned to receive either a retropubic sling (298 women) or a transobturator sling (299 women) (Fig. 1). A total of 291 of the 298 women in the retropubic-sling group and 292 of the 299 women in the transobturator-sling group were included in the per-protocol analysis. The median number of study procedures performed by each of the 43 surgeons during the study period was 10 (range, 2 to 58), and the median number of procedures performed according to site was 66 (range, 41 to 86). A total of 565 women — 94% of those in the retropubic-sling group and 95% of those in the transobturator-sling group — were assessed for treatment success at the 12-month visit or were considered to have had a treatment failure at or before that visit. The analysis of treatment failure at 12 months included data from up to 515 days after randomization.
Figure 1. Study Enrollment, Randomization, and Assessment.
The baseline demographic and clinical characteristics were similar between the two groups (Table 1, and Table 1 in the Supplementary Appendix). The mean Valsalva leak-point pressure was lower in the retropubic-sling group than in the transobturator-sling group (114.4 vs. 124.2 cm of water); otherwise the groups were well matched.
OUTCOMES
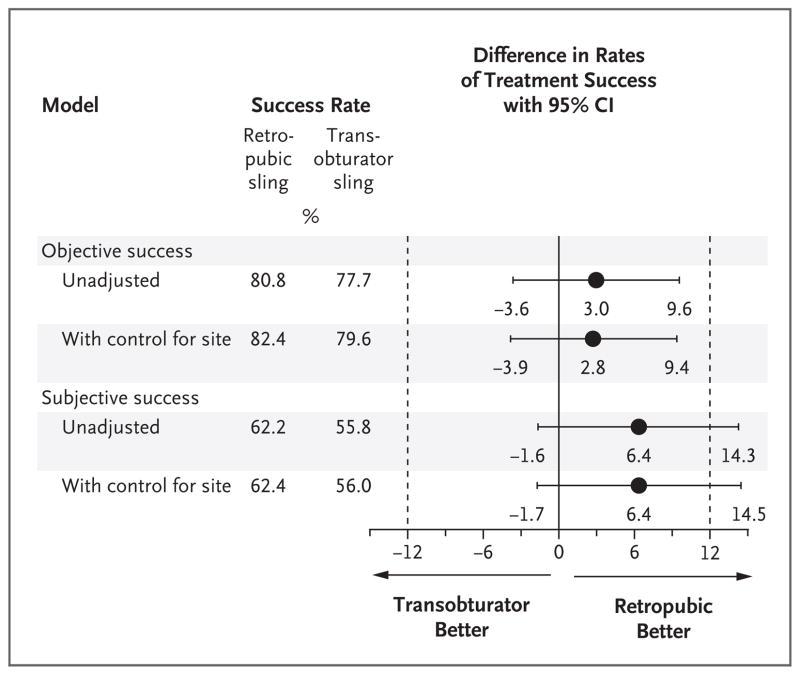
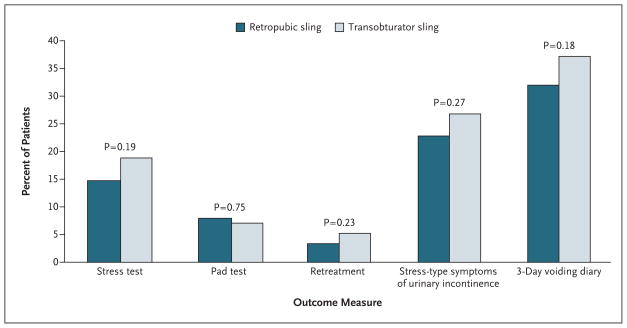
The unadjusted rates of treatment success with the retropubic and transobturator procedures according to objective criteria met the predefined criteria for equivalence (80.8% in the retropubic-sling group and 77.7% in the transobturator-sling group; 3.0 percentage-point difference; 95% confidence interval [CI], −3.6 to 9.6). The unadjusted rates of treatment success according to subjective criteria did not differ significantly between the two procedures but did not meet the predefined criteria for equivalence (62.2% and 55.8%, respectively, 6.4 percentage-point difference; 95% CI, −1.6 to 14.3) (Fig. 2). There was no material change in the rates of treatment success according to objective or subjective criteria when the analyses were adjusted for site or for the urodynamic measures of Valsalva leak-point pressure and maximal urethral closure pressure. There were no significant interactions between treatment and Valsalva leak-point pressure or maximal urethral closure pressure (P = 0.47 and P = 0.29 for interaction between treatment and Valsalva leak-point pressure and maximal urethral closure pressure, respectively, with respect to objectively assessed success; P = 0.71 and P = 0.38 for interaction between treatment and Valsalva leak-point pressure and maximal urethral closure pressure, respectively, with respect to subjectively assessed success). The rate of the occurrence of each component of the objective and subjective definitions of treatment success, as a percentage of all patients, did not differ significantly between the groups (Fig. 3).
Figure 2. Assessment of Equivalence at 12 Months between a Retropubic and a Transobturator Midurethral Sling as Treatment for Urinary Incontinence.
The difference in the rates of treatment success (retropubic minus transobturator) at 12 months is shown, with two-sided 95% confidence intervals (CIs). A value greater than 0 percentage points indicates that there is a higher success rate with the retropubic sling than with the transobturator sling; a value less than 0 indicates that there is a higher success rate with the transobturator sling than with the retropubic sling. If the entire confidence interval lies within a prespecified range of −12 to +12 percentage points, the retropubic and transobturator slings can be considered to be equivalent.
Figure 3. Proportion of Patients with Treatment Failure at 12 Months, According to Objective and Subjective Criteria.
Retreatment includes surgical, pharmacologic, or behavioral treatment, placement of a new device, and other treatment. Stress-type symptoms of urinary incontinence were assessed with the use of the Medical, Epidemiological and Social Aspects of Aging questionnaire.16
The results of the analysis of the intention-to-treat population were similar to those of the analysis of the per-protocol population. The results were also similar when patients who were lost to follow-up were considered to have had treatment failure and when patients who were lost to follow-up were excluded. The effect of treatment on the rates of treatment success, either objective or subjective, did not differ significantly according to whether the woman did or did not undergo concomitant surgery (P = 0.61 for the interaction between treatment and concomitant surgery with respect to objectively assessed success and P = 0.81 for the interaction between treatment and concomitant surgery with respect to subjectively assessed success.) After adjustment for site and treatment group, patients who underwent concomitant surgery had significantly higher rates of treatment success according to objective criteria than did those who did not undergo concomitant surgery (87.9% vs. 78.9%, P = 0.015), but the rates of treatment success according to subjective criteria did not differ significantly (61.9% and 58.3%, respectively; P=0.46).
Although the study was not powered for a comparison between the two transobturator approaches (the in-to-out method was used in the case of 161 women and the out-to-in method in the case of 137 women; one woman assigned to receive the transobturator sling received the retro-pubic sling instead), and assignment to these approaches was not randomized, a post hoc comparison showed that there were no significant differences between the two approaches in the rates of treatment success according to either objective or subjective criteria (objective rates: 77.6% with the in-to-out method and 77.4% with the out-to-in method, P = 0.96; subjective rates: 55.3% and 56.2%, with the two methods, respectively, P = 0.87). Therefore, the similarity in outcomes between the two main treatment groups was not due to our having averaged the difference in rates between the two transobturator groups.
The median estimated blood loss and operative time during the sling portion of the procedure were modestly, but significantly, higher in the retropubic-sling group than in the transobturator-sling group (blood loss, 50 ml vs. 25 ml; P<0.001; operative time, 30 minutes vs. 25 minutes; P<0.001).
ADVERSE EVENTS
The rates of intraoperative and postoperative adverse events and complications are shown in Table 2, and in Table 2 in the Supplementary Appendix. Bladder perforations from trocar passage and voiding dysfunction requiring surgical intervention were uncommon but occurred only in women who received the retropubic sling; women in this group were also more likely than women in the transobturator-sling group to have a higher (100 ml or more) residual volume after voiding at the time of discharge from the hospital (P = 0.02) and to have postoperative urinary tract infections (P = 0.04). More vaginal perforations occurred in the transobturator-sling group than in the retro-pubic-sling group (13 vs. 6); the majority of those in the transobturator-sling group occurred when the in-to-out approach was used (10). The frequency of neurologic symptoms was also higher in the transobturator-sling group than in the retropubic-sling group (P = 0.01); weakness in the upper leg was the most common neurologic symptom, occurring in 24 (60%) of those who reported neurologic symptoms.
Table 2.
Adverse Events, According to Treatment Group, Severity, and System.*
| Adverse Event | Retropubic Sling (N = 298) | Transobturator Sling (N = 299) | P Value | ||
|---|---|---|---|---|---|
| Events | Patients | Events | Patients | ||
| no. | no. (%) | no. | no. (%) | ||
| Serious adverse event | 43 | 41 (13.8) | 20 | 19 (6.4) | 0.003 |
| Wound-related event | 10 | 9 (3.0) | 5 | 5 (1.7) | 0.30 |
| Mesh exposure† | 9 | 8 (2.7) | 1 | 1 (0.3) | |
| Mesh erosion‡ | 1 | 1 (0.3) | 1 | 1 (0.3) | |
| Surgical-site infection | 0 | 0 | 2 | 2 (0.7) | |
| Granulation tissue | 0 | 0 | 1 | 1 (0.3) | |
| Genitourinary event | 23 | 23 (7.7) | 13 | 13 (4.3) | 0.09 |
| Urethral perforation | 1 | 1 (0.3) | 0 | 0 | |
| Bladder perforation§ | 15 | 15 (5.0) | 0 | 0 | |
| Vaginal epithelial perforation | 6 | 6 (2.0) | 13 | 13 (4.3) | |
| Recurrent cystitis, leading to diagnostic cystoscopy¶ | 1 | 1 (0.3) | 0 | 0 | |
| Vascular or hematologic event | 1 | 1 (0.3) | 1 | 1 (0.3) | >0.99 |
| Pulmonary embolus | 0 | 0 | 1 | 1 (0.3) | |
| Postoperative bleeding | 1 | 1 (0.3) | 0 | 0 | |
| Neurologic symptoms|| | 1 | 1 (0.3) | 0 | 0 | 0.50 |
| Voiding dysfunction requiring surgery, use of catheter, or both | 9 | 8 (2.7) | 0 | 0 | 0.004 |
| Other (urothelial abrasion) | 0 | 0 | 1 | 1 (0.3) | 0.50 |
| Adverse events, grades I and II | 151 | 110 (36.9) | 132 | 89 (29.8) | 0.07 |
| Wound-related event | 6 | 6 (2.0) | 5 | 5 (1.7) | 0.77 |
| Mesh exposure† | 4 | 4 (1.3) | 3 | 3 (1.0) | |
| Surgical-site infection | 2 | 2 (0.7) | 2 | 2 (0.7) | |
| Genitourinary event | 46 | 40 (13.4) | 27 | 24 (8.0) | 0.04 |
| Vascular or hematologic event | 20 | 18 (6.0) | 7 | 7 (2.3) | 0.03 |
| Neurologic symptoms | 15 | 12 (4.0) | 31 | 28 (9.4) | 0.01 |
| Numbness | 8 | 6 (2.0) | 9 | 7 (2.3) | |
| Weakness | 7 | 7 (2.3) | 22 | 21 (7.0) | |
| Voiding dysfunction | 16 | 10 (3.4) | 5 | 4 (1.3) | 0.11 |
| Self-reported pain ≥6 wk after procedure | 7 | 7 (2.3) | 7 | 6 (2.0) | 0.79 |
| New urge incontinence** | 0 | 0 | 1 | 1 (0.3) | 0.50 |
| Persistent urge incontinence†† | 54 | 36 (12.1) | 55 | 30 (10.0) | 0.44 |
| Other‡‡ | 7 | 6 (2.0) | 6 | 6 (2.0) | >0.99 |
An adverse event was defined as a deviation from the normal intraoperative or postoperative course. The severity grade was determined with the use of a slightly modified version of the Dindo17 classification, which is based on the level of therapy required to treat an event. Grades I and II events are listed as adverse events, and grades III and IV as serious adverse events. An event was considered to be a serious adverse event when surgical, endoscopic, or radiologic intervention was required or a life-threatening complication requiring intensive care developed. Specific information regarding the modified Dindo17 grading and system events are provided in Table 2 in the Supplementary Appendix.
Mesh exposure was defined as mesh visualized in the vagina through a prior incision area with or without an inflammatory reaction.
Mesh erosion was defined as erosion, after primary healing, into an organ or surrounding tissue.
All the bladder perforations occurred at the time of trocar placement and required minor surgical intervention to remove the trocar and replace it in the correct position.
Recurrent cystitis was defined as three or more presumed urinary tract infections that required treatment within 1 year, after the 6-week visit.
Neurologic symptoms were identified by self-report on a standardized form that asked about new paresthesias or alterations in motor function that developed between the time of the surgery and the 6-week visit. Symptoms were not assessed after the 6-week visit. The location of numbness or weakness was ascertained by having the patient mark a body map. The one serious neurologic adverse event that occurred was numbness in the patient’s upper leg that necessitated surgical intervention.
New urge urinary incontinence was considered to be present when a patient who had had only stress incontinence at baseline answered any question in the Medical, Epidemiological, and Social Aspects of Aging questionnaire16 regarding urge incontinence, at or after the 6-week visit, with “sometimes” or “often” or initiated treatment with anticholinergic medication for the treatment of urge urinary incontinence.
Persistent urge urinary incontinence was considered to be present when a patient who had had symptoms of both stress and urge incontinence (with stress incontinence predominant) at baseline answered any question in the Medical, Epidemiological, and Social Aspects of Aging questionnaire16 regarding urge incontinence with “sometimes” or “often” or initiated treatment with anticholinergic medication for the treatment of urge urinary incontinence.
Other adverse events included granulation tissue, anxiety, thrush, wound-edge separation, minor wound, medication reaction, and skin irritation.
The rates of patient satisfaction with the treatment were similar between the retropubic-sling group and the transobturator-sling group (85.9% and 90%, respectively; P = 0.14). There were no significant differences between the groups in changes between baseline and postoperative “distress” and “bother” scores (which measure the distress caused by symptoms of urinary incontinence and the degree to which the woman is bothered by those symptoms) or the effect of these symptoms on quality of life (Table 3 in the Supplementary Appendix).
DISCUSSION
This large, multicenter, comparative-effectiveness trial showed that there was statistical and clinical equivalence in the rates of treatment success according to objective criteria between the two most commonly performed midurethral sling procedures for the treatment of stress incontinence in women. The rates of treatment success according to subjective criteria appeared to be similar between the two procedures, but did not reach the predetermined criteria for equivalence. Patient-reported satisfaction with the results of the procedure, postoperative bother scores, and improvement in quality of life were also similar between the two procedures. The types of complications differed between the procedures; there was a higher frequency of bladder perforations, postoperative voiding dysfunction requiring surgical intervention, and urinary tract infections in the retropubic-sling group, whereas the frequency of neurologic symptoms was higher in the transobturator-sling group.
The rates of treatment success according to objective criteria that were reported in a recent Cochrane review8 (84% with the transobturator sling and 88% with the retropubic sling; relative risk, 0.96; 95% CI, 0.93 to 0.99) and in two meta-analyses7,13 (86 to 99% with the retropubic sling and 84 to 98% with the transobturator sling) are slightly higher than the rates of treatment success reported here. The use of a composite outcome to define treatment success in this trial, in contrast to the single outcome measure used in many of the previous studies of midurethral slings, may account for the apparently lower rates of treatment success in this study. Rates of treatment success as defined by validated subjective measures that evaluate many factors of continence and bladder function have been shown to be lower than rates of treatment success as defined by objective measures.21,22 However, subjective measures may be a more important outcome measure for patients, since they quantitate the effect of treatment on the patient’s quality of life. The inclusion of both objective and subjective outcomes is a strength of the present trial, particularly given the increasing recognition of the importance of measuring patient-oriented outcomes.
The overall number of serious adverse events as categorized according to the Dindo classification was higher in the retropubic-sling group than in the transobturator-sling group. Most of this difference was due to an increase in mesh exposure, voiding dysfunction requiring surgical intervention, and bladder perforation at the time of sling placement (although bladder perforation did not require surgical intervention other than replacement of the trocar). The frequency of non-serious adverse events (which were managed by expectant care or pharmacologic or other non-surgical interventions) varied according to the sling procedure. Patients in the transobturator-sling group were more likely to report neurologic symptoms, such as leg weakness and groin numbness (which were managed with expectant care), whereas postoperative urinary tract infections were more common after placement of retropubic slings. Our findings are consistent with previous reports of higher rates of voiding dysfunction after a retropubic-sling procedure than after a transobturator-sling procedure.23 The higher rate of this complication in the retropubic-sling group may be due to the relatively greater urethral obstruction that results from the fact that the retropubic sling is placed at a more vertical angle than is the transobturator sling.21,24 Two different approaches to the transobturator route were used in our trial, with the choice between the two left to the discretion of the surgeon. Although our study was not designed to compare these approaches, a subanalysis suggested that they resulted in similar rates of efficacy and adverse events, except that there was a higher rate of vaginal epithelial perforations with the in-to-out approach.
The number of retropubic and transobturator sling procedures that are performed to treat stress incontinence has increased dramatically in the United States and Europe.25 A recent Cochrane review8 and three meta-analyses7,13,23 evaluating outcomes after retropubic and transobturator sling procedures showed no significant differences in objective and subjective outcomes between the two sling approaches. However, most of the studies had insufficient sample sizes to assess differences in adverse events associated with each approach. Furthermore, the majority of the studies were designed as superiority trials. Therefore, when no significant difference was found between groups, investigators could not conclude that the treatments were equivalent or that one was not inferior to the other. One previous noninferiority trial that was performed at three clinical sites involved 180 women with urodynamic stress incontinence who were randomly assigned to undergo either a transobturator or a retropubic sling procedure.21 Treatment failure, defined as the presence of abnormal bladder function (incontinence, voiding dysfunction, or both), occurred in 46.6% of the women in the transobturator-sling group and 42.7% of the women in the retropubic-sling group. The authors concluded that the transobturator midurethral sling was not inferior to the retropubic sling; however, they could not determine whether the treatments were equivalent. In contrast to the present results, concomitant surgery for pro-lapse did not affect the treatment outcomes.
Our data suggest that patients with more severe urethral dysfunction, as reflected by lower Valsalva leak-point pressure or maximal urethral-closure pressure values, were no more likely to have treatment failure with the transobturator midurethral sling than with the retropubic midurethral sling, although the number of women in our study with a Valsalva leak-point pressure of 60 cm of water or less or a maximal urethral closure pressure of 20 cm of water or less was small. Although women who underwent the retropubic-sling procedure had lower baseline Valsalva leak-point pressures, this measure did not influence the relationship between the treatment and the outcome. Similar to the results of previous studies,26,27 we found that the transobturator and retropubic sling methods had similar efficacy regardless of sphincteric function. A large observational study of women undergoing a midurethral sling procedure showed that a Valsalva leak-point pressure of 60 cm of water or less or a maximal urethral closure pressure of 20 cm of water or less was an independent predictor of treatment failure with both retropubic and transobturator slings,28 whereas, in a randomized trial, a low Valsalva leak-point pressure was a predictor of a poor outcome with a transobturator sling but not with a retropubic sling.29 Further study is warranted.
Some strengths of the present trial include the relatively large sample size, the randomized, multicenter, nationally representative design (9 centers and 43 certified surgeons), the large, well-defined surgical cohort that included patients undergoing concomitant prolapse surgery, and the use of a well-defined composite outcome that included both objective and subjective criteria for treatment success. Furthermore, the postoperative course was monitored closely, to carefully identify and characterize early differences in side effects such as pain, voiding dysfunction, neurologic impairment, and mesh complications.
In summary, the rates of objectively assessed success of treatment for stress incontinence with a transobturator-sling approach and a retropubic-sling approach were equivalent at 1 year. The rates of subjectively assessed treatment success were slightly higher in the retropubic-sling group than in the transobturator-sling group and did not meet the predefined criteria for equivalence. However, the complications associated with the two procedures differ, and clinicians should counsel patients regarding these complications when discussing surgical options for stress urinary incontinence.
Supplementary Material
Acknowledgments
Supported by cooperative agreements (U01 DK58225, U01 DK58229, U01 DK58234, U01 DK58231, U01 DK60379, U01 DK60380, U01 DK60393, U01 DK60395, U01 DK60397, and U01 DK60401) from the National Institute of Diabetes and Digestive and Kidney Diseases and by the National Institute of Child Health and Human Development.
We thank Dr. Stuart Pocock for assistance in the design of the trial.
Footnotes
The names of the Urinary Incontinence Treatment Network investigators are listed in the Supplementary Appendix, available with the full text of this article at NEJM.org.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165:537–42. doi: 10.1001/archinte.165.5.537. [DOI] [PubMed] [Google Scholar]
- 2.Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc. 1998;46:473–80. doi: 10.1111/j.1532-5415.1998.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 3.Hampel C, Wienhold D, Benken N, Eggersmann C, Thuroff JW. Definition of overactive bladder and epidemiology of urinary incontinence. Urology. 1997;50(Suppl):4–14. doi: 10.1016/s0090-4295(97)00578-5. [DOI] [PubMed] [Google Scholar]
- 4.Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61:37–49. doi: 10.1016/s0090-4295(02)02243-4. [DOI] [PubMed] [Google Scholar]
- 5.Thom DH, Nygaard IE, Calhoun EA. Urologic Diseases in America Project: urinary incontinence in women — national trends in hospitalizations, office visits, treatment and economic impact. J Urol. 2005;173:1295–301. doi: 10.1097/01.ju.0000155679.77895.cb. [DOI] [PubMed] [Google Scholar]
- 6.Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:81–6. doi: 10.1007/BF01902378. [DOI] [PubMed] [Google Scholar]
- 7.Novara G, Ficarra V, Boscolo-Berto R, Secco S, Cavalleri S, Artibani W. Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol. 2007;52:663–78. doi: 10.1016/j.eururo.2007.06.018. [Erratum, Eur Eurol 2007;52:1548.] [DOI] [PubMed] [Google Scholar]
- 8.Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2009;4:CD006375. doi: 10.1002/14651858.CD006375.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Ward KL, Hilton P. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol. 2004;190:324–31. doi: 10.1016/j.ajog.2003.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: important outcomes for future clinical trials. J Urol. 2008;180:1890–7. doi: 10.1016/j.juro.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 11.Deng DY, Rutman M, Raz S, Rodriguez LV. Presentation and management of major complications of midurethral slings: are complications under-reported? Neurourol Urodyn. 2007;26:46–52. doi: 10.1002/nau.20357. [DOI] [PubMed] [Google Scholar]
- 12.Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306–13. (In French.) [PubMed] [Google Scholar]
- 13.Latthe PM, Foon R, Toozs-Hobson P. Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG. 2007;114:522–31. doi: 10.1111/j.1471-0528.2007.01268.x. [Erratum, BJOG 2007;114:1311.] [DOI] [PubMed] [Google Scholar]
- 14.Urinary Incontinence Treatment Network. The Trial of Mid-Urethral Slings (TOMUS): design and methodology. J Applied Res. 2008;8:1–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Schäfer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry and pressure flow studies. Neurourol Urodyn. 2002;21:261–74. doi: 10.1002/nau.10066. [DOI] [PubMed] [Google Scholar]
- 16.Herzog AR, Diokno AC, Brown MB, Normolle DP, Brock BM. Two-year incidence, remission, and change patterns of urinary incontinence in noninstitutionalized older adults. J Gerontol. 1990;45:M67–M74. doi: 10.1093/geronj/45.2.m67. [DOI] [PubMed] [Google Scholar]
- 17.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schabenberger O. Introducing the GLIMMIX procedure for generalized linear mixed models. Cary, NC: SAS Institute; 2005. [Google Scholar]
- 19.Brittain E, Lin D. A comparison of intent-to-treat and per-protocol results in antibiotic non-inferiority trials. Stat Med. 2005;24:1–10. doi: 10.1002/sim.1934. [DOI] [PubMed] [Google Scholar]
- 20.Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Qual Life Res. 1994;3:291–306. doi: 10.1007/BF00451721. [DOI] [PubMed] [Google Scholar]
- 21.Barber MD, Kleeman S, Karram MK, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2008;111:611–21. doi: 10.1097/AOG.0b013e318162f22e. [DOI] [PubMed] [Google Scholar]
- 22.Albo ME, Richter HE, Brubaker L, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356:2143–55. doi: 10.1056/NEJMoa070416. [DOI] [PubMed] [Google Scholar]
- 23.Novara G, Galfano A, Boscolo-Berto R, et al. Complication rates of tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials comparing tension-free midurethral tapes to other surgical procedures and different devices. Eur Urol. 2008;53:288–308. doi: 10.1016/j.eururo.2007.10.073. [DOI] [PubMed] [Google Scholar]
- 24.Whiteside JL, Walters MD. Anatomy of the obturator region: relations to a transobturator sling. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:223–6. doi: 10.1007/s00192-004-1143-y. [DOI] [PubMed] [Google Scholar]
- 25.Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in stress urinary incontinence inpatient procedures in the United States, 1979–2004. Am J Obstet Gynecol. 2009;200(5):521.e1–521.e6. doi: 10.1016/j.ajog.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barber MD, Kleeman S, Karram MM, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol. 2008;199(6):666.e1–666.e7. doi: 10.1016/j.ajog.2008.07.050. [DOI] [PubMed] [Google Scholar]
- 27.Costantini E, Lazzeri M, Giannantoni A, Bini V, del Zingaro M, Porena M. Pre-operative MUCP and VLPP did not predict long-term (4-year) outcomes after transobturator mid-urethral sling. Urol Int. 2009;83:392–8. doi: 10.1159/000251177. [DOI] [PubMed] [Google Scholar]
- 28.Stav K, Dwyer PL, Rosamilia A, Schierlitz L, Lim YN, Lee J. Risk factors of treatment failure of midurethral sling procedures for women with urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:149–55. doi: 10.1007/s00192-009-1020-9. [DOI] [PubMed] [Google Scholar]
- 29.Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Skorupski P. The clinical effectiveness of retropubic (IVS-02) and transobturator (IVS-04) midurethral slings: randomized trial. Eur Urol. 2009;56:24–30. doi: 10.1016/j.eururo.2009.02.038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.